What Are The Core Symptoms of Antenatal Depression? A Study Using Patient Health Questionnaire-9 among Japanese Pregnant Women in the First Trimester
Abstract
1. Introduction
2. Methods
2.1. Study Procedures and Participants
2.2. Measurements
2.3. Data Analysis
2.4. Ethical Consideration
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yin, X.; Sun, N.; Jiang, N.; Xu, X.; Gan, Y.; Zhang, J.; Qiu, L.; Yang, C.; Shi, X.; Chang, J.; et al. Prevalence and associated factors of antenatal depression: Symptomatic reviews and meta-analyses. Clin. Psychol. Rev. 2021, 83, 101932. [Google Scholar] [CrossRef] [PubMed]
- Feighner, J.P.; Robins, E.; Guze, S.; Woodruff, R.A.; Winokur, G.; Minoz, R. Diagnostic criteria for use in psychiatric research. Arch. Gen. Psychiatry 1972, 26, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Endicott, J.; Robins, E. Research Diagnostic Criteria (RDC) for a Selected Group of Functional Disorders, 3rd ed.; New York State Psychiatric Institute: New York, NY, USA, 1978. [Google Scholar]
- Endicott, J. Measurement of depression in patients with cancer. Cancer 1984, 53, 2243–2248. [Google Scholar] [CrossRef] [PubMed]
- Akechi, T.; Ietsugu, T.; Sukigara, M.; Okamura, H.; Nakano, T.; Akizuki, N.; Okamura, M.; Shimizu, K.; Okuyama, T.; Furukawa, T.A.; et al. Symptoms indicator of severity of depression in cancer patients: A comparison of the DSM-IV criteria with alternative diagnostic criteria. Gen. Hosp. Psychiatry 2009, 31, 225–232. [Google Scholar] [CrossRef] [PubMed]
- von Ammon Cavanaugh, S. Depression in the medically ill: Critical issues in diagnostic assessment. Psychosomatics 1983, 36, 48–59. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Beck, A.; Ward, C.; Mendelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef]
- Einarson, T.R.; Piwko, C.; Koren, G. Quantifying the global rates of nausea and vomiting of pregnancy: A meta-analysis. J. Popul. Ther. Clin. Pharmacol. 2013, 20, e171–e183. [Google Scholar]
- Matthey, S.; Ross-Hamid, C. The validity of DSM symptoms for depression and anxiety disorders during pregnancy. J. Affect. Disord. 2011, 133, 546–552. [Google Scholar] [CrossRef]
- Aksoy, H.; Aksoy, U.; Karadağ, Ō.I.; Hacimusalar, Y.; Açmaz, G.; Aykut, G.; Çağli, F.; Yücel, B.; Aydin, T.; Babayiğit, A. Depression levels in patients with hyperemesis gravidarum: A prospective case-control study. SpringerPlus 2015, 4, 34. [Google Scholar] [CrossRef]
- Fell, D.B.; Dodds, L.; Joseph, K.S.; Allen, V.M.; Butler, B. Risk factors for hyperemesis gravidarum requiring hospital admission during pregnancy. Obstet. Gynecol. 2006, 107, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Kjeldgaard, H.K.; Eberhard-Gran, M.; Benth, J.Š.; Nordeng, H.; Vikanes, V.Å. History of depression and risk of hyperemesis gravidarum: A population-based cohort study. Arch. Women’s Ment. Health 2017, 20, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Kjeldgaard, H.K.; Vikanes, Å.; Benth, J.Š.; Junge, C.; Garthus-Niegel, S.; Eberhard-Gran, M. The association between the degree of nausea in pregnancy and subsequent posttraumatic stress. Arch. Women’s Ment. Health 2019, 22, 493–501. [Google Scholar] [CrossRef] [PubMed]
