Measuring Knowledge of Healthcare Providers on Pediatric Palliative Care with an Online Questionnaire Based on the National Core Curriculum in Italy
Abstract
1. Introduction
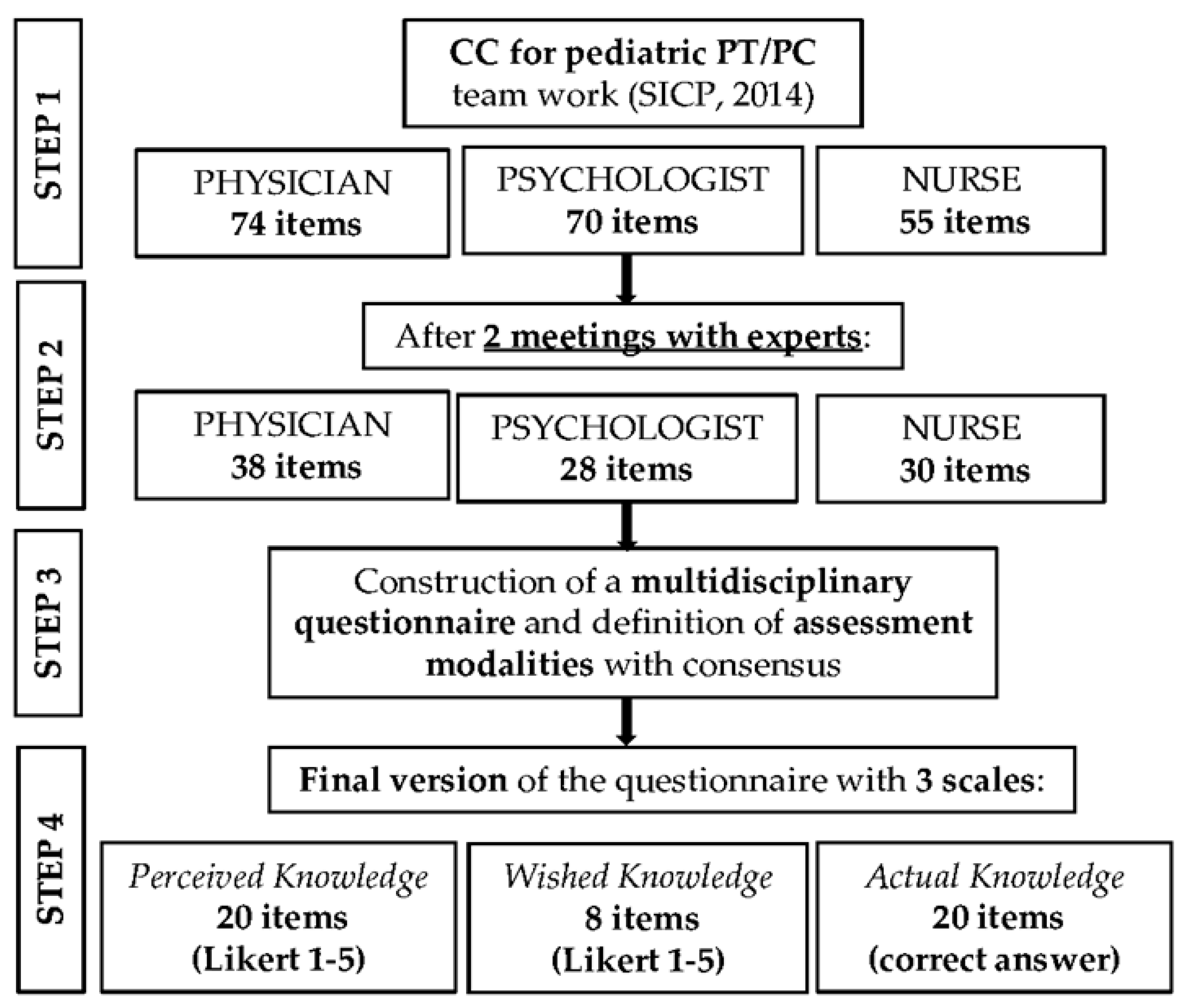
2. Materials and Methods
3. Results
3.1. Sample
3.2. Exploratory Factor Analysis (EFA)
3.3. Levels of Perceived, Wished and Actual Knowledge
4. Discussion
5. Study Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- van der Lee, J.H.; Mokkink, L.B. Definitions and measurement of chronic health conditions in childhood: A systematic review. JAMA 2007, 297, 2741–2751. [Google Scholar] [CrossRef]
- Jankovic, M.; De Zen, L. A consensus conference report on defining the eligibility criteria for pediatric palliative care in Italy. Ital. J. Pediatr. 2019, 45, 89. [Google Scholar] [CrossRef]
- Connor, S.R.; Downing, J. Estimating the Global Need for Palliative Care for Children: A Cross-sectional Analysis. J. Pain Symptom Manag. 2016, 53, 171–177. [Google Scholar] [CrossRef]
- Benini, F.; Bellentani, M. An estimation of the number of children requiring pediatric palliative care in Italy. Ital. J. Pediatr. 2021, 47, 4. [Google Scholar] [CrossRef] [PubMed]
- Rapoport, A.; Obwanga, C. Not just little adults: Palliative care physician attitudes toward pediatric patients. J. Palliat. Med. 2013, 16, 675–679. [Google Scholar] [CrossRef] [PubMed]
- Detsyk, O.Z.; Zolotarova, Z.M. Awareness of pediatric palliative care among healthcare workers. Wiad. Lek. 2018, 71 Pt 1, 574–578. [Google Scholar]
- Spruit, J.L.; Bell, C.J. Knowledge, Beliefs, and Behaviors Related to Palliative Care Delivery Among Pediatric Oncology Health Care Providers. J. Pediatr. Oncol. Nurs. 2018, 35, 247–256. [Google Scholar] [CrossRef]
