The Multimorbidity and Lifestyle Correlates in Chinese Population Residing in Macau: Findings from a Community-Based Needs Assessment Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Settings
2.2. Ethical Considerations
2.3. Participants
2.4. Sampling and Recruitment
2.5. Measures
2.5.1. Assessment of Chronic Diseases
2.5.2. Identification of Multimorbidity
2.5.3. Lifestyle Factors and Anthropometrics
2.5.4. Lifestyle Score Calculation
2.5.5. Socio-Demographics
2.6. Statistical Analysis
3. Results
3.1. Basic and Lifestyle Characteristics of the Participants
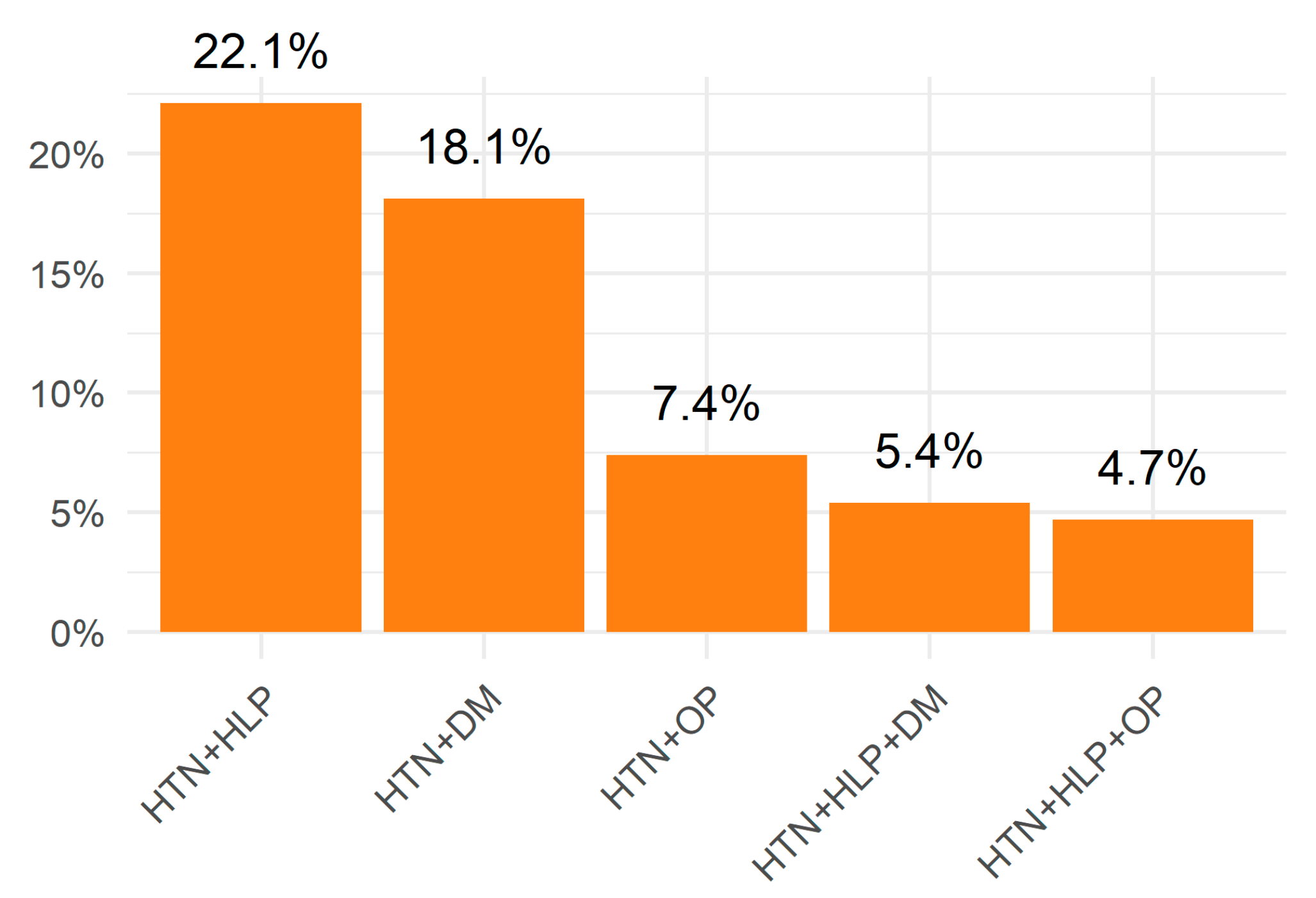
3.2. Prevalence of Chronic Diseases and Multimorbidity in the Study Population
3.3. Association between Lifestyle Factors and Lifestyle Score and Multimorbidity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Beard, J.R.; Officer, A.; de Carvalho, I.A.; Sadana, R.; Pot, A.M.; Michel, J.-P.; Lloyd-Sherlock, P.; Epping-Jordan, J.E.; Peeters, G.M.E.E.G.; Mahanani, W.R.; et al. The World report on ageing and health: A policy framework for healthy ageing. Lancet 2016, 387, 2145–2154. [Google Scholar] [CrossRef]
- Wang, H.H.; Wang, J.J.; Wong, S.Y.; Wong, M.C.; Li, F.J.; Wang, P.X.; Zhou, Z.H.; Zhu, C.Y.; Griffiths, S.M.; Mercer, S.W. Epidemiology of multimorbidity in China and implications for the healthcare system: Cross-sectional survey among 162,464 community household residents in southern China. BMC Med. 2014, 12, 188. [Google Scholar] [CrossRef] [PubMed]
- Newman, D.; Tong, M.; Levine, E.; Kishore, S. Prevalence of multiple chronic conditions by U.S. state and territory, 2017. PLoS ONE 2020, 15, e0232346. [Google Scholar] [CrossRef]
- Nunes, B.P.; Camargo-Figuera, F.A.; Guttier, M.; de Oliveira, P.D.; Munhoz, T.N.; Matijasevich, A.; Bertoldi, A.D.; Wehrmeister, F.C.; Silveira, M.P.T.; Thumé, E.; et al. Multimorbidity in adults from a southern Brazilian city: Occurrence and patterns. Int. J. Public Health 2016, 61, 1013–1020. [Google Scholar] [CrossRef] [PubMed]
- Chung, R.Y.; Mercer, S.; Lai, F.T.T.; Yip, B.H.K.; Wong, M.C.S.; Wong, S.Y.S. Socioeconomic Determinants of Multimorbidity: A Population-Based Household Survey of Hong Kong Chinese. PLoS ONE 2015, 10, e0140040. [Google Scholar] [CrossRef]
- Nguyen, H.; Manolova, G.; Daskalopoulou, C.; Vitoratou, S.; Prince, M.; Prina, A.M. Prevalence of multimorbidity in community settings: A systematic review and meta-analysis of observational studies. J. Comorbidity 2019, 9, 2235042x19870934. [Google Scholar] [CrossRef]