- Meltzer-Brody, S.; Maegbaek, M.L.; Medland, S.E.; Miller, W.C.; Sullivan, P.; Munk-Olsen, T. Obstetrical, pregnancy and socio-economic predictors for new-onset severe postpartum psychiatric disorders in primiparous women. Psychol. Med. 2017, 47, 1427–1441. [Google Scholar] [CrossRef] [PubMed]
- Pirimoglu, Z.M.; Guzelmeric, K.; Alpay, B.; Balcik, O.; Unal, O.; Turan, M.C. Psychological factors of hyperemesis gravidarum by using the SCL-90-R questionnaire. Clin. Exp. Obstet. Gynecol. 2009, 37, 56–59. [Google Scholar]
- Seng, J.S.; Schrot, J.A.; van de Ven, C.; Liberzon, I. Service use data analysis or pre-pregnancy psychiatric and somatic diagnosis in women with hyperemesis gravidarum. J. Psychosom. Obstet. Gynaecol. 2007, 28, 209–217. [Google Scholar] [CrossRef]
- Hizli, D.; Kamalak, Z.; Kosus, A.; Kosus, N.; Akkurt, G. Hyperemesis gravidarum and depression in pregnancy: Is there an association? J. Psychosom. Obstet. Gynaecol. 2012, 33, 171–175. [Google Scholar] [CrossRef]
- Kitamura, T.; Shima, S.; Sugawara, M.; Toda, M. Psychological and social correlates of the onset of affective disorders among pregnant women. Psychol. Med. 1993, 23, 967–975. [Google Scholar] [CrossRef]
- McCormack, D.; Scott-Heyes, G.; McCusker, C.G. The impact of hyperemesis gravidarum on maternal mental health and maternal-fetal attachment. J. Psychosom. Obstet. Gynaecol. 2011, 32, 79–87. [Google Scholar] [CrossRef]
- Mitchell-Jones, N.; Gallos, I.; Farren, J.; Tobias, A.; Bottomley, C.; Bourne, T. Psychological morbidity associated with hyperemesis gravidarum: A systematic review and meta-analysis. BJOG Int. J. Obstet. Gynaecol. 2016, 124, 20–30. [Google Scholar] [CrossRef]
- Kaufman, L.; Rousseeuw, P. Finding Groups in Data: An Introduction to Cluster Analysis; Wiley: New York, NY, USA, 1990. [Google Scholar]
- Lord, F.M. Applications of Item Response Theory to Practical Testing Problems; Routledge: Abingdon, UK, 1980. [Google Scholar]
- Nugent, W.R. Understanding DIF and DTF: Description, methods, and implications for social work research. J. Soc. Soc. Work Res. 2017, 8, 305–334. [Google Scholar] [CrossRef]
- Samejima, F. Estimation of reliability coefficients using the test information function and its modifications. Appl. Psychol. Meas. 1994, 18, 229–244. [Google Scholar] [CrossRef]
- Wakamatsu, M.; Minatani, M.; Hada, A.; Kitamura, T. The Patient Health Questionnaire-9 among first-trimester pregnant women in Japan: Factor structure and measurement and structural invariance between nulliparas and multiparas and across perinatal measurement time points. Open J. Depress. 2021, 10, 121–137. [Google Scholar] [CrossRef]
- Hada, A.; Minatani, M.; Wakamatsu, M.; Koren, G.; Kitamura, T. The pregnancy-unique quantification of emesis and nausea (PUQE-24): Configural, measurement, and structural invariance between nulliparas and multiparas and across two measurement time points. Healthcare 2021, 9, 1553. [Google Scholar] [CrossRef] [PubMed]
- Hada, A.; Minatani, M.; Wakamatsu, M.; Kitamura, T. Disability during early pregnancy: Using the Sheehan Disability Scale during the first trimester in Japan. Healthcare 2022, 10, 2514. [Google Scholar] [CrossRef] [PubMed]
