Comparison of the Effects of Self-Administered Moxibustion versus Acupressure on Blood Pressure, Stress, Sleep Quality, and Quality of Life in Hypertensive Patients: A Randomized Parallel Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Subjects
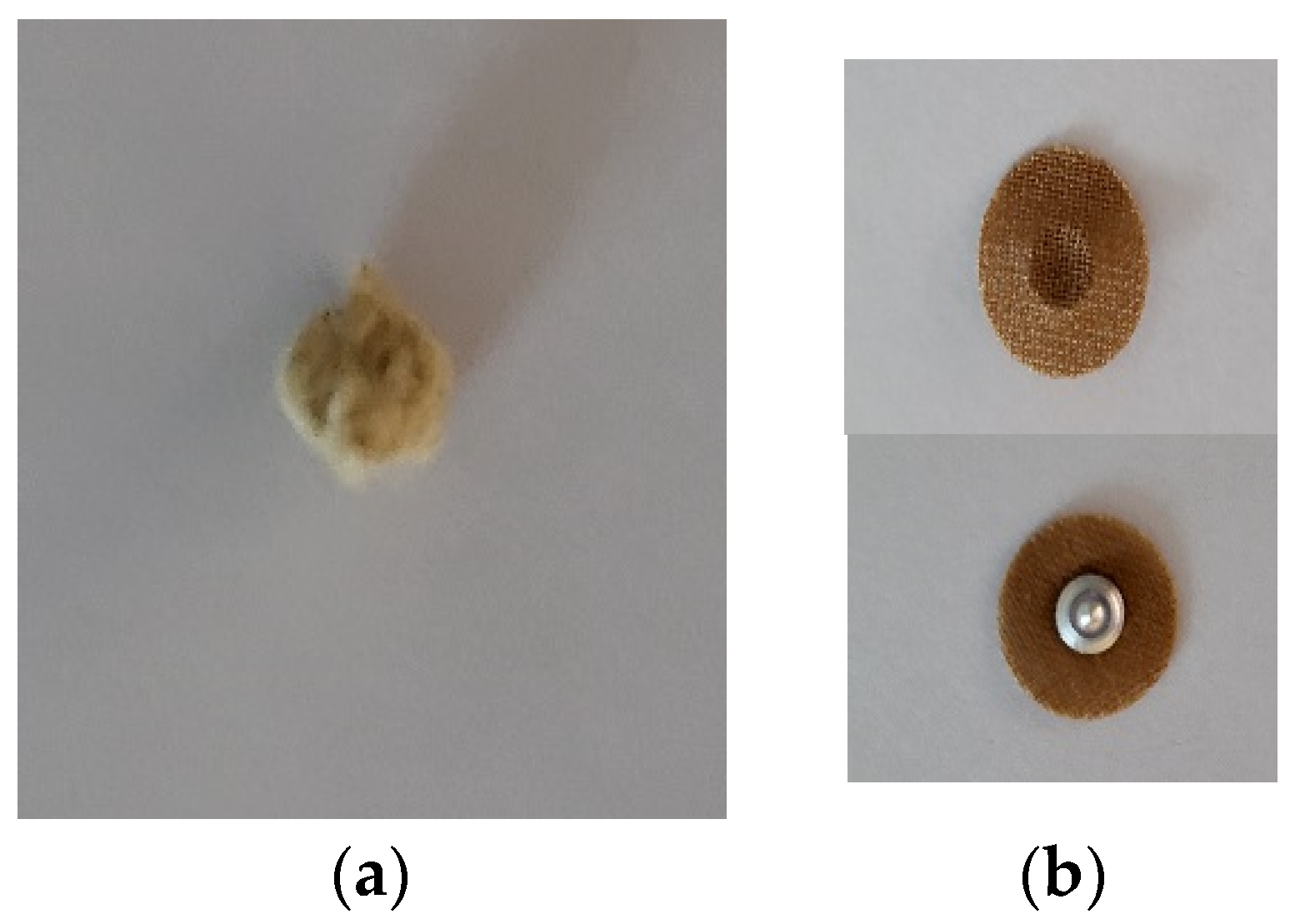
2.3. Interventions
2.4. Measurements
2.5. Sample Size
2.6. Data Analysis
3. Results
3.1. Participant Characteristics
| Variables | Category | Total (n = 41) | Moxibustion (n = 21) | Acupressure (n = 20) | p a |
|---|---|---|---|---|---|
| Age (years) | 61.7 ± 10.8 | 64.3 ± 9.2 | 59.1 ± 12.0 | 0.266 b | |
| Body mass index (kg/m2) | 26.0 ± 3.7 | 24.9.5 ± 3.4 | 27.2 ± 3.8 | 0.047 b | |
| Gender | Male | 27 (65.9) | 13 (61.9) | 14 (70.0) | 0.585 |
| Female | 14 (34.1) | 8 (38.1) | 6 (30.0) | ||
| Education | ≤High school | 7 (17.1) | 4 (19.0) | 3 (15.0) | 0.886 |
| College | 21 (51.2) | 11 (52.4) | 10 (50.0) | ||
| >College | 13 (31.7) | 6 (28.6) | 7 (35.0) | ||
| Marital status | Single | 2 (4.9) | 0 (0) | 2 (10.0) | 0.232 |
| Married | 39 (95.1) | 21 (100) | 18 (90.0) | ||
| Moderate-to-vigorous exercise | No | 35 (85.4) | 18 (85.7) | 17 (85.0) | 1.000 |
| Yes | 6 (14.6) | 3 (14.3) | 3 (15.0) | ||
| Smoking | No | 30 (73.2) | 16 (76.2) | 14 (70.0) | 0.896 |
| Yes | 2 (4.9) | 1 (4.8) | 1 (5.0) | ||
| Past smoker | 9 (22.0) | 4 (19.0) | 5 (25.0) | ||
| Drinking | No | 19 (46.3) | 11 (52.4) | 8 ((40.0) | 0.702 |
| Once per month | 5 (12.2) | 3 (14.3) | 2 (10.0) | ||
| 2–4 times/month | 9 (22.0) | 3 (14.3) | 6 (30.0) | ||
| 2–3 times/week | 5 (12.2) | 2 (9.5) | 3 (15.0) | ||
| ≥4 times/week | 3 (7.3) | 2 (9.5) | 1 (5.0) | ||
| Hypertension medication | No (hypertensive) | 17 (41.5) | 7 (33.3) | 8 (40.0) | 0.360 |
| No (pre-hypertensive) | 2 (4.9) | 2 (9.5) | 0 (0.0) | ||
| Yes | 24 (58.5) | 12 (57.1) | 12 (60.0) | ||
| Other medication | Hyperlipidemia | 8 (19.5) | 2 (9.5) | 6 (30.0) | Multiple responses |
| Diabetes mellitus | 8 (19.5) | 5 (23.8) | 3 (15.0) | ||
| Others | 4 (9.8) | 2 (9.5) | 2 (10.0) | ||
3.2. Changes in Blood Pressure and Stress
3.3. Changes in Sleep Quality and Quality of Life
3.4. Adverse Events
| Variables | Group | Baseline | Week 8 | p a | Effect Size c | Week 8–Baseline | p e | Effect Size c | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | ||||||
| Systolic blood pressure (mmHg) | Moxibustion | 144.3 ± 21.3 | 135.0 (130.0–150.0) | 130.5 ± 13.2 | 130.0 (120.0–140.0) | 0.000 *** | 0.78 | −13.8 ± 12.5 | −10.0 (−20.0–−2.5) | 0.289 | 0.17 |
| Acupressure | 140.5 ± 13.2 | 135.0 (130.0–150.0) | 133.0 ± 14.9 | 130.0 (120.0–140.0) | 0.024 * | 0.50 | −7.5 ± 16.2 | −10.0 (−20.0–0.0) | |||