- Garin, N.; Koyanagi, A.; Chatterji, S.; Tyrovolas, S.; Olaya, B.; Leonardi, M.; Lara, E.; Koskinen, S.; Tobiasz-Adamczyk, B.; Ayuso-Mateos, J.L.; et al. Global Multimorbidity Patterns: A Cross-Sectional, Population-Based, Multi-Country Study. J. Gerontol. Ser. A 2016, 71, 205–214. [Google Scholar] [CrossRef]
- Zhao, Y.; Atun, R.; Oldenburg, B.; McPake, B.; Tang, S.; Mercer, S.W.; E Cowling, T.; Sum, G.; Qin, V.M.; Lee, J.T. Physical multimorbidity, health service use, and catastrophic health expenditure by socioeconomic groups in China: An analysis of population-based panel data. Lancet Glob. Health 2020, 8, e840–e849. [Google Scholar] [CrossRef]
- Wong, E.L.Y.; Xu, R.H.; Cheung, A.W.L. Measuring the impact of chronic conditions and associated multimorbidity on health-related quality of life in the general population in Hong Kong SAR, China: A cross-sectional study. PLoS ONE 2019, 14, e0224970. [Google Scholar] [CrossRef]
- Nunes, B.P.; Flores, T.R.; Mielke, G.I.; Thumé, E.; Facchini, L.A. Multimorbidity and mortality in older adults: A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2016, 67, 130–138. [Google Scholar] [CrossRef]
- Nguyen, H.; Chua, K.-C.; Dregan, A.; Vitoratou, S.; Bayes-Marin, I.; Olaya, B.; Prina, A.M. Factors Associated With Multimorbidity Patterns in Older Adults in England: Findings From the English Longitudinal Study of Aging (ELSA). J. Aging Heal. 2019, 32, 1120–1132. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Sit, R.W.S.; Wong, C.; Zou, D.; Mercer, S.W.; Johnston, M.C.; Wong, S.Y.S. Cohort profile: The prospective study on Chinese elderly with multimorbidity in primary care in Hong Kong. BMJ open 2020, 10, e027279. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhou, L.; Liu, S.; Qiao, Y.; Wu, Y.; Key, C.; Shen, Y. Prevalence, correlates and outcomes of multimorbidity among the middle-aged and elderly: Findings from the China Health and Retirement Longitudinal Study. Arch. Gerontol. Geriatr. 2020, 90, 104135. [Google Scholar] [CrossRef] [PubMed]
- Palladino, R.; Lee, J.T.; Ashworth, M.; Triassi, M.; Millett, C. Associations between multimorbidity, healthcare utilisation and health status: Evidence from 16 European countries. Age Ageing 2016, 45, 431–435. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.S.; Egede, L.E. The Association Between Multimorbidity and Quality of Life, Health Status and Functional Disability. Am. J. Med. Sci. 2016, 352, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Aminisani, N.; Stephens, C.; Allen, J.; Alpass, F.; Shamshirgaran, S.M. Socio-demographic and lifestyle factors associated with multimorbidity in New Zealand. Epidemiol. Health 2020, 42, e2020001. [Google Scholar] [CrossRef]
