De Quervain Tenosynovitis as a Risk Factor of New-Onset Adhesive Capsulitis: A Nationwide Cohort Study
Abstract
1. Introduction
2. Materials and Methods
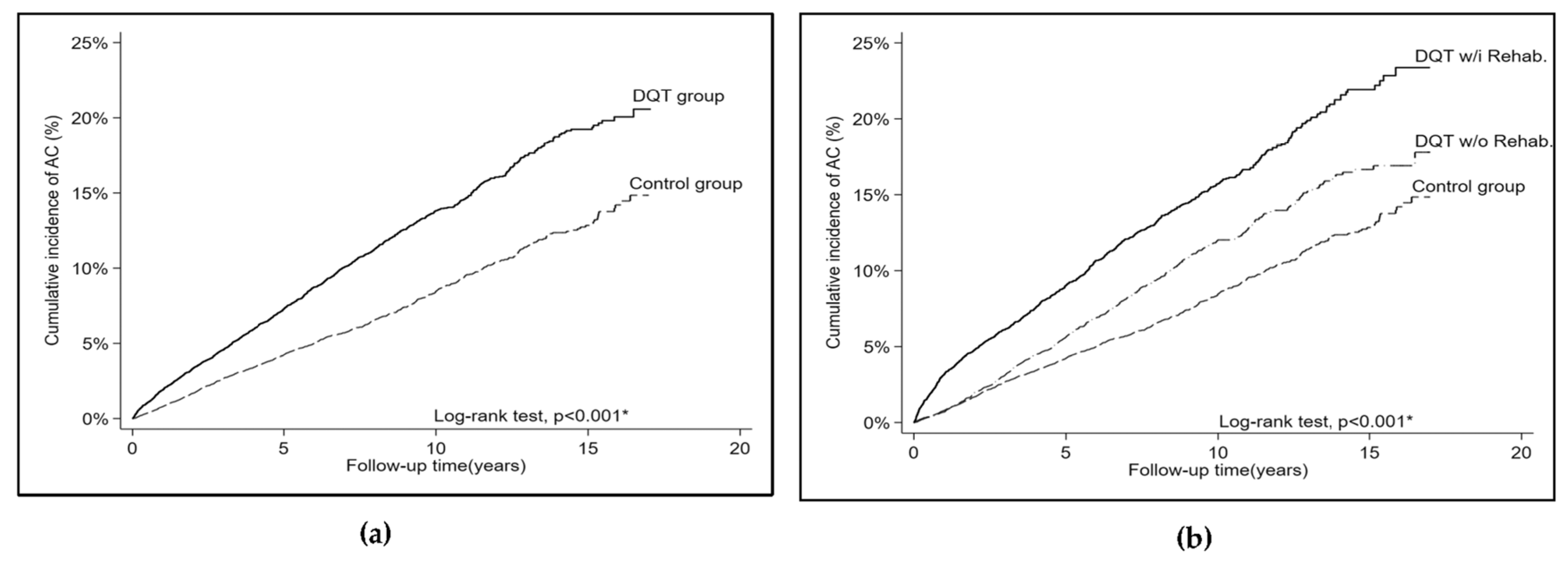
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ilyas, A.M.; Ast, M.; Schaffer, A.A.; Thoder, J. De Quervain tenosynovitis of the wrist. J. Am. Acad. Orthop. Surg. 2007, 15, 757–764. [Google Scholar] [CrossRef] [PubMed]
- Wolf, J.M.; Sturdivant, R.X.; Owens, B.D. Incidence of de Quervain’s tenosynovitis in a young, active population. J. Hand Surg. Am. 2009, 34, 112–115. [Google Scholar] [CrossRef] [PubMed]
- Ilyas, A.M. Nonsurgical treatment of de Quervain’s tenosynovitis. J. Hand Surg. Am. 2009, 34, 928–929. [Google Scholar] [CrossRef] [PubMed]
- Fedorczyk, J.M. Tendinopathies of the elbow, wrist, and hand: Histopathology and clinical considerations. J. Hand Ther. 2012, 25, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Robinson, B.S. Rehabilitation of a cellist after surgery for de Quervain’s tenosynovitis and intersection syndrome. Med. Probl. Perform. Artist. 2003, 18, 106–112. [Google Scholar] [CrossRef]
- Papa, J.A. Conservative management of de Quervain’s stenosing tenosynovitis: A case report. J. Can. Chiropr. Assoc. 2012, 56, 112–120. [Google Scholar]
- Jaworski, C.A.; Krause, M.; Brown, J. Rehabilitation of the wrist and hand following sports injury. Clin. Sport. Med. 2010, 29, 61–80. [Google Scholar] [CrossRef]
- Ramirez, J. Adhesive Capsulitis: Diagnosis and Management. Am. Fam. Physician 2019, 99, 297–300. [Google Scholar]
- Redler, L.H.; Dennis, E.R. Treatment of Adhesive Capsulitis of the Shoulder. J. Am. Acad. Orthop. Surg. 2019, 27, e544–e554. [Google Scholar] [CrossRef]
- D’Orsi, G.M.; Via, A.G.; Frizziero, A.; Oliva, F. Treatment of adhesive capsulitis: A review. Muscles Ligaments Tendons J. 2012, 2, 70–78. [Google Scholar]
- Harris, J.D.; Griesser, M.J.; Copelan, A.; Jones, G.L. Treatment of adhesive capsulitis with intra-articular hyaluronate: A systematic review. Int. J. Shoulder Surg. 2011, 5, 31–37. [Google Scholar] [CrossRef] [PubMed]
- McAlister, I.; Sems, S.A. Arthrofibrosis after periarticular fracture fixation. Orthop. Clin. N. Am. 2016, 47, 345–355. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Q.Y.; Zang, C.H.; Lin, L.; Chen, S.B.; Li, X.F.; Xiao, Z.Y.; Dong, H.Y.; Zhang, A.L.; Chen, R. Epidemiologic study of soft tissue rheumatism in Shantou and Taiyuan, China. Chin. Med. J. 2010, 123, 2058–2062. [Google Scholar] [PubMed]
