The Use of 3D Technology in the Management of Residual Asymmetry following Orthognathic Surgery: A Case Report
Abstract
:1. Introduction
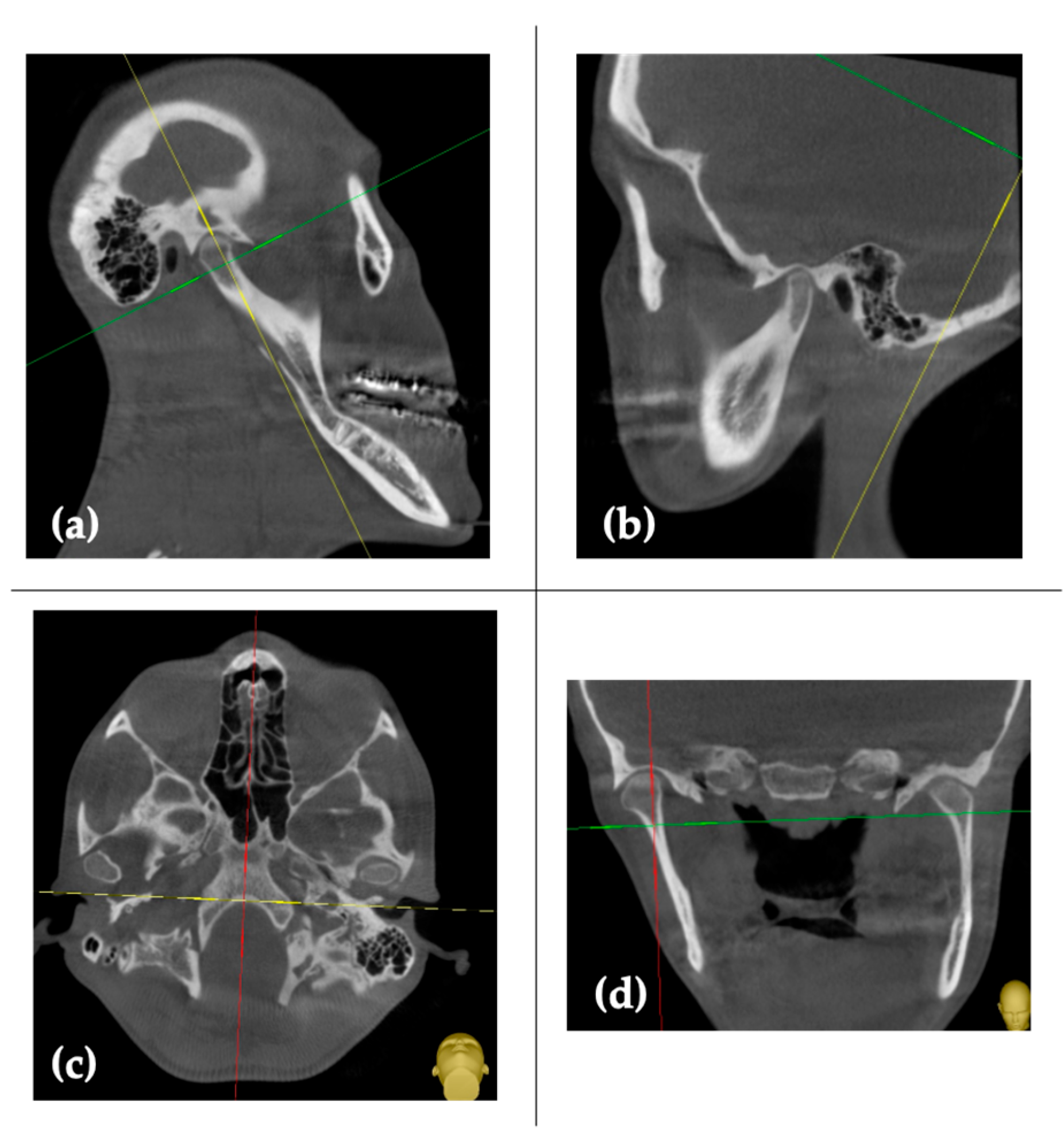
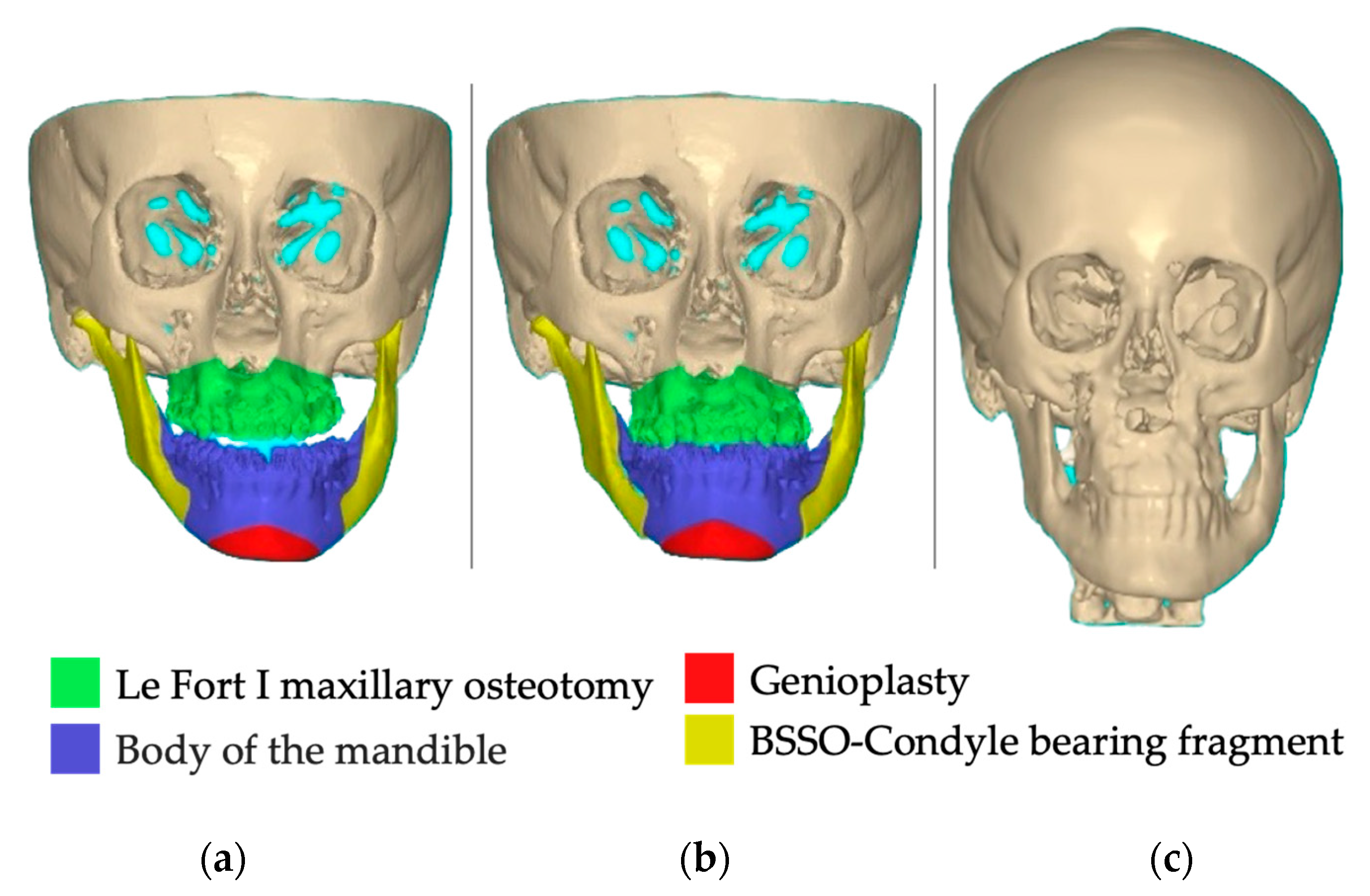
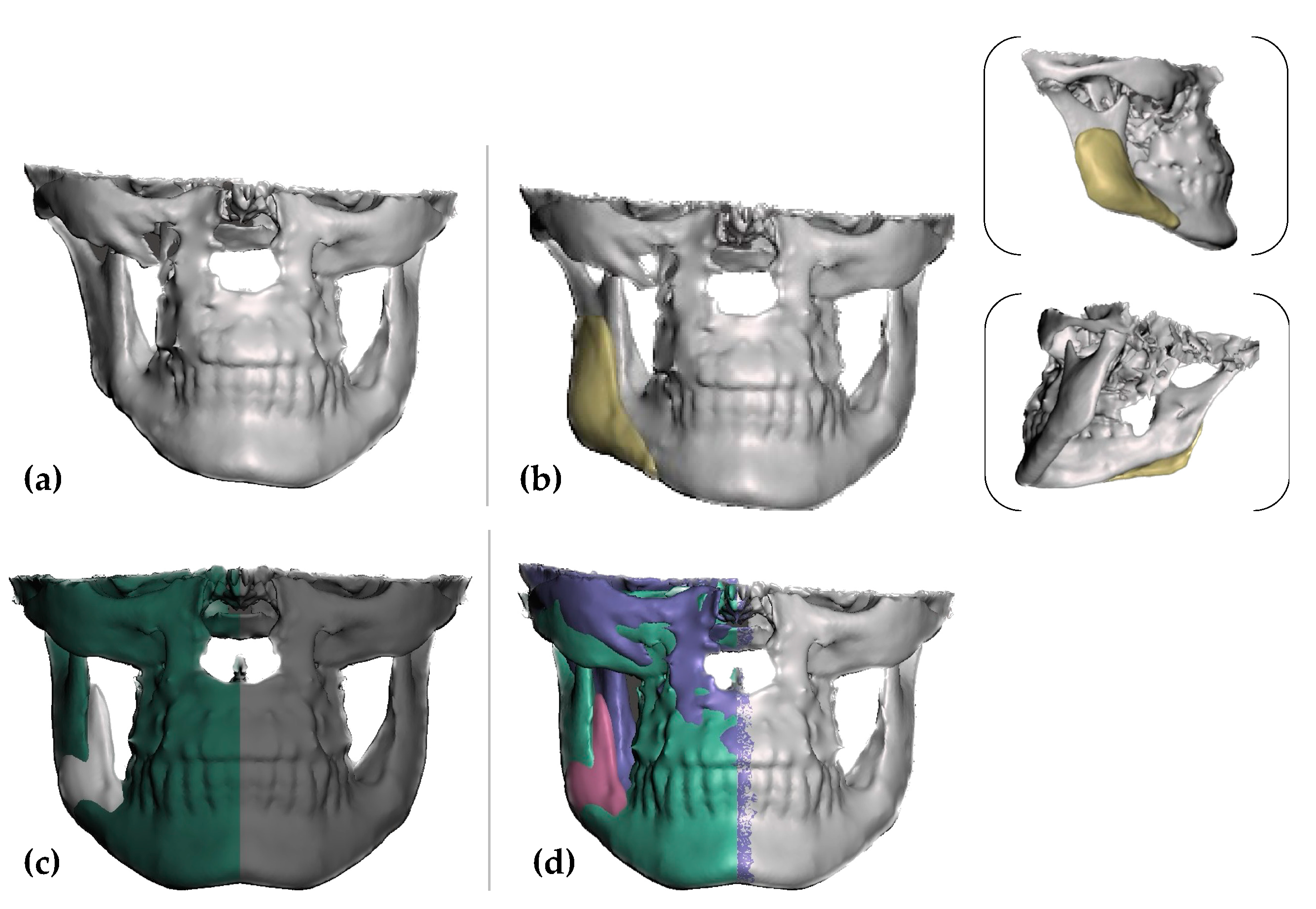
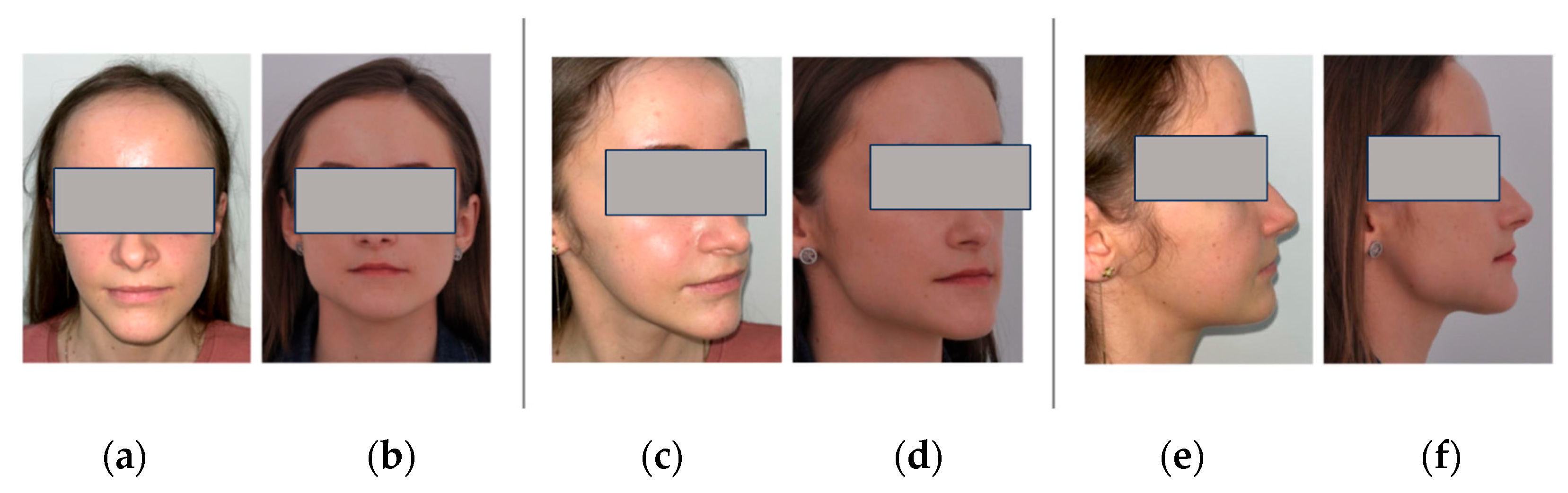
2. Case Report
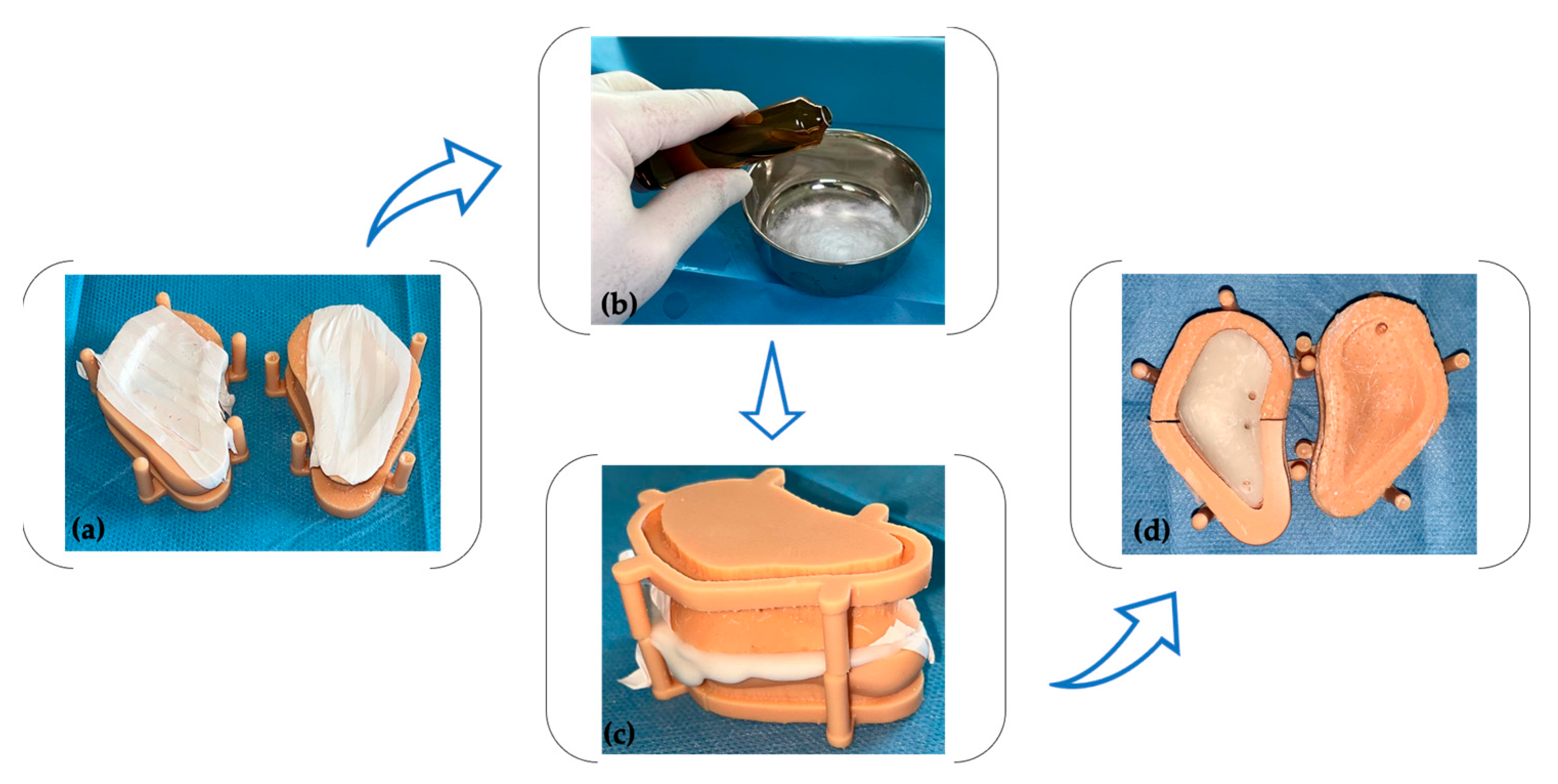
2.1. PSI’s Mold Design and Fabrication
2.2. Surgical Procedure
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kronmiller, J.E. Development of asymmetries. Semin. Orthod. 1998, 4, 134–137. [Google Scholar] [CrossRef] [PubMed]
- Bailey, L.J.; Collie, F.M.; White, R.P., Jr. Long-term soft tissue changes after orthognathic surgery. Int. J. Adult Orthod. Orthognath. Surg. 1996, 11, 7–18. [Google Scholar]
- Betts, N.J.; Dowd, K.F. Soft tissue changes associated with orthognathic surgery. Atlas Oral Maxillofac. Surg. Clin. 2000, 8, 13–38. [Google Scholar] [CrossRef]
- Jung, J.; Lee, C.H.; Lee, J.W.; Choi, B.J. Three dimensional evaluation of soft tissue after orthognathic surgery. Head Face Med. 2018, 14, 21. [Google Scholar] [CrossRef]
- Zinser, M.J.; Mischkowski, R.A.; Sailer, H.F.; Zöller, J.E. Computer-assisted orthognathic surgery: Feasibility study using multiple CAD/CAM surgical splints. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 113, 673–687. [Google Scholar] [CrossRef]
- Cheong, Y.W.; Lo, L.J. Facial asymmetry: Etiology, evaluation, and management. Chang. Gung Med. J. 2011, 34, 341–351. [Google Scholar]
