Obesity-Status-Linked Affecting Factors of Dyslipidemia in Korean Young-Adult Men: Based on the Korea National Health and Nutrition Examination Survey (2019–2021)
Abstract
1. Introduction
2. Materials and Methods
2.1. Data and Participants
2.2. Definitions of Variables
2.2.1. Dyslipidemia
2.2.2. General Characteristics
2.2.3. Health-Related Characteristics
2.3. Ethical Considerations
2.4. Statistical Analysis
3. Results
3.1. Dyslipidemia Prevalence by General and Health-Related Characteristics in Obese and Nonobese Groups
3.2. Affecting Factors of Dyslipidemia According to Obesity Status
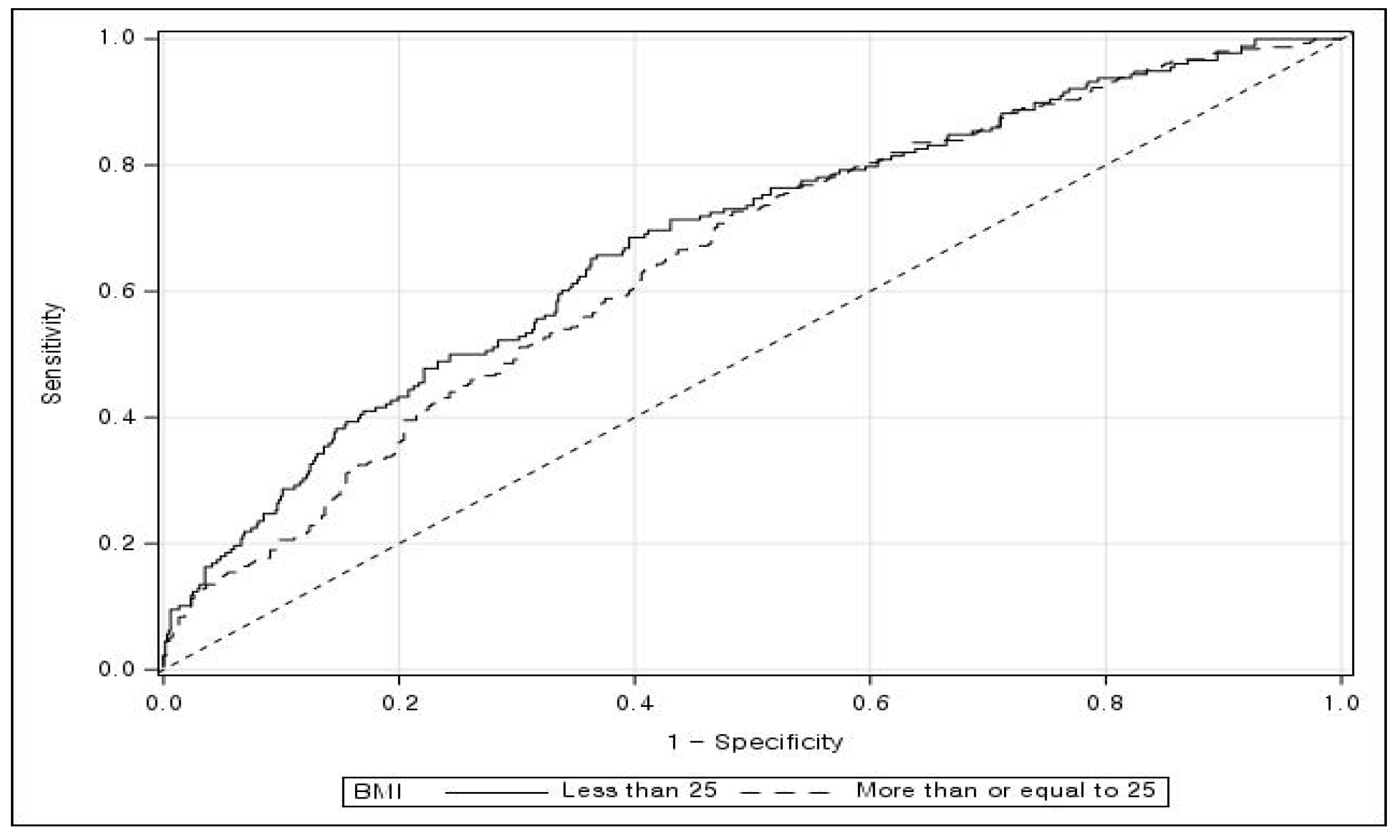
3.3. Model Fit
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rhee, E.J.; Kim, H.C.; Kim, J.H.; Lee, E.Y.; Kim, B.J.; Kim, E.M.; Song, Y.; Lim, J.H.; Kim, H.J.; Choi, S.; et al. 2018 Guidelines for the Management of Dyslipidemia in Korea. J. Lipid Atheroscler. 2019, 8, 78–131. [Google Scholar] [CrossRef]
- Pirillo, A.; Casula, M.; Olmastroni, E.; Norata, G.D.; Catapano, A.L. Global epidemiology of dyslipidaemias. Nat. Rev. Cardiol. 2021, 18, 689–700. [Google Scholar] [CrossRef]
- Bray, G.A.; Kim, K.K.; Wilding, J.P.H.; World Obesity Federation. Obesity: A chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes. Rev. 2017, 18, 715–723. [Google Scholar] [CrossRef]
- Weir, C.B.; Arif, J. BMI Classification Percentile and Cut off Points; StatPearls Publishing: Treasure Island, UK, 2021; pp. 1–5. Available online: https://www.ncbi.nlm.nih.gov/books/NBK541070 (accessed on 27 June 2022).