- Walker-Bone, K.; Palmer, K.T.; Reading, I.; Coggon, D.; Cooper, C. Prevalence and impact of musculoskeletal disorders of the upper limb in the general population. Arthritis Rheum. 2004, 51, 642–651. [Google Scholar] [CrossRef]
- Yeh, K.T.; Lee, R.P.; Yu, T.C.; Wang, J.H.; Liu, K.L.; Peng, C.H.; Chen, H.W.; Chen, I.H.; Hsu, C.Y.; Lin, C.L.; et al. Risk factors for carpal tunnel syndrome or trigger finger following distal radius fracture: A nationwide study. Sci. Rep. 2020, 10, 469. [Google Scholar] [CrossRef]
- Hsieh, H.H.; Wu, W.T.; Shih, J.T.; Wang, J.H.; Yeh, K.T. Incidence of carpal tunnel syndrome requiring surgery may increase in patients treated with trigger finger release: A retrospective cohort study. Clin. Epidemiol. 2022, 14, 1079–1086. [Google Scholar] [CrossRef]
- Petit Le Manac’h, A.; Roquelaure, Y.; Ha, C.; Bodin, J.; Meyer, G.; Bigot, F.; Veaudor, M.; Descatha, A.; Goldberg, M.; Imbernon, E. Risk factors for de Quervain’s disease in a French working population. Scand. J. Work Environ. Health 2011, 37, 394–401. [Google Scholar] [CrossRef]
- Wang, J.Y.; Liaw, C.K.; Huang, C.C.; Liou, T.H.; Lin, H.W.; Huang, S.W. Hyperlipidemia is a risk factor of adhesive capsulitis: Real-world evidence using the Taiwanese National Health Insurance Research Database. Orthop. J. Sport. Med. 2021, 9, 2325967120986808. [Google Scholar] [CrossRef]
- Cohen, C.; Leal, M.F.; Loyola, L.C.; Santos, S.E.B.; Ribeiro-Dos-Santos, Â.K.C.; Belangero, P.S.; Figueiredo, E.A.; Wajnsztejn, A.; de Oliveira, A.M.; Smith, M.C.; et al. Genetic variants involved in extracellular matrix homeostasis play a role in the susceptibility to frozen shoulder: A case-control study. J. Orthop. Res. 2019, 37, 948–956. [Google Scholar] [CrossRef]
- Clarke, M.T.; Lyall, H.A.; Grant, J.W.; Matthewson, M.H. The histopathology of de Quervain’s disease. J. Hand Surg. Br. 1998, 23, 732–734. [Google Scholar] [CrossRef]
- Selley, R.S.; Johnson, D.J.; Nicolay, R.W.; Ravi, K.; Lawton, C.D.; Tjong, V.K.; Terry, M.A. Risk factors for adhesive capsulitis requiring shoulder arthroscopy: A clinical retrospective case series study. J. Orthop. 2019, 19, 14–16. [Google Scholar] [CrossRef] [PubMed]
- Itoi, E.; Arce, G.; Bain, G.I.; Diercks, R.L.; Guttmann, D.; Imhoff, A.B.; Mazzocca, A.D.; Sugaya, H.; Yoo, Y.S. Shoulder Stiffness: Current Concepts and Concerns. Arthroscopy 2016, 32, 1402–1414. [Google Scholar] [CrossRef] [PubMed]
- Escamilla, R.F.; Hooks, T.R.; Wilk, K.E. Optimal management of shoulder impingement syndrome. Open Access J. Sport. Med. 2014, 5, 13–24. [Google Scholar] [CrossRef]
