Sleep Quality in Women with Premenstrual Syndrome Is Associated with Metabolic Syndrome-Related Variables
Abstract
1. Introduction
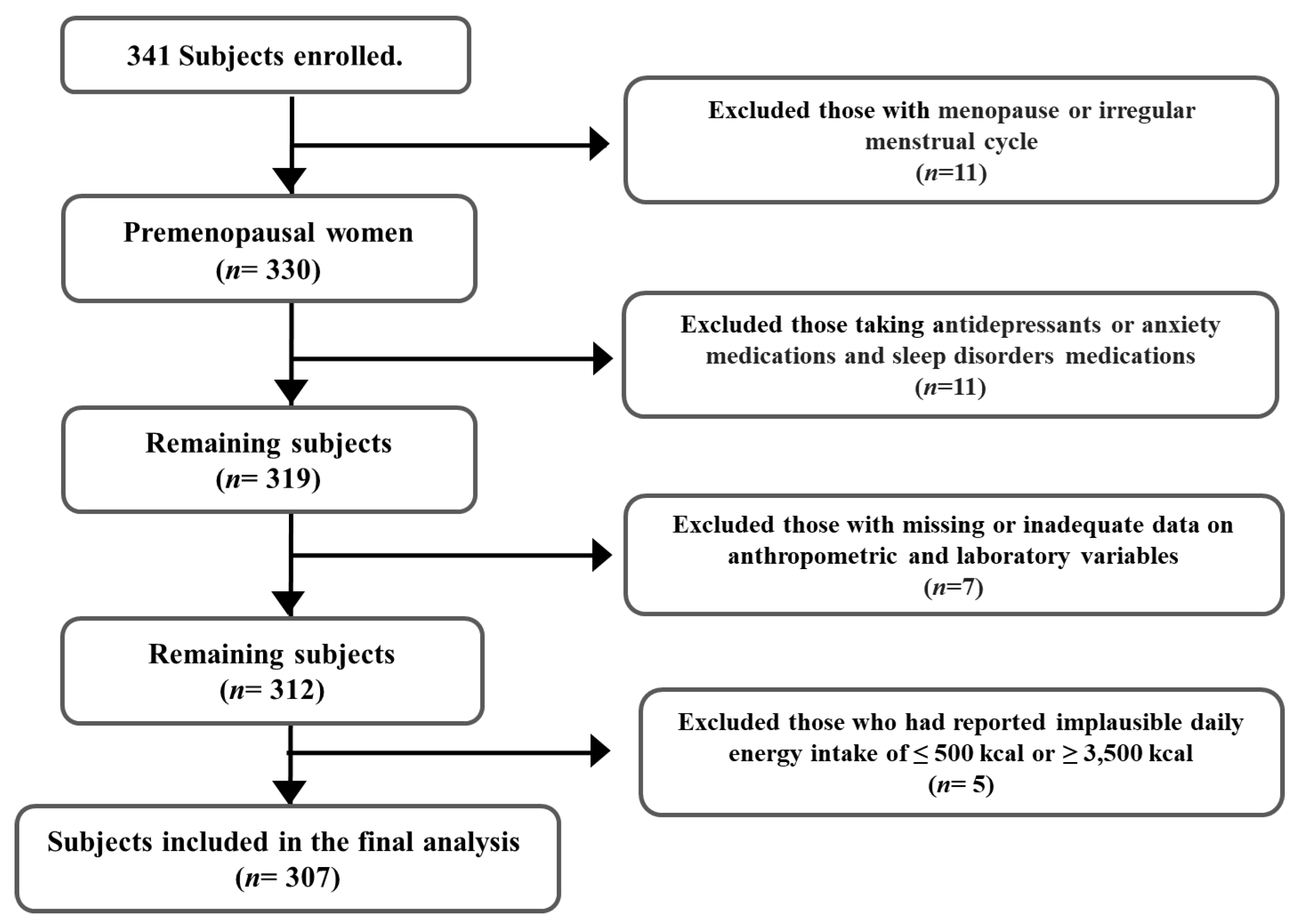
2. Subjects and Methods
2.1. Study Design and Subject Selection
2.2. Data Collection
2.3. Statistical Analyses
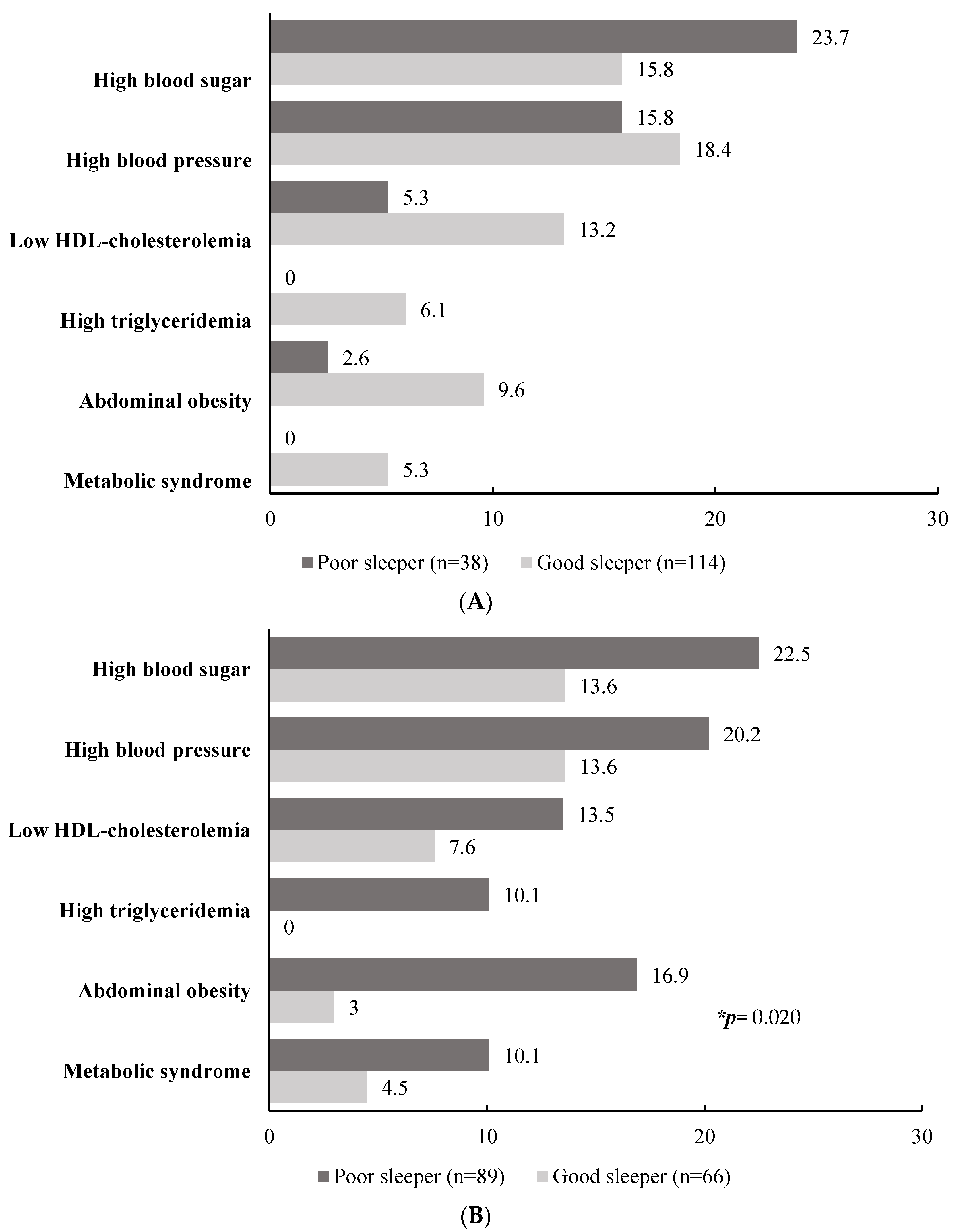
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Johnson, S.R. Premenstrual syndrome, premenstrual dysphoric disorder, and beyond: A clinical primer for practitioners. Obstet. Gynecol. 2004, 104, 845–859. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists. FAQs Premenstrual Syndrome (PMS). Available online: https://www.acog.org (accessed on 3 March 2023).
