Can the Day of the Week and the Time of Birth Predict the Mode of Delivery According to Robson Classification?
Abstract
:1. Introduction
2. Materials and Methods
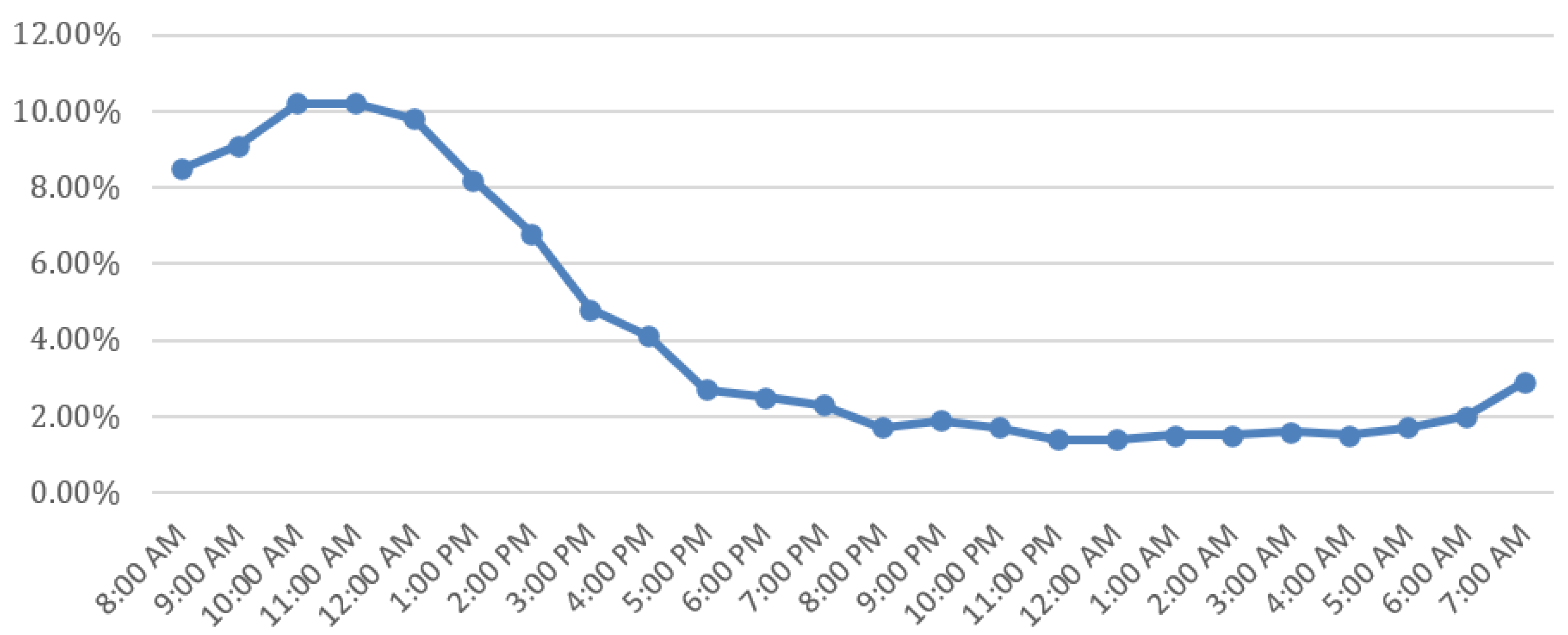
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pettker, C.M.; Grobman, W.A. Obstetric Safety and Quality. Obstet. Gynecol. 2015, 126, 196–206. [Google Scholar] [CrossRef]
- Gibbons, L.; Belizán, J.; Lauer, J.; Betrán, A.; Merialdi, M.; Althabe, F. The global numbers and costs of additionally needed and unnecessary caesarean sections performed per year: Overuse as a barrier to universal coverage. World Health Rep. 2010, 30, 1–31. [Google Scholar]
- Ye, J.; Betrán, A.P.; Vela, M.G.; Souza, J.P.; Zhang, J. Searching for the Optimal Rate of Medically Necessary Cesarean Delivery. Birth 2014, 41, 237–244. [Google Scholar] [CrossRef]
- Souza, J.; the WHO Global Survey on Maternal and Perinatal Health Research Group; Gülmezoglu, A.; Lumbiganon, P.; Laopaiboon, M.; Carroli, G.; Fawole, B.; Ruyan, P. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: The 2004–2008 WHO Global Survey on Maternal and Perinatal Health. BMC Med. 2010, 8, 71. [Google Scholar] [CrossRef] [Green Version]
- Betrán, A.P.; Ye, J.; Moller, A.-B.; Zhang, J.; Gülmezoglu, A.M.; Torloni, M.R. The Increasing Trend in Caesarean Section Rates: Global, Regional and National Estimates: 1990–2014. PLoS ONE 2016, 11, e0148343. [Google Scholar] [CrossRef] [Green Version]
- Le Ray, C.; Blondel, B.; Prunet, C.; Khireddine, I.; Deneux-Tharaux, C.; Goffinet, F. Stabilising the caesarean rate: Which target population? BJOG Int. 2015, 122, 690–699. [Google Scholar] [CrossRef]
- Brennan, D.J.; Murphy, M.; Robson, M.S.; O’Herlihy, C. The Singleton, Cephalic, Nulliparous Woman after 36 Weeks of Gestation: Contribution to Overall Cesarean Delivery Rates. Obstet. Gynecol. 2011, 117 Pt 1, 273–279. [Google Scholar] [CrossRef]
- Betran, A.; Torloni, M.R.; Zhang, J.; Gülmezoglu, A.; Aleem, H.; Althabe, F.; Bergholt, T.; Bernis, L.; Carroli, G.; Deneux-Tharaux, C.; et al. WHO Statement on Caesarean Section Rates. BJOG 2016, 123, 667–670. [Google Scholar] [CrossRef]
- Betran, A.P.; Ye, J.; Moller, A.-B.; Souza, J.P.; Zhang, J. Trends and projections of caesarean section rates: Global and regional estimates. BMJ Glob. Health 2021, 6, e005671. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Human Reproduction Programme, 10 April 2015 WHO Statement on caesarean section rates. Reprod. Health Matters 2015, 23, 149–150. [CrossRef] [PubMed] [Green Version]
