Excessive Noise in Neonatal Units and the Occupational Stress Experienced by Healthcare Professionals: An Assessment of Burnout and Measurement of Cortisol Levels
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Procedures
2.2.1. Sociodemographic and Work Conditions
2.2.2. Self-Perception of Burnout
2.2.3. Salivary Cortisol
2.2.4. Environmental Noise Measurements
- -
- LAeq,T is the A-weighted equivalent continuous sound pressure level integrated over a time T at the point evaluated;
- -
- T represents the total time evaluated in seconds;
- -
- m represents each measurement performed per second (LAeq,1s);
- -
- n is the total number of measurements.
2.2.5. Statistical Analysis
2.2.6. Ethical Approval
3. Results
3.1. Subjects’ Sociodemographic Characteristics
3.2. Health Professionals’ Work Conditions, Salivary Cortisol and Subjective Stress
3.3. Environmental Noise Measurements
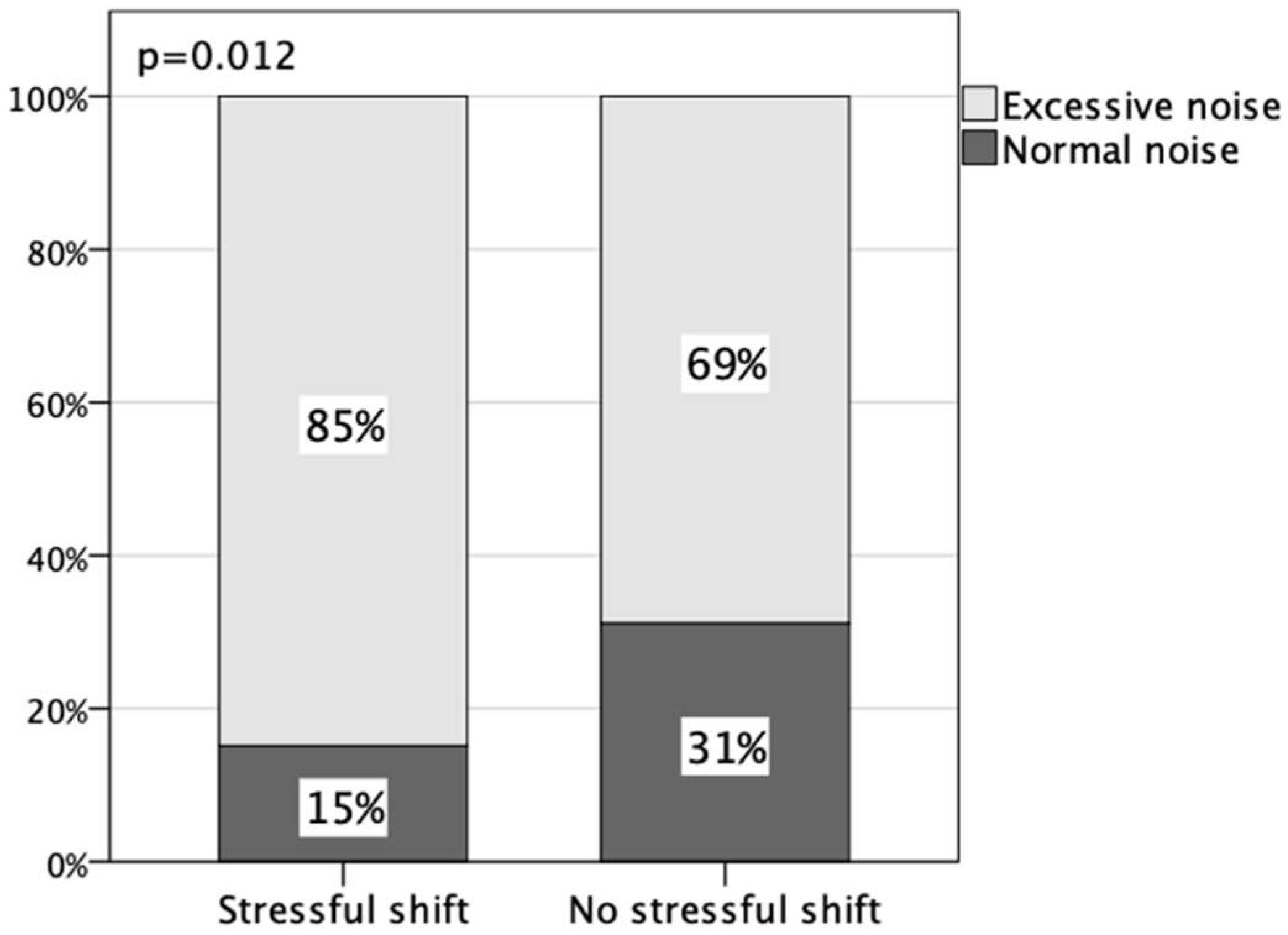
3.4. Factors Associated with Exposure to Noise Levels and Stress
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- de Souza, V.S.; da Silva, D.S.; Lima, L.V.; Teston, E.F.; Benedetti, G.M.d.S.; Costa, M.A.R.; Mendonça, R.R. Quality of life of nursing professionals working in critical sectors. Rev. Cuid. 2018, 9, 2177–2186. [Google Scholar] [CrossRef]
- Browne, J.; Cicco, R.; Dunn, M.S.; Graven, S.N.; Gregory, S.; Harrell, J.W.; Jaeger, C.B.; Johnson, B.H.; King, J.D. Recommended standards for newborn ICU design, eighth edition Consensus committee on recommended design standards for advanced neonatal care. J. Perinatol. 2013, 33, 2–16. [Google Scholar] [CrossRef]
- Teixeira, L.B.; Veloso, L.U.P.; Ribeiro, Í.A.P.; de Oliveira, T.N.; Cortez, A.C.L. Estresse ocupacional na enfermagem atuante na unidade de terapia intensiva. Investig. En Enfermería Imagen Y Desarro. 2017, 19, 195. [Google Scholar] [CrossRef]
- Campos, M.d.S.; Esteves, T.M.d.S.; de Oliveira, V.A.S.C.; Garcia, J.R. O Estresse ocupacional no enfermeiro na Unidade de Terapia Intensiva. Rev. Eletrônica E-F@Tec 2018, 8, 1–9. [Google Scholar]
- Pereira, A.; Santos, A.; Ribeiro, A.; Santos, C.; Pereira, D.; Sousa, D.; Pereira, E.; Peiemntel, E.; Santos, J. Fatores geradores de estresse atuam na linha de frente do COVID-19: Dos profissionais de enfermagem que ocupacional e seus impactos na saúde uma revisão bibliográfica. In Enfermagem: Desafios E Perspectivas Para a Integralidade Do Cuidado; da Silva, P.F., de Sousa, L.C., Eds.; Editora Científica Digital: São Paulo, Brasil, 2021; pp. 191–212. ISBN 9786589826828. Available online: www.editoracientifica.org (accessed on 22 October 2022).
- Aita, M.; Héon, M.; Lavallée, A.; De Clifford Faugère, G.; Altit, G.; Le May, S.; Dorval, V.; Lippé, S.; Larone Juneau, A.; Remmer, E.; et al. Nurturing and quiet intervention (NeuroN-QI) on preterm infants’ neurodevelopment and maternal stress and anxiety: A pilot randomized clinical trial protocol. J. Adv. Nurs. 2021, 77, 3192–3203. [Google Scholar] [CrossRef]
- Committee on Environmental Health. Noise: A hazard for the fetus and newborn. Pediatrics 1997, 100, 724–727. [Google Scholar] [CrossRef]
- Associação Brasileira de Normas Técnicas. ABNT NBR 10152: Acústica—Níveis De Pressão Sonora Em Ambientes Internos a Edificações; ABNT: Rio de Janeiro, Brazil, 2017; pp. 1–124. Available online: www.abnt.org.br (accessed on 4 September 2022).