- WHO. Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation; World Health Organization Technical Report Series; WHO: Geneva, Switzerland, 2000; Volume 894, pp. 1–253. [Google Scholar]
- WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004, 363, 157–163. [Google Scholar] [CrossRef]
- Kopin, L.; Lowenstein, C. Dyslipidemia. Ann. Intern. Med. 2017, 167, Itc81–Itc96. [Google Scholar] [CrossRef]
- Global Health Data Exchange. GBD Results Tool. Institute for Health Metrics and Evaluation. 2021. Available online: http://ghdx.healthdata.org/gbd-results-tool (accessed on 25 March 2023).
- Berberich, A.J.; Hegele, R.A. A modern approach to dyslipidemia. Endocr. Rev. 2022, 43, 611–653. [Google Scholar] [CrossRef]
- Park, J.B.; Kim, D.H.; Lee, H.; Lee, H.J.; Hwang, I.C.; Yoon, Y.E.; Park, H.E.; Lee, S.P.; Choi, S.Y.; Kim, Y.J.; et al. Effect of moderately but persistently elevated lipid levels on risks of stroke and myocardial infarction in young Korean adults. J. Am. Heart Assoc. 2021, 10, e020050. [Google Scholar] [CrossRef]
- [Dataset] Korea Disease Control and Prevention Agency. Korea National Health & Nutrition Examination Survey VIII-3. Available online: https://knhanes.kdca.go.kr/knhanes/sub03/sub03_02_05.do (accessed on 1 April 2023).
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Circulation 2002, 106, 3143–3421. [Google Scholar] [CrossRef]
- Zhang, H.; Kwapong, W.R.; Shao, M.-M.; Yan, J.-Y.; Lin, X.-D.; Chen, B.-B.; Chen, K.-Y. Predictors of the prevalence of dyslipidemia and influencing factors for young health examination cohort: A cross-sectional survey. Front. Public Health 2020, 8, 400. [Google Scholar] [CrossRef]
- Hudson, S.E.; Feigenbaum, M.S.; Patil, N.; Ding, E.; Ewing, A.; Trilk, J.L. Screening and socioeconomic associations of dyslipidemia in young adults. BMC Public Health 2020, 20, 104. [Google Scholar] [CrossRef]
- Jeon, M.Y.; Choi, W.H.; Seo, Y.M. Risk factors of dyslipidemia and related factors of medication adherence in Korea adults: KNHANES 2013-2015. J. Korean Biol. Nurs. Sci. 2017, 19, 131–140. [Google Scholar]
- Klop, B.; Elte, J.W.F.; Castro Cabezas, M. Dyslipidemia in obesity: Mechanisms and potential targets. Nutrients 2013, 5, 1218–1240. [Google Scholar] [CrossRef] [PubMed]
- Perone, F.; Pingitore, A.; Conte, E.; Halasz, G.; Ambrosetti, M.; Peruzzi, M.; Cavarretta, E. Obesity and cardiovascular risk: Systematic intervention is the key for prevention. Healthcare 2023, 11, 902. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Jimenez, F.; Almahmeed, W.; Bays, H.; Cuevas, A.; Di Angelantonio, E.; Le Roux, C.W.; Sattar, N.; Sun, M.C.; Wittert, G.; Pinto, F.J.; et al. Obesity and cardiovascular disease: Mechanistic insights and management strategies. A joint position paper by the World Heart Federation and World Obesity Federation. Eur. J. Prev. Cardiol. 2022, 29, 2218–2237. [Google Scholar] [CrossRef]
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Després, J.P.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. Obesity and cardiovascular disease: A scientific statement from the American Heart Association. Circulation 2021, 143, e984–e1010. [Google Scholar] [CrossRef]