- Stenekes, S.; Penner, J.L. Development and Implementation of a Survey to Assess Health-Care Provider’s Competency, Attitudes, and Knowledge About Perinatal Palliative Care. J. Palliat. Care 2018, 34, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Moya-Dionisio, V. Knowledge of primary care pediatricians about pediatric palliative care in the Principality of Asturias, Spain. Boletín Med. Hosp. Infant. Mex. 2020, 77, 195–201. [Google Scholar] [CrossRef]
- Rost, M.; De Clercq, E. Barriers to Palliative Care in Pediatric Oncology in Switzerland: A Focus Group Study. J. Pediatr. Oncol. Nurs. 2019, 37, 35–45. [Google Scholar] [CrossRef]
- World Health Organization. Worldwide Palliative Care Alliance. Global Atlas of Palliative Care at the End of Life. 2014. Available online: https://cdn.who.int/media/docs/default-source/integrated-health-services-(ihs)/csy/palliative-care/whpca_global_atlas_p5_digital_final.pdf?sfvrsn=1b54423a_3 (accessed on 10 January 2022).
- Law 15 March 2010 n. 38. Disposizioni per Garantire L’accesso Alle cure Palliative e alla Terapia del Dolore. Gazzetta Ufficiale, 19 March 2010, N. 65. Available online: https://www.gazzettaufficiale.it/gunewsletter/dettaglio.jsp?service=1&datagu=2010-03-19&task=dettaglio&numgu=65&redaz=010G0056&tmstp=1269600292070 (accessed on 11 January 2022).
- Ministry of Health. Law 15 March 2010 N. 38 and Implementing Measures-Collection of Legislation. 31 December 2020. Available online: https://www.salute.gov.it/imgs/C_17_pubblicazioni_3046_allegato.pdf (accessed on 11 January 2022).
- Ferrell, B.; Connor, R.S. The national agenda for quality palliative care: The National Consensus Project and the National Quality Forum. J. Pain Symptom Manag. 2007, 33, 737–744. [Google Scholar] [CrossRef] [PubMed]
- Italian Society of Palliative Care SICP. Il Core Curriculum in Terapia del Dolore e Cure Palliative Pediatriche—Il Lavoro in équipe—Curriculum del Medico, Dell’infermiere e dello Psicologo. 2014. Available online: https://www.sicp.it/wp-content/uploads/2018/12/10_CCCPP_BassaPerVisione_v2.pdf (accessed on 11 January 2022).