- Yamada, F.; Kataoka, Y.; Minatani, M.; Hada, A.; Wakamatsu, M.; Kitamura, T. The NVP QOL Questionnaire: Psychometric properties of the self-report measure of health-related quality of life for nausea and vomiting during pregnancy. PCN Rep. 2022, 1, e21. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kronke, K.; Williams, J.B.W. Patient Health Questionnaire Study Group Validity and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA 1999, 282, 1737–1744. [Google Scholar] [CrossRef]
- Inagaki, M.; Ohtsuki, T.; Yonemoto, N.; Kawashima, Y.; Saitoh, A.; Oikawa, Y.; Kurosawa, M.; Muramatsu, K.; Furukawa, T.A.; Yamada, M. Validity of the Patient Health Questionnaire (PHQ)-9 and PHQ-2 in general internal medicine primary care at a Japanese rural hospital: A cross-sectional study. Gen. Hosp. Psychiatry 2013, 35, 592–597. [Google Scholar] [CrossRef]
- Muramatsu, K.; Kamijima, K. Puraimarikea shinnryou to utubyou sukuri-ningu tsuru: Patient Health Questionnaire-9 nihongoban ‘Kokoroto Karadano Shitsumonhyou’ (Primary care and depression screening tool: The Japanese version of the Patient health Questionnaire-9 ‘Questionnaire of Mind and Body’). Shindan Chiryou 2009, 97, 1465–1473. (In Japanese) [Google Scholar]
- Ebrahimi, N.; Maltepe, C.; Garcia-Bournissen, F.; Koren, G. Nausea and vomiting of pregnancy: Using the 24-hour pregnancy-unique quantification of emesis (PUQE-24) scale. JOGC 2009, 31, 803–807. [Google Scholar] [CrossRef]
- Magee, L.A.; Chandra, K.; Mazzotta, P.; Stewart, D.; Koren, G.; Guyatt, G.H. Development of a health-related quality of the instrument for nausea and vomiting of pregnancy. Am. J. Obstet. Gynecol. 2002, 186, S232–S238. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, D.V. The Anxiety Disease; Scribner: New York, NY, USA, 1983. [Google Scholar]
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307. [Google Scholar] [CrossRef] [PubMed]
- Morin, C.M.; Belleville, G.; Bélanger, L.; Ivers, H. The Insomnia Severity Index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 2011, 34, 601–608. [Google Scholar] [CrossRef] [PubMed]
- Shinohara, E.; Minatani, M.; Wakamatsu, M.; Hada, A.; Kitamura, T. The Insomnia Severity Index: Factor structure and measurement and structural invariance across perinatal measurement time points (manuscript preparation). Healthcare 2023, 11, 1194. [Google Scholar] [CrossRef]
- Zwaig, M.H.; Campbell, G. Receiver-operating characteristic (ROC) plots: A fundamental evaluation tool in clinical medicine. Clin. Chem. 1993, 39, 561–577. [Google Scholar] [CrossRef]
- Samejima, F. Estimation of latent ability using a response pattern of graded scores 1. ETS Res. Bull. Ser. 1968, i-169. [Google Scholar] [CrossRef]
- Samejima, F. Estimation of latent ability using a response pattern of graded scores. Psychom. Monogr. Suppl. 1969, 34 Pt 2, 100. [Google Scholar] [CrossRef]
- Reeve, B.B.; Hays, R.D.; Bjorner, J.B.; Cook, K.F.; Crane, P.K.; Teresi, J.A.; Thissen, D.; Revicki, D.A.; Weiss, D.J.; Hambleton, R.K.; et al. Psychometric evaluation and calibration of health-related quality of life item banks: Plans for the Patient-Reported Outcomes Measurement Information System (PROMIS). Med. Care 2007, 45 (Suppl. S1), S22–S31. [Google Scholar] [CrossRef]
- The Patient-Reported Outcome Measurement Information System; PROMIS® Instrument Development and Validation Scientific Standards Version 2.0, (Revised May 2013). 2013. Available online: https://www.mcgill.ca/can-pro-network/files/can-pro-network/promisstandards_vers2.0_final.pdf (accessed on 18 May 2023).