- Wang, J.; Thornton, J.C.; Russell, M.; Burastero, S.; Heymsfield, S.; Pierson, R.N., Jr. Asians have lower body mass index (BMI) but higher percent body fat than do whites: Comparisons of anthropometric measurements. Am. J. Clin. Nutr. 1994, 60, 23–28. [Google Scholar] [CrossRef]
- Shibata, Y.; Ojima, T.; Nakamura, M.; Kuwabara, K.; Miyagawa, N.; Saito, Y.; Nakamura, Y.; Kiyohara, Y.; Nakagawa, H.; Fujiyoshi, A.; et al. Associations of overweight, obesity, and underweight with high serum total cholesterol level over 30 years among the Japanese elderly: NIPPON DATA 80, 90, and 2010. J. Epidemiol. 2019, 29, 133–138. [Google Scholar] [CrossRef]
- Korea Centers for Disease Control and Prevention. 2019–2021 National Health Statistics Reports, The 8th Korea National Health and Nutrition Examination Survey, Guidelines for Use of Raw Data; Centers for Disease Control and Prevention: Osong, Republic of Korea, 2023; Available online: https://knhanes.kdca.go.kr/knhanes/sub03/sub03_06_02.do (accessed on 8 April 2023).
- Committee for the Korean Guidelines for the Management of Dyslipidemia. 2015 Korean guidelines for management of dyslipidemia. J. Lipid Atheroscler. 2015, 4, 61–92. [Google Scholar] [CrossRef]
- Seo, M.H.; Lee, W.Y.; Kim, S.S.; Kang, J.H.; Kang, J.H.; Kim, K.K.; Kim, B.Y.; Kim, Y.H.; Kim, W.J.; Kim, E.M.; et al. 2018 Korean society for the study of obesity guideline for the management of obesity in Korea. J. Obes. Metab. Syndr. 2019, 28, 40–45. [Google Scholar] [CrossRef]
- Agarwal, D.P. Cardioprotective effects of light–moderate consumption of alcohol: A review of putative mechanisms. Alcohol Alcohol. 2002, 37, 409–415. [Google Scholar] [CrossRef] [PubMed]
- WHO AUDIT. The Alcohol Use Disorders Identification Test, 2nd ed.; WHO: Geneva, Switzerland, 2001; Available online: https://apps.who.int/iris/bitstream/handle/10665/67205/WHO_MSD_MSB_01.6a.pdf?sequence=1&isAllowed=y (accessed on 25 March 2023).
- Reid, M.C.; Fiellin, D.A.; O’Connor, P.G. Hazardous and harmful alcohol consumption in primary care. Arch. Intern. Med. 1999, 159, 1681–1689. [Google Scholar] [CrossRef]
- The Ministry of Health and Welfare & Korea Health Promotion Institute. 2022 Guideline on Integrated Community Health Promotion Program. Sejong, Republic of Korea. Available online: https://www.mohw.go.kr/react/gm/sgm0704vw.jsp?PAR_MENU_ID=13&MENU_ID=1304080701&page=1&CONT_SEQ=372347&PAR_CONT_SEQ=355835 (accessed on 1 April 2023).
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Katz, E.S.; Kheirandish-Gozal, L. National Sleep Foundation’s sleep time duration recommendations: Methodology and results summary. Sleep Health 2015, 1, 40–43. [Google Scholar] [CrossRef] [PubMed]
- 2020 Dietary Reference Intakes for Koreans (KDRIs). Available online: https://www.kns.or.kr/FileRoom/FileRoomview.asp?mode=mod&rstring=%252FFileRoom%252FFileRoom.asp%253Fxsearch%253D0%253D%253Dxrow%253D10%253D%253DBoardID%253DKdr%253D%253Dpage%253D1&idx=125&page=1&BoardID=Kdr&xsearch=1&cn_search= (accessed on 25 March 2023).