- World Health Organization. Robson Classification: Implementation Manual; WHO: Geneva, Switzerland, 2017; Available online: https://www.who.int/publications/i/item/9789241513197 (accessed on 22 April 2023).
- Ye, J.; Zhang, J.; Mikolajczyk, R.; Torloni, M.R.; Gülmezoglu, A.; Betran, A. Association between rates of caesarean section and maternal and neonatal mortality in the 21st century: A worldwide population-based ecological study with longitudinal data. BJOG 2016, 123, 745–753. [Google Scholar] [CrossRef] [Green Version]
- Betran, A.P.; Torloni, M.R.; Zhang, J.; Ye, J.; Mikolajczyk, R.; Deneux-Tharaux, C.; Oladapo, O.T.; Souza, J.P.; Tunçalp, Ö.; Vogel, J.P.; et al. What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reprod. Health 2015, 12, 57. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mylonas, I.; Friese, K. Indications for and Risks of Elective Cesarean Section. DtschArztebl Int. 2015, 112, 489–495. [Google Scholar] [CrossRef] [Green Version]
- Aminu, M.; Utz, B.; Halim, A.; Broek, N.V.D. Reasons for performing a caesarean section in public hospitals in rural Bangladesh. BMC Pregnancy Childbirth 2014, 14, 130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oner, C.; Catak, B.; Sütlü, S.; Kilinç, S. Effect of Social Factors on Cesarean Birth in Primiparous Women: A Cross Sectional Study (Social Factors and Cesarean Birth). Iran. J. Public Health 2016, 45, 768–773. [Google Scholar] [PubMed]
- Feng, X.L.; Xu, L.; Guo, Y.; Ronsmans, C. Factors influencing rising caesarean section rates in China between 1988 and 2008. Bull. World Health Organ. 2012, 90, 30A–39A. [Google Scholar] [CrossRef]
- Bernis, C.; Varea, C. Hour of birth and birth assistance: From a primate to a medicalized pattern? Am. J. Hum. Biol. 2011, 24, 14–21. [Google Scholar] [CrossRef]
- Camargo, C.C.; Ferrari, S.F. Observations of daytime births in two groups of red-handed howlers (Alouatta belzebul) on an Island in the tucuruí reservoir in Eastern Brazilian Amazonia. Am. J. Primatol. 2007, 69, 1075–1079. [Google Scholar] [CrossRef]
- Honnebier, M.; Nathanielsz, P. Primate parturition and the role of the maternal circadian system. Eur. J. Obstet. Gynecol. Reprod. Biol. 1994, 55, 193–203. [Google Scholar] [CrossRef]
- Trevathan, W.R. Human Birth: An Evolutionary Perspective; Aldine de Gruyter: New York, NY, USA, 1987. [Google Scholar]
