Neuroticism and Psychological Stress in Patients Suffering Oral Lichen Planus: Research Evidence of Psycho-Stomatology?
Abstract
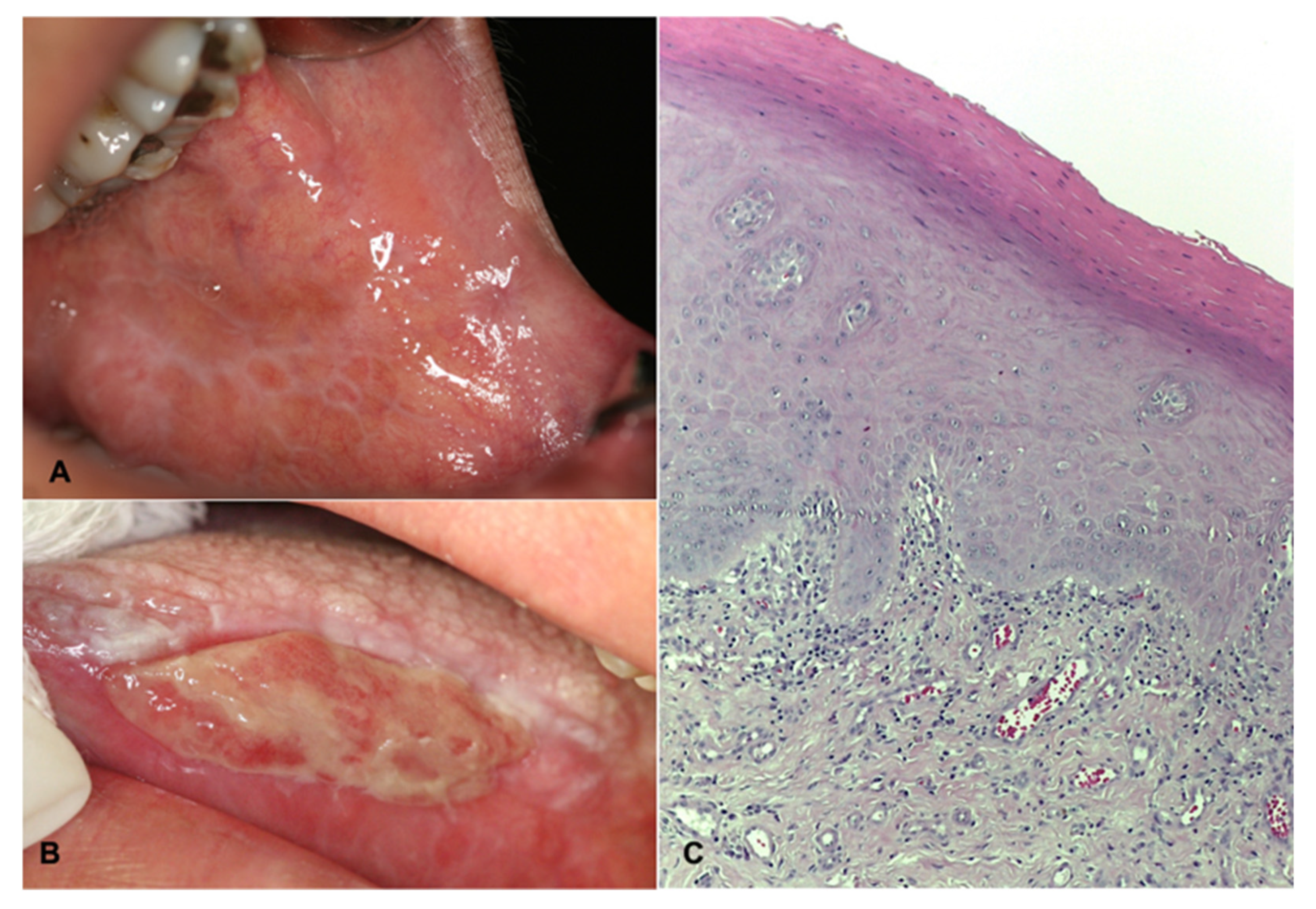
1. Introduction
2. Materials and Methods
3. Results
3.1. Psychosocial Variables
3.2. Oral Health-Related Quality of Life
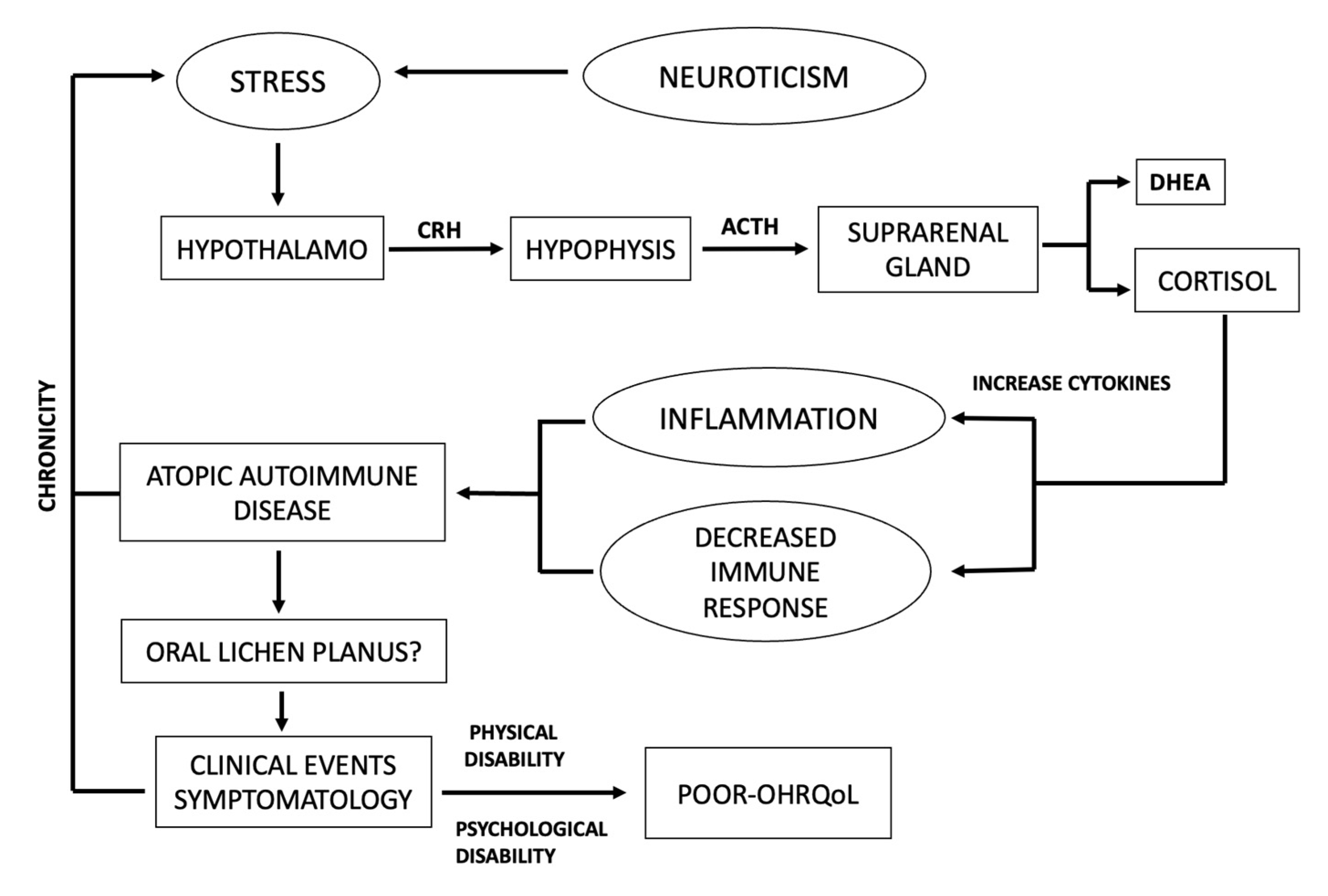
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- AL-Omiri, M.K.; Karasneh, J.; Lynch, E. Psychological profiles in patients with recurrent aphthous ulcers. Int. J. Oral Maxillofac. Surg. 2012, 41, 384–388. [Google Scholar] [CrossRef]
- Ivanovsky, K.; Nakova, M.; Warbourton, G.; Pesevska, S.; Filipovska, A.; Nares, S.; Nunn, M.E.; Angelova, D.; Angelov, N. Psychological profile in oral lichen planus. J. Clin. Periodontol. 2005, 32, 1034–1040. [Google Scholar] [CrossRef]
- Tokura, T.; Kimura, H.; Ito, M.; Nagashima, W.; Sato, N.; Kimura, Y.; Arao, M.; Aleksic, B.; Yoshida, K.; Kurita, K.; et al. Temperament and character profiles of patients with burning mouth syndrome. J. Psychosom. Res. 2015, 78, 495–498. [Google Scholar] [CrossRef]
- Reyes Zamorano, E.R.; Álvarez Carillo, C.; Peredo Silva, A.; Miranda Sandoval, A.M.; Rebolledo Pastrana, I.M. Psychometric properties of the big five inventory in a Mexican sample. Salud Ment. 2014, 37, 491–497. [Google Scholar] [CrossRef]
- McCrae, R.R.; Costa, P.T. Personality in Adulthood: A Five-Factor Theory Perspective, 2nd ed.; Guilford Press: New York, NY, USA, 2003. [Google Scholar]
- Schneiderman, N.; Ironson, G.; Siegel, S.D. Stress and health: Psychological, behavioral, and biological determinants. Annu. Rev. Clin. Psychol. 2005, 1, 607–628. [Google Scholar] [CrossRef]
- Selye, H. The general adaptation syndrome and the diseases of adaptation. J. Clin. Endocrinol. Metab. 1946, 6, 117–230. [Google Scholar] [CrossRef]
- Baiju, R.; Peter, E.; Varghese, N.; Sivaram, R. Oral health and quality of life: Current concepts. J. Clin. Diagn. Res. 2017, 11, ZE21–ZE26. [Google Scholar] [CrossRef]
- Mohamadi Hasel, K.; Besharat, M.A.; Abdolhoseini, A.; Alaei Nasab, S.; Niknam, S. Relationships of personality factors to perceived stress, depression, and oral lichen planus severity. Int. J. Behav. Med. 2013, 20, 286–292. [Google Scholar] [CrossRef]