- Benini, F.; Cauzzo, C. Training in pediatric palliative care in Italy: Still much to do. Ann. Ist. Super. Sanita 2019, 55, 240–245. [Google Scholar] [CrossRef]
- Brock, K.E.; Cohen, H.J. Reliability and Validity of the Pediatric Palliative Care Questionnaire for Measuring Self-Efficacy, Knowledge, and Adequacy of Prior Medical Education among Pediatric Fellows. J. Palliat. Med. 2015, 18, 842–848. [Google Scholar] [CrossRef]
- Ashley, J.L.; Fasolino, T.K. Palliative and Hospice Care: Educational Needs of Inpatient Registered Nurses. Creat. Nurs. 2016, 22, 114–120. [Google Scholar] [CrossRef]
- Bradford, N.K.; Greenslade, R. Educational Needs of Health Professionals Caring for Adolescents and Young Adults with Cancer. J. Adolesc. Young Adult Oncol. 2018, 7, 298–305. [Google Scholar] [CrossRef]
- Artino, A.R., Jr.; La Rochelle, J.S. Developing questionnaires for educational research: AMEE Guide No. 87. Med. Teach. 2014, 36, 463–474. [Google Scholar] [CrossRef] [PubMed]
- Schuwirth, L.; Van der Vleuten, C. Written assessments. In A Practical Guide for Medical Teachers; Dent, J.A., Harden, R.M., Eds.; Churchill Livingstone: London, UK, 2013; pp. 299–306. [Google Scholar]
- Gorsuch, R. L Factor Analysis, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1983. [Google Scholar]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, H.F. The Application of Electronic Computers to Factor Analysis. Educ. Psychol. Meas. 1960, 20, 141–151. [Google Scholar] [CrossRef]
- Stevens, J. Applied Multivariate Statistics for the Social Sciences, 2nd ed.; Lawrence Erlbaum Associates, Inc.: Mahwah, NJ, USA, 1992. [Google Scholar]
- Schulman-Green, D.; Ercolano, E. Developing and testing a web-based survey to assess educational needs of palliative and end-of-life health care professionals in Connecticut. Am. J. Hosp. Palliat. Med. 2010, 28, 219–229. [Google Scholar] [CrossRef]
- Lazenby, M.; Ercolano, E. Validity of the end-of-life professional caregiver survey to assess for multidisciplinary educational needs. J. Palliat. Med. 2012, 15, 427–431. [Google Scholar] [CrossRef]
- O’Shea, E.R.; Lavallee, M. Assessing Palliative and End-of-Life Educational Needs of Pediatric Health Care Professionals: Results of a Statewide Survey. J. Hosp. Palliat. Nurs. 2017, 19, 468–473. [Google Scholar] [CrossRef]
- Amery, J. Mapping children’s palliative care around the world: An online survey of children’s palliative care services and professionals’ educational needs. J. Palliat. Med. 2012, 15, 646–652. [Google Scholar] [CrossRef]
- Amery, J.M.; Rose, C.J. A study into the children’s palliative care educational needs of health professionals in Uganda. J. Palliat. Med. 2010, 13, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Luft, J.; Ingham, H. The JoHari window, a graphic model of interpersonal awareness. In Proceedings of the Western Training Laboratory in Group Development; UCLA: Los Angeles, CA, USA, 1955. [Google Scholar]
