The First Case of Human Hepatic Fasciolosis Presented as Hepatic Pseudotumor Histopathologically Diagnosed in Romania—A Case Report
Abstract
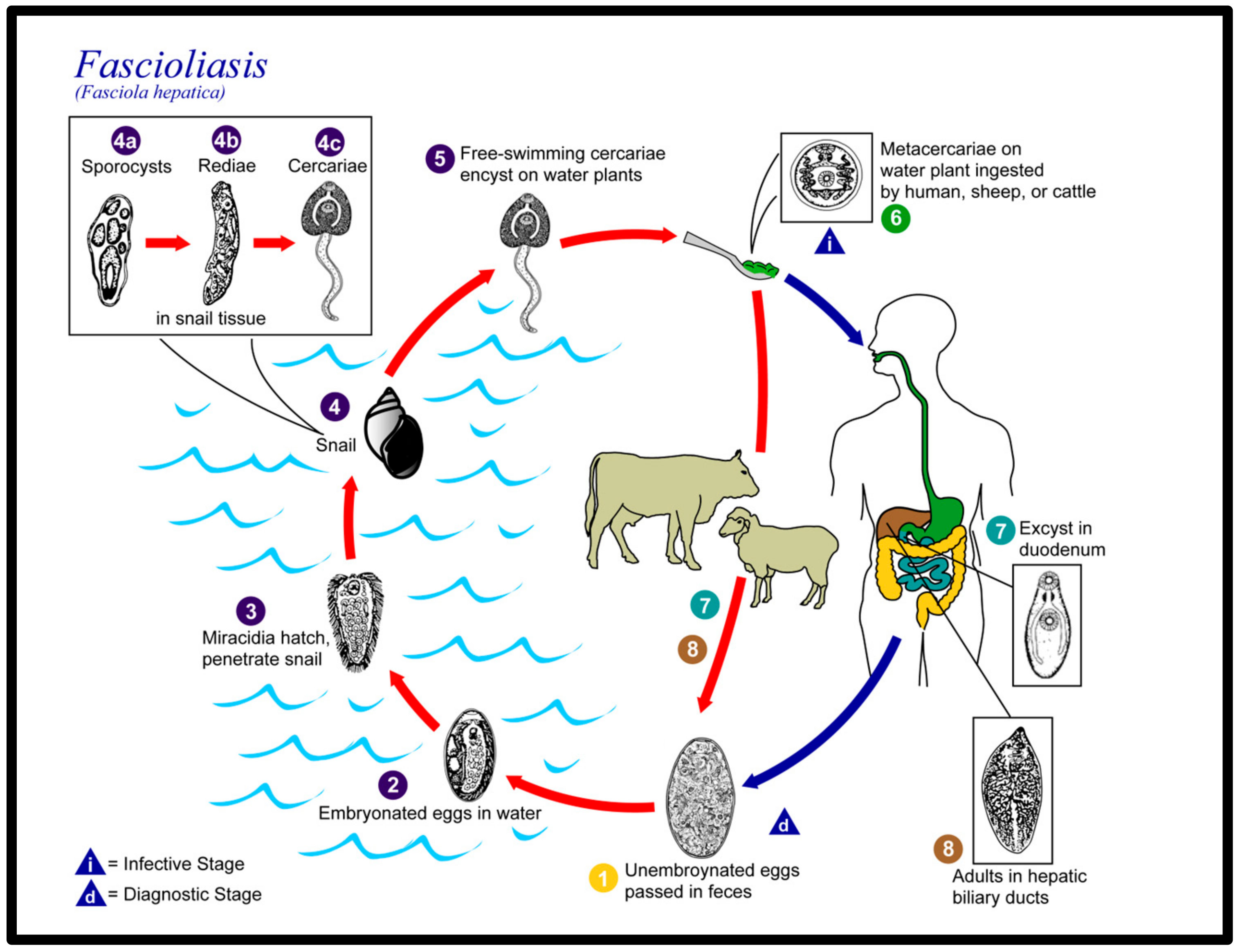
1. Introduction
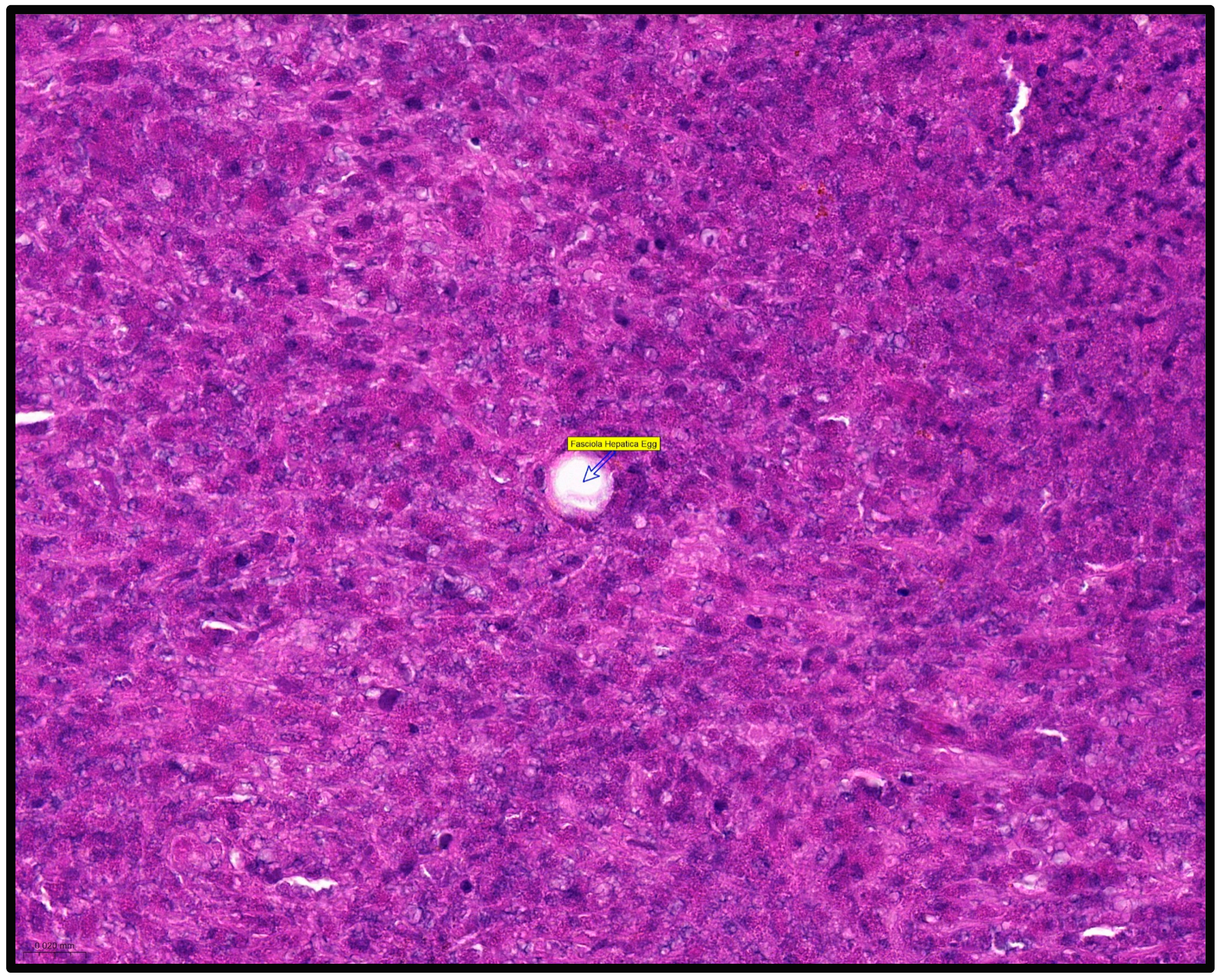
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fürst, T.; Duthaler, U.; Sripa, B.; Utzinger, J.; Keiser, J. Trematode infections: Liver and lung flukes. Infect Dis. Clin. N. Am. 2012, 26, 399–419. [Google Scholar] [CrossRef] [PubMed]
- Gabrielli, S.; Calderini, P.; Dall’oglio, L.; Paola, D.A.; Maurizio, D.A.; Federico, S.; Cancrini, G. Parasitological and Molecular Observations on a Little Family Outbreak of Human Fasciolosis Diagnosed in Italy. Sci. World J. 2014, 2014, 417159. [Google Scholar] [CrossRef] [PubMed]
- Mas-Coma, S.; Bargues, M.D.; Valero, M.A. Diagnosis of human fascioliasis by stool and blood techniques: Update for the present global scenario. Parasitology 2014, 141, 1918–1946. [Google Scholar] [CrossRef]
- Qureshi, A.W.; Zeb, A.; Mansoor, A.; Hayat, A.; Mas-Coma, S. Fasciola hepatica infection in children actively detected in a survey in rural areas of Mardan district, Khyber Pakhtunkhawa province, northern Pakistan. Parasitol. Int. 2018, 69, 39–46. [Google Scholar] [CrossRef]
- Sah, R.; Khadka, S.; Khadka, M.; Gurubacharya, D.; Sherchand, J.B.; Parajuli, K.; Shah, N.P.; Kattel, H.P.; Pokharel, B.M.; Rijal, B. Human fascioliasis by Fasciola hepatica: The first case report in Nepal. BMC Res. Notes 2017, 10, 439. [Google Scholar] [CrossRef]