- Vancampfort, D.; Koyanagi, A.; Ward, P.B.; Rosenbaum, S.; Schuch, F.B.; Mugisha, J.; Richards, J.; Firth, J.; Stubbs, B. Chronic physical conditions, multimorbidity and physical activity across 46 low- and middle-income countries. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 6. [Google Scholar] [CrossRef]
- Fortin, M.; Haggerty, J.; Almirall, J.; Bouhali, T.; Sasseville, M.; Lemieux, M. Lifestyle factors and multimorbidity: A cross sectional study. BMC Public Health 2014, 14, 686. [Google Scholar] [CrossRef]
- Wikström, K.; Lindström, J.; Harald, K.; Peltonen, M.; Laatikainen, T. Clinical and lifestyle-related risk factors for incident multimorbidity: 10-year follow-up of Finnish population-based cohorts 1982–2012. Eur. J. Intern. Med. 2015, 26, 211–216. [Google Scholar] [CrossRef]
- Wang, S.; Li, B.; Wu, Y.; Ungvari, G.S.; Ng, C.H.; Fu, Y.; Kou, C.; Yu, Y.; Sun, H.-Q.; Xiang, Y.-T. Relationship of Sleep Duration with Sociodemographic Characteristics, Lifestyle, Mental Health, and Chronic Diseases in a Large Chinese Adult Population. J. Clin. Sleep Med. 2017, 13, 377–384. [Google Scholar] [CrossRef]
- Agrawal, S.; Agrawal, P.K. Association Between Body Mass index and Prevalence of Multimorbidity in Low-and Middle-income Countries: A Cross-Sectional Study. Int. J. Med. Public Health 2016, 6, 73–83. [Google Scholar] [CrossRef]
- Booth, H.P.; Prevost, A.T.; Guilford, M.C. Impact of body mass index on prevalence of multimorbidity in primary care: Cohort study. Fam. Pract. 2014, 31, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Xu, L.; Li, J.; Sun, L.; Qin, W. Association between obesity-related anthropometric indices and multimorbidity among older adults in Shandong, China: A cross-sectional study. BMJ Open 2020, 10, e036664. [Google Scholar] [CrossRef]
- Kivimäki, M.; Strandberg, T.; Pentti, J.; Nyberg, S.T.; Frank, P.; Jokela, M.; Ervasti, J.; Suominen, S.B.; Vahtera, J.; Sipilä, P.N.; et al. Body-mass index and risk of obesity-related complex multimorbidity: An observational multicohort study. Lancet Diabetes Endocrinol. 2022, 10, 253–263. [Google Scholar] [CrossRef] [PubMed]
- Sakib, M.N.; Shooshtari, S.; St. John, P.; Menec, V. The prevalence of multimorbidity and associations with lifestyle factors among middle-aged Canadians: An analysis of Canadian Longitudinal Study on Aging data. BMC Public Health 2019, 19, 243. [Google Scholar] [CrossRef] [PubMed]
- Number of Casinos in Macao 2012–2022. Available online: https://www.statista.com/statistics/253763/number-of-casinos-inmacao/ (accessed on 28 June 2023).