- Martin, R.D. The evolution of human reproduction: A primatological perspective. Am. J. Phys. Anthr. 2007, 134, 59–84. [Google Scholar] [CrossRef]
- Burns, L.R.; Geller, S.E.; Wholey, D.R. The Effect of Physician Factors on the Cesarean Section Decision. Med. Care 1995, 33, 365–382. [Google Scholar] [CrossRef]
- Evans, M.I.; Richardson, D.A.; Sholl, J.S.; Johnson, B.A. Cesarean section. Assessment of the convenience factor. J. Reprod. Med. 1984, 29, 676. [Google Scholar]
- Giaxi, P.; Gourounti, K.; Vivilaki, V.; Zdanis, P.; Galanos, A.; Antsaklis, A.; Lykeridou, A. Implementation of the Robson Classification in Greece: A Retrospective Cross-Sectional Study. Healthcare 2023, 11, 908. [Google Scholar] [CrossRef] [PubMed]
- Hoxha, I.; Syrogiannouli, L.; Luta, X.; Tal, K.; Goodman, D.C.; Da Costa, B.R.; Jüni, P. Caesarean sections and for-profit status of hospitals: Systematic review and meta-analysis. BMJ Open 2017, 7, e013670. [Google Scholar] [CrossRef] [Green Version]
- Gruber, J.; Kim, J.; Mayzlin, D. Physician fees and procedure intensity: The case of cesarean delivery. J. Health Econ. 1999, 18, 473–490. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mossialos, E.; Allin, S.; Karras, K.; Davaki, K. An investigation of Caesarean sections in three Greek hospitals: The impact of financial incentives and convenience. Eur. J. Public Health 2005, 15, 288–295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- del Carmen, G.A.; Stapleton, S.; Qadan, M.; del Carmen, M.G.; Chang, D. Does the Day of the Week Predict a Cesarean Section? A Statewide Analysis. J. Surg. Res. 2020, 245, 288–294. [Google Scholar] [CrossRef] [Green Version]
- Knight, H.E.; van der Meulen, J.H.; Gurol-Urganci, I.; Smith, G.C.; Kiran, A.; Thornton, S.; Richmond, D.; Cameron, A.; Cromwell, D.A. Birth “Out-of-Hours”: An Evaluation of Obstetric Practice and Outcome According to the Presence of Senior Obstetricians on the Labour Ward. PLOS Med. 2016, 13, e1002000. [Google Scholar] [CrossRef] [Green Version]
- Windsperger, K.; Kiss, H.; Oberaigner, W.; Leitner, H.; Muin, D.A.; Husslein, P.W.; Farr, A. Working-hour phenomenon in obstetrics is an attainable target to improve neonatal outcomes. Am. J. Obstet. Gynecol. 2019, 221, 257.e1–257.e9. [Google Scholar] [CrossRef]
- Kanwar, S.; Rabindran, R.; Lindow, S.W. Delivery outcomes after day and night onset of labour. J. Perinat. Med. 2015, 43, 729–733. [Google Scholar] [CrossRef]