- Suojanen, J.; Leikola, J.; Stoor, P. The use of patient-specific implants in orthognathic surgery: A series of 32 maxillary osteotomy patients. J. Cranio-Maxillofac. Surg. 2016, 44, 1913–1916. [Google Scholar] [CrossRef] [Green Version]
- Suojanen, J.; Leikola, J.; Stoor, P. The use of patient-specific implants in orthognathic surgery: A series of 30 mandible sagittal split osteotomy patients. J. Cranio-Maxillofac. Surg. 2017, 45, 990–994. [Google Scholar] [CrossRef] [Green Version]
- Rammos, C.K.; Cayci, C.; Castro-Garcia, J.A.; Feiz-Erfan, I.; Lettieri, S.C. Patient-specific polyetheretherketone implants for repair of craniofacial defects. J. Craniofacial Surg. 2015, 26, 631–633. [Google Scholar] [CrossRef] [Green Version]
- Jalbert, F.; Boetto, S.; Nadon, F.; Lauwers, F.; Schmidt, E.; Lopez, R. One-step primary reconstruction for complex craniofacial resection with PEEK custom-made implants. J. Cranio-Maxillofac. Surg. 2014, 42, 141–148. [Google Scholar] [CrossRef]
- Binder, W.J. Custom-designed facial implants. Facial Plast. Surg. Clin. North Am. 2008, 16, 133–146. [Google Scholar] [CrossRef] [PubMed]
- Ridwan-Pramana, A.; Wolff, J.; Raziei, A.; Ashton-James, C.E.; Forouzanfar, T. Porous polyethylene implants in facial reconstruction: Outcome and complications. J. Craniomaxillofac. Surg. 2015, 43, 1330–1334. [Google Scholar] [CrossRef]