- Dvorak, G.; Rappersberger, K.; Rausch-Fan, X.; Bruckmann, C.; Hofmann, E. Effect of personality traits on the oral health-related quality of life in patients with oral lichen planus undergoing treatment. Clin. Oral Investig. 2021, 25, 2381–2389. [Google Scholar] [CrossRef]
- Alrashdan, M.S.; Cirillo, N.; McCullough, M. Oral lichen planus: A literature review and update. Arch. Dematol. Res. 2016, 308, 539–551. [Google Scholar] [CrossRef]
- Olson, M.A.; Rogers, R.S., III; Bruce, A.J. Oral lichen planus. Clin. Dermatol. 2016, 34, 495–504. [Google Scholar] [CrossRef]
- Kumari, P.; Debta, P.; Dixit, A. Oral potentially malignant disorders: Etiology, pathogenesis, and transformation into oral cancer. Front. Pharmacol. 2022, 13, 825266. [Google Scholar] [CrossRef]
- Chiang, C.P.; Chang JY, F.; Wang, Y.P.; Wu, Y.H.; Lu, S.Y.; Sun, A. Oral lichen planus-differential diagnoses, serum autoantibodies, hematinic deficiencies, and management. J. Formos. Med. Assoc. 2018, 117, 756–765. [Google Scholar] [CrossRef]
- Gonzalez-Moles, M.; Gil-Montoya, J.; Gonzalez-Ruiz, L.; Ramos, P.; Bravo, M. Outcomes of oral lichen planus and oral lichenoid lesions treated with topical corticosteroid. Oral Dis. 2017, 4, 573–579. [Google Scholar] [CrossRef] [PubMed]
- Adamo, D.; Calabria, E.; Canfora, F.; Coppola, N.; Leuci, S.; Mignogna, M.; Muzio, L.L.; Spirito, F.; Giuliani, M.; Azzi, L.; et al. Anxiety and depression in keratotic oral lichen planus: A multicentric study from the SIPMO. Clin. Oral Investig. 2023. [Google Scholar] [CrossRef]
- González-Moles, M.A.; Ruiz-Ávila, I.; González-Ruiz, L.; Ayén, A.; Gil-Montoya, J.A.; Ramos-García, P. Malignant transformation risk of oral lichen planus: A systematic review and comprehensive meta-analysis. Oral Oncol. 2019, 96, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Moosavi, M.S.; Tavakol, F. Literature review of cancer stem cells in oral lichen planus: A premalignant lesion. Stem Cell Investig. 2021, 8, 25. [Google Scholar] [CrossRef]
- Holmes, T.H.; Rahe, R.H. The Social Readjustment Rating Scale. J. Psychosom. Res. 1967, 11, 213–218. [Google Scholar] [CrossRef]