- Schulz, P.; Steimer, T. Neurobiology of Circadian Systems. CNS Drugs 2009, 23, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Lindow, S.W.; Newham, A.; Hendricks, M.S.; Thompson, J.W.; Van Der Spuy, Z.M. The 24-hour rhythm of oxytocin and Β-endorphin secretion in human pregnancy. Clin. Endocrinol. 1996, 45, 443–446. [Google Scholar] [CrossRef] [PubMed]
- Charitou, A.; Charos, D.; Vamenou, I.; Vivilaki, V.G. Maternal and neonatal outcomes for women giving birth after previous cesarean. Eur. J. Midwifery 2019, 3, 8. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Frequency (n) | Percentage (%) | |
|---|---|---|---|
| Maternal age (years) | mean ± SD (Min, Max) | 34.16 ± 4.90 (17–52) | |
| <20 | 16 | 0.2 | |
| 20–29 | 1392 | 16.2 | |
| 30–39 | 6084 | 71.0 | |
| ≥40 | 1080 | 12.6 | |
| Nationality | Other | 464 | 5.4 |
| Greek | 8108 | 94.6 | |
| Gestational age (weeks) | <37+0 | 1160 | 13.5 |
| 37+0–38+6 | 4039 | 47.1 | |
| 39+0–41+6 | 3367 | 39.3 | |
| ≥42+0 | 6 | 0.1 | |
| Type of pregnancy | Single | 8194 | 95.6 |
| Multiple | 378 | 4.4 | |
| Parity | 0 | 4938 | 57.6 |
| 1 | 3030 | 35.3 | |
| ≥2 | 604 | 7.0 | |
| Mode of delivery | Vaginal delivery | 2620 | 30.6 |
| Operative vaginal delivery | 728 | 8.5 | |
| Cesarean section | 5224 | 60.9 | |
| Newborn’s sex | Male | 4596 | 51.4 |
| Female | 4351 | 48.6 | |
| Newborn’s birth weight (g) | <2500 | 1055 | 11.8 |
| 2500–2999 | 2234 | 25.0 | |
| 3000–3999 | 5397 | 60.3 | |
| ≥4000 | 261 | 2.9 | |
| Mode of Delivery | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Vaginal Delivery | Operative Vaginal Delivery | Cesarean Section | Total | ||||||
| Count | % within Robson | Count | % within Robson | Count | % within Robson | Count | % within Robson | ||
| Robson Class | 1 | 390 | 42.0% | 179 | 19.3% | 359 | 38.7% | 928 | 10.8 |
| 2a | 793 | 46.4% | 358 | 20.9% | 558 | 32.7% | 1709 | 20.0 | |
| 2b | 0 | 0.0% | 0 | 0.0% | 1247 | 100.0% | 1247 | 14.5 | |
| 3 | 330 | 88.7% | 30 | 8.1% | 12 | 3.2% | 372 | 4.3 | |
| 4a | 904 | 89.8% | 83 | 8.2% | 20 | 2.0% | 1007 | 11.7 | |
| 4b | 0 | 0.0% | 0 | 0.0% | 29 | 100.0% | 29 | 0.3 | |
| 5.1 | 60 | 4.0% | 40 | 2.7% | 1387 | 93.3% | 1487 | 17.3 | |
| 5.2 | 2 | 0.9% | 0 | 0.0% | 213 | 99.1% | 215 | 2.5 | |
| 6 | 1 | 0.4% | 1 | 0.4% | 278 | 99.3% | 280 | 3.3 | |
| 7 | 1 | 0.9% | 3 | 2.8% | 102 | 96.2% | 106 | 1.2 | |
| 8 | 7 | 1.8% | 5 | 1.3% | 367 | 96.8% | 379 | 4.4 | |