- Soleymani Eil Bakhtiari, S.; Bakhsheshi-Rad, H.R.; Karbasi, S.; Tavakoli, M.; Razzaghi, M.; Ismail, A.F.; RamaKrishna, S.; Berto, F. Polymethyl Methacrylate-Based Bone Cements Containing Carbon Nanotubes and Graphene Oxide: An Overview of Physical, Mechanical, and Biological Properties. Polymers 2020, 12, 1469. [Google Scholar] [CrossRef] [PubMed]
- Dukle, A.; Murugan, D.; Nathanael, A.J.; Rangasamy, L.; Oh, T.H. Can 3D-Printed Bioactive Glasses Be the Future of Bone Tissue Engineering? Polymers 2022, 14, 1627. [Google Scholar] [CrossRef] [PubMed]
- Jean, W.C.; Huang, M.C.; Felbaum, D.R. Optimization of skull base exposure using navigation-integrated, virtual reality templates. J. Clin. Neurosci. 2020, 80, 125–130. [Google Scholar] [CrossRef]
- Slimani, M.; Baus, A.; Bich, C.S.; de Rousiers, A.; Duhoux, A.; Brachet, M.; Duhamel, P.; Bey, E. Methylmetacrylate (PMMA) cranioplasty technique: Technical interest of intraoperative modeling and review of the literature. Ann. Chir. Plast. Esthet. 2023, 68, 99–105. [Google Scholar] [CrossRef]
- Lye, K.W.; Tideman, H.; Merkx, M.A.; Jansen, J.A. Bone cements and their potential use in a mandibular endoprosthesis. Tissue Eng. Part. B Rev. 2009, 15, 485–496. [Google Scholar] [CrossRef] [Green Version]
- Mommaerts, M.Y. Guidelines for patient-specific jawline definition with titanium implants in esthetic, deformity, and malformation surgery. Ann. Maxillofac. Surg. 2016, 6, 287–291. [Google Scholar] [CrossRef] [Green Version]