- Crowson, C.S.; Atkinson, E.J.; Therneau, T.M. Assessing calibration of prognostic risk scores. Stat. Methods Med. Res. 2016, 25, 1692–1706. [Google Scholar] [CrossRef] [PubMed]
- Robin, X.; Turck, N.; Hainard, A.; Tiberti, N.; Lisacek, F.; Sanchez, J.-C.; Müller, M.; Siegert, S.; Doering, M.; Billings, Z. Package pROC: Display and Analyze ROC Curves. 2023. Available online: http://expasy.org/tools/pROC/ (accessed on 6 July 2023).
- Nagelkerke, N.J.D. A note on a general definition of the coefficient of determination. Biometrika 1991, 78, 691–692. [Google Scholar] [CrossRef]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef]
- Cho, S.M.J.; Lee, H.; Lee, H.-H.; Baek, J.; Heo, J.E.; Joo, H.J.; Hong, S.J.; Kim, H.C. Dyslipidemia fact sheets in Korea 2020: An analysis of nationwide population-based data. J. Lipid Atheroscler. 2021, 10, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Domanski, M.J.; Tian, X.; Wu, C.O.; Reis, J.P.; Dey, A.K.; Gu, Y.; Zhao, L.; Bae, S.; Liu, K.; Hasan, A.A.; et al. Time course of LDL cholesterol exposure and cardiovascular disease event risk. J. Am. Coll. Cardiol. 2020, 76, 1507–1516. [Google Scholar] [CrossRef]
- Shapiro, M.D.; Bhatt, D.L. “Cholesterol-years” for ASCVD risk prediction and treatment. J. Am. Coll. Cardiol. 2020, 76, 1517–1520. [Google Scholar] [CrossRef]
- Swami, V.; Frederick, D.A.; Aavik, T.; Alcalay, L.; Allik, J.; Anderson, D.; Andrianto, S.; Arora, A.; Brännström, Å.; Cunningham, J. The attractive female body weight and female body dissatisfaction in 26 countries across 10 world regions: Results of the International Body Project I. Personal. Soc. Psychol. Bull. 2010, 36, 309–325. [Google Scholar] [CrossRef]
- Lim, Y.-S.; Park, N.-R.; Jeon, S.-B.; Jeong, S.-Y.; Tserendejid, Z.; Park, H.-R. Analysis of weight control behaviors by body image perception among Korean women in different age groups: Using the 2010 Korea National Health and Nutrition Examination Survey data. Korean J. Community Nutr. 2015, 20, 141–150. [Google Scholar] [CrossRef]
- Chen, K.K.; Wee, S.L.; Pang, B.W.J.; Lau, L.K.; Jabbar, K.A.; Seah, W.T.; Ng, T.P. Relationship between BMI with percentage body fat and obesity in Singaporean adults—The Yishun Study. BMC Public Health 2021, 21, 1030. [Google Scholar] [CrossRef] [PubMed]
- Choi, W.H.; Seo, Y.M.; Jeon, M.Y.; Choi, S.Y. Convergence study on the comparison of risk factors for dyslipidemia by age and gender: Based on the Korea National Health and Nutrition Examination Survey (2013~2015 year). J. Korea Converg. Soc. 2018, 9, 571–587. [Google Scholar]
- Chong, M.Y. Analyzing the association of dyslipidemia based on total cholesterol according to dietary life and health characteristics using Korea National Health and Nutrition Examination Survey (KNHANES VII-1). J. Digit. Converg. 2020, 18, 615–630. [Google Scholar]
- Ross, R.; Neeland, I.J.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; Cuevas, A.; Hu, F.B. Waist circumference as a vital sign in clinical practice: A Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 2020, 16, 177–189. [Google Scholar] [CrossRef]