- Hardy, C.; Hunter, M.S. Premenstrual Symptoms and Work: Exploring Female Staff Experiences and Recommendations for Workplaces. Int. J. Environ. Res. Public Health 2021, 18, 3647. [Google Scholar] [CrossRef] [PubMed]
- Jehan, S.; Auguste, E.; Hussain, M.; Pandi-Perumal, S.R.; Brzezinski, A.; Gupta, R.; Attarian, H.; Jean-Louis, G.; McFarlane, S.I. Sleep and Premenstrual Syndrome. J. Sleep Med. Disord. 2016, 3, 1061. [Google Scholar]
- Conzatti, M.; Perez, A.V.; Maciel, R.F.; De Castro, D.H.; Sbaraini, M.; Wender, M.C.O. Sleep quality and excessive daytime sleepiness in women with Premenstrual Syndrome. Gynecol. Endocrinol. 2021, 37, 945–949. [Google Scholar] [CrossRef]
- Fernández, M.D.M.; Saulyte, J.; Inskip, H.M.; Takkouche, B. Premenstrual syndrome and alcohol consumption: A systematic review and meta-analysis. BMJ Open 2018, 8, e019490. [Google Scholar] [CrossRef] [PubMed]
- Isgin-Atici, K.; Kanbur, N.; Akgül, S.; Buyuktuncer, Z. Diet quality in adolescents with premenstrual syndrome: A cross-sectional study. Nutr. Diet. 2020, 77, 351–358. [Google Scholar] [CrossRef]
- Hashim, M.S.; Obaideen, A.A.; Jahrami, H.A.; Radwan, H.; Hamad, H.J.; Owais, A.A.; Alardah, L.G.; Qiblawi, S.; Al-Yateem, N.; Faris, M.A.E. Premenstrual syndrome is associated with dietary and lifestyle behaviors among university students: A cross-sectional study from Sharjah, UAE. Nutrients 2019, 11, 1939. [Google Scholar] [CrossRef] [PubMed]
- Farasati, N.; Siassi, F.; Koohdani, F.; Qorbani, M.; Abashzadeh, K.; Sotoudeh, G. Western dietary pattern is related to premenstrual syndrome: A case-control study. Br. J. Nutr. 2015, 114, 2016–2021. [Google Scholar] [CrossRef] [PubMed]
- Nagata, C.; Hirokawa, K.; Shimizu, N.; Shimizu, H. Soy, fat and other dietary factors in relation to premenstrual symptoms in Japanese women. BJOG 2004, 111, 594–599. [Google Scholar] [CrossRef]
- Wu, A.H.; Pike, M.C.; Stram, D.O. Meta-analysis: Dietary fat intake, serum estrogen levels, and the risk of breast cancer. J. Natl. Cancer Inst. 1999, 91, 529–534. [Google Scholar] [CrossRef]
- Fahed, G.; Aoun, L.; Zerdan, M.B.; Allam, S.; Zerdan, M.B.; Bouferraa, Y.; Assi, H.I. Metabolic Syndrome: Updates on Pathophysiology and Management in 2021. Int. J. Mol. Sci. 2022, 23, 786. [Google Scholar] [CrossRef]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 12. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, S.; Ramezan, I.; Tehrani, F.; Mohammadi, N.; Dovom, M.R.; Torkestani, F.; Simbar, M.; Azizi, F. Comparison of Metabolic and Hormonal Profiles of Women with and without Premenstrual Syndrome: A Community Based Cross-Sectional Study. Int. J. Endocrinol. Metab. 2016, 14, e28422. [Google Scholar] [CrossRef]