- Benet-Martínez, V.; John, O.P. Los cinco grandes across cultures and ethnic groups: Multitrait multimethod analyses of the Big Five in Spanish and english. J. Pers. Soc. Psychol. 1998, 75, 729–750. [Google Scholar] [CrossRef] [PubMed]
- Castrejon-Perez, R.C.; Borges-Yanez, S.A.; Irigoyen-Camacho, M.E. Validation of an instrument for measuring the effects of oral health on the quality of life of older adults in Mexico. Rev. Panam. Salud Publica 2010, 27, 321–329. [Google Scholar] [CrossRef] [PubMed]
- De Porras-Carrique, T.; González-Moles, M.Á.; Warnakulasuriya, S.; Ramos-García, P. Depression, anxiety, and stress in oral lichen planus: A systematic review and meta-analysis. Clin. Oral Investig. 2022, 26, 1391–1408. [Google Scholar] [CrossRef]
- Cankovic, M.; Bokor-Bratić, M.; Novović, Z. Stressful Life Events and Personality Traits in Patients with Oral Lichen Planus. Acta Dermatovenerol. Croat. 2015, 23, 270–276. [Google Scholar]
- Yang, C.; Liu, L.; Shi, H.; Zhang, Y. Psychological problems and quality of life of patients with oral mucosal diseases: A preliminary study in Chinese population. BMC Oral Health 2018, 18, 226. [Google Scholar] [CrossRef]
- Vilar-Villanueva, M.; Gándara-Vila, P.; Blanco-Aguilera, E.; Otero-Rey, E.M.; Rodríguez-Lado, L.; García-García, A.; Blanco-Carrión, A. Psychological disorders and quality of life in oral lichen planus patients and a control group. Oral Dis. 2019, 25, 1645–1651. [Google Scholar] [CrossRef] [PubMed]
- Adamo, D.; Pecoraro, G.; Fortuna, G.; Amato, M.; Marenzi, G.; Aria, M.; Mignogna, M.D. Assessment of oral health-related quality of life, measured by OHIP-14 and GOHAI, and psychological profiling in burning mouth syndrome: A case-control clinical study. J. Oral Rehabil. 2019, 47, 42–52. [Google Scholar] [CrossRef] [PubMed]
- López-Jornet, P.; Camacho-Alonso, F. Quality of life in patients with oral lichen planus. J. Eval. Clin. Pract. 2010, 16, 111–113. [Google Scholar] [CrossRef] [PubMed]
- Tabolli, S.; Bergamo, F.; Alessandroni, L.; Di Pietro, C.; Sampogna, F.; Abeni, D. Quality of life and psychological problems of patients with oral mucosal disease in dermatological practice. Dermatology 2009, 218, 314–320. [Google Scholar] [CrossRef]
