Time-Varying Hazard of Patient Falls in Hospital: A Retrospective Case–Control Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Fall-Related Factors and Fall Risk Assessment
2.2. Study Subjects
2.3. Data Collection and Analysis
3. Results
3.1. Homogeneity for General Chracteristics between Fall Group and Non-Fall Group
3.2. Comparison of Patient Falls Prevalence by Latent Risk Factors
3.3. Association between Physical Impairments and the Fall Risk by the MFS
3.4. Stepwise Logistic Regression to Anlalyze the Contribution of Factors to Patient Falls
3.5. Odds Ratio in Logistic Regression Analysis for Patient Falls by Risk Factors
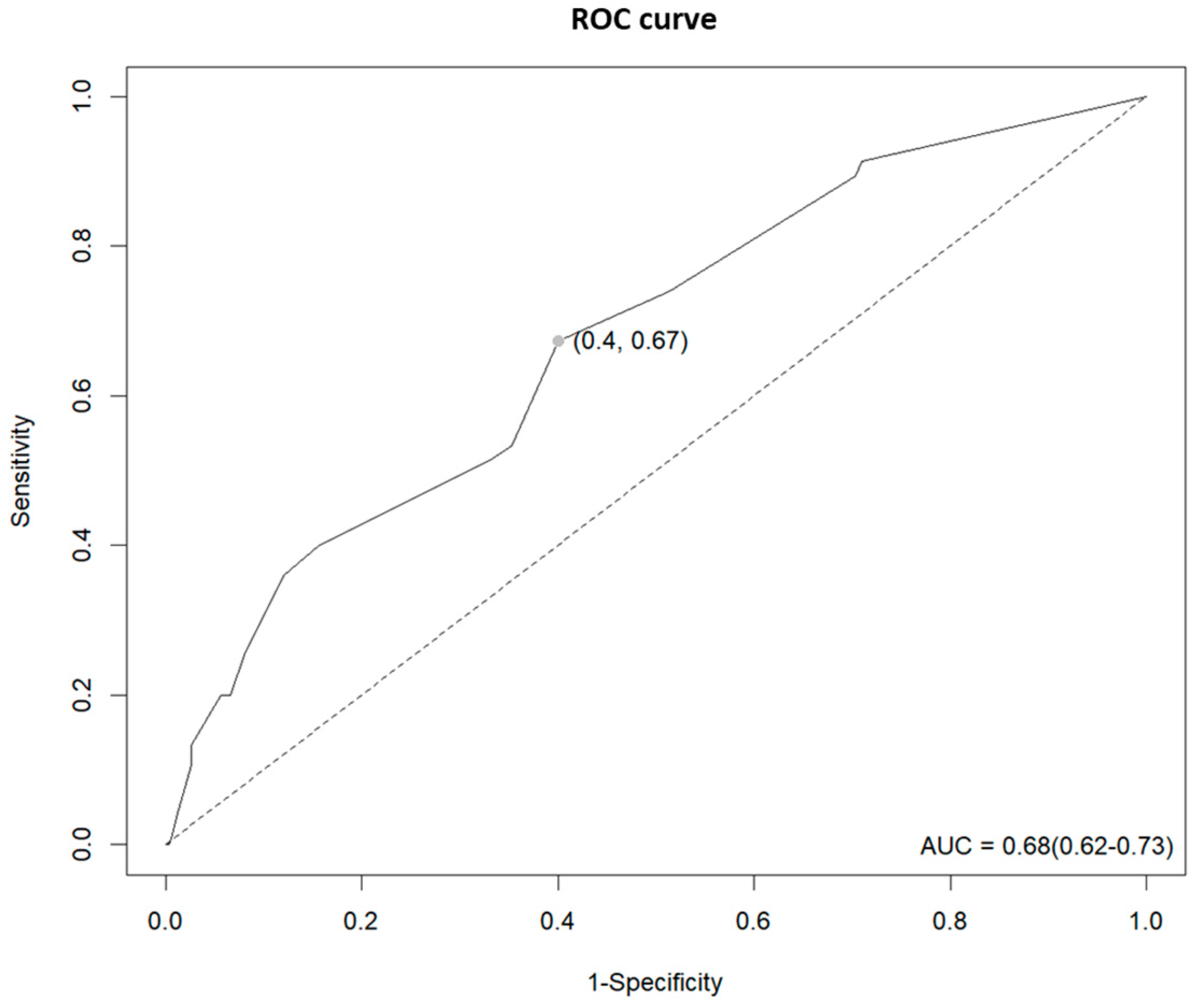
3.6. AUC Analysis for Fall Prediction of the MFS
3.7. Kaplan–Meier Estimates for the Fall-Free Survival Probability against Time by Risk Factors
3.8. Hazard Ratio in Time-Dependent Cox Regression Analysis for Patient Falls by Risk Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Step Safely: Strategies for Preventing and Managing Falls across the Life-Course. 2021. Available online: https://www.who.int/publications/i/item/978924002191-4 (accessed on 25 February 2022).