- Hu, S.X.; Luk, A.; Leong, C.; U, C.; Van, F. The Correlations of Work Conditions with Unhealthy Lifestyles and Occupational Health Problems of Casino Croupiers in Macau. J. Gambl. Stud. 2013, 29, 255–268. [Google Scholar] [CrossRef] [PubMed]
- Life Expectancy at Birth, Total (Years). Available online: https://data.worldbank.org/indicator/SP.DYN.LE00.IN (accessed on 15 April 2023).
- Statistics and Census Service the Statistics and Census Service, Governo da Região Administrativa Especial de Macau. Detailed Results of 2016 Population By-Census. Available online: https://www.dsec.gov.mo/Statistic/Demographic/GlobalResultsOfBy-Census/2016%E4%B8%AD%E6%9C%9F%E4%BA%BA%E5%8F%A3%E7%B5%B1%E8%A8%88.aspx?lang=en-US (accessed on 15 April 2023).
- Zhou, M.; Wang, H.; Zeng, X.; Yin, P.; Zhu, J.; Chen, W.; Li, X.; Wang, L.; Wang, L.; Liu, Y.; et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 394, 1145–1158. [Google Scholar] [CrossRef]
- Diederichs, C.; Berger, K.; Bartels, D.B. The Measurement of Multiple Chronic Diseases—A Systematic Review on Existing Multimorbidity Indices. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2011, 66, 301–311. [Google Scholar] [CrossRef]
- Yang, H.-L.; Mo, B.-R.; Molassiotis, A.; Wang, M.; He, G.-L.; Xie, Y.J. Relationship between multimorbidity and composite lifestyle status in Shenzhen, China. J. Multimorb. Comorbidity 2022, 12, 26335565221123990. [Google Scholar] [CrossRef]
- Hagströmer, M.; Oja, P.; Sjöström, M. The International Physical Activity Questionnaire (IPAQ): A study of concurrent and construct validity. Public Health Nutr. 2006, 9, 755–762. [Google Scholar] [CrossRef]
- Nyberg, S.T.; Singh-Manoux, A.; Pentti, J.; Madsen, I.E.H.; Sabia, S.; Alfredsson, L.; Bjorner, J.B.; Borritz, M.; Burr, H.; Goldberg, M.; et al. Association of Healthy Lifestyle with Years Lived Without Major Chronic Diseases. JAMA Intern. Med. 2020, 180, 760–768. [Google Scholar] [CrossRef]
- Macfarlane, D.J.; Lee, C.C.; Ho, E.Y.; Chan, K.; Chan, D.T. Reliability and validity of the Chinese version of IPAQ (short, last 7 days). J. Sci. Med. Sport 2007, 10, 45–51. [Google Scholar] [CrossRef]
- Tsai, P.-S.; Wang, S.-Y.; Wang, M.-Y.; Su, C.-T.; Yang, T.-T.; Huang, C.-J.; Fang, S.-C. Psychometric Evaluation of the Chinese Version of the Pittsburgh Sleep Quality Index (CPSQI) in Primary Insomnia and Control Subjects. Qual. Life Res. 2005, 14, 1943–1952. [Google Scholar] [CrossRef]
- WHO. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. Available online: https://apps.who.int/iris/handle/10665/206936 (accessed on 15 April 2023).