| Diastolic blood pressure (mmHg) | Moxibustion | 94.1 ± 15.8 | 90.0 (80.0–105.0) | 81.9 ± 10.8 | 80.0 (75.0–90.0) | 0.001 ** | 0.76 | −12.1 ± 11.2 | −10.0 (−20.0–−5.0) | 0.391 f | 0.27 d |
| Acupressure | 91.8 ± 8.2 | 90.0 (90.0–93.8) | 82.5 ± 7.2 | 80.0 (80.0–90.0) | 0.002 ** | 0.69 | −9.3 ± 10.0 | −17.5 (−20.0–0.0) | |||
| Epinephrine (pg/mL) | Moxibustion | 56.0 ± 23.4 | 57.5 (36.1–71.5) | 44.0 ± 17.6 | 41.9 (29.9–50.3) | 0.085 b | 0.40 d | −12.0 ± 30.4 | −14.6 (−34.2–4.9) | 0.823 f | 0.07 d |
| Acupressure | 49.9 ± 21.2 | 53.3 (29.1–70.6) | 39.7 ± 17.4 | 35.6 (28.6–45.0) | 0.076 | 0.40 | −10.2 ± 22.1 | −8.0 (−29.0–7.9) | |||
| Norepinephrine (pg/mL) | Moxibustion | 587.9 ± 285.2 | 483.0 (420.0–605.2) | 505.1 ± 224.7 | 458.1 (360.9–573.6) | 0.122 | 0.34 | −82.8 ± 289.6 | −98.3 (−174.0–87.1) | 0.639 | 0.07 |
| Acupressure | 557.8 ± 294.8 | 503.9 (338.6–638.1) | 482.3 ± 188.1 | 486.3 (369.4–589.6) | 0.370 | 0.20 | −75.5 ± 231.5 | −17.1 (−192.4–125.6) | |||
| Perceived stress | Moxibustion | 15.7 ± 4.1 | 15.0 (13.0–19.0) | 12.8 ± 4.7 | 12.0 (8.5–15.5) | 0.028 * | 0.48 | −2.9 ± 5.2 | −3.0 (−5.0–1.5) | 0.355 f | 0.29 d |
| Acupressure | 14.2 ± 3.7 | 14.0 (12.0–16.0) | 12.7 ± 5.3 | 12.5 (8.0–16.5) | 0.185 b | 0.31 d | −1.5 ± 4.7 | −0.5 (−5.8–1.8) | |||
| Variables | Group | Baseline | Week 8 | p a | Effect Size d | Week 8–Baseline | p e | Effect Size d | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | ||||||
| PSQI Subscales | |||||||||||
| Subjective sleep quality | Moxibustion | 1.1 ± 0.7 | 1.0 (1.0–2.0) | 0.8 ± 0.5 | 1.0 (0.5–1.0) | 0.071 | 0.39 | −0.3 ± 0.8 | 0.0 (−1.0–0.0) | 0.418 | 0.13 |
| Acupressure | 1.2 ± 0.8 | 1.0 (1.0–2.0) | 1.1 ± 0.6 | 1.0 (1.0–1.0) | 0.564 | 0.13 | −0.1 ± 0.8 | 0.0 (−1.0–0.0) | |||
| Sleep latency | Moxibustion | 1.0 ± 0.9 | 1.0 (0.0–2.0) | 0.8 ± 0.6 | 1.0 (0.0–1.0) | 0.109 | 0.35 | −0.3 ± 0.8 | 0.0 (−1.0–0.0) | 0.499 | 0.11 |
| Acupressure | 1.0 ± 0.7 | 1.0 (0.3–1.8) | 0.9 ± 0.7 | 1.0 (0.0–1.0) | 0.180 | 0.30 | −0.2 ± 0.5 | 0.0 (0.0–0.0) | |||
| Sleep duration | Moxibustion | 1.1 ± 0.7 | 1.0 (1.0–1.5) | 1.1 ± 0.5 | 1.0 (1.0–1.0) | 0.739 | 0.07 | −0.0 ± 0.7 | 0.0 (−0.5–0.0) | 0.383 | 0.14 |
| Acupressure | 0.9 ± 1.1 | 1.0 (0.0–1.0) | 1.0 ± 0.9 | 1.0 (0.3–1.0) | 0.564 | 0.13 | 0.1 ± 0.8 | 0.0 (0.0–1.0) | |||
| Habitual sleep efficiency | Moxibustion | 0.4 ± 0.7 | 0.0 (0.0–1.0) | 0.2 ± 0.5 | 0.0 (0.0–0.0) | 0.470 | 0.16 | −0.1 ± 0.9 | 0.0 (−0.5–0.0) | 0.621 | 0.08 |
| Acupressure | 0.3 ± 0.7 | 0.0 (0.0–0.0) | 0.3 ± 0.6 | 0.0 (0.0–0.0) | 0.739 | 0.07 | −0.1 ± 0.7 | 0.0 (0.0–0.0) | |||
| Sleep disturbance | Moxibustion | 1.2 ± 0.6 | 1.0 (1.0–2.0) | 1.3 ± 0.6 | 1.0 (1.0–1.5) | 0.527 | 0.14 | 0.1 ± 0.7 | 0.0 (0.0–1.0) | 0.232 | 0.19 |