- Knowles, M. The Adult Learner: A Neglected Species; Gulf: Houston, TX, USA, 1988. [Google Scholar]
- Taylor, D.C.M.; Hamdy, H. Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83. Med. Teach. 2013, 35, e1561–e1572. [Google Scholar] [CrossRef] [PubMed]
- Postier, C.A.; Wolfe, J. Education in Palliative and End-of-Life Care-Pediatrics: Curriculum Use and Dissemination. J. Pain Symptom Manag. 2021, 63, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Braithwaite, D.; Emery, J. Using the Internet to conduct surveys of health professionals: A valid alternative? Fam. Pract. 2003, 20, 545–551. [Google Scholar] [CrossRef]
- Lusk, C.; Delclos, G.L. Mail Versus Internet Surveys: Determinants of Method of Response Preferences among Health Professionals. Eval. Health Prof. 2007, 30, 186–201. [Google Scholar] [CrossRef]
- Audibert, C.; Glass, D. Method and transparency of online physician surveys: An overview. Surv. Methods Insights Field 2020. [Google Scholar] [CrossRef]
| Socio-Demographic Variables | N = 105 | Physician N = 31 | Nurse N = 56 | Psychologist N = 15 | Other N = 3 | p-Value |
|---|---|---|---|---|---|---|
| Gender, N (%) | 0.294 | |||||
| Male | 15 (14.3) | 8 (25.0) | 6 (10.9) | 1 (6.7) | 0 | |
| Female | 90 (85.7) | 24 (75.0) | 49 (89.1) | 14 (93.3) | 3 (100) | |
| Age class, N (%) | 0.236 | |||||
| ≤30 | 12 (11.4) | 1 (3.1) | 8 (14.6) | 3 (20.0) | 0 | |
| 31–45 | 36 (34.3) | 12 (37.5) | 18 (32.7) | 6 (40.0) | 0 | |
| 46–60 | 49 (46.7) | 14 (43.8) | 27 (49.1) | 5 (33.3) | 3 (100.0) | |
| ≥61 | 8 (7.6) | 5 (14.6) | 2 (3.6) | 1 (6.7) | 0 | |
| Amount of work with pediatric patients, N (%) | 0.027 ** | |||||
| None | 19 (18.1) | 1 (3.1) | 12 (21.8) | 5 (33.3) | 0 | |
| <50% | 15 (14.3) | 3 (9.4) | 10 (18.2) | 2 (13.3) | 0 | |
| >50% and <100% | 17 (16.2) | 4 (12.5) | 8 (14.6) | 4 (26.7) | 1 (33.3) | |
| 100% | 54 (51.4) | 24 (75.0) | 25 (45.4) | 4 (26.7) | 2 (66.7) | |
| Primary work setting, N (%) | <0.001 ** | |||||
| Hospital | 57 (54.3) | 16 (50.0) | 34 (61.8) | 6 (40.0) | 1 (33.3) | |
| Community | 21 (20.0) | 0 | 15 (27.3) | 4 (26.7) | 2 (66.7) | |
| Hospital and Community | 6 (5.7) | 1 (3.1) | 2 (3.6) | 3 (20.0) | 0 | |
| Other | 21 (20.0) | 15 (46.9) | 4 (7.3) | 2 (13.3) | 0 | |
| Length of service experience, N (%) | 0.299 | |||||
| <5 years | 19 (18.1) | 6 (18.7) | 4 (7.3) | 2 (13.3) | 0 | |
| 5–10 years | 12 (11.4) | 6 (18.7) | 8 (14.5) | 5 (33.3) | 0 | |
| >10 years | 74 (70.5) | 20 (62.6) | 43 (78.2) | 8 (53.4) | 3 (100.0) | |
| Prior education on PC/PPC, N (%) | 0.675 | |||||
| None | 35 (33.3) | 13 (40.6) | 16 (29.1) | 4 (26.7) | 2 (66.7) | |
| Congresses/seminars | 63 (60.0) | 18 (56.3) | 35 (63.7) | 9 (59.9) | 1 (33.3) | |
| Advanced courses in PC or PPC (with or without congresses/seminars) | 3 (2.9) | 0 | 2 (3.6) | 1 (6.7) | 0 | |
| Master in PC (with or without congresses/seminars/advanced courses) | 4 (3.8) | 1 (3.1) | 2 (3.6) | 1 (6.7) | 0 | |