- World Health Organization. Patient Safety Incident Reporting and Learning Systems: Technical Report and Guidance. 2020. Available online: https://www.who.int/publications/i/item/9789240010338 (accessed on 11 March 2022).
- Korea Institute for Healthcare Accreditation. Korea Patient Safety Reporting & Learning System; Patient Safety Statistics. Available online: https://www.koiha-kops.org/main.do (accessed on 15 March 2022).
- Royal College of Physicians. National Audit of Inpatient Falls Audit Report 2017. Available online: https://www.hqip.org.uk/wp-content/uploads/2018/02/national-audit-of-inpatient-falls-audit-report-2017.pdf (accessed on 22 March 2022).
- Joint Commission International. Sentinel Event Alert 55: Preventing Falls and Fall Related Injuries in Health Care Facilities. Available online: https://www.jointcommission.org/resources/sentinel-event/sentinel-event-alert-newsletters/sentinel-event-alert-55-preventing-falls-and-fall-related-injuries-in-health-care-facilities (accessed on 29 March 2022).
- Heng, H.; Jazayeri, D.; Shaw, L.; Kiegaldie, D.; Hill, A.M.; Morris, M.E. Hospital falls prevention with patient education: A scoping review. BMC Geriatr. 2020, 20, 140. [Google Scholar] [CrossRef] [Green Version]
- Dykes, P.C.; Burns, Z.; Adelman, J.; Benneyan, J.; Bogaisky, M.; Carter, E.; Ergai, A.; Lindros, M.E.; Lipsitz, S.R.; Scanlan, M.; et al. Evaluation of a Patient-Centered Fall-Prevention Tool Kit to Reduce Falls and Injuries: A Nonrandomized Controlled Trial. JAMA Netw. Open 2020, 3, e2025889. [Google Scholar] [CrossRef] [PubMed]
- Strini, V.; Schiavolin, R.; Prendin, A. Fall Risk Assessment Scales: A Systematic Literature Review. Nurs. Rep. 2021, 11, 430–443. [Google Scholar] [CrossRef] [PubMed]
- Sardo, P.M.G.; Simões, C.S.O.; Alvarelhão, J.J.M.; Simões, J.F.F.L. Fall risk assessment: Retrospective analysis of Morse Fall Scale scores in Portuguese hospitalized adult patients. Appl. Nurs. Res. 2016, 31, 34–40. [Google Scholar] [CrossRef]
- Oliver, D.; Britton, M.; Seed, P.; Martin, F.C.; Hopper, A.H. Development and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: Case-control and cohort studies. BMJ (Clin. Res. Ed.) 1997, 315, 1049–1053. [Google Scholar] [CrossRef] [Green Version]
- Hendrich, A.; Nyhuis, A.; Kippenbrock, T.; Soja, M.E. Hospital falls: Development of a predictive model for clinical practice. Appl. Nurs. Res. 1995, 8, 129–139. [Google Scholar] [CrossRef]
- Watson, B.J.; Salmoni, A.W.; Zecevic, A.A. The use of the Morse Fall Scale in an acute care hospital. Clin. Nurs. Stud. 2016, 4, 32–40. [Google Scholar] [CrossRef] [Green Version]