| Acupressure | 1.1 ± 0.4 | 1.0 (1.0–1.0) | 0.9 ± 0.7 | 1.0 (0.0–1.0) | 0.257 | 0.25 | −0.2 ± 0.6 | 0.0 (−0.8–0.0) | |||
| Use of sleeping medication | Moxibustion | 0.0 ± 0.0 | 0.0 (0.0–0.0) | 0.1 ± 0.2 | 0.0 (0.0–0.0) | 0.317 | 0.22 | 0.0 ± 0.2 | 0.0 (0.0–0.0) | 0.972 | 0.01 |
| Acupressure | 0.0 ± 0.0 | 0.0 (0.0–0.0) | 0.1 ± 0.2 | 0.0 (0.0–0.0) | 0.317 | 0.22 | 0.1 ± 0.2 | 0.0 (0.0–0.0) | |||
| Daytime dysfunction | Moxibustion | 1.1 ± 1.0 | 1.0 (0.0–2.0) | 1.0 ± 0.7 | 1.0 (0.5–1.0) | 0.458 | 0.16 | −0.2 ± 1.1 | 0.0 (−1.0–0.0) | 0.872 | 0.03 |
| Acupressure | 1.2 ± 0.8 | 1.0 (0.3–2.0) | 1.0 ± 0.9 | 1.0 (0.0–2.0) | 0.435 | 0.17 | −0.2 ± 1.0 | 0.0 (0.0–0.0) | |||
| WHOQOL-BREF domain | |||||||||||
| Social relationships | Moxibustion | 68.6 ± 10.1 | 66.7 (60.0–73.3) | 72.1 ± 10.2 | 73.3 (66.7–80.0) | 0.044 * | 0.44 | 3.5 ± 7.8 | 0.0 (−3.3–13.3) | 0.915 | 0.02 |
| Acupressure | 66.3 ± 10.5 | 66.7 (60.0–73.3) | 69.3 ± 12.9 | 70.0 (60.0–80.0) | 0.317 b | 0.23 c | 3.0 ± 13.1 | 0.0 (−5.0–16.7) | |||
| Variables | Group | Baseline | Week 8 | p (η2) | ||
|---|---|---|---|---|---|---|
| Time | Group | Interaction | ||||
| PSQI | ||||||
| Total score | Moxibustion | 6.0 ± 2.6 | 5.2 ± 1.9 | 0.069 | 0.684 | 0.564 |
| Acupressure | 5.6 ± 3.0 | 5.1 ± 2.5 | (0.082) | (0.004) | (0.009) | |
| WHOQOL-BREF domain | ||||||
| Physical health | Moxibustion | 67.9 ± 13.4 | 72.8 ± 12.2 | 0.002 ** | 0.263 | 0.556 |
| Acupressure | 72.7 ± 12.1 | 76.1 ± 10.7 | (0.225) | (0.032) | (0.009) | |
| Psychological health | Moxibustion | 71.1 ± 11.9 | 73.2 ± 11.8 | 0.076 | 0.699 | 0.703 |
| Acupressure | 69.3 ± 9.3 | 72.5 ± 10.9 | (0.079) | (0.004) | (0.079) | |
| Environment | Moxibustion | 68.1 ± 13.9 | 71.5 ± 13.5 | 0.035 * | 0.669 | 0.563 |
| Acupressure | 70.4 ± 11.1 | 72.4 ± 9.9 | (0.110) | (0.005) | (0.009) | |
| Complete blood count | ||||||
| Hematocrit | Moxibustion | 40.8 ± 4.7 | 40.8 ± 4.7 | 0.961 | 0.238 | 0.909 |
| Acupressure | 42.3 ± 3.5 | 42.3 ± 3.4 | (0.000) | (0.035) | (0.000) | |
| Variables | Group | Baseline | Week 8 | p a | Effect Size d | Week 8–Baseline | p e | Effect Size d | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | Mean ± SD | Median (IQR) | ||||||
| White blood cells (103/µL) | Moxibustion | 6.4 ± 2.0 | 5.9 (5.4–7.1) | 6.3 ± 1.5 | 5.9 (5.2–7.1) | 0.651 | 0.10 | −0.1 ± 1.5 | −0.4 (−0.8–0.8) | 0.481 | 0.11 |
| Acupressure | 6.0 ± 1.5 | 5.9 (5.0–7.2) | 6.2 ± 2.2 | 5.7 (4.9–6.6) | 0.422 | 0.18 | 0.2 ± 1.7 | 0.2 (−0.4–0.6) | |||
| Platelets (103/µL) | Moxibustion | 248.0 ± 54.7 | 246.0 (203.0–283.5) | 234.7 ± 61.1 | 248.0 (180.5–284.0) | 0.213 b | 0.28 c | −13.2 ± 47.2 | −9.0 (−27.0–15.5) | 0.611 | 0.08 |