- Cucchi, D.; Marmotti, A.; De Giorgi, S.; Costa, A.; D’Apolito, R.; Conca, M.; Russo, A.; Saccomanno, M.F.; de Girolamo, L. Risk factors for shoulder stiffness: Current concepts. Joints 2017, 5, 217–223. [Google Scholar] [CrossRef]
- Denard, P.J.; Lädermann, A.; Burkhart, S.S. Prevention and management of stiffness after arthroscopic rotator cuff repair: Systematic review and implications for rotator cuff healing. Arthroscopy 2011, 27, 842–848. [Google Scholar] [CrossRef] [PubMed]
- Koorevaar, R.C.T.; Van’t Riet, E.; Ipskamp, M.; Bulstra, S.K. Incidence and prognostic factors for postoperative frozen shoulder after shoulder surgery: A prospective cohort study. Arch. Orthop. Trauma Surg. 2017, 137, 293–301. [Google Scholar] [CrossRef]
- Frank, C.; Kobesova, A.; Kolar, P. Dynamic neuromuscular stabilization & sports rehabilitation. Int. J. Sport. Phys. Ther. 2013, 8, 62–73. [Google Scholar]
- Chan, H.B.Y.; Pua, P.Y.; How, C.H. Physical therapy in the management of frozen shoulder. Singap. Med. J. 2017, 58, 685–689. [Google Scholar] [CrossRef]
- Ludewig, P.M.; Reynolds, J.F. The association of scapular kinematics and glenohumeral joint pathologies. J. Orthop. Sport. Phys. Ther. 2009, 39, 90–104. [Google Scholar] [CrossRef]
- Steultjens, E.M.; Dekker, J.; Bouter, L.M.; van Schaardenburg, D.; van Kuyk, M.A.; van den Ende, C.H. Occupational therapy for rheumatoid arthritis. Cochrane Database Syst. Rev. 2004, 2004, CD003114. [Google Scholar] [CrossRef]
- Schlussel, A.T.; Maykel, J.A. Ergonomics and Musculoskeletal Health of the Surgeon. Clin. Colon Rectal Surg. 2019, 32, 424–434. [Google Scholar] [CrossRef]
- Fakoya, A.O.; Tarzian, M.; Sabater, E.L.; Burgos, D.M.; Maldonado Marty, G.I. De Quervain’s Disease: A Discourse on Etiology, Diagnosis, and Treatment. Cureus 2023, 15, e38079. [Google Scholar] [CrossRef] [PubMed]
- Parel, I.; Candoli, V.; Filippi, M.V.; Padolino, A.; Merolla, G.; Sanniti, S.; Galassi, R.; Paladini, P.; Cutti, A.G. Shoulder Rehabilitation Exercises with Kinematic Biofeedback after Arthroscopic Rotator Cuff Repair: Protocol for a New Integrated Rehabilitation Program. JMIR Res. Protoc. 2023, 12, e35757. [Google Scholar] [CrossRef] [PubMed]
- Hoe, V.C.; Urquhart, D.M.; Kelsall, H.L.; Zamri, E.N.; Sim, M.R. Ergonomic interventions for preventing work-related musculoskeletal disorders of the upper limb and neck among office workers. Cochrane Database Syst. Rev. 2018, 10, CD008570. [Google Scholar] [CrossRef] [PubMed]
- Goel, R.; Abzug, J.M. De Quervain’s tenosynovitis: A review of the rehabilitative options. Hand 2015, 10, 1–5. [Google Scholar] [CrossRef]