- Matarese, M.; Ivziku, D.; Bartolozzi, F.; Piredda, M.; De Marinis, M.G. Systematic review of fall risk screening tools for older patients in acute hospitals. J. Adv. Nurs. 2015, 71, 1198–1209. [Google Scholar] [CrossRef]
- Campanini, I.; Bargellini, A.; Mastrangelo, S.; Lombardi, F.; Tolomelli, S.; Lusuardi, M.; Merlo, A. Performance of the Hendrich Fall Risk Model II in Patients Discharged from Rehabilitation Wards. A Preliminary Study of Predictive Ability. Int. J. Environ. Res. Public Health 2021, 18, 1444. [Google Scholar] [CrossRef]
- Morse, J.M.; Morse, R.M.; Tylko, S.J. Development of a scale to identify the fall-prone patient. Can. J. Aging/Rev. Can. Vieil. 1989, 8, 366–377. [Google Scholar] [CrossRef]
- Jang, I.S.; Lee, S.G. Fall risk factors and characteristics of an acute hospital setting across clinical departments. J. Korean Acad. Fundam. Nurs. 2014, 21, 264–274. [Google Scholar] [CrossRef] [Green Version]
- Montero-Odasso, M.; van der Velde, N.; Martin, F.C.; Petrovic, M.; Tan, M.P.; Ryg, J.; Aguilar-Navarro, S.; Alexander, N.B.; Becker, C.; Blain, H.; et al. World guidelines for falls prevention and management for older adults: A global initiative. Age Ageing 2022, 51, afac205. [Google Scholar] [CrossRef] [PubMed]
- Quigley, P.A.; White, S.V. Hospital-based fall program measurement and improvement in high reliability organizations. Online J. Issues Nurs. 2013, 18, 1. [Google Scholar] [CrossRef]
- Oshiro, C.E.S.; Frankland, T.B.; Rosales, A.G.; Perrin, N.A.; Bell, C.L.; Lo, S.H.Y.; Trinacty, C.M. Fall ascertainment and development of a risk prediction model using electronic medical records. J. Am. Geriatr. Soc. 2019, 67, 1417–1422. [Google Scholar] [CrossRef]
- World Health Organization. Falls. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/falls (accessed on 17 April 2022).
- Hailpern, S.M.; Visintainer, P.F. Odds ratios and logistic regression: Further examples of their use and interpretation. Stata J. 2003, 3, 213–225. [Google Scholar] [CrossRef] [Green Version]
- Unal, I. Defining an Optimal Cut-Point Value in ROC Analysis: An Alternative Approach. Comput. Math. Methods Med. 2017, 2017, 2651. [Google Scholar] [CrossRef] [PubMed]
- Schober, P.; Vetter, T.R. Survival analysis and interpretation of time-to-event data: The tortoise and the hare. Anesth. Analg. 2018, 127, 792. [Google Scholar] [CrossRef]
- Cox, D.R. Regression Models and Life-Tables. J. R. Stat. Soc. Ser. B (Methodol.) 1972, 34, 187–220. Available online: http://www.jstor.org/stable/2985181 (accessed on 18 August 2022). [CrossRef]
- Kuitunen, I.; Ponkilainen, V.T.; Uimonen, M.M.; Eskelinen, A.; Reito, A. Testing the proportional hazards assumption in cox regression and dealing with possible non-proportionality in total joint arthroplasty research: Methodological perspectives and review. BMC Musculoskelet Disord. 2021, 22, 489. [Google Scholar] [CrossRef]