| Acupressure | 241.1 ± 46.8 | 231.5 (217.5–269.8) | 226.9 ± 50.4 | 234.5 (213.8–254.0) | 0.079 | 0.39 | −14.2 ± 30.6 | −15.0 (−34.5–11.8) | |||
| Red blood cells (106/µL) | Moxibustion | 4.5 ± 0.5 | 4.6 (4.1–4.8) | 4.5 ± 0.5 | 4.6 (4.2–4.9) | 0.737 | 0.07 | 0.0 ± 0.2 | 0.0 (−0.2–0.2) | 0.734 | 0.05 |
| Acupressure | 4.6 ± 0.4 | 4.6 (4.4–4.9) | 4.6 ± 0.4 | 4.6 (4.3–5.0) | 0.484 b | 0.16 c | −0.0 ± 0.3 | 0.0 (−0.2–0.1) | |||
| Hemoglobin (g/dL) | Moxibustion | 15.2 ± 6.9 | 14.0 (12.8–15.3) | 13.5 ± 1.7 | 13.7 (12.8–14.8) | 0.423 | 0.17 | −1.7 ± 7.4 | −0.2 (−0.5–0.5) | 0.296 | 0.16 |
| Acupressure | 14.1 ± 1.4 | 14.4 (13.4–15.0) | 14.1 ± 1.2 | 14.1 (13.4–15.2) | 1.00 b | 0.00 c | 0.0 ± 0.9 | 0.2 (−0.3–0.4) | |||
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Oparil, S.; Acelajado, M.C.; Bakris, G.L.; Berlowitz, D.R.; Cífková, R.; Dominiczak, A.F.; Grassi, G.; Jordan, J.; Poulter, N.R.; Rodgers, A.; et al. Hypertension. Nat. Rev. Dis. Primers. 2018, 4, 18014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J. Hypertens. 2018, 36, 1953–2041. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cuffee, Y.; Ogedegbe, C.; Williams, N.J.; Ogedegbe, G.; Schoenthaler, A. Psychosocial risk factors for hypertension: An update of the literature. Curr. Hypertens. Rep. 2014, 16, 483. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Lee, E.T.; Fabsitz, R.R.; Devereux, R.; Best, L.; Welty, T.K.; Howard, B.V. A longitudinal study of hypertension risk factors and their relation to cardiovascular disease: The Strong Heart Study. Hypertension 2006, 47, 403–409. [Google Scholar] [CrossRef] [Green Version]
- Vrijens, B.; Antoniou, S.; Burnier, M.; de la Sierra, A.; Volpe, M. Current Situation of Medication Adherence in Hypertension. Front. Pharmacol. 2017, 8, 100. [Google Scholar] [CrossRef] [Green Version]
- Cuspidi, C.; Tadic, M.; Grassi, G.; Mancia, G. Treatment of hypertension: The ESH/ESC guidelines recommendations. Pharmacol. Res. 2018, 128, 315–321. [Google Scholar] [CrossRef]
- Lee, W.R.; Yoo, K.B.; Jeong, J.; Koo, J.H. Chronic Disease Management for People with Hypertension. Int. J. Public Health 2022, 67, 1604452. [Google Scholar] [CrossRef]
- Niriayo, Y.L.; Ibrahim, S.; Kassa, T.D.; Asgedom, S.W.; Atey, T.M.; Gidey, K.; Demoz, G.T.; Kahsay, D. Practice and predictors of self-care behaviors among ambulatory patients with hypertension in Ethiopia. PLoS ONE 2019, 14, e0218947. [Google Scholar] [CrossRef] [Green Version]