- Goldsmith, D.; Horowitz, A.; Orentlicher, G. Facial skeletal augmentation using custom facial implants. Atlas Oral. Maxillofac. Surg. Clin. 2012, 20, 119–134. [Google Scholar] [CrossRef]
- Möllmann, H.L.; Apeltrath, L.; Karnatz, N.; Wilkat, M.; Riedel, E.; Singh, D.D.; Rana, M. Comparison of the Accuracy and Clinical Parameters of Patient-Specific and Conventionally Bended Plates for Mandibular Reconstruction. Front. Oncol. 2021, 11, 719028. [Google Scholar] [CrossRef]
- Shetty, S.R.; Al-Bayatti, S.; AlKawas, S.; Talaat, W.; Narasimhan, S.; Gaballah, K.; Al-Rawi, N.; Alsaegh, M.; Madiyal, A.; Balan, P.; et al. Analysis of the Volumetric Asymmetry of the Mandibular Condyles Using CBCT. Int. Dent. J. 2022, 72, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Shetty, S.; Guddadararangiah, S. Case Report: Unilateral condylar hyperplasia. F1000Research 2021, 10, 46. [Google Scholar] [CrossRef]
- Woo, J.M.; Baek, S.H.; Kim, J.C.; Choi, J.Y. Contour Restoration of Over-Resected Mandibular Angle and Lower Border by Reduction Mandibuloplasty Using Three-Dimensional Planning and Computer-Aided Design and Manufacturing Custom-Made Titanium Implants. J. Craniofac. Surg. 2018, 29, e340–e343. [Google Scholar] [CrossRef] [PubMed]