- Outa, J.O.; Sattmann, H.; Köhsler, M.; Walochnik, J.; Jirsa, F. Diversity of digenean trematode larvae in snails from Lake Victoria, Kenya: First reports and bioindicative aspects. Acta Trop. 2020, 206, 105437. [Google Scholar] [CrossRef]
- Carolus, H.; Muzarabani, K.C.; Hammoud, C.; Schols, R.; Volckaert, F.A.; Barson, M.; Huyse, T. A cascade of biological invasions and parasite spillback in man-made Lake Kariba. Sci. Total Environ. 2018, 659, 1283–1292. [Google Scholar] [CrossRef]
- Carmona, C.; Tort, J. Fasciolosis in South America: Epidemiology and control challenges. J. Helminthol. 2016, 91, 99–109. [Google Scholar] [CrossRef]
- Parkinson, M.; O’neill, S.M.; Dalton, J.P. Controlling fasciolosis in the Bolivian Altiplano. Trends Parasitol. 2007, 23, 238–239. [Google Scholar] [CrossRef]
- Sierra, R.M.Y.; Agramunt, V.H.; Cuervo, P.; Mas-Coma, S. Human fascioliasis in Argentina: Retrospective overview, critical analysis and baseline for future research. Parasites Vectors 2011, 4, 104. [Google Scholar] [CrossRef]
- Hotez, P.J.; Savioli, L.; Fenwick, A. Neglected Tropical Diseases of the Middle East and North Africa: Review of Their Prevalence, Distribution, and Opportunities for Control. PLoS Neglected Trop. Dis. 2012, 6, e1475. [Google Scholar] [CrossRef]
- Temido, H.; Oliveira-Santos, M.; Parente, F.; Santos, L. Fascioliasis—A rare cause of hepatic nodules. BMJ Case Rep. 2017, 2017, 220363. [Google Scholar] [CrossRef]
- Remacha, M.A.; Goñi, M.P.; Espinel, J. Obstructive jaundice of a parasitic etiology. Rev. Esp. Enferm. Dig. 2019, 111, 165–166. [Google Scholar] [CrossRef]
- Otranto, D.; Eberhard, M.L. Zoonotic helminths affecting the human eye. Parasites Vectors 2011, 4, 41. [Google Scholar] [CrossRef]