- World Health Organisation. 2. Noise Sources and Their Measurement. 2.1. Basic Aspects of Acoustical Measurements. In Guidel Community Noise; WHO: Geneva, Switzerland, 1987; pp. 22–23. Available online: http://www.who.int/docstore/peh/noise/guidelines2.html (accessed on 18 October 2022).
- Andrade, K.P.; de Oliveira, L.L.A.; Souza, R.d.P.; de Matos, I.M.; Andrade, K.P.; de Oliveira, L.L.A.; Souza, R.d.P.; de Matos, I.M. Medida do nível de ruído hospitalar e seus efeitos em funcionários a partir do relato de queixas. Rev. CEFAC 2016, 18, 1379–1388. [Google Scholar] [CrossRef]
- Generaal, E.; Timmermans, E.J.; Dekkers, J.E.C.; Smit, J.H.; Penninx, B.W.J.H. Not urbanization level but socioeconomic, physical and social neighbourhood characteristics are associated with presence and severity of depressive and anxiety disorders. Psychol. Med. 2019, 49, 149–161. [Google Scholar] [CrossRef]
- Garrido Galindo, A.P.; Camargo Caicedo, Y.; Vélez-Pereira, A.M. Nivel continuo equivalente de ruido en la unidad de cuidado intensivo neonatal asociado al síndrome de burnout. Enferm. Intensiv. 2015, 26, 92–100. [Google Scholar] [CrossRef]
- dos Santos, N.A.R.; dos Santos, J.; da Silva, V.R.; Passos, J.P. Estresse ocupacional na assistência de cuidados paliativos em oncologia. Cogitare Enferm. 2017, 22, 50686. [Google Scholar] [CrossRef]
- Ruettgers, N.; Naef, A.C.; Rossier, M.; Knobel, S.E.J.; Jeitziner, M.M.; Holtforth, M.G.; Zante, B.; Schefold, J.C.; Nef, T.; Gerber, S.M. Perceived sounds and their reported level of disturbance in intensive care units: A multinational survey among healthcare professionals. PLoS ONE 2022, 17, e0279603. [Google Scholar] [CrossRef] [PubMed]
- Niu, S.F.; Chung, M.H.; Chu, H.; Tsai, J.C.; Lin, C.C.; Liao, Y.M.; Ou, K.L.; O’Brien, A.P.; Chou, K.R. Differences in cortisol profiles and circadian adjustment time between nurses working night shifts and regular day shifts: A prospective longitudinal study. Int. J. Nurs. Stud. 2015, 52, 1193–1201. [Google Scholar] [CrossRef]
- Bauer, M.E.; Vedhara, K.; Perks, P.; Wilcock, G.K.; Lightman, S.L.; Shanks, N. Chronic stress in caregivers of dementia patients is associated with reduced lymphocyte sensitivity to glucocorticoids. J. Neuroimmunol. 2000, 103, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Rojas-González, L.; Martínez-Leal, R.; Paz-Araviche, V.; Chacín-Almarza, B.; Corzo-Alvarez, G.; Sanabria-Vera, C.; Montiel-López, M. Niveles de cortisol sérico al inicio y al final de la jornada laboral y manifestaciones extra auditivas en trabajadores expuestos a ruido en una industria cervecera. Investig. Clin. 2004, 45, 297–307. [Google Scholar]
- da Cunha, S.M.M.; da Silva, V.R.M.; Dendasck, C.V.; Moreira, E.C.d.M.; de Oliveira, M.; de Oliveira, E. Estresse Ocupacional da Equipe de Enfermagem que Atua em Unidade de Terapia Intensiva. Rev. Científica Multidiscip. Núcleo Do Conhecimento 2017, 4, 68–78. [Google Scholar] [CrossRef]
- Ali, H.H.; Qasim, A.; Althahab, J.; Vuksanovic, B.; Al-Mosawi, M.; Machimbarrena, M.; Arias, R. Noise in ICUs: Review and Detailed Analysis of Long-Term SPL Monitoring in ICUs in Northern Spain. Sensors 2022, 22, 9038. [Google Scholar] [CrossRef]
- Tamayo, M.R.; Tróccoli, B.T. Construção e validação fatorial da Escala de Caracterização do Burnout (ECB). Estud. Psicol. 2009, 14, 213–221. [Google Scholar] [CrossRef]