- Goel, S.; Sharma, A.; Garg, A. Effect of Alcohol Consumption on Cardiovascular Health. Curr. Cardiol. Rep. 2018, 20, 19. [Google Scholar] [CrossRef] [PubMed]
- Traversy, G.; Chaput, J.-P. Alcohol Consumption and Obesity: An Update. Curr. Obes. Rep. 2015, 4, 122–130. [Google Scholar] [CrossRef]
- Machado, V.D.S.S.; Valadares, A.L.R.; da Costa-Paiva, L.S.; Moraes, S.S.; Pinto-Neto, A.M. Multimorbidity and associated factors in Brazilian women aged 40 to 65 years. Menopause 2012, 19, 569–575. [Google Scholar] [CrossRef]
- Wang, S.; D'Arcy, C.; Yu, Y.; Li, B.; Liu, Y.; Tao, Y.; Wu, Y.; Zhang, Q.; Xu, Z.; Fu, Y.; et al. Prevalence and patterns of multimorbidity in northeastern China: A cross-sectional study. Public Health 2015, 129, 1539–1546. [Google Scholar] [CrossRef] [PubMed]
- Franken, D.L.; Olinto, M.T.A.; Dias-Da-Costa, J.S.; de Bairros, F.S.; Paniz, V.M.V. Lifestyle, high Body Mass Index, and markers of socioeconomic conditions associated with multimorbidity in women. Rev. Bras. Epidemiologia 2022, 25, e220007. [Google Scholar] [CrossRef]
- Bureau, M.H. Macao Health Survey 2016. Available online: https://www.ssm.gov.mo/docs/12954/12954_639e8f42a2d942c0ad740130546aa16d_000.pdf (accessed on 15 April 2023).
- Dhalwani, N.N.; Zaccardi, F.; O’donovan, G.; Carter, P.; Hamer, M.; Yates, T.; Davies, M.; Khunti, K. Association Between Lifestyle Factors and the Incidence of Multimorbidity in an Older English Population. J. Gerontol. Ser. A 2017, 72, 528–534. [Google Scholar] [CrossRef] [PubMed]
- Nunes, B.P.; Batista, S.R.R.; Andrade, F.B.; Souza Junior, P.R.B.; Lima-Costa, M.F.; Facchini, L.A. Multimorbidity: The Brazilian Longitudinal Study of Aging (ELSI-Brazil). Revisit Sauce Publican 2018, 52, 10s. [Google Scholar] [CrossRef]
- Lin, Y.; Hu, Y.; Guo, J.; Chen, M.; Xu, X.; Wen, Y.; Yang, L.; Lin, S.; Li, H.; Wu, S. Association between sleep and multimorbidity in Chinese elderly: Results from the Chinese Longitudinal Healthy Longevity Survey (CLHLS). Sleep Med. 2022, 98, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, K.; Rodrigues, R.; Anderson, K.K.; Wilk, P.; Guaiana, G.; Stranges, S. Sleep behaviours and multimorbidity occurrence in middle-aged and older adults: Findings from the Canadian Longitudinal Study on Aging (CLSA). Sleep Med. 2020, 75, 156–162. [Google Scholar] [CrossRef] [PubMed]
- Xue, B.; Xue, Y.; Dong, F.; Zheng, X.; Shi, L.; Xiao, S.; Zhang, J.; Ou, W.; Wang, Q.; Zhang, C. The impact of socioeconomic status and sleep quality on the prevalence of multimorbidity in older adults. Front. Public Health 2022, 10, 959700. [Google Scholar] [CrossRef]
- Gulia, K.K.; Kumar, V.M. Sleep disorders in the elderly: A growing challenge. Psychogeriatrics 2018, 18, 155–165. [Google Scholar] [CrossRef]
- Röhr, S.; Wittmann, F.; Engel, C.; Enzenbach, C.; Witte, A.V.; Villringer, A.; Löffler, M.; Riedel-Heller, S.G. Social factors and the prevalence of social isolation in a population-based adult cohort. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 1959–1968. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.H.-J.; Olmstead, R.; Choi, H.; Carrillo, C.; Seeman, T.E.; Irwin, M.R. Associations of objective versus subjective social isolation with sleep disturbance, depression, and fatigue in community-dwelling older adults. Aging Ment. Health 2018, 23, 1130–1138. [Google Scholar] [CrossRef] [PubMed]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Adams Hillard, P.J.; Katz, E.S.; et al. National Sleep Foundation’s updated sleep duration recommendations: Final report. Sleep Health 2015, 1, 233–243. [Google Scholar] [CrossRef]