- Butcher, S.K.; Lord, J.M. Stress responses and innate immunity: Aging as a contributory factor. Aging Cell 2004, 3, 151–160. [Google Scholar] [CrossRef]
- Cohen, S.; Hamrick, N. Stable individual differences in physiological response to stressors: Implications for stress-elicited changes in immune related health. Brain Behav. Immun. 2003, 17, 407–414. [Google Scholar] [CrossRef]
- Padgett, D.; Glaser, R. How stress influences immune response. Trends Immunol. 2003, 24, 444–448. [Google Scholar] [CrossRef]
- Stojanovich, L. Stress and autoimmunity. Autoimmun. Rev. 2010, 9, A271–A276. [Google Scholar] [CrossRef] [PubMed]
- Straub, R.H.; Cutolo, M. Psychoneuroimmunology-developments in stress research. Wien. Med. Wochenschr. 2018, 168, 76–84. [Google Scholar] [CrossRef]
- Hasselmann, H.; Gamradt, S.; Taenzer, A.; Nowacki, J.; Zain, R.; Patas, K.; Ramien, C.; Paul, F.; Wingenfeld, K.; Piber, D.; et al. Pro-inflammatory monocyte phenotype and cell-specific steroid signaling alterations in unmedicated patients with major depressive disorder. Font. Immunol. 2018, 9, 2693. [Google Scholar] [CrossRef]
- Ishikawa, Y.; Furuyashiki, T. The impact of stress on immune systems and its relevance to mental illness. Neurosci. Res. 2022, 175, 16–24. [Google Scholar] [CrossRef]
- Ilchmann-Diounou, H.; Menard, S. Psychological Stress, Intestinal Barrier Dysfunctions, and Autoimmune Disorders: An Overview. Front. Immunol. 2020, 11, 1823. [Google Scholar] [CrossRef]
- Tohid, H.; Shenefelt, P.D.; Burney, W.A.; Aqueel., N. Psychodermatology: An Association of Primary Psychiatric Disorders with Skin. Rev. Colomb. Psiquiatr. (Engl. Ed.) 2019, 48, 50–57. [Google Scholar] [CrossRef] [PubMed]
- De Souza, F.T.; Kummer, A.; Silva, M.L.; Amaral, T.M.; Abdo, E.N.; Abreu, M.H.; Silva, T.A.; Teixeira, A.L. The association of openness personality trait with stress-related salivary biomarkers in burning mouth syndrome. Neuroimmunomodulation 2015, 22, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Paykel, E.S.; Prusoff, B.A.; Uhlenhuth, E.H. Scaling of life events. Arch. Gen. Psychiatry 1971, 25, 340–347. [Google Scholar] [CrossRef]