- Ferreira LB, D.S.; Ribeiro RD CH, M.; Pompeo, D.A.; Contrin, L.M.; Werneck, A.L.; Ribeiro, R.M.; Sousa, C.N. Nível de estresse e avaliação preliminar da síndrome de Burnout em Enfermeiro da UTI na COVID-19—Estudo de caso. Res. Soc. Dev. 2022, 11, e31111225658. [Google Scholar] [CrossRef]
- Sarstedt, A. Catálogo de Produtos. Available online: https://www.sarstedt.com/pt/produtos/diagnostico/salivaexcrecao/product/51.1534.500/ (accessed on 25 November 2022).
- Nery, A.L.P.; Baader, W.J. Quimioflorescencia. Quim. Nova 2001, 24, 626. [Google Scholar] [CrossRef]
- Miller, R.; Stalder, T.; Jarczok, M.; Almeida, D.M.; Badrick, E.; Bartels, M.; Boomsma, D.I.; Coe, C.L.; Dekker, M.C.J.; Donzella, B.; et al. The CIRCORT database: Reference ranges and seasonal changes in diurnal salivary cortisol derived from a meta-dataset comprised of 15 field studies. Psychoneuroendocrinology 2016, 73, 16–23. [Google Scholar] [CrossRef]
- Aita, M.; Robins, S.; Charbonneau, L.; Doray-Demers, P.; Feeley, N. Comparing light and noise levels before and after a NICU change of design. J. Perinatol. 2021, 41, 2235–2243. [Google Scholar] [CrossRef] [PubMed]
- Garrido Galindo, A.P.; Camargo Caicedo, Y.; Velez-Pereira, A.M. Noise level in a neonatal intensive care unit in Santa Marta—Colombia. Colomb. Medica 2017, 48, 120–125. [Google Scholar] [CrossRef]
- Jordão, M.M.; Costa, R.; Santos, S.V.; Locks, M.O.H.; Assuiti, L.F.C.; de Lima, M.M. Ruídos na unidade neonatal: Identificando o problema e propondo soluções. Cogit. Enferm. (Online) 2017, 22, 1–8. [Google Scholar] [CrossRef]
- Capriolo, C.; Viscardi, R.M.; Broderick, K.A.; Nassebeh, S.; Kochan, M.; Solanki, N.S.; Leung, J.C. Assessment of Neonatal Intensive Care Unit Sound Exposure Using a Smartphone Application. Am. J. Perinatol. 2020, 39, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, M.d.F.H.; Ramos, E.G.; Peixoto, M.V.M. Identificação das fontes de ruído e de pressão sonora em unidade neonatal. Rev. Enferm. UERJ 2011, 19, 517–523. [Google Scholar]
- Nazário, A.P.; Santos, V.C.B.J.; Rossetto, E.G.; de Souza, S.N.D.H.; Amorim, N.E.Z.; Scochi, C.G.S.; Pinheiro Nazario, A.; Benetti Jacinto Santos, V.C.; Giovanini Rossetto, E.; Degau Hegeto de Souza, S.N.; et al. Avaliação dos ruídos em uma unidade neonatal de um hospital universitário. Semin. Cienc. Biol. Saude 2015, 36 (Suppl. S1), 189–198. [Google Scholar] [CrossRef]
- Shoemark, H.; Harcourt, E.; Arnup, S.J.; Hunt, R.W. Characterising the ambient sound environment for infants in intensive care wards. J. Paediatr. Child Health 2016, 52, 436–440. [Google Scholar] [CrossRef]
- Hernández-Salazar, A.D.; Gallegos-Martínez, J.; Reyes-Hernández, J. Level and Noise Sources in the Neonatal Intensive Care Unit of a Reference Hospital. Investig. Educ. Enferm. 2020, 38, e13. [Google Scholar] [CrossRef]
- Sabetsarvestani, R.; Köse, S.; Geçkil, E.; Tosun, E.E.; Tokan Özkiliçaslan, F.; Karaarslan, F.; Altunhan, H. Noise in a Neonatal Intensive Care Unit: Exploring Its State and Solutions. Adv. Neonatal Care 2022, 22, E183–E190. [Google Scholar] [CrossRef]
- Beken, S.; Önal, E.; Gündüz, B.; Çakir, U.; Karagöz, İ.; Kemaloğlu, Y.K. Negative Effects of Noise on NICU Graduates’ Cochlear Functions. Fetal Pediatr. Pathol. 2021, 40, 295–304. [Google Scholar] [CrossRef]