- Medic, G.; Wile, M.; Hamels, M.E. Short- and long-term health consequences of sleep disruption. Nat. Sci. Sleep 2017, 9, 151–161. [Google Scholar] [CrossRef]
- Liu, S.; Li, Y.; Zeng, X.; Wang, H.; Yin, P.; Wang, L.; Liu, Y.; Liu, J.; Qi, J.; Ran, S.; et al. Burden of Cardiovascular Diseases in China, 1990-2016: Findings From the 2016 Global Burden of Disease Study. JAMA Cardiol. 2019, 4, 342–352. [Google Scholar] [CrossRef]
- Ke, L.; Ho, J.; Feng, J.; Mpofu, E.; Dibley, M.J.; Li, Y.; Feng, X.; Van, F.; Lau, W.; Brock, K.E. Prevalence, Awareness, Treatment and Control of Hypertension in Macau: Results from a Cross-Sectional Epidemiological Study in Macau, China. Am. J. Hypertens. 2015, 28, 159–165. [Google Scholar] [CrossRef]
- Dorans, K.S.; Mills, K.T.; Liu, Y.; He, J. Trends in Prevalence and Control of Hypertension According to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) Guideline. J. Am. Hear. Assoc. 2018, 7, e008888. [Google Scholar] [CrossRef]
- Hu, R.-H.; Hsiao, F.-Y.; Chen, L.-J.; Huang, P.-T.; Hsu, W.W.-Y. Increasing age- and gender-specific burden and complexity of multimorbidity in Taiwan, 2003–2013: A cross-sectional study based on nationwide claims data. BMJ Open 2019, 9, e028333. [Google Scholar] [CrossRef]
- Lin, X.; Xing, D.; Peng, Y.Q.; Sheng, Z.F.; Wu, X.Y.; Wu, X.P.; Wu, F.; Yuan, L.Q.; Liao, E.Y. Epidemiology and management of osteoporosis in the People's Republic of China: Current perspectives. Clin. Interv. Aging 2015, 10, 1017–1033. [Google Scholar] [CrossRef]
- China CDC Weekly. Available online: https://weekly.chinacdc.cn/en/article/doi/10.46234/ccdcw2020.142 (accessed on 28 June 2023).
- Violin, C.; Foguet-Boreu, Q.; Flores-Mateo, G.; Salisbury, C.; Bloom, J.; Freitag, M.; Glynn, L.; Moth, C.; Balderas, J.M. Prevalence, determinants and patterns of multimorbidity in primary care: A systematic review of observational studies. PLoS ONE 2014, 9, e102149. [Google Scholar] [CrossRef] [PubMed]
- Lai, S.; Gao, J.; Zhou, Z.; Yang, X.; Xu, Y.; Zhou, Z.; Chen, G. Prevalence’s and trends of chronic diseases in Shaanxi Province, China: Evidence from representative cross-sectional surveys in 2003, 2008 and 2013. PLoS ONE 2018, 13, e0202886. [Google Scholar] [CrossRef] [PubMed]
- Nunes, B.P.; Filho, A.D.P.C.; Pati, S.; Teixeira, D.S.C.; Flores, T.R.; Camargo-Figuera, F.A.; Munhoz, T.; Thumé, E.; A Facchini, L.; Batista, S.R. Contextual and individual inequalities of multimorbidity in Brazilian adults: A cross-sectional national-based study. BMJ Open 2017, 7, e015885. [Google Scholar] [CrossRef]
- De Carvalho, J.N.; Roncalli, Â.G.; Cancela, M.D.C.; De Souza, D.L.B. Prevalence of multimorbidity in the Brazilian adult population according to socioeconomic and demographic characteristics. PLoS ONE 2017, 12, e0174322. [Google Scholar] [CrossRef] [PubMed]