| 9 | 0 | 0.0% | 0 | 0.0% | 43 | 100.0% | 43 | 0.5 | |
| 10 | 132 | 17.1% | 29 | 3.8% | 609 | 79.1% | 770 | 9.0 | |
| Robson Classification | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Day Distribution | 1 | 2a | 2b | 3 | 4a | 4b | 5.1 | 5.2 | 6 | 7 | 8 | 9 | 10 |
| Ν (%) | Ν (%) | Ν (%) | Ν (%) | Ν (%) | Ν (%) | Ν (%) | Ν (%) | Ν (%) | Ν (%) | Ν (%) | Ν (%) | Ν (%) | |
| Monday | 101 (13.5) | 176 (13.0) | 157 (12.6) | 50 (14.6) | 83 (9.0) | 4 (13.8) | 255 (15.5) | 33 (15.3) | 34 (12.2) | 13 (12.6) | 52 (13.9) | 4 (9.3) | 103 (13.9) |
| Tuesday | 103 (13.8) | 237 (17.5) | 254 (20.4) | 59 (17.2) | 148 (16.0) | 6 (20.7) | 248 (17.1) | 40 (18.6) | 38 (13.6) | 15 (14.6) | 73 (19.5) | 7 (16.3) | 112 (15.1) |
| Wednesday | 115 (15.4) | 209 (15.5) | 164 (13.2) | 53 (15.5) | 149 (16.1) | 6 (20.7) | 204 (14.1) | 28 (13.0) | 38 (13.6) | 10 (9.7) | 44 (11.8) | 4 (9.3) | 104 (14.0) |
| Thursday | 97 (13.0) | 183 (13.5) | 216 (17.3) | 32 (9.3) | 139 (15.0) | 4 (13.8) | 247 (17.1) | 44 (20.5) | 51 (18.3) | 18 (17.5) | 66 (17.6) | 13 (30.2) | 134 (18.1) |
| Friday | 131 (17.5) | 293 (21.7) | 264 (21.2) | 64 (18.2) | 199 (21.5) | 5 (17.2) | 309 (21.4) | 40 (18.6) | 61 (21.9) | 29 (28.2) | 69 (18.4) | 6 (14.0) | 115 (15.5) |
| Saturday | 111 (14.8) | 173 (12.8) | 171 (13.7) | 42 (12.2) | 138 (14.9) | 4 (13.8) | 165(11.4) | 20 (9.3) | 40 (14.3) | 15 (14.6) | 47 (12.6) | 8 (16.8) | 112 (15.1) |
| Sunday | 91 (12.1) | 81 (6.0) | 21 (1.7) | 43 (12.5) | 71 (7.7) | 0 (0) | 49(3.4) | 10 (4.7) | 17 (6.1) | 3 (2.9) | 23 (6.1) | 1 (2.3) | 61 (8.2) |
| Mode of Delivery | Total | ||||
|---|---|---|---|---|---|
| Vaginal Delivery | Cesarean Section | ||||
| Time period | 12:00 A.M.–07:59 A.M. | Count | 644 | 457 | 1101 |
| % within ΤΙΜΕ | 58.5% | 41.5% | 100.0% | ||
| 08:00 A.M.–03:59 P.M. | Count | 1328 | 3983 | 5311 | |
| % within ΤΙΜΕ | 25.0% | 75.0% | 100.0% | ||
| 04:00 P.M.–11:59 P.M. | Count | 653 | 784 | 1437 | |
| % within ΤΙΜΕ | 45.4% | 54.6% | 100.0% | ||
| Total | Count | 2625 | 5224 | 7849 | |
| % within ΤΙΜΕ | 33.4% | 66.6% | 100.0% | ||
| Robson Class | Delivery | p-Value | |||||
|---|---|---|---|---|---|---|---|
| Vaginal Delivery | Cesarean Section | ||||||
| N | % | N | % | ||||
| 1 | Τime period | 12:00 A.M.–07:59 A.M. | 128 | 63.7% | 73 | 36.3% | <0.005 |
| 08:00 A.M.–03:59 P.M. | 170 | 50.3% | 168 | 49.7% | |||
| 04:00 P.M.–11:59 P.M. | 92 | 43.8% | 118 | 56.2% | |||