- Bellera, C.A.; MacGrogan, G.; Debled, M.; Tunon de Lara, C.; Brouste, V.; Mathoulin-Pélissier, S. Variables with time-varying effects and the Cox model: Some statistical concepts illustrated with a prognostic factor study in breast cancer. BMC Med. Res. Methodol. 2010, 10, 20. [Google Scholar] [CrossRef] [Green Version]
- De Souza, A.B.; Röhsig, V.; Maestri, R.N.; Mutlaq, M.F.P.; Lorenzini, E.; Alves, B.M.; Oliveira, D.; Gatto, D.C. In hospital falls of a large hospital. BMC Res. Notes 2019, 12, 284. [Google Scholar] [CrossRef] [PubMed]
- Mohsen, M.M.; Okby, O.M.; Elfeshawy, R. Fall Reduction Intervention for Hospitalized Pediatric Patients at Risk for falls. Menoufia Nurs. J. 2017, 2, 71–91. [Google Scholar] [CrossRef]
- Salari, N.; Darvishi, N.; Ahmadipanah, M.; Shohaimi, S.; Mohammadi, M. Global prevalence of falls in the older adults: A comprehensive systematic review and meta-analysis. J. Orthop. Surg. Res. 2022, 17, 334. [Google Scholar] [CrossRef]
- Tricco, A.C.; Thomas, S.M.; Veroniki, A.A.; Hamid, J.S.; Cogo, E.; Strifler, L.; Straus, S.E. Comparisons of interventions for preventing falls in older adults: A systematic review and meta-analysis. JAMA 2017, 318, 1687–1699. [Google Scholar] [CrossRef]
- Pasa, T.S.; Magnago, T.S.B.S.; Urbanetto, J.S.; Baratto, M.A.M.; Morais, B.X.; Carollo, J.B. Risk assessment and incidence of falls in adult hospitalized patients. Rev. Lat. Am. Enferm. 2017, 25, e2862. [Google Scholar] [CrossRef] [PubMed]
- Chow, S.K.; Lai, C.K.; Wong, T.K.; Suen, L.K.; Kong, S.K.; Chan, C.K.; Wong, I.Y. Evaluation of the Morse Fall Scale: Applicability in Chinese hospital populations. Int. J. Nurs. Stud. 2007, 44, 556–565. [Google Scholar] [CrossRef]
- Saverino, A.; Waller, D.; Rantell, K.; Parry, R.; Moriarty, A.; Playford, E.D. The role of cognitive factors in predicting balance and fall risk in a neuro-rehabilitation setting. PLoS ONE 2016, 11, e0153469. [Google Scholar] [CrossRef] [Green Version]
- Kawazoe, Y.; Shimamoto, K.; Shibata, D.; Shinohara, E.; Kawaguchi, H.; Yamamoto, T. Impact of a Clinical Text-Based Fall Prediction Model on Preventing Extended Hospital Stays for Elderly Inpatients: Model Development and Performance Evaluation. JMIR Med. Inform. 2022, 10, e37913. [Google Scholar] [CrossRef]
- Mitchell, R.J.; Lord, S.R.; Harvey, L.A.; Close, J.C. Associations between obesity and overweight and fall risk, health status and quality of life in older people. Aust. N. Z. J. Public Health 2014, 38, 13–18. [Google Scholar] [CrossRef]
- Alyono, J.C. Vertigo and Dizziness: Understanding and Managing Fall Risk. Otolaryngol. Clin. N. Am. 2018, 51, 725–740. [Google Scholar] [CrossRef]