- Biçer, S.; Ünsal, A.; Taşcı, S.; Demir, G.; Ceyhan, Y.Ş. The Effect of Acupressure on Blood Pressure Level and Pulse Rate in Individuals with Essential Hypertension: A Randomized Controlled Trial. Holist. Nurs. Pract. 2021, 35, 40–48. [Google Scholar] [CrossRef]
- Lin, G.H.; Chang, W.C.; Chen, K.J.; Tsai, C.C.; Hu, S.Y.; Chen, L.L. Effectiveness of Acupressure on the Taichong Acupoint in Lowering Blood Pressure in Patients with Hypertension: A Randomized Clinical Trial. Evid. Based Complement. Altern. Med. 2016, 2016, 1549658. [Google Scholar] [CrossRef] [Green Version]
- Tan, X.; Pan, Y.; Su, W.; Gong, S.; Zhu, H.; Chen, H.; Lu, S. Acupuncture therapy for essential hypertension: A network meta-analysis. Ann. Transl. Me. 2019, 7, 266. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Wu, Q.; Liu, M.; Zhu, W.; Ren, Q.; Wang, Y.; Sun, X.; Chen, J. Moxibustion for Essential Hypertension and Hypertensive Symptoms: A Systematic Review of 18 Randomized Controlled Trials. Complement. Med. Res. 2021, 28, 435–445. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Wu, Q.; Zhang, G.; Wang, Y.; Li, S.; Wang, B.; Chen, Z.; Zhu, W.; Wang, F.; Gan, C. Heat-sensitive moxibustion self-administration in patients in the community with primary hypertension: A protocol for a multi-center, pragmatic, non-randomized trial. Medicine 2020, 99, e22230. [Google Scholar] [CrossRef] [PubMed]
- Matos, L.C.; Machado, J.P.; Monteiro, F.J.; Greten, H.J. Understanding Traditional Chinese Medicine Therapeutics: An Overview of the Basics and Clinical Applications. Healthcare 2021, 9, 257. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Shen, C.L.; Peck, K.; Brismée, J.M.; Doctolero, S.; Lo, D.F.; Lim, Y.; Lao, L. Training Self-Administered Acupressure Exercise among Postmenopausal Women with Osteoarthritic Knee Pain: A Feasibility Study and Lessons Learned. Evid. Based Complement. Alternat. Med. 2012, 2012, 570431. [Google Scholar] [CrossRef]
- Shin, K.M.; Park, J.E.; Yook, T.H.; Kim, J.U.; Kwon, O.; Choi, S.M. Moxibustion for prehypertension and stage I hypertension: A pilot randomized controlled trial. Integr. Med. Res. 2019, 8, 1–7. [Google Scholar] [CrossRef]
- Wang, J.; Xiong, X. Evidence-based chinese medicine for hypertension. Evid. Based Complement. Alternat. Med. 2013, 2013, 978398. [Google Scholar] [CrossRef] [Green Version]
- Trevisol, D.J.; Moreira, L.B.; Kerkhoff, A.; Fuchs, S.C.; Fuchs, F.D. Health-related quality of life and hypertension: A systematic review and meta-analysis of observational studies. J. Hypertens. 2011, 29, 179–188. [Google Scholar] [CrossRef]
- Ames, S.C.; Jones, G.N.; Howe, J.T.; Brantley, P.J. A prospective study of the impact of stress on quality of life: An investigation of low-income individuals with hypertension. Ann. Behav. Med. 2001, 23, 112–119. [Google Scholar] [CrossRef]