| 2a | Τime period | 12:00 A.M.–07:59 A.M. | 142 | 75.9% | 45 | 24.1% | <0.005 |
| 08:00 A.M.–03:59 P.M. | 410 | 59.2% | 283 | 40.8% | |||
| 04:00 P.M.–11:59 P.M. | 242 | 51.3% | 230 | 48.7% | |||
| 2b | Τime period | 12:00 A.M.–07:59 A.M. | - | - | 54 | 100.0% | --- |
| 08:00 A.M.–03:59 P.M. | - | - | 1126 | 100.0% | |||
| 04:00 P.M.–11:59 P.M. | - | - | 67 | 100.0% | |||
| 3 | Τime period | 12:00 A.M.–07:59 A.M. | 133 | 97.8% | 3 | 2.2% | --- |
| 08:00 A.M.–03:59 P.M. | 133 | 96.4% | 5 | 3.6% | |||
| 04:00 P.M.–11:59 P.M. | 65 | 94.2% | 4 | 5.8% | |||
| 4a | Τime period | 12:00 A.M.–07:59 A.M. | 176 | 98.3% | 3 | 1.7% | --- |
| 08:00 A.M.–03:59 P.M. | 546 | 98.7% | 7 | 1.3% | |||
| 04:00 P.M.–11:59 P.M. | 185 | 94.9% | 10 | 5.1% | |||
| 4b | Τime period | 08:00 A.M.–03:59 P.M. | - | - | 26 | 100.0% | --- |
| 04:00 P.M.–11:59 P.M. | - | - | 3 | 100.0% | |||
| 5.1 | Τime period | 12:00 A.M.–07:59 A.M. | 21 | 20.0% | 84 | 80.0% | <0.005 |
| 08:00 A.M.–03:59 P.M. | 18 | 1.5% | 1201 | 98.5% | |||
| 04:00 P.M.–11:59 P.M. | 21 | 17.1% | 102 | 82.9% | |||
| 5.2 | Τime period | 12:00 A.M.–07:59 A.M. | 2 | 13.3% | 13 | 86.7% | --- |
| 08:00 A.M.–03:59 P.M. | 0 | 0.0% | 184 | 100.0% | |||
| 04:00 P.M.–11:59 P.M. | 0 | 0.0% | 16 | 100.0% | |||
| 6 | Τime period | 12:00 A.M.–07:59 A.M. | 1 | 2.4% | 40 | 97.6% | --- |
| 08:00 A.M.–03:59 P.M. | 0 | 0.0% | 207 | 100.0% | |||
| 04:00 P.M.–11:59 P.M. | 0 | 0.0% | 31 | 100.0% | |||
| 7 | Τime period | 12:00 A.M.–07:59 A.M. | 1 | 11.1% | 8 | 88.9% | --- |
| 08:00 A.M.–03:59 P.M. | 0 | 0.0% | 77 | 100.0% | |||
| 04:00 P.M.–11:59 P.M. | 0 | 0.0% | 17 | 100.0% | |||
| 8 | Τime period | 12:00 A.M.–07:59 A.M. | 1 | 2.0% | 48 | 98.0% | --- |
| 08:00 A.M.–03:59 P.M. | 3 | 1.1% | 260 | 98.9% | |||
| 04:00 P.M.–11:59 P.M. | 3 | 4.8% | 59 | 95.2% | |||
| 9 | Τime period | 12:00 A.M.–07:59 A.M. | - | - | 4 | 100.0% | --- |
| 08:00 A.M.–03:59 P.M. | - | - | 36 | 100.0% | |||
| 04:00 P.M.–11:59 P.M. | - | - | 3 | 100.0% | |||
| 10 | Τime period | 12:00 A.M.–07:59 A.M. | 39 | 32.2% | 82 | 67.8% | <0.005 |
| 08:00 A.M.–03:59 P.M. | 48 | 10.6% | 403 | 89.4% | |||
| 04:00 P.M.–11:59 P.M. | 45 | 26.6% | 124 | 73.4% | |||
| Crude OR | 95% CI | p-Value | Adjusted OR | 95% CI | p-Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Τime Period | |||||||||
| Total | <0.005 | <0.005 | |||||||
| 12:00 A.M.–07:59 A.M. | 1.00 | 1.00 | |||||||
| 08:00 A.M.–03:59 P.M. | 4.23 | 3.69 | 4.84 | <0.005 | 4.53 | 3.93 | 5.24 | <0.005 | |