| Sociodemographic Characteristics | Cases (n = 20) | Controls (n = 20) | p | |
|---|---|---|---|---|
| Age | 58.05 ± 15.61 | 57.4 ± 15.37 | 0.89 § | |
| Gender | Female | 15 (75%) | 15 (75%) | |
| Male | 5 (25%) | 5 (25%) | 1.00 * | |
| Marital status | Single | 7 (35.0%) | 4 (20.0%) | |
| Married | 5 (25.0%) | 10 (50.0%) | ||
| Divorced | 4 (20.0%) | 3 (15.0%) | ||
| Widowed | 4 (20.0%) | 3 (15.0%) | 0.43 * | |
| Occupation | Home | 6 (30.0%) | 10 (50.0%) | |
| Merchant | 2 (10.0%) | 3 (15.0%) | ||
| Employee | 6 (30.0%) | 2 (10.0%) | ||
| Pensioner/retired | 4 (20.0%) | 3 (15.0%) | ||
| Student | 2 (10.0%) | 2 (10.0%) | 0.50 * | |
| Personality categories | ||||
| Openness (R: 1–50) | 34.2 (±4.7) | 38.2 (±4.1) | 0.01 § | |
| Neuroticism (R: 1–40) | 25.5 (±5.4) | 21.7 (±5.1) | 0.03 § | |
| Extroversion (R: 1–40) | 24.5 (±4.6) | 25.6 (±2.7) | 0.36 § | |
| Responsibility (R: 1–45) | 32.2 (±4.5) | 34.3 (±3.6) | 0.10 § | |
| Agreeableness (R:1–45) | 30.5 (±3.6) | 34 (±4.3) | 0.01 § | |
| Stress categories | ||||
| High (R: 301–max) | 9 (45.0%) | 8 (40.0%) | ||
| Medium (R: 151–300) | 5 (25.0%) | 9 (45.0%) | ||
| Low (R: 0–150) | 6 (30.0%) | 3 (15.0%) | 0.37 * | |
| Total, obtained | 316.1 (±257.0) | 352.4 (±251.5) | 0.65 § | |
| OHIP-49 | ||||
| Functional limitation (R: 0–36) | 18.3 (±7.2) | 13.4 (±9.9) | 0.082 § | |
| Physical pain (R: 0–36) | 15.7 (±8.0) | 11.6 (±9.9) | 0.158 § | |
| Psychological discomfort (R: 0–20) | 11.2 (±5.7) | 7.6 (±6.8) | 0.077 § | |
| Physical disability (R: 0–36) | 14.5 (±7.9) | 8.6 (±9.9) | 0.042 § | |
| Psychological disability (R: 0–24) | 8.3 (±6.4) | 6.0 (±6.5) | 0.277 § | |
| Social disability (R: 0–20) | 3.7 (±4.3) | 2.0 (±2.6) | 0.143 § | |
| Handicap (R: 0–24) | 6.8 (±7.1) | 3.2 (±4.2) | 0.060 § | |
| Total (R: 0–196) | 78.8 (±39.0) | 52.7 (±44.8) | 0.056 § | |
| People with high stress (n = 17) | ||||
| Neuroticism | 28.0 (±5.3) | 24.5 (±5.8) | 0.2262 § | |
| Psychological discomfort | 13.5 (±4.4) | 11.2 (±7.2) | 0.4328 § | |
| Psychological disability | 10.3 (±6.7) | 9.5 (±6.2) | 0.7943 § | |
| Total, OHIP | 97.3 (±34.6) | 76.9 (±41.8) | 0.2867 § | |