- Spruill, T.M. Chronic psychosocial stress and hypertension. Curr. Hypertens. Rep. 2010, 12, 10–16. [Google Scholar] [CrossRef] [Green Version]
- Kharibam, P.; Pathania, M.; Naithani, M.; Singh, Y.; Bahurupi, Y.; Dhar, M.; Yadav, S.R.; Singh, N. A Comparative Study of Baseline Heart Rate Variability, Sleep Quality, and Oxidative Stress Levels in Hypertensive Versus Normotensive Subjects: A Cross-Sectional Study. Cureus 2022, 14, e25855. [Google Scholar] [CrossRef] [PubMed]
- Ushakov, A.V.; Ivanchenko, V.S.; Gagarina, A.A. Psychological Stress in Pathogenesis of Essential Hypertension. Curr. Hypertens. Rev. 2016, 12, 203–214. [Google Scholar] [CrossRef] [PubMed]
- Hwang, K.H.; Jang, K.; Nam, S.Y.; Kim, Y.J. Cortisol Secretion and Subsequent Impaired Lymphopoiesis after Starvation Can Be Reduced by Moxibustion Treatment. Evid. Based Complement. Alternat. Med. 2021, 2021, 8856687. [Google Scholar] [CrossRef]
- Li, J.T.; Guan, H.Y.; Ma, J.J.; Fu, C.L.; Shao, Y.X.; Wang, L.J.; Xue, T.; Wu, Y.Q.; Ma, H.F. Moxibustion improved gastric ulcer by reducing contents of corticotrophin-releasing hormone and adrenocorticotropic hormone in serum and hypothalamus-pituitary tissues in rats with stress-induced gastric ulcer. Zhen Ci Yan Jiu 2019, 44, 347–351. [Google Scholar] [CrossRef]
- Wang, C.C.; Han, E.Y.; Jenkins, M.; Hong, X.; Pang, S.; Whitehead, L.; Kirk, D.L.; Williams, A. The safety and efficacy of using moxibustion and or acupuncture for cancer-related insomnia: A systematic review and meta-analysis of randomised controlled trials. Palliat. Care Soc. Pract. 2022, 16, 26323524211070569. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D.; CONSORT Group. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Reis, R.S.; Hino, A.A.; Añez, C.R. Perceived stress scale: Reliability and validity study in Brazil. J. Health Psychol. 2010, 15, 107–114. [Google Scholar] [CrossRef] [Green Version]
- Park, J.N.; Seo, Y.S. Validation of the Perceived Stress Scale on samples of Korean university students. Korean J. Psychol. Gen. 2010, 29, 611–629. [Google Scholar]
- Mollayeva, T.; Thurairajah, P.; Burton, K.; Mollayeva, S.; Shapiro, C.M.; Colantonio, A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med. Rev. 2016, 25, 52–73. [Google Scholar] [CrossRef]
- Sohn, S.I.; Kim, D.H.; Lee, M.Y.; Cho, Y.W. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath. 2012, 16, 803–812. [Google Scholar] [CrossRef] [PubMed]