- Stone, K.L.; Blackwell, T.L.; Ancoli-Israel, S.; Cauley, J.A.; Redline, S.; Marshall, L.M.; Ensrud, K.E.; Osteoporotic Fractures in Men Study Group. Sleep disturbances and risk of falls in older community-dwelling men: The outcomes of Sleep Disorders in Older Men (MrOS Sleep) Study. J. Am. Geriatr. Soc. 2014, 62, 299–305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mesas, A.E.; López-García, E.; Rodríguez-Artalejo, F. Self-reported sleep duration and falls in older adults. J. Sleep Res. 2011, 20 Pt 1, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Roggeman, S.; Weiss, J.P.; Van Laecke, E.; Vande Walle, J.; Everaert, K.; Bower, W.F. The role of lower urinary tract symptoms in fall risk assessment tools in hospitals: A review. F1000Research 2020, 9, 236. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.; Zhu, X.; Song, Y. Retrospective analysis and nursing management of inpatient falls: Case series. Medicine 2021, 100, e27977. [Google Scholar] [CrossRef]
- Rosendahl, E.; Lundin-Olsson, L.; Kallin, K.; Jensen, J.; Gustafson, Y.; Nyberg, L. Prediction of falls among older people in residential care facilities by the Downton index. Aging Clin. Exp. Res. 2003, 15, 142–147. [Google Scholar] [CrossRef] [Green Version]
- Sterke, C.S.; Ziere, G.; van Beeck, E.F.; Looman, C.W.; van der Cammen, T.J. Dose–response relationship between selective serotonin re-uptake inhibitors and injurious falls: A study in nursing home residents with dementia. Br. J. Clin. Pharmacol. 2012, 73, 812–820. [Google Scholar] [CrossRef] [PubMed]
- Ardaneh, M.; Fararouei, M.; Hassanzadeh, J. Factors Contributing to Falls Leading to Fracture among Older Adults. Popul. Ageing 2023, 16, 121–135. [Google Scholar] [CrossRef]
- Martinussen, T.; Scheike, T.H.; Skovgaard, I.M. Efficient estimation of fixed and time-varying covariate effects in multiplicative intensity models. Scand. J. Stat. 2002, 29, 57–74. [Google Scholar] [CrossRef]
- Tapper, E.B.; Nikirk, S.; Parikh, N.D.; Zhao, L. Falls are common, morbid, and predictable in patients with cirrhosis. J. Hepatol. 2021, 75, 582–588. [Google Scholar] [CrossRef]
- Bagui, S.; Long, T.; Bagui, S. Selecting the Optimal Morse Falls Scale Cut-Off Point for Patient Fall Risk. Health 2019, 11, 924. [Google Scholar] [CrossRef] [Green Version]
- Bóriková, I.; Tomagová, M.; Miertová, M.; Žiaková, K. Predictive value of the morse fall scale. Cent. Eur. J. Nurs. Midwifery 2017, 8, 588–595. [Google Scholar] [CrossRef] [Green Version]
- Sujianto, U.; Johan, A. Fall Risk Assessment Using Morse Fall Scale and STRATIFY Fall Scale. Avicenna J. Ilm. 2022, 17, 1–13. [Google Scholar] [CrossRef]