- Han, T.S.; Lean, M.E. A clinical perspective of obesity, metabolic syndrome and cardiovascular disease. JRSM Cardiovasc. Dis. 2016, 5, 2048004016633371. [Google Scholar] [CrossRef]
- Shin, S.; Lee, S. Relation between the total diet quality based on Korean Healthy Eating Index and the incidence of metabolic syndrome constituents and metabolic syndrome among a prospective cohort of Korean adults. Korean J. Community Nutr. 2020, 25, 61–70. [Google Scholar] [CrossRef]
- Tenk, J.; Mátrai, P.; Hegyi, P.; Rostás, I.; Garami, A.; Szabó, I.; Hartmann, P.; Pétervári, E.; Czopf, L.; Hussain, A. Perceived stress correlates with visceral obesity and lipid parameters of the metabolic syndrome: A systematic review and meta-analysis. Psychoneuroendocrinology 2018, 95, 63–73. [Google Scholar] [CrossRef]
- Gostynski, M.; Gutzwiller, F.; Kuulasmaa, K.; Döring, A.; Ferrario, M.; Grafnetter, D.; Pajak, A. Analysis of the relationship between total cholesterol, age, body mass index among males and females in the WHO MONICA Project. Int. J. Obes. 2004, 28, 1082–1090. [Google Scholar] [CrossRef]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. ESC Scientific Document Group. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef]
- Di Fusco, S.A.; Arca, M.; Scicchitano, P.; Alonzo, A.; Perone, F.; Gulizia, M.M.; Gabrielli, D.; Oliva, F.; Imperoli, G.; Colivicchi, F. Lipoprotein(a): A risk factor for atherosclerosis and an emerging therapeutic target. Heart 2022, 109, 18–25. [Google Scholar] [CrossRef]
- Sokolova, M.; Japkowicz, N.; Szpakowicz, S. Beyond accuracy, F-score and ROC: A family of discriminant measures for performance evaluation. In AI 2006: Advances in Artificial Intelligence; Sattar, A., Kang, B.-H., Eds.; Springer: Berlin/Heidelberg, Germany, 2006; pp. 1015–1021. [Google Scholar]
- Menardi, G.; Torelli, N. Training and assessing classification rules with imbalanced data. Data Min. Knowl. Discov. 2014, 28, 92–122. [Google Scholar] [CrossRef]

| Variable | Category | BMI, kg/m2 | |||||
|---|---|---|---|---|---|---|---|
| <25 | ≥25 | ||||||
| Dyslipidemia | Rao–Scott Chi-Squared Test (p-Value) | Dyslipidemia | Rao–Scott Chi-Squared Test (p-Value) | ||||
| No | Yes | No | Yes | ||||
| n (% 1) | n (% 1) | n (% 1) | n (% 1) | ||||
| Total | 683 (79.3) | 178 (20.7) | - | 387(55.4) | 311 (44.6) | - | |
| Age, years | 28.5 ± 0.27 2 | 30.5 ± 0.47 2 | −4.22 (<0.001) 3 | 29.5. ± 0.35 2 | 31.7 ± 0.37 2 | −4.49 ( < 0.001) 3 | |
| Education | High school or below | 354 (81.9) | 74 (18.1) | 2.83 (0.0924) | 182 (59.1) | 121 (40.9) | 2.18 (0.1402) |
| College or above | 329 (76.6) | 104 (23.4) | 205 (52.8) | 190 (47.2) | |||
| Income | 1st quartile | 155 (75.3) | 47 (24.7) | 1.89 (0.5963) | 98 (52.9) | 88 (47.1) | 1.75 (0.6250) |
| 2nd quartile | 179 (79.9) | 48 (20.1) | 99 (53.5) | 86 (46.5) | |||
| 3rd quartile | 166 (80.6) | 42 (19.4) | 101 (60.2) | 69 (39.8) | |||
| 4th quartile | 183 (80.6) | 41 (19.4) | 89 (55.9) | 68 (44.1) | |||
| Body image perception | Skinny | 234 (87.1) | 32 (12.9) | 15.88 (0.0004) | - | - | 0.18 (0.6678) |