- Sinno, Z.C.; Shay, D.; Kruppa, J.; Klopfenstein, S.A.I.; Giesa, N.; Flint, A.R.; Herren, P.; Scheibe, F.; Spies, C.; Hinrichs, C.; et al. The influence of patient characteristics on the alarm rate in intensive care units: A retrospective cohort study. Sci. Rep. 2022, 12, 21801. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa, Y.; Ryherd, E.; Ryan, C.S.; Darcy-Mahoney, A. Examining the Utility of Perceptual Noise Categorization in Pediatric and Neonatal Hospital Units. HERD Health Environ. Res. Des. J. 2020, 13, 144–157. [Google Scholar] [CrossRef] [PubMed]
- Waterson, J.; Bedner, A. Types and frequency of infusion pump alarms and infusion-interruption to infusion-recovery times for critical short half-life infusions: Retrospective data analysis. JMIR Hum. Factors 2019, 6, e14123. [Google Scholar] [CrossRef]
- Silva, E.; Ramos, A.; Duarte, J.; Silva, D. Noise in neonatology: Perception of health professionals. Rev. Enferm. Ref. 2019, 4, 67–76. [Google Scholar] [CrossRef]
- Hawksley, E.J.; Helliwell, F. Noise in the NICU. Introducing a noise reduction policy to southmead neonatal intensive care unit: Primary results from a 3 month service improvement project. J. Pediatr. Neonatal Individ. Med. 2017, 6, 34. [Google Scholar] [CrossRef]
- Bertsch, M.; Reuter, C.; Czedik-Eysenberg, I.; Berger, A.; Olischar, M.; Bartha-Doering, L.; Giordano, V. The “Sound of Silence” in a Neonatal Intensive Care Unit—Listening to Speech and Music Inside an Incubator. Front. Psychol. 2020, 11, 1055. [Google Scholar] [CrossRef] [PubMed]
- Kramer, B.; Joshi, P.; Heard, C. Noise pollution levels in the pediatric intensive care unit. J. Crit. Care 2016, 36, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Disher, T.C.; Benoit, B.; Inglis, D.; Burgess, S.A.; Ellsmere, B.; Hewitt, B.E.; Bishop, T.M.; Sheppard, C.L.; Jangaard, K.A.; Morrison, G.C.; et al. Striving for Optimum Noise-Decreasing Strategies in Critical Care: Initial Measurements and Observations. J. Perinat. Neonatal Nurs. 2017, 31, 58–66. [Google Scholar] [CrossRef]
- Hu, R.F.; Hegadoren, K.M.; Wang, X.Y.; Jiang, X.Y. An investigation of light and sound levels on intensive care units in China. Aust. Crit. Care 2016, 29, 62–67. [Google Scholar] [CrossRef]
- Joshi, R.; Van Straaten, H.; Van De Mortel, H.; Long, X.; Andriessen, P.; Van Pul, C. Does the architectural layout of a NICU affect alarm pressure? A comparative clinical audit of a single-family room and an open bay area NICU using a retrospective study design. BMJ Open 2018, 8, e022813. [Google Scholar] [CrossRef]
- Bringel, J.M.d.A.; de Abreu, I.M.C.; Muniz, M.C.M.C.; Silva, M.-R.G. Saúde ambiental e níveis de ruído nas unidades de terapia intensiva neonatal: Uma revisão integrativa. Res. Soc. Dev. 2022, 11, e437111436263. [Google Scholar] [CrossRef]
- Santos, J.; Carvalhais, C.; Xavier, A.; Silva, M.V. Assessment and characterization of sound pressure levels in Portuguese neonatal intensive care units. Arch. Environ. Occup. Health 2018, 73, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Chawla, S.; Barach, P.; Dwaihy, M.; Kamat, D.; Shankaran, S.; Panaitescu, B.; Wang, B.; Natarajan, G. A targeted noise reduction observational study for reducing noise in a neonatal intensive unit. J. Perinatol. 2017, 37, 1060–1064. [Google Scholar] [CrossRef] [PubMed]
- Liszka, L.; Heiny, E.; Smith, J.; Schlaggar, B.L.; Mathur, A.; Pineda, R. Auditory exposure of high-risk infants discharged from the NICU and the impact of social factors. Acta Paediatr. 2020, 109, 2049–2056. [Google Scholar] [CrossRef]