| Score | BMI | Total Physical Activity | Alcohol Consumption | Smoking Status | Sleep Quality |
|---|---|---|---|---|---|
| 0 (poor) | ≥25 | no | ≥8 dose/week for women or ≥15 dose/week for men | Current smokers | PSQI score > 5 |
| 1 (intermediate) | 23–24.9 | <150 min | no | Former smokers | PSQI score ≤ 5 |
| 2 (optimal) | <23 | ≥150 min | 1–7 dose/week for women or 1–14 dose/week for men | Never | - |
| Total score | 0–9 |
| Overall | Stratified by Multimorbidity Status | Effect Size a | p-Value b | ||
|---|---|---|---|---|---|
| No | Yes | ||||
| No. of participants | 1443 | 1294 | 149 | ||
| Baseline characteristics | |||||
| Gender, n (%) | 0.01 | 0.755 | |||
| Men | 646 (44.8) | 577 (44.6) | 69 (46.3) | ||
| Women | 797 (55.2) | 717 (55.4) | 80 (53.7) | ||
| Age group, n (%) | 0.35 | <0.001 | |||
| Young Adult (18–44) | 696 (48.2) | 682 (52.7) | 14 (9.4) | ||
| Middle Age (45–64) | 555 (38.5) | 487 (37.6) | 68 (45.6) | ||
| Elderly (≥65) | 192 (13.3) | 125 (9.7) | 67 (45.0) | ||
| Educational Level, n (%) | 0.25 | <0.001 | |||
| Primary or lower | 280 (19.4) | 210 (16.2) | 70 (47.0) | ||
| Secondary | 723 (50.1) | 658 (50.9) | 65 (43.6) | ||
| Tertiary or above | 440 (30.5) | 426 (32.9) | 14 (9.4) | ||
| Marital status, n (%) | 0.11 | <0.001 | |||
| Single | 540 (37.4) | 508 (39.3) | 32 (21.5) | ||
| Couple | 903 (62.6) | 786 (60.7) | 117 (78.5) | ||
| Employment status, n (%) | 0.29 | <0.001 | |||
| Employed | 1042 (72.2) | 978 (75.6) | 64 (43.0) | ||
| Unemployed | 176 (12.2) | 161 (12.4) | 15 (10.1) | ||
| Retired/Housewife | 225 (15.6) | 155 (12.0) | 70 (47.0) | ||
| Monthly family income, n (%) | 0.03 | 0.778 | |||
| $29,999 or less | 718 (49.8) | 642 (49.6) | 76 (51.0) | ||
| $30,000–$59,999 | 394 (27.3) | 353 (27.3) | 41 (27.5) | ||
| $60,000 or more | 108 (7.5) | 100 (7.7) | 8 (5.4) | ||
| Unknown | 223 (15.5) | 199 (15.4) | 24 (16.1) | ||
| Lifestyle characteristics | |||||
| BMI category, n (%) | 0.20 | <0.001 | |||
| Underweight/Normal weight (<23.0 kg/m2) | 873 (60.5) | 823 (63.6) | 50 (33.6) | ||
| Overweight (23–24.9 kg/m2) | 283 (19.6) | 244 (18.9) | 39 (26.2) | ||
| Obesity (≥25 kg/m2) | 287 (19.9) | 227 (17.5) | 60 (40.3) | ||
| VPA Weekly, n (%) | 0.06 | 0.03 | |||
| Not enough (<75 min) | 1157 (80.2) | 1027 (79.4) | 130 (87.2) | ||
| Enough (≥75 min) | 286 (19.8) | 267 (20.6) | 19 (12.8) | ||
| MPA Weekly, n (%) | 0.02 | 0.43 | |||
| Not enough (<150 min) | 1141 (79.1) | 1019 (78.7) | 122 (81.9) | ||
| Enough (≥150 min) | 302 (20.9) | 275 (21.3) | 27 (18.1) | ||
| TOPA Weekly, n (%) | 0.06 | 0.03 | |||
| Not enough (<150 min) | 989 (68.5) | 875 (67.6) | 114 (76.5) | ||
| Enough (≥150 min) | 454 (31.5) | 419 (32.4) | 35 (23.5) | ||
| Drinking status, n (%) | 0.11 | <0.001 | |||
| Never | 981 (68.0) | 890 (68.8) | 91 (61.1) | ||
| Quitted | 97 (6.7) | 75 (5.8) | 22 (14.8) | ||
| Yes | 365 (25.3) | 329 (25.4) | 36 (24.2) | ||
| Smoking, n (%) | 0.11 | <0.001 | |||
| Never | 1200 (83.2) | 1090 (84.2) | 110 (73.8) | ||
| Quitted | 127 (8.8) | 100 (7.7) | 27 (18.1) | ||
| Yes | 116 (8.0) | 104 (8.0) | 12 (8.1) | ||
| Sleep quality, n (%) | 0.09 | 0.001 | |||