| Prior work experience in PC/PPC, N (%) | 0.096 * | |||||
| None | 62 (59.1) | 2 (6.2) | 3 (5.4) | 5 (33.3)) | 0 | |
| Only PC | 18 (17.1) | 20 (62.5) | 33 (60.0) | 6 (40.1) | 3 (100.0) | |
| Only PPC | 15 (14.3) | 3 (9.4) | 13 (23.6) | 2 (13.3) | 0 | |
| Both | 10 (9.5) | 7 (21.9) | 6 (10.9) | 2 (13.3) | 0 |
| Scale/Item | Score | Factors | |||
|---|---|---|---|---|---|
| Perceived Knowledge | Median (IQR) | Basic Concepts | Policies and Protocols | Communication with Child and Families | Transitional Care |
| Clinical and healthcare needs in PPC/PT | 3 (2–3) | 0.40 | |||
| QOL in PPC/PT | 3 (2–4) | 0.55 | |||
| Personalized care and QOL | 3 (2–3) | 0.56 | |||
| Psychosocial needs in the EOL | 3 (2–3) | 0.67 | |||
| Clinical issues in the EOL | 3 (2–3) | 0.50 | |||
| Ethical dilemmas | 3 (2–3) | 0.85 | |||
| Mourning | 3 (2–4) | 0.96 | |||
| PPC/PT Definition/Philosophy | 3 (2–3) | 0.75 | |||
| PPC/PT Regulatory Framework | 2 (1–3) | 0.68 | |||
| PPC/PT Ethics/Deontology | 2 (2–3) | 0.60 | |||
| PPC/PT Eligibility criteria | 2 (1–3) | 0.47 | |||
| Pain assessment | 4 (3–4) | 0.70 | |||
| PT/PPC Healthcare pathways | 2 (2–3) | 0.65 | |||
| Pain management | 3 (2–4) | 0.62 | |||
| Child’s information right | 3 (2–4) | 0.68 | |||
| Communication with child | 3 (2–4) | 0.99 | |||
| Communication with family | 3 (2–4) | 0.81 | |||
| Child/family’s needs assessment | 3 (2–4) | 0.83 | |||
| Continuity of care | 3 (2–4) | 0.81 | |||
| Children–adult services transition | 2 (2–3) | 0.90 | |||
| Eigenvalues | 10.76 | 1.76 | 1.35 | 1.11 | |
| Cronbach’s Alpha by Factor | 0.90 | 0.93 | 0.89 | 0.75 | |
| Average Cronbach’s Alpha | 0.95 | ||||
| Wished Knowledge | Median (IQR) | Desired training | - | - | - |
| Evaluation for PPC/PT network access | 4 (3–4) | 0.86 | |||
| Reception in PPC/PT network | 4 (3–5) | 0.91 | |||
| Charge in PPC/PT network settings | 4 (3–4) | 0.89 | |||
| Team work | 4 (3–5) | 0.84 | |||
| Management of self | 4 (3–5) | 0.83 | |||
| PPC/PT Reference center management | 3.5 (3–4) | 0.80 | |||
| Training on PPC/PT | 4 (3–5) | 0.84 | |||
| Research on PPC/PT | 3 (2–4) | 0.86 | |||
| Eigenvalues | 5.87 | ||||
| Cronbach’s Alpha of the Factor | 0.94 | ||||
| Actual Knowledge | N (%) | Basic concepts | Policies and protocols | EOL issues | Family- centered Care |
| Pathologies for PPC/PT | 48 (47.1) | 0.53 | |||
| Child’s information right | 81 (79.4) | 0.87 | |||
| Continuity of care | 99 (97.1) | 0.64 | |||
| PPC/PT Regulatory framework | 69 (67.7) | 0.64 | |||
| Buckman Protocol | 62 (60.8) | 0.71 | |||
| Palliative vs. terminal sedation | 70 (68.3) | 0.62 | |||
| Mourning | 60 (58.8) | 0.71 | |||
| EOL symptoms | 58 (56.9) | 0.62 | |||
| Family’s multi-professional care | 86 (84.3) | 0.84 | |||
| Eigenvalues | 1.56 | 1.41 | 1.37 | 1.18 | |
| Scale/Item Text | Total | Physicians | Nurses | Psychologists | ||
|---|---|---|---|---|---|---|