- Dang, N.; Khalil, D.; Sun, J.; Naveed, A.; Soumare, F.; Hamidovic, A. Waist Circumference and Its Association with Premenstrual Food Craving: The PHASE Longitudinal Study. Front. Psychiatry 2022, 13, 784316. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Li, P.H.; Barrow, T.M.; Colicino, E.; Li, C.; Song, R.; Liu, H.; Tang, N.J.; Liu, S.; Guo, L.; et al. Obesity as an effect modifier of the association between menstrual abnormalities and hypertension in young adult women: Results from Project ELEFANT. PLoS ONE 2018, 13, e0207929. [Google Scholar] [CrossRef] [PubMed]
- Moos, R.H. The Development of a Menstrual Distress Questionnaire. Psychosom. Med. 1968, 30, 853–867. [Google Scholar] [CrossRef]
- Kim, S.J.; Han, C.J. Effects of Isoflavone and Cynanchum wilfordii Supplementation on Premenstrual Syndrome, Dysmenorrhea—Focus on 20’s Women. East Asian Soc. Diet. Life 2015, 25, 64–72. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Radloff, L.S. The CES-D scale: A self report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.; Vagg, P.R.; Jacobs, G.A. Manual for the State-Trait Anxiety Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1993. [Google Scholar]
- Ministry of Health and Welfare; The Korean Nutrition Society. Dietary Reference Intakes for Koreans 2020; The Korean Nutrition Society: Seoul, Republic of Korea, 2020. [Google Scholar]
- Expert Panel on Detection, Evaluation. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001, 285, 2486. [Google Scholar] [CrossRef]
- Yoon, Y.S.; Oh, S.W. Optimal waist circumference cutoff values for the diagnosis of abdominal obesity in Korean adults. Endocrinol. Metab. 2014, 29, 418–426. [Google Scholar] [CrossRef]
- Meers, J.M.; Nowakowski, S. Sleep, premenstrual mood disorder, and women’s health. Curr. Opin. Psychol. 2020, 34, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Meers, J.M.; Bower, J.L.; Alfano, C.A. Poor sleep and emotion dysregulation mediate the association between depressive and premenstrual symptoms in young adult women. Arch. Womens Ment. Health 2020, 23, 351–359. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, P.J.; Martinez, P.E.; Nieman, L.K.; Koziol, D.E.; Thompson, K.D.; Schenkel, L.; Wakim, P.G.; Rubinow, D.R. Premenstrual Dysphoric Disorder Symptoms Following Ovarian Suppression: Triggered by Change in Ovarian Steroid Levels but Not Continuous Stable Levels. Am. J. Psychiatry 2017, 174, 980–989. [Google Scholar] [CrossRef]
- Yen, J.Y.; Liu, T.L.; Chen, I.J.; Chen, S.Y.; Ko, C.H. Premenstrual appetite and emotional responses to foods among women with premenstrual dysphoric disorder. Appetite 2018, 125, 18–23. [Google Scholar] [CrossRef]