- Lalor, R.; Cwiklinski, K.; Calvani, N.E.D.; Dorey, A.; Hamon, S.; Corrales, J.L.; Dalton, J.P.; Verissimo, C.D.M. Pathogenicity and virulence of the liver flukes Fasciola hepatica and Fasciola gigantica that cause the zoonosis Fasciolosis. Virulence 2021, 12, 2839–2867. [Google Scholar] [CrossRef]
- McManus, D.P. Recent Progress in the Development of Liver Fluke and Blood Fluke Vaccines. Vaccines 2020, 8, 553. [Google Scholar] [CrossRef]
- Fried, B.; Abruzzi, A. Food-borne trematode infections of humans in the United States of America. Parasitol. Res. 2010, 106, 1263–1280. [Google Scholar] [CrossRef]
- Micic, D.; Oto, A.; Charlton, M.R.; Benoit, J.-L.; Siegler, M. Hiding in the Water. N. Engl. J. Med. 2020, 382, 1844–1849. [Google Scholar] [CrossRef]
- Kain, D.; Mukkala, A.N.; Boggild, A.K. Prolonged antibiotic use leading to Clostridium difficile colitis in an ill returned traveller with acute fascioliasis. J. Travel Med. 2018, 25, 1. [Google Scholar] [CrossRef]
- Kwok, J.; Buxbaum, J.L. Liver fluke. N. Engl. J. Med. 2019, 381, e34. [Google Scholar] [CrossRef]
- Weisenberg, S.A.; Perlada, D.E. Case report: Domestically acquired fascioliasis in northern california. Am. J. Trop. Med. Hyg. 2013, 89, 588–591. [Google Scholar] [CrossRef]
- Caravedo, M.A.; Cabada, M.M. Human Fascioliasis: Current Epidemiological Status and Strategies for Diagnosis, Treatment, and Control. Res. Rep. Trop. Med. 2020, 11, 149–158. [Google Scholar] [CrossRef]
- Centers of Disease Control and Prevention. Available online: https://phil.cdc.gov/Details.aspx?pid=3392 (accessed on 16 May 2023).