- Marik, T.L.; Roll, S.C. Effectiveness of Occupational Therapy Interventions for Musculoskeletal Shoulder Conditions: A Systematic Review. Am. J. Occup. Ther. 2017, 71, 7101180020p1–7101180020p11. [Google Scholar] [CrossRef]
- Lowe, B.D.; Dick, R.B. Workplace exercise for control of occupational neck/shoulder disorders: A review of prospective studies. Environ. Health Insights 2015, 8 (Suppl. S1), 75–95. [Google Scholar] [CrossRef]
- Benites-Zapata, V.A.; Jiménez-Torres, V.E.; Ayala-Roldán, M.P. Problematic smartphone use is associated with de Quervain’s tenosynovitis symptomatology among young adults. Musculoskelet. Sci. Pract. 2021, 53, 102356. [Google Scholar] [CrossRef]
- Kingston, K.; Curry, E.J.; Galvin, J.W.; Li, X. Shoulder adhesive capsulitis: Epidemiology and predictors of surgery. J. Shoulder Elbow. Surg. 2018, 27, 1437–1443. [Google Scholar] [CrossRef]
- Mandiroglu, S.; Alemdaroglu, E. Idiopathic carpal tunnel syndrome and de Quervain’s tenosynovitis: Is there an association? Somatosens. Mot. Res. 2021, 38, 353–356. [Google Scholar] [CrossRef]

| Variables | Control (n = 16,024) | De Quervain Tenosynovitis (n = 16,024) | p-Value |
|---|---|---|---|
| Age (years) | 45.3 ± 13.6 | 45.3 ± 13.7 | 0.960 |
| Age group | 0.966 | ||
| <20 years | 277 (1.7%) | 280 (1.8%) | |
| 20–40 years | 5567 (34.7%) | 5583 (34.8%) | |
| 40–60 years | 7882 (49.2%) | 7840 (48.9%) | |
| ≥60 years | 2298 (14.3%) | 2321 (14.5%) | |
| Age group | 0.826 | ||
| <40 years | 5844 (36.5%) | 5863 (36.6%) | |
| ≥40 years | 10,180 (63.5%) | 10,161 (63.4%) | |
| Gender | 0.815 | ||
| Male | 3886 (24.3%) | 3904 (24.4%) | |
| Female | 12,138 (75.7%) | 12,120 (75.6%) | |
| Rehabilitation (%) | NA | 8108 (50.6%) | |
| Comorbidity | |||
| Hypertension | 2438 (15.2%) | 2416 (15.1%) | 0.732 |
| Diabetes mellitus | 1274 (8.0%) | 1261 (7.9%) | 0.788 |
| Hyperlipidemia | 1721 (10.7%) | 1702 (10.6%) | 0.731 |
| Coronary artery disease | 503 (3.1%) | 527 (3.3%) | 0.447 |
| Chronic liver disease | 684 (4.3%) | 695 (4.3%) | 0.762 |
| Hyperthyroidism | 87 (0.5%) | 104 (0.7%) | 0.217 |
| Variables | De Quervain Tenosynovitis | |
|---|---|---|
| Yes | No | |
| Patient numbers | 16,024 | 16,024 |
| Adhesive capsulitis of shoulder cases | 1563 | 906 |
| Person-years | 98,842 | 101,683 |
| Incidence rate a | 15.8 | 8.9 |
| Univariate model | ||
| Crude HR (95% CI) | 1.68 (1.55–1.83) | 1 (ref.) |
| p-value | <0.001 * | |
| Multivariate model b | ||
| aHR (95% CI) | 1.68 (1.54–1.82) | 1 (ref.) |
| p-value | <0.001 * | |
| Variables | De Quervain Tenosynovitis | Control | |