- Doo, M.; Kim, Y. Association between sleep duration and obesity is modified by dietary macronutrients intake in Korean. Obes. Res. Clin. Pract. 2016, 10, 424–431. [Google Scholar] [CrossRef]
- Kim, Y.J.; Yeom, H.E. Interactive Impact of Sleep Duration and Sleep Quality on the Risk of Developing Metabolic Syndrome in Korean Adults. Healthcare 2020, 8, 186. [Google Scholar] [CrossRef] [PubMed]
- Lian, Y.; Yuan, Q.; Wang, G.; Tang, F. Association between sleep quality and metabolic syndrome: A systematic review and meta-analysis. Psychiatry Res. 2019, 274, 66–74. [Google Scholar] [CrossRef] [PubMed]
- Bertone-Johnson, E.R.; Whitcomb, B.W.; Rich-Edwards, J.W.; Hankinson, S.E.; Manson, J.E. Premenstrual Syndrome and Subsequent Risk of Hypertension in a Prospective Study. Am. J. Epidemiol. 2015, 182, 1000–1009. [Google Scholar] [CrossRef]
- Bertone-Johnson, E.R.; Houghton, S.C.; Whitcomb, B.W.; Sievert, L.L.; Zagarins, S.E.; Ronnenberg, A.G. Association of Premenstrual Syndrome with Blood Pressure in Young Adult Women. J. Womens Health 2016, 25, 1122–1128. [Google Scholar] [CrossRef]
- Geiker, N.R.W.; Astrup, A.; Hjorth, M.F.; Sjödin, A.; Pijls, L.; Markus, C.R. Does stress influence sleep patterns, food intake, weight gain, abdominal obesity and weight loss interventions and vice versa? Obes. Rev. 2018, 19, 81–97. [Google Scholar] [CrossRef] [PubMed]
- Sanlier, N.; Üstün, D. Egg consumption and health effects: A narrative review. J. Food Sci. 2021, 86, 4250–4261. [Google Scholar] [CrossRef]
- Marangoni, F.; Pellegrino, L.; Verduci, E.; Ghiselli, A.; Bernabei, R.; Calvani, R.; Cetin, I.; Giampietro, M.; Perticone, F.; Piretta, L.; et al. Cow’s Milk Consumption and Health: A Health Professional’s Guide. J. Am. Coll. Nutr. 2019, 38, 197–208. [Google Scholar] [CrossRef] [PubMed]
- Siminiuc, R.; Ţurcanu, D. Impact of nutritional diet therapy on premenstrual syndrome. Front. Nutr. 2023, 10, 1079417. [Google Scholar] [CrossRef] [PubMed]
| Did Not Experience (n = 152) | Experienced (n = 155) | p Value * | |
|---|---|---|---|
| Age, years | 39.84 ± 5.87 (22–54) | 39.31 ± 6.94 (21–53) | 0.468 |
| Educational level, ≥college | 90.1 | 85.8 | 0.294 |
| Occupation, housewife | 24.3 | 32.3 | 0.131 |
| Marriage status, yes | 80.9 | 80.6 | 0.533 |
| Current smoking, no | 94.1 | 91.9 | 0.505 |
| Alcohol drinking, no | 35.5 | 29.0 | 0.272 |
| Physical activity by IPAQ, low | 46.1 | 44.5 | 0.566 |
| Dietary supplementary intake, yes | 32.2 | 26.5 | 0.316 |
| Sleep quality by PSQI | 4.45 ± 2.78 | 6.24 ± 2.82 | <0.001 |
| Depression level | 28.54 ± 5.98 | 34.88 ± 8.40 | <0.001 |