- Saba, R.; Korkmaz, M.; Inan, D.; Mamikoğlu, L.; Turhan, Ö.; Günseren, F.; Çevikol, C.; Kabaalioğlu, A. Human fascioliasis. Clin. Microbiol. Infect. 2004, 10, 385–387. [Google Scholar] [CrossRef]
- Torres, G.B.; Iwashita, A.T.; Vargas, C.M.; Luján, L.V.; Bianchi, H.A.; Casanova, R.T. Human fasciolasis and gastrointestinal compromise: Study of 277 patients in the Cayetano Heredia National Hospital (1970–2002). Rev. Gastroenterol. Peru 2004, 24, 143–157. [Google Scholar]
- Chang Wong, M.R.; Pinto Elera, J.O.A.; Guzman Rojas, P.; Terashima Iwashita, A.; Samalvides Cuba, F. Demographic and clinical aspects of hepatic fascioliasis between 2013–2010 in National Hospital Cayetano Heredia, Lima, Peru. Rev. Gastroenterol. Peru 2016, 36, 23–28. [Google Scholar]
- Krsak, M.; Patel, N.U.; Poeschla, E.M. Case Report: Hepatic Fascioliasis in a Young Afghani Woman with Severe Wheezing, High-Grade Peripheral Eosinophilia, and Liver Lesions: A Brief Literature Review. Am. J. Trop. Med. Hyg. 2019, 100, 588–590. [Google Scholar] [CrossRef]
- Aksoy, D.Y.; Kerimoğlu, U.; Oto, A.; Ergüven, S.; Arslan, S.; Unal, S.; Batman, F.; Bayraktar, Y. Fasciola hepatica infection: Clinical and computerized tomographic findings of ten patients. Turk. J. Gastroenterol. 2006, 17, 40–45. [Google Scholar]
- Choi Sy Kim, J.W.; Jang, J.C. Hepatobiliary Fascioliasis with Multiple Aneurysms and Active Bleeding: A Case Report. J. Korean Soc. Radiol. 2015, 72, 291–294. [Google Scholar] [CrossRef]
- Lim, J.H.; Mairiang, E.; Ahn, G.H. Biliary parasitic diseases including clonorchiasis, opisthorchiasis and fascioliasis. Abdom. Imaging 2008, 33, 157–165. [Google Scholar] [CrossRef]
- Taghipour, A.; Zaki, L.; Rostami, A.; Foroutan, M.; Ghaffarifar, F.; Fathi, A.; Abdoli, A. Highlights of human ectopic fascioliasis: A systematic review. Infect Dis. 2019, 51, 785–792. [Google Scholar] [CrossRef]
- Keiser, J.; Engels, D.; Büscher, G.; Utzinger, J. Triclabendazole for the treatment of fascioliasis and paragonimiasis. Expert Opin. Investig. Drugs 2005, 14, 1513–1526. [Google Scholar] [CrossRef]
- Favennec, L.; Ortiz, J.J.; Gargala, G.; Chegne, N.L.; Ayoub, A.; Rossignol, J.F. Double-blind, randomized, placebo-controlled study of nitazoxanide in the treatment of fascioliasis in adults and children from northern Peru. Aliment. Pharmacol. Ther. 2003, 17, 265–270. [Google Scholar] [CrossRef]
- Castillo Contreras, O.B.; Velarde, O.F. Pseudotumor hepático en fasciolosis aguda. Acta Gastroenterol. Latinoam. 2013, 43, 53–58. [Google Scholar] [PubMed]
- Neghina, R.; Neghina, A.M.; Marincu, I.; Iacobiciu, I. Epidemiology and history of human parasitic diseases in Romania. Parasitol. Res. 2011, 108, 1333–1346. [Google Scholar] [CrossRef] [PubMed]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Birlutiu, V.; Birlutiu, R.-M. The First Case of Human Hepatic Fasciolosis Presented as Hepatic Pseudotumor Histopathologically Diagnosed in Romania—A Case Report. Healthcare 2023, 11, 1451. https://doi.org/10.3390/healthcare11101451
Birlutiu V, Birlutiu R-M. The First Case of Human Hepatic Fasciolosis Presented as Hepatic Pseudotumor Histopathologically Diagnosed in Romania—A Case Report. Healthcare. 2023; 11(10):1451. https://doi.org/10.3390/healthcare11101451
Chicago/Turabian StyleBirlutiu, Victoria, and Rares-Mircea Birlutiu. 2023. "The First Case of Human Hepatic Fasciolosis Presented as Hepatic Pseudotumor Histopathologically Diagnosed in Romania—A Case Report" Healthcare 11, no. 10: 1451. https://doi.org/10.3390/healthcare11101451
APA StyleBirlutiu, V., & Birlutiu, R.-M. (2023). The First Case of Human Hepatic Fasciolosis Presented as Hepatic Pseudotumor Histopathologically Diagnosed in Romania—A Case Report. Healthcare, 11(10), 1451. https://doi.org/10.3390/healthcare11101451