| Mean neuroticism according to quality of life | ||||
| Good | 22.3 (±5.6) | 20.5 (±4.6) | 0.4429 § | |
| Poor | 27.4 (±4.6) | 24.1 (±5.4) | 0.1769 § | |
| Quality of Life | Cases | Controls | Total | OR | CI | p | |||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||||
| Functional limitation | |||||||||
| Good | 9 | 45 | 13 | 65 | 22 | 55 | 2.27 | 0.54–9.82 | 0.20 |
| Poor | 11 | 55 | 7 | 35 | 18 | 45 | |||
| TOTAL | 20 | 100 | 20 | 100 | 40 | 100 | |||
| Physical pain | |||||||||
| Good | 8 | 40 | 12 | 60 | 20 | 50 | 2.25 | 0.54–9.61 | 0.21 |
| Poor | 12 | 60 | 8 | 40 | 20 | 50 | |||
| TOTAL | 20 | 100 | 20 | 100 | 40 | 100 | |||
| Psychological discomfort | |||||||||
| Good | 6 | 30 | 14 | 70 | 20 | 50 | 5.44 | 1.18–26.25 | 0.01 |
| Poor | 14 | 70 | 6 | 30 | 20 | 50 | |||
| TOTAL | 20 | 100 | 20 | 100 | 40 | 100 | |||
| Physical disability | |||||||||
| Good | 7 | 35 | 14 | 70 | 21 | 52.5 | 4.33 | 0.97–20.19 | 0.03 |
| Poor | 13 | 65 | 6 | 30 | 19 | 47.5 | |||
| TOTAL | 20 | 100 | 20 | 100 | 40 | 100 | |||
| Psychological disability | |||||||||
| Good | 9 | 45 | 12 | 60 | 21 | 52.5 | 1.83 | 0.44–7.72 | 0.34 |
| Poor | 11 | 55 | 8 | 40 | 19 | 47.5 | |||
| TOTAL | 20 | 100 | 20 | 100 | 40 | 100 | |||
| Social disability | |||||||||
| Good | 8 | 40 | 13 | 65 | 21 | 52.5 | 2.77 | 0.65–12.20 | 0.11 |
| Poor | 12 | 60 | 7 | 35 | 19 | 47.5 | |||
| TOTAL | 20 | 100 | 20 | 100 | 40 | 100 | |||
| Handicap | |||||||||
| Good | 9 | 45 | 13 | 65 | 22 | 55 | 2.27 | 0.54–9.82 | 0.20 |
| Poor | 11 | 55 | 7 | 35 | 18 | 45 | |||
| TOTAL | 20 | 100 | 20 | 100 | 40 | 100 | |||
| Total, OHIP | |||||||||
| Good | 7 | 35 | 13 | 65 | 20 | 50 | 3.45 | 0.79–15.46 | 0.06 |
| Poor | 13 | 65 | 7 | 35 | 20 | 50 | |||
| TOTAL | 20 | 100 | 20 | 100 | 40 | 100 | |||
| Model Variables | p | OR | CI 95% |
|---|---|---|---|
| Marital status | |||
| Married | 0.28 | 0.26 | 0.02–2.88 |
| Divorced | 0.82 | 0.70 | 0.03–15.48 |
| Widowed | 0.72 | 1.69 | 0.10–28.95 |
| Stress | |||
| Medium | 0.47 | 0.35 | 0.02–5.94 |
| High | 0.96 | 0.93 | 0.04–19.88 |
| Personality | |||
| Openness | 0.13 | 0.79 | 0.58–1.07 |
| Neuroticism | 0.33 | 1.12 | 0.89–1.39 |