| Anxiety level | 35.57 ± 7.99 | 41.70 ± 8.52 | <0.001 |
| Did Not Experience | Experienced | |||||
|---|---|---|---|---|---|---|
| Good Sleeper (n = 114) | Poor Sleeper (n = 38) | p Value * | Good Sleeper (n = 66) | Poor Sleeper (n = 89) | p Value * | |
| WC (cm) | 72.38 ± 8.33 | 70.66 ± 5.42 | 0.372 | 70.36 ± 10.59 | 74.10 ± 9.88 | 0.018 |
| SBP (mmHg) | 114.63 ± 14.42 | 114.84 ± 12.51 | 0.552 | 112.55 ± 12.62 | 115.16 ± 14.84 | 0.258 |
| DBP (mmHg) | 69.69 ± 10.62 | 71.63 ± 9.79 | 0.559 | 67.95 ± 9.12 | 71.99 ± 10.93 | 0.012 |
| FG (mg/dL) | 94.18 ± 19.36 | 95.92 ± 7.66 | 0.611 | 90.64 ± 8.93 | 92.93 ± 10.10 | 0.129 |
| TG (mg/dL) | 88.43 ± 60.43 | 74.92 ± 20.71 | 0.398 | 78.58 ± 29.23 | 90.51 ± 46.98 | 0.169 |
| HDL-C (mg/dL) | 68.21 ± 15.75 | 75.55 ± 15.65 | 0.090 | 70.51 ± 16.88 | 69.23 ± 18.48 | 0.891 |
| Did Not Experience | Experienced | |||||
|---|---|---|---|---|---|---|
| Good Sleeper (n = 114) | Poor Sleeper (n = 38) | p Value * | Good Sleeper (n = 66) | Poor Sleeper (n = 89) | p Value * | |
| Carbohydrate (g) | 120.67 ± 23.78 | 114.02 ± 28.18 | 0.131 | 119.98 ± 25.25 | 117.75 ± 29.58 | 0.789 |
| Fat (g) | 34.70 ± 9.30 | 35.91 ± 10.12 | 0.376 | 35.81 ± 9.28 | 34.69 ± 9.80 | 0.383 |
| Protein (g) | 43.94 ± 11.83 | 44.00 ± 11.16 | 0.881 | 42.72 ± 8.54 | 43.07 ± 10.28 | 0.795 |
| Calcium (mg) | 272.56 ± 112.60 | 249.30 ± 123.51 | 0.057 | 259.79 ± 108.71 | 260.22 ± 121.35 | 0.714 |
| Phosphorus(mg) | 651.50 ± 174.15 | 617.03 ± 160.97 | 0.209 | 631.15 ± 130.75 | 631.96 ± 160.83 | 0.755 |
| Iron (mg) | 8.53 ± 3.41 | 8.42 ± 4.19 | 0.721 | 7.82 ± 2.42 | 8.47 ± 3.71 | 0.117 |
| Vitamin A (μg RAE) | 253.63 ± 146.56 | 245.09 ± 126.84 | 0.458 | 256.44 ± 133.94 | 239.88 ± 139.44 | 0.714 |
| Thiamin (mg) | 1.18 ± 0.43 | 1.17 ± 0.45 | 0.863 | 1.17 ± 0.39 | 1.14 ± 0.45 | 0.431 |
| Niacin (mg) | 9.25 ± 4.76 | 8.77 ± 5.07 | 0.686 | 8.65 ± 3.28 | 8.20 ± 3.32 | 0.631 |
| Folate (μg) | 285.59 ± 122.31 | 303.21 ± 197.16 | 0.977 | 310.10 ± 149.60 | 278.98 ± 116.95 | 0.178 |
| Vitamin C (mg) | 63.85 ± 61.77 | 67.25 ± 84.43 | 0.989 | 64.51 ± 54.68 | 53.49 ± 45.96 | 0.322 |
| Did Not Experience | Experienced | |||||
|---|---|---|---|---|---|---|
| Good Sleeper (n = 114) | Poor Sleeper (n = 38) | p Value * | Good Sleeper (n = 66) | Poor Sleeper (n = 89) | p Value * | |
| Grains (g) | 110.76 ± 49.07 104.50 (84.12–130.50) | 97.37 ± 41.02 89.61 (70.23–128.69) | 0.133 | 122.04 ± 56.52 113.64 (84.90–145.52) | 108.33 ± 51.73 95.60 (76.89–129.91) | 0.076 |
| Sugar (g) | 5.32 ± 6.44 2.86 (1.19–7.02) | 4.11 ± 4.17 3.46 (0.77–6.21) | 0.152 | 4.00 ± 4.09 2.92 (0.90–5.69) | 4.77 ± 5.22 3.40 (1.46–6.30) | 0.214 |