| Item | Scale | |
|---|---|---|
| 1. History of falling: immediate or within 3 months | No | 0 |
| Yes | 25 | |
| 2. Secondary diagnosis | No | 0 |
| Yes | 15 | |
| 3. Ambulatory aid | ||
| Bed rest/nurse assist | 0 | |
| Crutches/cane/walker | 15 | |
| Furniture | 30 | |
| 4. IV 1/Heparin lock | No | 0 |
| Yes | 20 | |
| 5. Gait/Transferring | ||
| Normal/bedrest/immobile | 0 | |
| Weak | 10 | |
| Impaired | 20 | |
| 6. Mental status | ||
| Oriented to own ability | 0 | |
| Forget limitations | 15 | |
| Variable | Total | Fall (n = 150) | Non-Fall (n = 300) | χ2, t | p-Value |
|---|---|---|---|---|---|
| n (%), Mean ± SD | n (%), Mean ± SD | n (%), Mean ± SD | |||
| Sex | 0.000 | 1.000 | |||
| Male | 222 (49.3) | 74 (33.3) | 148 (66.7) | ||
| Female | 228 (50.7) | 76 (33.3) | 152 (66.7) | ||
| Age 1 | 68.5 ± 14.9 | 68.9 ± 15.0 | 68.3 ± 14.8 | 0.403 | 0.687 |
| <65 | 151 (33.6) | 51 (33.8) | 100 (66.2) | 0.020 | 0.888 |
| ≥65 | 299 (66.4) | 99 (33.1) | 200 (66.9) |
| Variable | Total | Fall (n = 150) | Non-Fall (n = 300) | χ2, t | p-Value |
|---|---|---|---|---|---|
| n (%), Mean ± SD | n (%), Mean ± SD | n (%), Mean ± SD | |||
| MFS 1 | 25.82 ± 20.87 | 34.53 ± 21.49 | 21.47 ± 10.15 | −6.548 *** | <0.001 |
| No risk (0–24) | 229 (50.9) | 49 (21.4) | 180 (78.6) | 35.839 *** | <0.001 |
| Low risk (25–50) | 171 (38.0) | 71 (41.5) | 100 (58.5) | ||
| High risk (≥51) | 50 (11.1) | 30 (60.0) | 20 (40.0) | ||
| Length of stay 2 | 8.85 ± 6.71 | 11.86 ± 7.04 | 7.34 ± 6.011 | −7.089 *** | <0.001 |
| Department | 5.209 | 0.074 | |||
| Internal | 223 (49.6) | 63 (28.3) | 160 (71.7) | ||
| Surgical | 182 (40.4) | 69 (37.9) | 113 (62.1) | ||
| Others | 45 (10.0) | 18 (40.0) | 27 (60.0) | ||
| Hospitalization route 3 | 1.923 | 0.382 | |||
| ED | 158 (35.1) | 56 (35.4) | 102 (64.6) | ||
| OPD/IPD | 284 (63.1) | 93 (32.7) | 191 (67.3) | ||
| Others | 8 (1.8) | 1 (12.5) | 7 (87.5) | ||
| History of admission | 9.512 ** | 0.002 | |||
| No | 142 (31.6) | 33 (23.2) | 109 (76.8) | ||
| Yes | 308 (68.4) | 117 (38.0) | 191 (62.0) | ||
| History of surgery | 2.263 | 0.133 | |||
| No | 175 (38.9) | 51 (29.1) | 124 (70.9) | ||
| Yes | 275 (61.1) | 99 (36.0) | 176 (64.0) | ||
| Dizziness | 6.801 ** | 0.009 | |||
| No | 407 (90.4) | 128 (31.4) | 279 (68.6) | ||
| Yes | 43 (9.6) | 22 (51.2) | 21 (48.8) | ||
| Vision impairment | 0.450 | ||||
| No | 442 (98.2) | 146 (33.0) | 296 (67.0) | ||
| Yes | 8 (1.8) | 4 (50.0) | 4 (50.0) | ||
| Hearing impairment | 1.549 | 0.211 | |||
| No | 415 (92.2) | 135 (32.5) | 280 (67.5) | ||
| Yes | 35 (7.8) | 15 (42.9) | 20 (57.1) | ||
| Sleep disorder | 19.565 *** | <0.001 | |||
| No | 414 (92.0) | 126 (30.4) | 288 (69.6) | ||