- Degorre, C.; Ghyselen, L.; Barcat, L.; Dégrugilliers, L.; Kongolo, G.; Leké, A.; Tourneux, P. Noise level in the NICU: Impact of monitoring equipment. Arch. Pediatr. 2017, 24, 100–106. [Google Scholar] [CrossRef]
- Barsam, F.J.B.G.; da Silva, N.Y.E.B.; Uramoto, L.C.L.; Teixeira, C.L.S.B.; Camargo, F.C.; Zullo, S.A. Identificação do ruído ao longo dos turnos na terapia intensiva neonatal de hospital de ensino. J. Nurs. Health 2019, 9, 1–10. [Google Scholar] [CrossRef]
- Carvalhais, C.; Santos, J.; da Silva, M.V.; Xavier, A. Is There Sufficient Training of Health Care Staff on Noise Reduction in Neonatal Intensive Care Units? a Pilot Study From Neonoise Project. J. Toxicol. Environ. Health A 2015, 78, 897–903. [Google Scholar] [CrossRef]
- Batista, K.D.M.; Bianchi, E.R.F. Estresse do enfermeiro em unidade de emergência. Rev. Lat. Am. Enferm. 2006, 14, 534–539. [Google Scholar] [CrossRef]
- Santos, É.K.M.; Durães, R.F.; Guedes, M.d.S.; Rocha, M.F.O.; Rocha, F.C.; Torres, J.D.R.V.; Barbosa, H.A. O estresse nos profissionais de saúde: Uma revisão de literatura. HU Rev. 2019, 45, 203–211. [Google Scholar] [CrossRef]
- Harbs, T.; Rodrigues, T.; Quadros, V. Estresse da equipe de enfermagem em um centro de urgência e emergência. Bol. Enferm. 2008, 1, 41–56. [Google Scholar]
- Maslach, C.; Schaufeli, W.B.; Leiter, M. Job Burnout. Annu. Rev. Psychol. 2001, 52, 397–422. [Google Scholar] [CrossRef] [PubMed]
- West, C.P.; Dyrbye, L.N.; Shanafelt, T.D. Physician burnout: Contributors, consequences and solutions. J. Intern. Med. 2018, 283, 516–529. [Google Scholar] [CrossRef] [PubMed]
- da Silva, R.A.D.; Araújo, B.; Morais, C.C.A.; Campos, S.L.; de Andrade, A.D.; Brandão, D.C. Síndrome de Burnout: Realidade dos fisioterapeutas intensivistas? Fisioter. E Pesqui. 2018, 25, 388–394. [Google Scholar] [CrossRef]
- Nantsupawat, A.; Srisuphan, W.; Kunaviktikul, W.; Wichaikhum, O.A.; Aungsuroch, Y.; Aiken, L.H. Impact of nurse work environment and staffing on hospital nurse and quality of care in Thailand. J. Nurs. Scholarsh. 2011, 43, 426–432. [Google Scholar] [CrossRef]
- Fogaça, M.d.C.; de Carvalho, W.B.; Cítero, V.d.A.; Nogueira-Martins, L.A. Fatores que tornam estressante o trabalho de médicos e enfermeiros em terapia intensiva pediátrica e neonatal: Estudo de revisão bibliográfica. Rev. Bras. De Ter. Intensiv. 2008, 20, 261–266. [Google Scholar] [CrossRef]
- Bringel, J.M.d.A.; Abreu, I.; Muniz, M.C.M.C.; de Almeida, P.C.; Silva, M.R.G. Health Professionals’ Chronotype Association with Salivary Cortisol and Occupational Stress in Neonatal Intensive Care Units. Int. J. Environ. Res. Public Health 2023, 20, 5683. [Google Scholar] [CrossRef]
- Vidotti, V.; Ribeiro, R.P.; Galdino, M.J.Q.; Martins, J.T. Burnout Syndrome and shift work among the nursing staff. Rev. Lat. Am. Enferm. 2018, 26, e3022. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.; Bogossian, F.; Ahern, K. Stress and coping in Australian nurses: A systematic review. Int. Nurs. Rev. 2010, 57, 22–31. [Google Scholar] [CrossRef]
- Khamisa, N.; Oldenburg, B.; Peltzer, K.; Ilic, D. Work Related Stress, Burnout, Job Satisfaction and General Health of Nurses. Int. J. Environ. Res. Public Health 2015, 12, 652–666. [Google Scholar] [CrossRef]