| Soy and products (g) | 17.14 ± 33.25 4.61 (0.00–19.28) | 9.89 ± 22.82 3.18 (0.00–9.08) | 0.431 | 20.89 ± 37.89 4.98 (0.00–25.54) | 16.40 ± 35.31 2.59 (0.00–16.67) | 0.449 |
| Vegetables and mushrooms (g) | 159.47 ± 97.38 142.44 (100.43–201.37) | 158.24 ± 71.92 160.25 (98.17–212.14) | 0.494 | 166.12 ± 108.77 153.84 (106.64–210.84) | 156.24 ± 72.16 148.50 (102.01–206.58) | 0.505 |
| Fruits and products (g) | 110.30 ± 105.47 92.84 (16.47–161.43) | 122.83 ± 127.68 94.48 (4.44–203.33) | 0.757 | 109.81 ± 116.13 80.19 (0.00–188.10) | 110.70 ± 116.09 90.06 (0.00–163.82) | 0.724 |
| Meat (g) | 78.37 ± 52.70 73.26 (46.49–104.35) | 94.93 ± 63.99 85.70 (45.56–137.53) | 0.072 | 71.90 ± 39.30 72.37 (49.46–100.19) | 75.72 ± 44.99 74.30 (43.67–107.46) | 0.787 |
| Eggs (g) | 14.03 ± 21.84 0.00 (0.00–24.60) | 18.90 ± 22.36 10.41 (0.00–31.79) | 0.466 | 29.39 ± 39.12 0.00 (0.00–43.71) | 16.69 ± 28.14 0.00 (0.00–30.32) | 0.028 |
| Fish and shellfish (g) | 37.57 ± 50.43 9.06 (0.00–60.91) | 40.35 ± 56.33 10.01 (0.00–65.30) | 0.950 | 32.44 ± 38.92 14.54 (0.00–60.72) | 30.60 ± 40.41 9.18 (0.00–51.81) | 0.773 |
| Milk and dairy products(g) | 57.56 ± 75.98 0.00 (0.00–112.19) | 28.84 ± 48.27 0.00 (0.00–53.97) | 0.020 | 43.16 ± 73.77 0.00 (0.00–80.21) | 54.73 ± 91.18 0.00 (0.00–94.59) | 0.345 |
| Oil (g) | 4.61 ± 3.33 4.07 (2.10–6.18) | 4.11 ± 3.10 3.58 (1.98–5.81) | 0.183 | 4.63 ± 3.58 3.98 (1.97–5.83) | 4.05 ± 3.13 3.56 (1.46–6.21) | 0.403 |
| Seasoning (g) | 15.26 ± 9.02 15.06 (7.89–20.07) | 15.40 ± 7.77 15.11 (9.07–20.13) | 0.817 | 13.99 ± 9.35 11.40 (7.74–19.99) | 14.57 ± 8.91 13.58 (8.68–17.76) | 0.663 |
| Alcoholic drinks (g) | 40.91 ± 91.66 1.34 (0.00–37.40) | 40.51 ± 110.34 0.15 (0.00–41.52) | 0.914 | 24.90 ± 42.00 0.00 (0.00–34.88) | 70.19 ± 113.87 25.75 (0.00–106.55) | 0.006 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chun, H.; Doo, M. Sleep Quality in Women with Premenstrual Syndrome Is Associated with Metabolic Syndrome-Related Variables. Healthcare 2023, 11, 1492. https://doi.org/10.3390/healthcare11101492
Chun H, Doo M. Sleep Quality in Women with Premenstrual Syndrome Is Associated with Metabolic Syndrome-Related Variables. Healthcare. 2023; 11(10):1492. https://doi.org/10.3390/healthcare11101492
Chicago/Turabian StyleChun, Hyejin, and Miae Doo. 2023. "Sleep Quality in Women with Premenstrual Syndrome Is Associated with Metabolic Syndrome-Related Variables" Healthcare 11, no. 10: 1492. https://doi.org/10.3390/healthcare11101492
APA StyleChun, H., & Doo, M. (2023). Sleep Quality in Women with Premenstrual Syndrome Is Associated with Metabolic Syndrome-Related Variables. Healthcare, 11(10), 1492. https://doi.org/10.3390/healthcare11101492