| 04:00 P.M.–11:59 P.M. | 1.69 | 1.44 | 1.98 | <0.005 | 1.98 | 1.67 | 2.34 | <0.005 | |
| Robson 1 | <0.005 | <0.005 | |||||||
| 12:00 A.M.–07:59 A.M. | 1.00 | 1.00 | |||||||
| 08:00 A.M.–03:59 P.M. | 1.73 | 1.21 | 2.47 | <0.005 | 1.76 | 1.22 | 2.54 | <0.005 | |
| 04:00 P.M.–11:59 P.M. | 2.25 | 1.51 | 3.34 | <0.005 | 2.35 | 1.57 | 3.53 | <0.005 | |
| Robson 2a | <0.005 | <0.005 | |||||||
| 12:00 A.M.–07:59 A.M. | 1.00 | 1.00 | |||||||
| 08:00 A.M.–03:59 P.M. | 2.18 | 1.51 | 3.14 | <0.005 | 2.10 | 1.44 | 1.86 | <0.005 | |
| 04:00 P.M.–11:59 P.M. | 3.00 | 2.05 | 4.38 | <0.005 | 2.79 | 1.89 | 4.12 | <0.005 | |
| Robson 5.1 | <0.005 | <0.005 | |||||||
| 12:00 A.M.–07:59 A.M. | 1.00 | 1.00 | |||||||
| 08:00 A.M.–03:59 P.M. | 16.68 | 8.56 | 32.50 | <0.005 | 19.17 | 8.98 | 40.90 | <0.005 | |
| 04:00 P.M.–11:59 P.M. | 1.21 | 0.62 | 2.37 | 0.570 | 1.85 | 0.83 | 4.12 | 0.133 | |
| Robson 10 | <0.005 | <0.005 | |||||||
| 12:00 A.M.–07:59 A.M. | 1.00 | 1.00 | |||||||
| 08:00 A.M.–03:59 P.M. | 4.00 | 2.46 | 6.48 | <0.005 | 4.12 | 2.51 | 6.78 | <0.0005 | |
| 04:00 P.M.–11:59 P.M. | 1.31 | 0.79 | 2.18 | 0.300 | 1.54 | 0.91 | 2.62 | 0.111 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giaxi, P.; Gourounti, K.; Vivilaki, V.; Metallinou, D.; Zdanis, P.; Galanos, A.; Lykeridou, A. Can the Day of the Week and the Time of Birth Predict the Mode of Delivery According to Robson Classification? Healthcare 2023, 11, 2158. https://doi.org/10.3390/healthcare11152158
Giaxi P, Gourounti K, Vivilaki V, Metallinou D, Zdanis P, Galanos A, Lykeridou A. Can the Day of the Week and the Time of Birth Predict the Mode of Delivery According to Robson Classification? Healthcare. 2023; 11(15):2158. https://doi.org/10.3390/healthcare11152158
Chicago/Turabian StyleGiaxi, Paraskevi, Kleanthi Gourounti, Victoria Vivilaki, Dimitra Metallinou, Panagiotis Zdanis, Antonis Galanos, and Aikaterini Lykeridou. 2023. "Can the Day of the Week and the Time of Birth Predict the Mode of Delivery According to Robson Classification?" Healthcare 11, no. 15: 2158. https://doi.org/10.3390/healthcare11152158
APA StyleGiaxi, P., Gourounti, K., Vivilaki, V., Metallinou, D., Zdanis, P., Galanos, A., & Lykeridou, A. (2023). Can the Day of the Week and the Time of Birth Predict the Mode of Delivery According to Robson Classification? Healthcare, 11(15), 2158. https://doi.org/10.3390/healthcare11152158