- Rimehaug, S.A.; Kaat, A.J.; Nordvik, J.E.; Klokkerud, M.; Robinson, H.S. Psychometric properties of the PROMIS-57 questionnaire, Norwegian version. Qual. Life Res. 2022, 31, 269–280. [Google Scholar] [CrossRef]
- Mokken, R.A. Theory and Procedure of Scale Analysis: With Applications in Political Research; De Gruyter Mouton: Berlin, Germany; New York, NY, USA, 2011. [Google Scholar] [CrossRef]
- Revelle, W. Psych: Procedures for Psychological, Psychometric, and Personality Research, R package version 2.2.9; Northwestern University: Evanston, IL, USA, 2022. [Google Scholar]
- Rosseel, Y. Lavaan: An R package for structural equation modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef]
- Van der Ark, L.A. Mokken scale analysis in R. J. Stat. Softw. 2007, 20, 1–19. [Google Scholar] [CrossRef]
- Rizopoulos, D. ltm: An R package for latent variable modelling and item response theory analyses. J. Stat. Softw. 2006, 17, 1–25. [Google Scholar] [CrossRef]
- Leu, S.H.; Chou, J.Y.; Lee, P.C.; Cheng, H.C.; Shao, W.C.; Hsien, W.L.; Huang, C.L.; Chen, V.C.H. Validity and reliability of the Chinese version of the Sheehan Disability Scale (SDS-C). Asia-Pac. Psychiatry 2015, 7, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Luciano, J.V.; Bertsch, J.; Salvador-Carulla, L.; Tomás, J.M.; Fernández, A.; Pinto-Meza, A.; Haro, J.M.; Palao, D.J.; Serrano-Blanco, A. Factor structure, internal consistency, and construct validity of the Sheehan Disability Scale in a Spanish primary care sample. J. Eval. Clin. Pract. 2010, 16, 895–901. [Google Scholar] [CrossRef] [PubMed]