- Yim, H.W.; Nguyen, A.; Kim, Y.K. Facial Contouring Surgery with Custom Silicone Implants Based on a 3D Prototype Model and CT-Scan: A Preliminary Study. Aesthet. Plast. Surg. 2015, 39, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Staal, F.; Pluijmers, B.; Wolvius, E.; Koudstaal, M. Patient-specific implant for residual facial asymmetry following orthognathic surgery in unilateral craniofacial microsomia. Craniomaxillofacial Trauma. Reconstr. 2016, 9, 264–267. [Google Scholar] [CrossRef] [Green Version]
- Neovius, E.; Engstrand, T. Craniofacial reconstruction with bone and biomaterials: Review over the last 11 years. J. Plast. Reconstr. Aesthet. Surg. 2010, 63, 1615–1623. [Google Scholar] [CrossRef]
- Kerkfeld, V.; Schorn, L.; Depprich, R.; Lommen, J.; Wilkat, M.; Kübler, N.; Rana, M.; Meyer, U. Simultaneous PSI-Based Orthognathic and PEEK Bone Augmentation Surgery Leads to Improved Symmetric Facial Appearance in Craniofacial Malformations. J. Pers. Med. 2022, 12, 1653. [Google Scholar] [CrossRef]
- Hsu, S.S.-P.; Gateno, J.; Bell, R.B.; Hirsch, D.L.; Markiewicz, M.R.; Teichgraeber, J.F.; Zhou, X.; Xia, J.J. Accuracy of a computer-aided surgical simulation protocol for orthognathic surgery: A prospective multicenter study. J. Oral. Maxillofac. Surg. 2013, 71, 128–142. [Google Scholar] [CrossRef] [Green Version]
- Sannino, G.; Gloria, F.; Schiavetti, R.; Ottria, L.; Barlattani, A. Dental Wings CAD/CAM system precision: An internal and marginal fit sperimental analisys. Oral Implant. 2009, 2, 11–20. [Google Scholar]