|---|---|---|---|
| W/I Rehabilitation | W/O Rehabilitation | ||
| Patient numbers | 7860 | 8164 | 16,024 |
| Adhesive capsulitis of shoulder cases | 910 | 653 | 906 |
| Person-years | 46,819 | 52,023 | 101,683 |
| Incidence rate a | 19.4 | 12.6 | 8.9 |
| Univariate model | |||
| Crude HR (95% CI) | 2.05 (1.87–2.25) | 1.35 (1.22–1.50) | 1 (ref.) |
| p-value | <0.001 * | <0.001 * | |
| Model 1 b | |||
| aHR (95% CI) | 2.12 (1.93–2.33) | 1.30 (1.18–1.44) | 1 (ref.) |
| p-value | <0.001 * | <0.001 * | |
| Model 2 c | |||
| aHR (95% CI) | 1.62 (1.46–1.80) | 1 (ref.) | |
| p-value | <0.001 * | ||
| Variables | Crude HR a (95% CI) | p-Value | Adjusted HR a (95% CI) | p-Value | p for Interaction |
|---|---|---|---|---|---|
| Main model | |||||
| Control | 1.00 | 1.00 | |||
| De Quervain tenosynovitis | 1.68 (1.55–1.83) | <0.001 * | 1.68 (1.54–1.82) | <0.001 * | |
| Age | |||||
| <40 years | |||||
| Control | 1.00 | 1.00 | |||
| De Quervain tenosynovitis | 1.88 (1.47–2.39) | <0.001 * | 1.87 (1.47–2.38) | <0.001 * | 0.415 |
| ≥40 years | |||||
| Control | 1.00 | 1.00 | |||
| De Quervain tenosynovitis | 1.67 (1.53–1.82) | <0.001 * | 1.67 (1.53–1.83) | <0.001 * | |
| Gender | |||||
| Male | |||||
| Control | 1.00 | 1.00 | |||
| De Quervain tenosynovitis | 2.09 (1.72–2.55) | <0.001 * | 2.10 (1.72–2.56) | <0.001 * | 0.021 * |
| Female | |||||
| Control | 1.00 | 1.00 | |||
| De Quervain tenosynovitis | 1.60 (1.46–1.76) | <0.001 * | 1.62 (1.48–1.77) | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, P.; Hong, C.-I.; Liang, C.-C.; Wu, W.-T.; Wang, J.-H.; Yeh, K.-T. De Quervain Tenosynovitis as a Risk Factor of New-Onset Adhesive Capsulitis: A Nationwide Cohort Study. Healthcare 2023, 11, 1758. https://doi.org/10.3390/healthcare11121758
Huang P, Hong C-I, Liang C-C, Wu W-T, Wang J-H, Yeh K-T. De Quervain Tenosynovitis as a Risk Factor of New-Onset Adhesive Capsulitis: A Nationwide Cohort Study. Healthcare. 2023; 11(12):1758. https://doi.org/10.3390/healthcare11121758
Chicago/Turabian StyleHuang, Pao, Ching-I Hong, Chung-Chao Liang, Wen-Tien Wu, Jen-Hung Wang, and Kuang-Ting Yeh. 2023. "De Quervain Tenosynovitis as a Risk Factor of New-Onset Adhesive Capsulitis: A Nationwide Cohort Study" Healthcare 11, no. 12: 1758. https://doi.org/10.3390/healthcare11121758
APA StyleHuang, P., Hong, C.-I., Liang, C.-C., Wu, W.-T., Wang, J.-H., & Yeh, K.-T. (2023). De Quervain Tenosynovitis as a Risk Factor of New-Onset Adhesive Capsulitis: A Nationwide Cohort Study. Healthcare, 11(12), 1758. https://doi.org/10.3390/healthcare11121758