- Min, S.K.; Kim, K.I.; Lee, C.I.; Jung, Y.C.; Suh, S.Y.; Kim, D.K. Development of the Korean versions of WHO Quality of Life scale and WHOQOL-BREF. Qual. Life Res. 2002, 11, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Skevington, S.M.; Lotfy, M.; O’Connell, K.A.; WHOQOL Group. The World Health Organization’s WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Qual. Life Res. 2004, 13, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.H.; Hahn, S.J.; Im, H.J.; Yang, K.S. Reliability and Validity of the Korean World Health Organization Quality of Life (WHOQOL)-BREF in People with Physical Impairments. Ann. Rehabil. Med. 2013, 37, 488–497. [Google Scholar] [CrossRef] [Green Version]
- Lakens, D. Calculating and reporting effect sizes to facilitate cumulative science: A practical primer for t-tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomczak, M.; Tomczak, E. The need to report effect size estimates revisited. An overview of some recommended measures of effect size. Trends Sport Sci. 2014, 1, 19–25. [Google Scholar]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Shi, Y.N.; Wang, R.Y.; Liu, T.; Xu, J.; Mao, W.; Sun, Q.H. Home-based traditional Chinese medicine nursing interventions for discharged patients with COVID-19: A rapid review of Chinese guidelines. Integr. Med. Res. 2020, 9, 100479. [Google Scholar] [CrossRef]
- Yoon, C.; Cho, Y.S.; Park, S.; Chung, S.P.; Choi, Y.H. Epidemiology of burns caused by moxibustion in Korea. Burns 2016, 42, 1588–1592. [Google Scholar] [CrossRef]
- Deng, H.; Shen, X. The mechanism of moxibustion: Ancient theory and modern research. Evid. Based Complement. Alternat. Med. 2013, 2013, 379291. [Google Scholar] [CrossRef] [Green Version]
- Cheung, T.; Ho, Y.S.; Yuen, C.S.; Lam, C.S.; Chun-Lung So, B.; Chen, S.C.; Leung, D.Y.P.; Kwai-Ping Suen, L.; Tin-Yau So, L.; Chun-Hei Ho, A.; et al. Electromoxibustion for knee osteoarthritis in older adults: A pilot randomized controlled trial. Complement. Ther. Clin. Pract. 2020, 41, 101254. [Google Scholar] [CrossRef]
- Bilek, F.; Bahcecioglu-Turan, G.; Ozer, Z. The effect of self-acupressure on quality of life, physical and cognitive function in relapsing remitting multiple sclerosis patients: A randomized controlled study. Explore 2022, 19, 84–90. [Google Scholar] [CrossRef]
- Salmani Mood, M.; Yavari, Z.; Bahrami Taghanaki, H.; Mahmoudirad, G. The effect of acupressure on fasting blood glucose, glycosylated hemoglobin and stress in patients with type 2 diabetes. Complement. Ther. Clin. Pract. 2021, 43, 101393. [Google Scholar] [CrossRef]
- Song, H.J.; Seo, H.J.; Lee, H.; Son, H.; Choi, S.M.; Lee, S. Effect of self-acupressure for symptom management: A systematic review. Complement. Ther. Med. 2015, 23, 68–78. [Google Scholar] [CrossRef]