| Extroversion | 0.93 | 1.01 | 0.72–1.42 |
| Responsibility | 0.79 | 1.04 | 0.78–1.39 |
| Agreeableness | 0.11 | 0.81 | 0.62–1.05 |
| Psychological discomfort dimension of the OHIP-49 | |||
| Group | |||
| Case | 0.03 | 38.02 | 1.41–1022.74 |
| Stress | |||
| Medium | 0.16 | 8.71 | 0.41–183.38 |
| High | 0.09 | 16.16 | 0.66–397.80 |
| Personality | |||
| Openness | 0.85 | 1.03 | 0.78–1.34 |
| Neuroticism | 0.04 | 1.47 | 1.03–2.11 |
| Extroversion | 0.57 | 0.90 | 0.65–1.26 |
| Responsibility | 0.22 | 1.18 | 0.90–1.56 |
| Agreeableness | 0.09 | 1.39 | 0.95–2.05 |
| Physical disability dimension of the OHIP-49 | |||
| Group | |||
| Case | 0.03 | 45.35 | 1.50–1367.6 |
| Stress | |||
| Medium | 0.07 | 21.65 | 0.80–588.67 |
| High | 0.07 | 28.30 | 0.79–1008.4 |
| Personality | |||
| Openness | 0.31 | 1.25 | 0.81–1.94 |
| Neuroticism | 0.11 | 1.28 | 0.94–1.75 |
| Extroversion | 0.81 | 1.04 | 0.75–1.45 |
| Responsibility | 0.61 | 0.93 | 0.70–1.24 |
| Agreeableness | 0.91 | 1.02 | 0.77–1.33 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gaitán-Cepeda, L.A.; Rivera-Reza, D.I.; Villanueva-Vilchis, M.d.C. Neuroticism and Psychological Stress in Patients Suffering Oral Lichen Planus: Research Evidence of Psycho-Stomatology? Healthcare 2023, 11, 1738. https://doi.org/10.3390/healthcare11121738
Gaitán-Cepeda LA, Rivera-Reza DI, Villanueva-Vilchis MdC. Neuroticism and Psychological Stress in Patients Suffering Oral Lichen Planus: Research Evidence of Psycho-Stomatology? Healthcare. 2023; 11(12):1738. https://doi.org/10.3390/healthcare11121738
Chicago/Turabian StyleGaitán-Cepeda, Luis Alberto, Diana Ivette Rivera-Reza, and María del Carmen Villanueva-Vilchis. 2023. "Neuroticism and Psychological Stress in Patients Suffering Oral Lichen Planus: Research Evidence of Psycho-Stomatology?" Healthcare 11, no. 12: 1738. https://doi.org/10.3390/healthcare11121738
APA StyleGaitán-Cepeda, L. A., Rivera-Reza, D. I., & Villanueva-Vilchis, M. d. C. (2023). Neuroticism and Psychological Stress in Patients Suffering Oral Lichen Planus: Research Evidence of Psycho-Stomatology? Healthcare, 11(12), 1738. https://doi.org/10.3390/healthcare11121738