| Optimal (PSQI score ≤ 5) | 977 (67.7) | 934 (69.1) | 1337 (55.7) | ||
| Poor/Insomnia (PSQI score > 5) | 466 (32.3) | 400 (30.9) | 66 (44.3) | ||
| Lifestyle score, mean (SD) | 6.09 (1.56) | 6.19 (1.52) | 5.17 (1.57) | 0.67 | <0.001 |
| Lifestyle Characteristics | Multimorbidity, Cases (%) | Model 1 | Model 2 | ||
|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | ||
| Model 2a | |||||
| BMI category | |||||
| Underweight/Normal weight (<23.0 kg/m2) | 50 (5.7) | Ref | - | Ref | - |
| Overweight (23–24.9 kg/m2) | 39 (13.8) | 2.63 (1.69, 4.09) | <0.001 | 1.95 (1.18, 3.20) | 0.009 |
| Obesity (≥25 kg/m2) | 60 (20.9) | 4.35 (2.91, 6.51) | <0.001 | 3.76 (2.38, 5.96) | <0.001 |
| VPA Weekly | |||||
| Not enough (<75 min) | 130 (11.2) | Ref | - | Ref | - |
| Enough (≥75 min) | 19 (6.6) | 0.56 (0.34, 0.93) | 0.02 | 0.83 (0.44, 1.54) | 0.55 |
| MPA Weekly | |||||
| Not enough (<150 min) | 122 (10.7) | Ref | - | Ref | - |
| Enough (≥150 min) | 27 (8.9) | 0.82 (0.53, 1.27) | 0.37 | 1.00 (0.58, 1.74) | 0.99 |
| Drinking status | |||||
| Never | 91 (9.3) | Ref | - | Ref | - |
| Quit | 22 (22.7) | 2.87 (1.70, 4.83) | <0.001 | 2.43 (1.26, 4.69) | 0.008 |
| Yes | 36 (9.9) | 1.07 (0.71, 1.61) | 0.74 | 1.36 (0.81, 2.26) | 0.24 |
| Smoking status | |||||
| Never | 110 (9.2) | Ref | - | Ref | - |
| Quit | 27 (21.3) | 2.68 (1.68, 4.27) | <0.001 | 1.16 (0.64, 2.09) | 0.63 |
| Yes | 12 (10.3) | 1.14 (0.61, 2.14) | 0.68 | 0.74 (0.34, 1.62) | 0.46 |
| Sleep quality | |||||
| Optimal (PSQI score ≤ 5) | 83 (8.5) | Ref | - | Ref | - |
| Poor/Insomnia (PSQI score > 5) | 66 (14.2) | 1.78 (1.26, 2.51) | 0.001 | 2.25 (1.49, 3.40) | <0.001 |
| Model 2b | |||||
| Lifestyle score | - | 0.64 (0.57, 0.72) | <0.001 | 0.67 (0.59, 0.77) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Q.; Zhang, Q.; Ngai, F.W.; Wang, S.; Zhang, D.; Gao, Y.; Hao, C.; Wang, H.H.; Nogueira, O.C.B.L.; Liu, M.; et al. The Multimorbidity and Lifestyle Correlates in Chinese Population Residing in Macau: Findings from a Community-Based Needs Assessment Study. Healthcare 2023, 11, 1906. https://doi.org/10.3390/healthcare11131906
Yang Q, Zhang Q, Ngai FW, Wang S, Zhang D, Gao Y, Hao C, Wang HH, Nogueira OCBL, Liu M, et al. The Multimorbidity and Lifestyle Correlates in Chinese Population Residing in Macau: Findings from a Community-Based Needs Assessment Study. Healthcare. 2023; 11(13):1906. https://doi.org/10.3390/healthcare11131906
Chicago/Turabian StyleYang, Qingling, Quanzhi Zhang, Fei Wan Ngai, Shaoling Wang, Dexing Zhang, Yang Gao, Chun Hao, Harry Haoxiang Wang, Oi Ching Bernice Lam Nogueira, Ming Liu, and et al. 2023. "The Multimorbidity and Lifestyle Correlates in Chinese Population Residing in Macau: Findings from a Community-Based Needs Assessment Study" Healthcare 11, no. 13: 1906. https://doi.org/10.3390/healthcare11131906
APA StyleYang, Q., Zhang, Q., Ngai, F. W., Wang, S., Zhang, D., Gao, Y., Hao, C., Wang, H. H., Nogueira, O. C. B. L., Liu, M., Molasiotis, A., Loke, A., & Xie, Y. (2023). The Multimorbidity and Lifestyle Correlates in Chinese Population Residing in Macau: Findings from a Community-Based Needs Assessment Study. Healthcare, 11(13), 1906. https://doi.org/10.3390/healthcare11131906