| Normal | 333 (78.1) | 95 (21.9) | 46 (58.1) | 31 (41.9) | |||
| Overweight | 116 (69.1) | 51 (30.9) | 341 (55.2) | 280 (44.8) | |||
| Stress | No | 510 (81.7) | 119 (18.3) | 7.13 (0.0076) | 254 (57.8) | 183 (42.2) | 1.87 (0.1719) |
| Yes | 173 (72.4) | 59 (27.6) | 133 (51.7) | 128 (48.3) | |||
| Subjective health | Good | 332 (79.7) | 86 (20.3) | 0.40 (0.8196) | 148 (57.8) | 104 (42.2) | 4.96 (0.0836) |
| Normal | 297 (79.3) | 79 (20.7) | 191 (56.9) | 153 (43.1) | |||
| Bad | 54 (75.9) | 13 (24.1) | 48 (44.9) | 54 (55.1) | |||
| Drinking | No | 64 (81.4) | 18 (18.6) | 0.93 (0.6267) | 30 (46.6) | 36 (53.4) | 1.91 (0.3844) |
| Moderate | 550 (78.5) | 145 (21.5) | 297 (56.4) | 229 (43.6) | |||
| High | 69 (82.7) | 15 (17.3) | 60 (56.7) | 46 (43.3) | |||
| Smoking | No | 294 (81.8) | 65 (18.2) | 1.83 (0.1765) | 152 (58.9) | 111 (41.1) | 1.35 (0.2446) |
| Yes | 389 (77.4) | 113 (22.6) | 235 (53.5) | 200 (46.5) | |||
| Walking | No | 361 (76.6) | 105 (23.4) | 3.28 (0.0702) | 198 (49.9) | 189 (50.1) | 8.84 (0.0029) |
| Yes | 322 (82.3) | 73 (17.7) | 189 (61.9) | 122 (38.1) | |||
| Muscle exercise | No | 382 (77.1) | 112 (22.9) | 2.53 (0.1116) | 248 (52.3) | 224 (47.7) | 4.08 (0.0435) |
| Yes | 301 (82.0) | 66 (18.0) | 139 (61.5) | 87 (38.5) | |||
| Aerobic exercise | No | 266 (75.5) | 82 (24.5) | 3.95 (0.0468) | 143 (50.9) | 143 (549.1) | 3.04 (0.0814) |
| Yes | 417 (81.7) | 96 (18.3) | 244 (58.5) | 168 (41.5) | |||
| Sleep | Insufficient | 454 (80.0) | 117 (20.0) | 0.39 (0.5308) | 237 (57.1) | 187 (42.9) | 0.72 (0.3951) |
| Normal | 229 (77.7) | 61 (22.3) | 150 (53.2) | 124 (46.8) | |||
| Working hours, minutes | 33.7 ± 0.87 2 | 35.6 ± 1.72 2 | −1.06 (0.2909) 3 | 35.4 ± 1.19 2 | 38.1 ± 1.25 2 | −1.54 (0.1236)3 | |
| Waist circumference, cm | <90 | 674 (80.9) | 160 (19.1) | 33.71 (<0.001) | 131 (66.9) | 60 (33.1) | 10.11 (0.0015) |
| ≥90 | 9 (33.0) | 18 (67.0) | 256 (51.5) | 251 (48.5) | |||
| Energy intake | Normal | 544 (78.7) | 147 (21.3) | 0.42 (0.5176) | 313 (56.4) | 250 (43.6) | 0.90 (0.3421) |
| Excessive | 139 (81.3) | 31 (18.7) | 74 (51.6) | 61 (48.4) | |||
| Fat intake | Normal | 456 (78.8) | 127 (21.2) | 0.19 (0.6647) | 278 (55.4) | 226 (44.5) | 0.01 (0.9375) |
| Excessive | 227 (80.2) | 51 (19.8) | 109 (55.8) | 85 (44.2) | |||
| Carbohydrate intake | Normal | 557 (78.7) | 152 (21.2) | 0.44 (0.5092) | 324 (56.6) | 257 (43.4) | 1.47 (0.2260) |
| Excessive | 126 (81.5) | 26 (18.5) | 63 (49.6) | 54 (50.4) | |||
| Sodium intake | Normal | 93 (79.1) | 27 (20.9) | 0.0003 (0.9855) | 60 (63.4) | 36 (36.6) | 2.25 (0.1338) |
| Excessive | 590 (79.2) | 151 (20.8) | 327 (54.2) | 275 (45.8) | |||
| Variable | Category | BMI, kg/m2 | |||
|---|---|---|---|---|---|
| <25 | ≥25 | ||||
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | ||
| Age, years | 1.04 (1.00–1.09) | 0.0434 | 1.06 (1.02–1.11) | 0.0030 | |
| Education (Ref: High school or below) | College or above | 1.05 (0.68–1.64) | 0.8187 | 1.01 (0.65,1.60) | 0.9692 |
| Income (Ref: 1st quartile) | 2nd quartile | 0.65 (0.36–1.18) | 0.4318 | 0.97 (0.59–1.60) | 0.4869 |