| Perceived Knowledge | Factor | Median (IQR) | p-Value | |||
| Clinical and healthcare needs in PT/PPC | Basic concepts | 3 (2–3) | 2.5 (2–3) | 2 (2–3) | 3 (1–4) | 0.430 |
| QOL in PT/PPC | Basic concepts | 3 (2–4) | 3 (2–4) | 3 (2–3) | 4 (2–5) | 0.116 |
| Personalized care and QOL | Basic concepts | 3 (2–3) | 3 (2–3) | 3 (2–3) | 4 (2–5) | 0.248 |
| Psychosocial needs in the EOL | Basic concepts | 3 (2–3) | 2.5 (2.3) | 2 (2–3) | 4 (2–4) | 0.006 ** |
| Clinical issues in the EOL | Basic concepts | 3 (2–3) | 2.5 (2–3) | 3 (2–4) | 3 (2–4) | 0.342 |
| Ethical dilemmas | Basic concepts | 3 (2–3) | 3 (2–3) | 3 (2–3) | 3 (2–4) | 0.379 |
| Mourning | Basic concepts | 3 (2–4) | 2.5 (1.0) | 2.7 (1.2) | 3.7 (1.0) | 0.003 ** |
| PPC/PT Definition/Philosophy | Policies and protocols | 3 (2–3) | 3 (2–3) | 3 (2–3) | 3 (2–3) | 0.596 |
| PPC/PT Regulatory framework | Policies and protocols | 2 (1–3) | 2 (1.5–3) | 2 (1–3) | 3 (1–4) | 0.315 |
| PPC/PT Ethics/Deontology | Policies and protocols | 2 (2–3) | 2.5 (2–3) | 2 (2–3) | 3 (2–4) | 0.049 ** |
| PPC/PT eligibility criteria | Policies and protocols | 2 (1–3) | 2 (1–3) | 2 (1–3) | 3 (1–3) | 0.355 |
| Pain assessment | Policies and protocols | 4 (3–4) | 3.5 (3–4) | 4 (3–4) | 3 (2–4) | 0.273 |
| PPC/PT Healthcare pathways | Policies and protocols | 2 (2–3) | 2 (2–3) | 3 (1–3) | 2 (2–4) | 0.658 |
| Pain management | Policies and protocols | 3 (2–4) | 2 (3–4) | 3 (3–4) | 3 (1–4) | 0.294 |
| Child’s information right | Communication with child and family | 3 (2–4) | 3 (2–4) | 3 (2–3) | 4 (2–5) | 0.140 |
| Communication with child | Communication with child and family | 3 (2–4) | 3 (2–4) | 3 (2–4) | 4 (2–4) | 0.293 |
| Communication with family | Communication with child and family | 3 (2–4) | 3 (2–4) | 3 (2–4) | 4 (3–5) | 0.171 |
| Child/family’s needs assessment | Communication with child and family | 3 (2–4) | 3 (2–3) | 3 (2–3) | 4 (2–5) | 0.189 |
| Continuity of care | Transitional Care | 3 (2–4) | 3 (2–3) | 3 (2–4) | 3 (2–4) | 0.806 |
| Children–adult services transition | Transitional Care | 2 (2–3) | 2 (2–3) | 2 (1–3) | 2 (2–3) | 0.976 |
| Total score | 52 (44–66) | 54 (42–60) | 51 (44–65) | 67 (35–80) | 0.341 | |
| Wished Knowledge | Factor | Median (IQR) | p-value | |||
| Evaluation for PPC/PT network access | Desired training | 4 (3–4) | 4 (3–4) | 4 (3–5) | 4 (3–4) | 0.460 |
| Reception in the PPC/PT network | Desired training | 4 (3–5) | 3 (3–4) | 4 (3–5) | 4 (3–5) | 0.364 |
| Charge in the PPC/PT network settings | Desired training | 4 (3–4) | 4 (3–4) | 4 (3–5) | 4 (3–5) | 0.388 |
| Team work | Desired training | 4 (3–5) | 4 (3–5) | 4 (3–5) | 4 (3–5) | 0.904 |
| Management of self | Desired training | 4 (3–5) | 3.5 (3–4) | 4 (3–5) | 4 (2–5) | 0.943 |
| PPC/PT Reference center management | Desired training | 3.5 (3–4) | 3 (2–4) | 4 (3–5) | 4 (3–5) | 0.117 |
| Training on PPC/PT | Desired training | 4 (3–5) | 3 (3–4) | 4 (3–5) | 3 (2–4) | 0.155 |