- Edmonson, C.; Zelonka, C. Our own worst enemies the nurse bullying epidemic. Nurs. Adm. Q. 2019, 43, 274–279. [Google Scholar] [CrossRef]
- Arabacı, A.; Önler, E. The Effect of Noise Levels in the Operating Room on the Stress Levels and Workload of the Operating Room Team. J. Perianesthesia Nurs. 2021, 36, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Rahmati, F.; Safari, S.; Hashemi, B.; Baratloo, A.; Rad, K. Prevalence of Depression and Personality Disorders in the Beginning and End of Emergency Medicine Residency Program; a Prospective Cross Sectional Study. Arch. Acad. Emerg. Med. 2019, 7, 5. [Google Scholar]
- Karacic, J.; Bursztajn, H.J.; Arvanitakis, M. Who cares what the doctor feels: The responsibility of health politics for burnout in the pandemic. Healthcare 2021, 9, 1550. [Google Scholar] [CrossRef] [PubMed]
- Hahad, O.; Prochaska, J.H.; Daiber, A.; Muenzel, T. Environmental Noise-Induced Effects on Stress Hormones, Oxidative Stress, and Vascular Dysfunction: Key Factors in the Relationship between Cerebrocardiovascular and Psychological Disorders. Oxid. Med. Cell. Longev. 2019, 2019, 4623109. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Valdecantos, D.; Caballero-García, A.; Del Castillo-Sanz, T.; Bello, H.J.; Roche, E.; Córdova, A. Stress Salivary Biomarkers Variation during the Work Day in Emergencies in Healthcare Professionals. Int. J. Environ. Res. Public Health 2021, 18, 3937. [Google Scholar] [CrossRef] [PubMed]
- Dias, E.N.; Pais-Ribeiro, J.L. O Modelo de Coping de Folkman e Lazarus: Aspectos Históricos e Conceituais. Rev. Psicol. E Saúde 2019, 11, 55–66. [Google Scholar] [CrossRef]
- Lin, Y.-H.; Jen, H.-J.; Lin, Y.-K.; Seo, J.-D.; Chang, W.-P. Cortisol Awakening Response and Stress in Female Nurses on Monthly Shift Rotations: A Longitudinal Study. BioMed Res. Int. 2022, 2022, 9506583. [Google Scholar] [CrossRef]
- Anjum, B.; Verma, N.S.; Tiwari, S.; Singh, R.; Mahdi, A.A.; Singh, R.B.; Singh, R.K. Association of salivary cortisol with chronomics of 24 hours ambulatory blood pressure/heart rate among night shift workers. Biosci. Trends 2011, 5, 182–188. [Google Scholar] [CrossRef]
- Bracci, M.; Ciarapica, V.; Copertaro, A.; Barbaresi, M.; Manzella, N.; Tomasetti, M.; Gaetani, S.; Monaco, F.; Amati, M.; Valentino, M.; et al. Peripheral Skin Temperature and Circadian Biological Clock in Shift Nurses after a Day off. Int. J. Mol. Sci. 2016, 17, 623. [Google Scholar] [CrossRef]
- de Assis, D.C.; de Resende, D.V.; Marziale, M.H.P. Association between shift work, salivary cortisol levels, stress and fatigue in nurses: Integrative review. Esc. Anna Nery 2018, 22, 2018. [Google Scholar] [CrossRef]
- Vasconcelos, S.; Marqueze, E.; Gonçalves, L.; Lemos, L.; Araújo, L.; Fischer, F.M.; Moreno, C.R.C. Morbidity among nursing personnel and its association with working conditions and work organization. Work 2012, 41, 3732–3737. [Google Scholar] [CrossRef] [PubMed]
- Ta, V.P.; Gesselman, A.N.; Perry, B.L.; Fisher, H.E.; Garcia, J.R. Stress of Singlehood: Marital Status, Domain-Specific Stress, and Anxiety in a National U.S. Sample. J. Soc. Clin. Psychol. 2017, 36, 461–485. [Google Scholar] [CrossRef]