- Koot, M.H.; Boelig, R.C.; van’t Hooft, J.; Limpens, J.; Rosebom, T.J.; Painter, R.C.; Grooten, I.J. Variation in hyperemesis gravidarum definition and outcome reporting in randomised clinical trials: A systematic review. BJOG 2018, 125, 1514–1521. [Google Scholar] [CrossRef] [PubMed]
- Huey, N.S.; Guan, N.C.; Gill, J.S.; Hui, K.O.; Sulaiman, A.H.; Kangasundram, S. Core symptoms of major depressive disorder among palliative care patients. Int. J. Environ. 2018, 15, 1758. [Google Scholar] [CrossRef] [PubMed]
- Kitamura, T.; Shima, S.; Sugawara, M.; Toda, M.A. Clinical and psychosocial correlates of antenatal depression: A review. Psychother. Psychosom. 1996, 65, 117–123. [Google Scholar] [CrossRef]
- Salomonsson, B. Psychodynamic Interventions in Pregnancy and Infancy: Clinical and Theoretical Perspectives; Routledge: Abingdon, UK, 2018. [Google Scholar]
- Evans, K.; Spildy, H.; Morrell, J.C. Non-pharmacological interventions to reduce the symptoms of mild to moderate anxiety in pregnant women: A systematic review and narrative synthesis of women’s views on the acceptability of and satisfaction with interventions. Arch. Women’s Ment. Health 2020, 23, 11–28. [Google Scholar] [CrossRef] [PubMed]
- Angst, J.; Dobler-Mikola, A. Do the diagnostic criteria determine the sex ratio in depression? J. Affect. 1984, 7, 189–198. [Google Scholar] [CrossRef]
- Angst, J.; Dobler-Mikola, A. The Zurich study III. Diagnosis of depression. Eur. Arch. Psychiatry Neurol. Sci. 1984, 234, 30–37. [Google Scholar] [CrossRef]
| Subscales | Mean | SD | Skewness | Kurtosis |
|---|---|---|---|---|
| Somatic | 7.63 | 2.55 | 0.80 | −0.99 |
| Non-somatic | 8.79 | 3.18 | 1.40 | 1.60 |