| 3rd quartile | 0.71 (0.40–1.28) | 0.69 (0.41–1.17) | |||
| 4th quartile | 0.67 (0.39–1.16) | 0.97 (0.58–1.63) | |||
| Body image perception (Ref: Skinny) | Normal | 1.89 (1.12–3.18) | 0.0093 | - | 0.7979 |
| Overweight | 2.66 (1.40–5.08) | 0.92 (0.49–1.73) 1 | |||
| Stress (Ref: No) | Yes | 1.64 (1.05–2.59) | 0.0329 | 1.05 (0.71–1.54) | 0.8226 |
| Subjective health (Ref: Good) | Normal | 0.76 (0.50–1.18) | 0.3419 | 0.80 (0.54–1.18) | 0.1721 |
| Bad | 1.22 (0.55–2.71) | 1.21 (0.68–2.14) | |||
| Drinking (Ref: No) | Moderate | 1.13 (0.57–2.23) | 0.4187 | 0.66 (0.35–1.23) | 0.2442 |
| Heavy | 0.71 (0.29–1.77) | 0.52 (0.24–1.12) | |||
| Smoking (Ref: No) | Yes | 1.17 (0.77–1.79) | 0.4668 | 1.21 (0.77–1.90) | 0.4082 |
| Walking (Ref: No) | Yes | 0.78 (0.51–1.18) | 0.2332 | 0.72 (0.50–1.05) | 0.0886 |
| Muscle exercise (Ref: No) | Yes | 0.89 (0.57–1.37) | 0.5864 | 0.980 (0.65–1.48) | 0.9273 |
| Aerobic exercise (Ref: No) | Yes | 0.81 (0.53–1.26) | 0.3515 | 0.91 (0.61–1.35) | 0.6332 |
| Sleep (Ref: Normal) | Insufficient | 1.08 (0.68–1.73) | 0.7342 | 1.09 (0.74–1.60) | 0.6571 |
| Working hours, minutes | 1.00 (0.99–1.01) | 0.7310 | 1.00 (0.99–1.01) | 0.9967 | |
| Waist circumference (Ref: <90 cm) | ≥90 cm | 7.48 (2.70–20.79) | <0.001 | 1.69 (1.08–2.64) | 0.0231 |
| Energy intake (Ref: Normal) | Excessive | 0.92 (0.44–1.90) | 0.8119 | 1.04 (0.54–2.02) | 0.9005 |
| Fat intake (Ref: Normal) | Excessive | 1.20 (0.71–2.03) | 0.5049 | 0.96 (0.56–1.63) | 0.8763 |
| Carbohydrate intake (Ref: Normal) | Excessive | 0.78 (0.41–1.49) | 0.4512 | 1.16 (0.65–2.06) | 0.6140 |
| Sodium intake (Ref: Normal) | Excessive | 1.06 (0.61–1.84) | 0.8434 | 1.18 (0.68–2.04) | 0.5611 |
| Model fit measures | Nagelkerke R2 | 0.137 | 0.101 | ||
| Concordant pairs (%) | 67.8 | 65.1 | |||
| AUC (95% CI) | 0.680 (0.636–0.724) | 0.652 (0.612–0.693) | |||
| Accuracy | 0.803 | 0.609 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, M.; Kim, J.; Cha, E. Obesity-Status-Linked Affecting Factors of Dyslipidemia in Korean Young-Adult Men: Based on the Korea National Health and Nutrition Examination Survey (2019–2021). Healthcare 2023, 11, 2015. https://doi.org/10.3390/healthcare11142015
Kwon M, Kim J, Cha E. Obesity-Status-Linked Affecting Factors of Dyslipidemia in Korean Young-Adult Men: Based on the Korea National Health and Nutrition Examination Survey (2019–2021). Healthcare. 2023; 11(14):2015. https://doi.org/10.3390/healthcare11142015
Chicago/Turabian StyleKwon, Min, Jinheum Kim, and Eunjeong Cha. 2023. "Obesity-Status-Linked Affecting Factors of Dyslipidemia in Korean Young-Adult Men: Based on the Korea National Health and Nutrition Examination Survey (2019–2021)" Healthcare 11, no. 14: 2015. https://doi.org/10.3390/healthcare11142015
APA StyleKwon, M., Kim, J., & Cha, E. (2023). Obesity-Status-Linked Affecting Factors of Dyslipidemia in Korean Young-Adult Men: Based on the Korea National Health and Nutrition Examination Survey (2019–2021). Healthcare, 11(14), 2015. https://doi.org/10.3390/healthcare11142015