- Nourizadeh, R.; Khanipour, S.; Zamiri, R.E.; Namin, M.S.; Khalili, A.; Hakimi, S. A Comparison of the Effects of Self-Acupressure and Aerobic Exercises on Sleep Disorders of Breast Cancer Survivors: A Controlled Randomized Clinical Trial. Med. Acupunct. 2022, 34, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Messerli, F.H.; Bangalore, S.; Schmieder, R.E. Wilder’s principle: Pre-treatment value determines post-treatment response. Eur. Heart J. 2015, 36, 576–579. [Google Scholar] [CrossRef] [Green Version]
- Law, M.R.; Wald, N.J.; Morris, J.K.; Jordan, R.E. Value of low dose combination treatment with blood pressure lowering drugs: Analysis of 354 randomised trials. BMJ 2003, 326, 1427. [Google Scholar] [CrossRef] [Green Version]
- Hu, H.; Zhang, J.; Wang, Y.; Tian, Z.; Liu, D.; Zhang, G.; Gu, G.; Zheng, H.; Xie, R.; Cui, W. Impact of baseline blood pressure on the magnitude of blood pressure lowering by nifedipine gastrointestinal therapeutic system: Refreshing the Wilder’s principle. Drug Des. Devel. Ther. 2017, 11, 3179–3186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bundy, J.D.; Li, C.; Stuchlik, P.; Bu, X.; Kelly, T.N.; Mills, K.T.; He, H.; Chen, J.; Whelton, P.K.; He, J. Systolic Blood Pressure Reduction and Risk of Cardiovascular Disease and Mortality: A Systematic Review and Network Meta-analysis. JAMA Cardiol. 2017, 2, 775–781. [Google Scholar] [CrossRef] [Green Version]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jung, J.; Kim, J. Comparison of the Effects of Self-Administered Moxibustion versus Acupressure on Blood Pressure, Stress, Sleep Quality, and Quality of Life in Hypertensive Patients: A Randomized Parallel Trial. Healthcare 2023, 11, 2182. https://doi.org/10.3390/healthcare11152182
Jung J, Kim J. Comparison of the Effects of Self-Administered Moxibustion versus Acupressure on Blood Pressure, Stress, Sleep Quality, and Quality of Life in Hypertensive Patients: A Randomized Parallel Trial. Healthcare. 2023; 11(15):2182. https://doi.org/10.3390/healthcare11152182
Chicago/Turabian StyleJung, Jongsin, and Jaehee Kim. 2023. "Comparison of the Effects of Self-Administered Moxibustion versus Acupressure on Blood Pressure, Stress, Sleep Quality, and Quality of Life in Hypertensive Patients: A Randomized Parallel Trial" Healthcare 11, no. 15: 2182. https://doi.org/10.3390/healthcare11152182
APA StyleJung, J., & Kim, J. (2023). Comparison of the Effects of Self-Administered Moxibustion versus Acupressure on Blood Pressure, Stress, Sleep Quality, and Quality of Life in Hypertensive Patients: A Randomized Parallel Trial. Healthcare, 11(15), 2182. https://doi.org/10.3390/healthcare11152182