- Chin, B.; Murphy, M.L.M.; Janicki-Deverts, D.; Cohen, S. Marital status as a predictor of diurnal salivary cortisol levels and slopes in a community sample of healthy adults. Psychoneuroendocrinology 2017, 78, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Paiva, T.; Reis, C.; Feliciano, A.; Canas-Simião, H.; Machado, M.A.; Gaspar, T.; Tomé, G.; Branquinho, C.; Silva, M.R.; Ramiro, L.; et al. Sleep and awakening quality during COVID-19 confinement: Complexity and relevance for health and behavior. Int. J. Environ. Res. Public Health 2021, 18, 3506. [Google Scholar] [CrossRef] [PubMed]

| Period | American Academy of Pediatrics (1997) (dBA) | World Health Organization (2006) (dBA) | Brazilian Association of Technical Procedures (2017) (dBA) |
|---|---|---|---|
| Day | 45 | 35 | - |
| Night | 35 | 30 | - |
| Range | - | - | 35 to 40 |
| Characteristics | n (%) |
|---|---|
| Considering the shift tiring (n = 226) | |
| Yes | 128 (56.6) |
| No | 98 (43.3) |
| Considering the shift stressful (n = 219) | |
| Yes | 100 (45.7) |
| No | 119 (54.3) |
| Considering noise level in the environment to be excessive (n = 204) | |
| Yes | 160 (78.4) |
| No | 44 (21.6) |
| Cortisol level (beginning of the shift) (n = 225) | |
| Normal | 181 (80.4) |
| Increased | 44 (19.6) |
| Cortisol level (end of the shift) (n = 230) | |
| Normal | 222 (96.5) |
| Increased | 8 (3.5) |
| Burnout occurrence (n = 246) | |
| Possibility | 64 (26.1) |
| Initial | 145 (58.9) |
| Installed | 37 (15.0) |
| Characteristics | Cortisol Level at the Beginning of the Work Shift | ||
|---|---|---|---|
| Normal (n = 182) | Increased (n = 44) | p | |
| Age | 40 ± 10 | 37 ± 9 | 0.087 |
| Gender | 0.080 | ||
| Male | 12 (6.6) | 0 (0) | |
| Female | 170 (93.4) | 44 (100) | |
| Marital status | 0.010 | ||
| Married | 99 (55) | 18 (41.9) | |
| Stable unit | 10 (5.6) | 9 (20.9) | |
| Single | 56 (31.1) | 14 (32.6) | |
| Divorced | 15 (8.3) | 2 (4.7) | |
| Having children | 0.516 | ||
| Yes | 114 (63.3) | 31 (72.1) | |
| No | 61 (36.7) | 12 (27.9) | |
| Function | 0.213 | ||
| Doctor | 44 (24.4) | 6 (14) | |
| Nurse | 33 (18.3) | 10 (23.3) | |
| Nurse technician | 89 (49.4) | 26 (60.5) | |
| Physiotherapist or speech therapist | 14 (7.8) | 1 (2.3) | |
| Time spent commuting (min) | 0.846 | ||
| <30 min | 76 (41.7) | 15 (34.9) | |
| 31–60 min | 68 (37.8) | 20 (46.5) | |
| 61 or more | 36 (20) | 8 (18.6) | |
| Having another job | 0.277 | ||
| Yes | 72 (40) | 13 (31) | |
| No | 108 (60) | 29 (69) | |
| Coming to work from another job | 0.020 | ||
| Yes | 24 (13.3) | 12 (27.9) | |
| No | 156 (86.7) | 31 (72.1) | |
| Continuous hours of work | 0.316 | ||
| 6 h | 3 (13.6) | 2 (20) | |
| 12 h | 8 (36.4) | 2 (20) | |
| 18 h | 3 (13.6) | 4 (40) | |
| 24 h | 8 (36.4) | 2 (20) | |
| Characteristics | LAeq | p | |
|---|---|---|---|
| n (%) | Mean ± DP | ||
| BURNOUT classification (n = 246) | 0.391 ¹ | ||
| Possibility | 64 (26.1) | 63.65 ± 2.26 | |
| Initial | 145 (58.9) | 63.8 ± 1.69 | |
| Frequent | 37 (15) | 63.26 ± 3.3 | |
| Cortisol level (beginning of the shift) (n = 225) | 0.062 ² | ||
| Normal | 181(80.4) | 63.87 ± 1.89 | |
| Altered | 44(19.6) | 62.92 ± 3.18 | |
| Cortisol level (end of the shift) (n = 230) | 0.580 ² | ||
| Normal | 222 (96.6) | 63.67 ± 2.23 | |
| Altered | 8 (3.4) | 64.11 ± 2.02 | |
| Job function (n = 251) | 0.073 ¹ | ||
| Doctors | 57 (22.7) | 64.13 ± 1.04 | |
| Nurse | 48 (19.1) | 63.09 ± 3.03 | |
| Nursing technician | 130 (51.8) | 63.65 ± 2.13 | |
| Physiotherapist and speech therapist | 16 (6.4) | 64.13 ± 1.45 | |
| Work shift (n = 256) | 0.005 1,* | ||
| 6 h—Morning | 34 (13.3) | 64.24 ± 1.08 | |