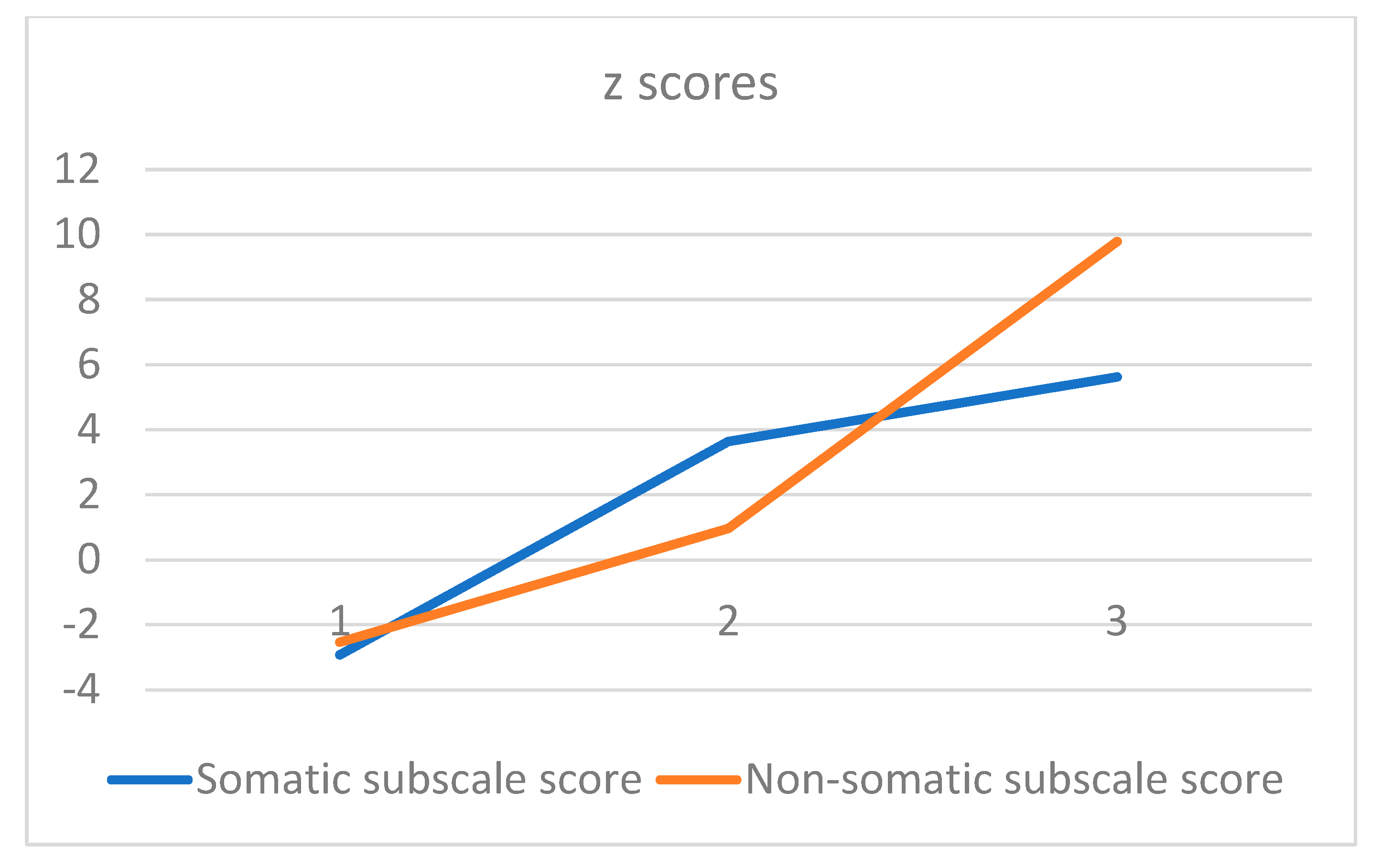
| Cluster | Cluster 1 (n = 135) | Cluster 2 (n = 144) | Cluster 3 (n = 98) | F | Post Hoc Comparison |
|---|---|---|---|---|---|
| Somatic subscale (z score) | −2.92 | 3.64 | 5.63 | 382.9 *** | 1 < 2 < 3 |
| Non-somatic subscale (z score) | −2.53 | 0.96 | 9.79 | 458.3 *** | 1 < 2 < 3 |
| MDE, n (%) | 0 (0.0) | 1 (0.7) | 45 (45.9) | 140.6 *** | – |
| PUQE-24 (z score) | 2.51 | 4.13 | 5.23 | 30.8 *** | 1 < 2 < 3 |
| NVP-QOL (z score) | 73.59 | 105.10 | 137.76 | 88.8 *** | 1 < 2 < 3 |
| Nausea therapy (z score) | −0.20 | −0.16 | 0.03 | 1.7 NS | – |
| SDS (z score) | 1.99 | 6.90 | 12.98 | 88.1 *** | 1 < 2 < 3 |
| ISI severity (z score) | 3.02 | 6.53 | 8.46 | 63.5 *** | 1 < 2 < 3 |
| ISI impact (z score) | 1.19 | 3.95 | 4.68 | 38.0 *** | 1 < 2 < 3 |
| Own age | 25.48 | 24.75 | 25.84 | 0.8 NS | |
| Partner’s age | 27.33 | 28.88 | 28.17 | 3.7 * | 1, 3 < 2 |
| Nulliparae, n (%) | 59 (44.0) | 66 (46.5) | 41 (41.8) | χ2 = 0.52 NS | – |
| Multiparae, n (%) | 75 (56.0) | 76 (53.5) | 57 (58.2) | – |
| No. | Item | Clusters 1 + 2 | Cluster 3 | AUC |
|---|---|---|---|---|
| 1 | Loss of interest | 1.42 (0.58) | 2.84 (0.92) | 0.883 |
| 2 | Depressed mood | 1.31 (0.49) | 2.47 (0.88) | 0.858 |
| 3 | Sleep | 2.24 (1.06) | 3.16 (0.89) | 0.735 |
| 4 | Fatigue | 2.25 (0.86) | 3.32 (0.73) | 0.810 |
| 5 | Appetite | 2.36 (1.00) | 3.34 (0.81) | 0.761 |
| 6 | Self-esteem | 1.16 (0.41) | 2.39 (0.95) | 0.858 |
| 7 | Poor concentration | 1.23 (0.49) | 2.64 (0.88) | 0.896 |
| 8 | Psychomotor | 1.10 (0.35) | 1.78 (0.96) | 0.701 |
| 9 | Suicidality | 1.01 (0.09) | 1.12 (0.36) | 0.553 |
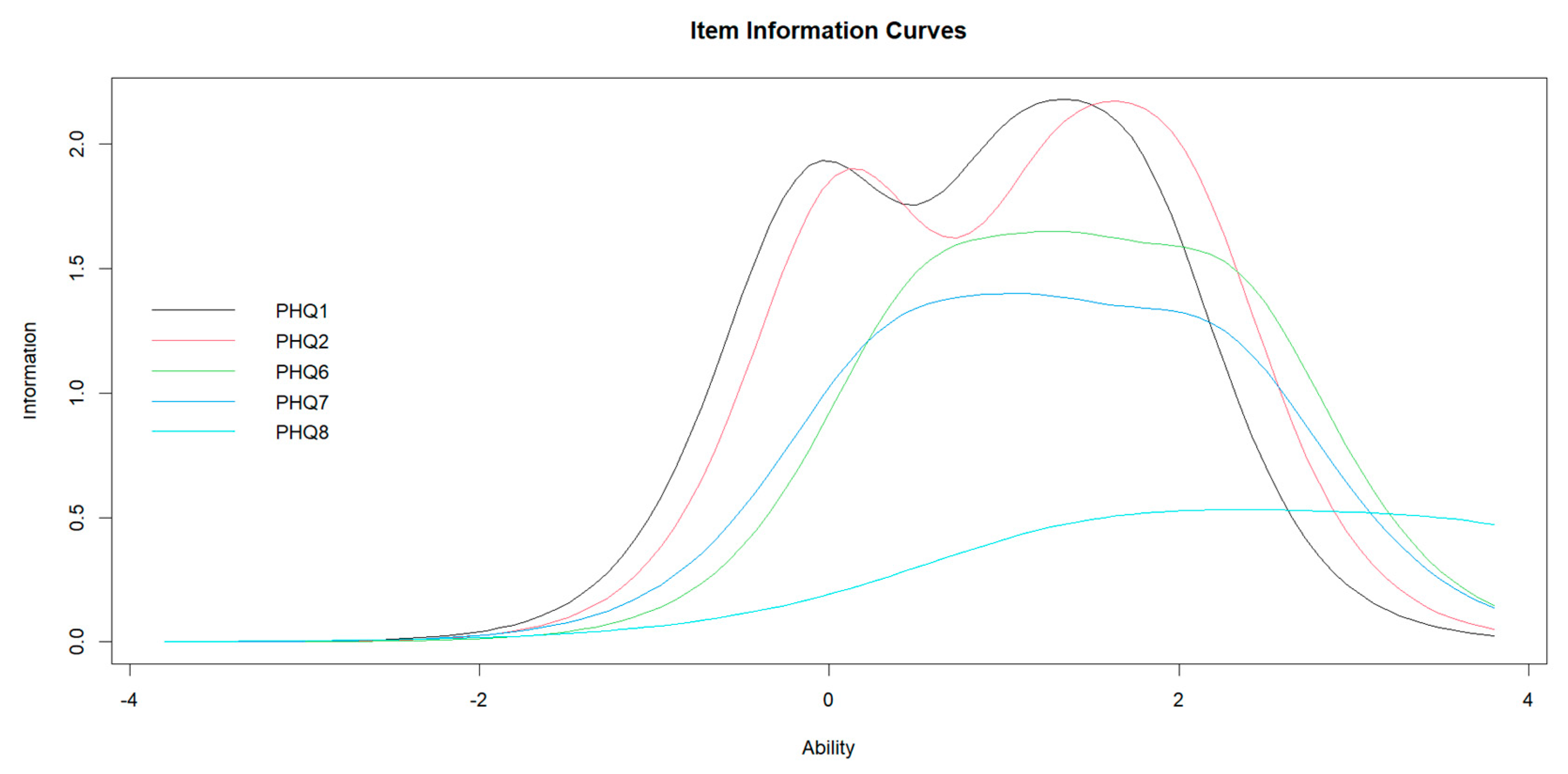