- Villavisanis, D.F.; Workman, C.I.; Cho, D.Y.; Zapatero, Z.D.; Wagner, C.S.; Blum, J.D.; Bartlett, S.P.; Swanson, J.W.; Chatterjee, A.; Taylor, J.A. Associations of Facial Proportionality, Attractiveness, and Character Traits. J. Craniofac. Surg. 2022, 33, 1431–1435. [Google Scholar] [CrossRef]
- Parthasarathy, J. 3D modeling, custom implants and its future perspectives in craniofacial surgery. Ann. Maxillofac. Surg. 2014, 4, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Keller, E.E.; Triplett, W.W. Iliac bone grafting: Review of 160 consecutive cases. J. Oral. Maxillofac. Surg. 1987, 45, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Olate, S.; Huetequeo-Molina, C.; Requena, R.; Uribe, F. Patient Specific Implants to Solve Structural Facial Asymmetry after Orthognathic Surgery. J. Craniofac. Surg. 2021, 32, e269–e271. [Google Scholar] [CrossRef] [PubMed]
- Scolozzi, P.; Martinez, A.; Jaques, B. Complex orbito-fronto-temporal reconstruction using computer-designed PEEK implant. J. Craniofac. Surg. 2007, 18, 224–228. [Google Scholar] [CrossRef]
- Saponaro, G.; Doneddu, P.; Gasparini, G.; Staderini, E.; Boniello, R.; Todaro, M.; D’Amato, G.; Pelo, S.; Moro, A. Custom made onlay implants in peek in maxillofacial surgery: A volumetric study. Childʹs Nerv. Syst. 2020, 36, 385–391. [Google Scholar] [CrossRef]
- Thrivikraman, G.; Athirasala, A.; Twohig, C.; Boda, S.K.; Bertassoni, L.E. Biomaterials for Craniofacial Bone Regeneration. Dent. Clin. N. Am. 2017, 61, 835–856. [Google Scholar] [CrossRef]