| Research on PPC/PT | Desired training | 3 (2–4) | 3 (2–3) | 4 (2–4) | 3 (2–4) | 0.150 |
| Total score | 28.5 (24–34) | 27 (23.5–31.5) | 31 (25–37) | 27 (23–34) | 0.247 | |
| Total | Physicians | Nurses | Psychologists | ||||
|---|---|---|---|---|---|---|---|
| Actual Knowledge | Factor | DP | N (%) | p-Value | |||
| Pathologies for PPC/PT | Basic concepts | 1.00 | 48 (47.1) | 15 (46.9) | 20 (36.4) | 13 (86.7) | 0.002 * |
| Child’s information right | Basic concepts | 0.65 | 81 (79.4) | 24 (75.0) | 43 (78.2) | 14 (93.3) | 0.327 |
| Continuity of care | Basic concepts | 0.11 | 99 (97.1) | 31 (96.9) | 53 (96.4) | 15 (100.0) | 1 |
| PPC/PT Regulatory framework | Policies and protocols | 0.88 | 69 (67.7) | 18 (56.3) | 39 (70.9) | 12 (80.0) | 0.242 |
| Buckman protocol | Policies and protocols | 0.95 | 62 (60.8) | 17 (53.1) | 34 (61.8) | 11 (73.3) | 0.425 |
| Palliative vs. terminal sedation | Policies and protocols | 0.86 | 70 (68.3) | 24 (75.0) | 35 (63.6) | 11 (73.3) | 0.51 |
| Mourning | EOL issues | 0.97 | 60 (58.8) | 22 (68.8) | 32 (58.2) | 6 (40.0) | 0.178 |
| EOL symptoms | EOL issues | 0.98 | 58 (56.9) | 18 (56.3) | 32 (58.2) | 8 (53.3) | 0.962 |
| Family’s multi-professional care | Family-centered care | 0.53 | 86 (84.3) | 23 (71.9) | 51 (92.7) | 12 (80.0) | 0.023 ** |
| Total score | 6 (5–7) | 6 (4–7) | 6 (5–7) | 7 (6–8) | 0.020 ** | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zanello, E.; Vecchi, R.; Zamagni, G.; Biagi, M.C.; Bruno, I.; Cragnolin, E.; Danielli, E.; Paoletti, S.; Rabusin, M.; Ronfani, L.; et al. Measuring Knowledge of Healthcare Providers on Pediatric Palliative Care with an Online Questionnaire Based on the National Core Curriculum in Italy. Healthcare 2023, 11, 1971. https://doi.org/10.3390/healthcare11131971
Zanello E, Vecchi R, Zamagni G, Biagi MC, Bruno I, Cragnolin E, Danielli E, Paoletti S, Rabusin M, Ronfani L, et al. Measuring Knowledge of Healthcare Providers on Pediatric Palliative Care with an Online Questionnaire Based on the National Core Curriculum in Italy. Healthcare. 2023; 11(13):1971. https://doi.org/10.3390/healthcare11131971
Chicago/Turabian StyleZanello, Elisa, Roberta Vecchi, Giulia Zamagni, Maria Celeste Biagi, Irene Bruno, Elisa Cragnolin, Elisabetta Danielli, Silvia Paoletti, Marco Rabusin, Luca Ronfani, and et al. 2023. "Measuring Knowledge of Healthcare Providers on Pediatric Palliative Care with an Online Questionnaire Based on the National Core Curriculum in Italy" Healthcare 11, no. 13: 1971. https://doi.org/10.3390/healthcare11131971
APA StyleZanello, E., Vecchi, R., Zamagni, G., Biagi, M. C., Bruno, I., Cragnolin, E., Danielli, E., Paoletti, S., Rabusin, M., Ronfani, L., & Pessa Valente, E. (2023). Measuring Knowledge of Healthcare Providers on Pediatric Palliative Care with an Online Questionnaire Based on the National Core Curriculum in Italy. Healthcare, 11(13), 1971. https://doi.org/10.3390/healthcare11131971