| 6 h—Afternoon | 23 (9.0) | 64.56 ± 1.02 | |
| 12 h—Daytime | 108 (42.2) | 63.82 ± 2.21 | |
| 12 h—Night-time | 91 (35.5) | 63.14 ± 2.39 | |
| Physical health (initial) (n = 243) | 0.360 ¹ | ||
| Very tired | 25 (10.2) | 63.76 ± 1.18 | |
| Slightly tired | 130 (53.5) | 63.89 ± 1.84 | |
| Rested | 88 (36.3) | 63.5 ± 2.35 | |
| Physical health (Final) (n = 227) | 0.558 ¹ | ||
| Very tired | 81 (35.7) | 63.88 ± 2 | |
| Slightly tired | 103 (45.4) | 63.56 ± 2.57 | |
| Rested | 43 (18.9) | 63.52 ± 1.69 | |
| Tiring shift (n = 226) | 0.216 ² | ||
| Yes | 128 (56.6) | 63.83 ± 2.13 | |
| No | 98 (43.3) | 63.49 ± 1.91 | |
| Stressful shift (n = 219) | 0.270 ² | ||
| Yes | 100 (45.7) | 63.54 ± 2.61 | |
| No | 119 (54.3) | 63.85 ± 1.36 | |
| Environment with excessive noise (n = 204) | 0.603 ² | ||
| Yes | 160 (78.4) | 63.65 ± 2.42 | |
| No | 44 (21.6) | 63.85 ± 1.47 | |
| Characteristics | LAeq | p | |
|---|---|---|---|
| n | rho | ||
| Total group | |||
| Cortisol level (end of the shift) | 231 | −0.054 | 0.417 |
| Cortisol variation until the end of the shift (End–Start) | 221 | −0.001 | 0.983 |
| Male | |||
| Cortisol level (end of the shift) | 12 | −0.261 | 0.412 |
| Cortisol variation until the end of the shift (End–Start) | 12 | 0.062 | 0.849 |
| Female | |||
| Cortisol level (end of the shift) | 219 | −0.039 | 0.561 |
| Cortisol variation until the end of the shift (End–Start) | 209 | −0.003 | 0.960 |
| Burnout: “Possible” | |||
| Cortisol level (end of the shift) | 59 | −0.064 | 0.632 |
| Cortisol variation until the end of the shift (End–Start) | 56 | −0.05 | 0.713 |
| Burnout: “Initial” | |||
| Cortisol level (end of the shift) | 133 | −0.086 | 0.325 |
| Cortisol variation until the end of the shift (End–Start) | 127 | −0.035 | 0.699 |
| Burnout: “Frequent” | |||
| Cortisol level (end of the shift) | 33 | −0.031 | 0.864 |
| Cortisol variation until the end of the shift (End–Start) | 32 | 0.032 | 0.861 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bringel, J.M.d.A.; Abreu, I.; Muniz, M.-C.M.C.; de Almeida, P.C.; Silva, M.-R.G. Excessive Noise in Neonatal Units and the Occupational Stress Experienced by Healthcare Professionals: An Assessment of Burnout and Measurement of Cortisol Levels. Healthcare 2023, 11, 2002. https://doi.org/10.3390/healthcare11142002
Bringel JMdA, Abreu I, Muniz M-CMC, de Almeida PC, Silva M-RG. Excessive Noise in Neonatal Units and the Occupational Stress Experienced by Healthcare Professionals: An Assessment of Burnout and Measurement of Cortisol Levels. Healthcare. 2023; 11(14):2002. https://doi.org/10.3390/healthcare11142002
Chicago/Turabian StyleBringel, Jocélia Maria de Azevedo, Isabel Abreu, Maria-Cláudia Mendes Caminha Muniz, Paulo César de Almeida, and Maria-Raquel G. Silva. 2023. "Excessive Noise in Neonatal Units and the Occupational Stress Experienced by Healthcare Professionals: An Assessment of Burnout and Measurement of Cortisol Levels" Healthcare 11, no. 14: 2002. https://doi.org/10.3390/healthcare11142002
APA StyleBringel, J. M. d. A., Abreu, I., Muniz, M.-C. M. C., de Almeida, P. C., & Silva, M.-R. G. (2023). Excessive Noise in Neonatal Units and the Occupational Stress Experienced by Healthcare Professionals: An Assessment of Burnout and Measurement of Cortisol Levels. Healthcare, 11(14), 2002. https://doi.org/10.3390/healthcare11142002