- Kalmar, C.L.; Humphries, L.S.; Zimmerman, C.E.; Vu, G.H.; Swanson, J.W.; Bartlett, S.P.; Taylor, J.A. Orthognathic Hardware Complications in the Era of Patient-Specific Implants. Plast. Reconstr. Surg. 2020, 146, 609e–621e. [Google Scholar] [CrossRef]
- Deng, L.; Deng, Y.; Xie, K. AgNPs-decorated 3D printed PEEK implant for infection control and bone repair. Colloids Surf. B Biointerfaces 2017, 160, 483–492. [Google Scholar] [CrossRef]
- Thien, A.; King, N.K.; Ang, B.T.; Wang, E.; Ng, I. Comparison of polyetheretherketone and titanium cranioplasty after decompressive craniectomy. World Neurosurg. 2015, 83, 176–180. [Google Scholar] [CrossRef]
- Bakhtiari, S.E.; Bakhsheshi-Rad, H.R.; Karbasi, S.; Tavakoli, M.; Hassanzadeh Tabrizi, S.A.; Ismail, A.F.; Seifalian, A.; RamaKrishna, S.; Berto, F. Poly(methyl methacrylate) bone cement, its rise, growth, downfall and future. Polym. Int. 2021, 70, 1182–1201. [Google Scholar] [CrossRef]
- Zamorano, L.; Kadi, A.; Dong, A. Computer-assisted neurosurgery: Simulation and automation. Stereot. Funct. Neuros. 1992, 59, 115–122. [Google Scholar] [CrossRef]
- Fernández-de Thomas, R.J.; Munakomi, S.; De Jesus, O. Craniotomy. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Aiache, A.E. Mandibular angle implants. Aesthet. Plast. Surg. 1992, 16, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Olate, S.; Uribe, F.; Huentequeo-Molina, C.; Goulart, D.R.; Sigua-Rodriguez, E.A.; Alister, J.P. Mandibular Angle Contouring Using Porous Polyethylene Stock or PEEK-based Patient Specific Implants. A Critical Analysis. J. Craniofac. Surg. 2021, 32, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Alasseri, N.; Alasraj, A. Patient-specific implants for maxillofacial defects: Challenges and solutions. Maxillofac. Plast. Reconstr. Surg. 2020, 42, 15. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Onică, N.; Onică, C.A.; Budală, D.G.; Gelețu, G.L.; Balan, M.; Baciu, E.-R.; Murariu, A.; Pertea, M. The Use of 3D Technology in the Management of Residual Asymmetry following Orthognathic Surgery: A Case Report. Healthcare 2023, 11, 2172. https://doi.org/10.3390/healthcare11152172
Onică N, Onică CA, Budală DG, Gelețu GL, Balan M, Baciu E-R, Murariu A, Pertea M. The Use of 3D Technology in the Management of Residual Asymmetry following Orthognathic Surgery: A Case Report. Healthcare. 2023; 11(15):2172. https://doi.org/10.3390/healthcare11152172
Chicago/Turabian StyleOnică, Neculai, Cezara Andreea Onică, Dana Gabriela Budală, Gabriela Luminița Gelețu, Mihail Balan, Elena-Raluca Baciu, Alice Murariu, and Mihaela Pertea. 2023. "The Use of 3D Technology in the Management of Residual Asymmetry following Orthognathic Surgery: A Case Report" Healthcare 11, no. 15: 2172. https://doi.org/10.3390/healthcare11152172