| PHQ-9 | b1 | b2 | b3 | a | Information | |
|---|---|---|---|---|---|---|
| 1 | Loss of interest | −0.093 | 1.060 | 1.711 | 2.722 | 6.34 |
| 2 | Depressed mood | 0.085 | 1.345 | 1.974 | 2.714 | 6.37 |
| 6 | Self-esteem | 0.572 | 1.387 | 2.285 | 2.365 | 5.18 |
| 7 | Poor concentration | 0.379 | 1.215 | 2.200 | 2.171 | 4.70 |
| 8 | Psychomotor | 1.468 | 2.436 | 3.724 | 1.315 | 2.52 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kitamura, T.; Usui, Y.; Wakamatsu, M.; Minatani, M.; Hada, A. What Are The Core Symptoms of Antenatal Depression? A Study Using Patient Health Questionnaire-9 among Japanese Pregnant Women in the First Trimester. Healthcare 2023, 11, 1494. https://doi.org/10.3390/healthcare11101494
Kitamura T, Usui Y, Wakamatsu M, Minatani M, Hada A. What Are The Core Symptoms of Antenatal Depression? A Study Using Patient Health Questionnaire-9 among Japanese Pregnant Women in the First Trimester. Healthcare. 2023; 11(10):1494. https://doi.org/10.3390/healthcare11101494
Chicago/Turabian StyleKitamura, Toshinori, Yuriko Usui, Mikiyo Wakamatsu, Mariko Minatani, and Ayako Hada. 2023. "What Are The Core Symptoms of Antenatal Depression? A Study Using Patient Health Questionnaire-9 among Japanese Pregnant Women in the First Trimester" Healthcare 11, no. 10: 1494. https://doi.org/10.3390/healthcare11101494
APA StyleKitamura, T., Usui, Y., Wakamatsu, M., Minatani, M., & Hada, A. (2023). What Are The Core Symptoms of Antenatal Depression? A Study Using Patient Health Questionnaire-9 among Japanese Pregnant Women in the First Trimester. Healthcare, 11(10), 1494. https://doi.org/10.3390/healthcare11101494