| Yes | 36 (8.0) | 24 (66.7) | 12 (33.3) | ||
| Bowel dysfunction | <0.001 | ||||
| No | 443 (98.4) | 143 (32.3) | 300 (67.7) | ||
| Yes | 7 (1.6) | 7 (100.0) | 0 (0.0) | ||
| Urinary incontinence | 25.532 *** | <0.001 | |||
| No | 423 (94.0) | 129 (30.5) | 294 (69.5) | ||
| Yes | 27 (6.0) | 21 (77.8) | 6 (22.2) | ||
| BMI 4 | 22.96 ± 3.69 | 23.29 ± 3.84 | 22.79 ± 3.61 | −1.363 | 0.174 |
| Underweight | 44 (9.9) | 15 (34.1) | 29 (65.9) | 4.115 | 0.249 |
| Normal | 278 (62.6) | 85 (30.6) | 193 (69.4) | ||
| Overweight | 107 (24.1) | 44 (41.1) | 63 (58.9) | ||
| Obesity | 15 (3.4) | 6 (40.0) | 9 (60.0) |
| Variable | No Risk (n = 229) | Low Risk (n = 171) | High Risk (n = 50) | χ2, t | p-Value |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| Dizziness | 13.684 ** | 0.001 | |||
| No | 218 (53.5) | 144 (35.4) | 45 (11.1) | ||
| Yes | 11 (25.6) | 27 (62.8) | 5 (11.6) | ||
| Vision impairment | 4.912 | 0.086 | |||
| No | 227 (51.4) | 165 (37.3) | 50 (11.3) | ||
| Yes | 2 (25.0) | 6 (75.0) | 0 (0.0) | ||
| Hearing impairment | 4.201 | 0.122 | |||
| No | 217 (52.3) | 153 (36.9) | 45 (10.8) | ||
| Yes | 12 (34.3) | 18 (51.4) | 5 (14.3) | ||
| Sleep disorder | 11.499 ** | 0.003 | |||
| No | 216 (52.2) | 158 (38.2) | 40 (9.6) | ||
| Yes | 13 (36.1) | 13 (36.1) | 10 (27.8) | ||
| Bowel dysfunction | 0.285 | 0.869 | |||
| No | 225 (50.8) | 169 (38.1) | 49 (11.1) | ||
| Yes | 4 (57.1) | 2 (28.6) | 1 (14.3) | ||
| Urinary incontinence | 19.122 *** | <0.001 | |||
| No | 226 (53.4) | 151 (35.7) | 46 (10.9) | ||
| Yes | 3 (11.1) | 20 (74.1) | 4 (14.8) |
| Variable | B | S.E. | Wald | df | p-Value | exp (B) |
|---|---|---|---|---|---|---|
| MFS 1 | ||||||
| No risk (0–24) | ||||||
| Low risk (25–50) | 0.679 | 0.244 | 7.765 | 1.000 | 0.005 ** | 1.97 |
| High risk (≥51) | 1.196 | 0.355 | 11.355 | 1.000 | 0.001 ** | 3.31 |
| Length of stay 2 | 0.080 | 0.017 | 22.356 | 1.000 | <0.001 *** | 1.08 |
| Sleep disorder | ||||||
| No | ||||||
| Yes | 1.291 | 0.400 | 10.437 | 1.000 | 0.001 ** | 3.64 |
| Urinary incontinence | ||||||
| No | ||||||
| Yes | 1.704 | 0.502 | 11.518 | 1.000 | 0.001 ** | 5.49 |
| Goodness of fit | ||||||
| Cox&Snell R2/Nagelkerke R2 | 0.197/0.273 | |||||
| χ2(df), p-value | 97.577(7), <0.001 | |||||
| Variable | Unadjusted OR 1 | Adjusted OR 2 | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| MFS 3 | ||||
| No risk (0–24) | ||||
| Low risk (25–50) | 2.61 (1.68–4.04) *** | <0.001 | 1.95 (1.21–3.13) ** | 0.006 |
| High risk (≥ 51) | 5.51 (2.88–10.53) *** | <0.001 | 3.34 (1.66–6.70) ** | 0.001 |
| Length of stay 4 | 1.11 (1.07–1.14) *** | <0.001 | 1.08 (1.05–1.12) *** | <0.001 |
| Sleep disorder | ||||
| No | ||||
| Yes | 4.57 (2.22–9.43) *** | <0.001 | 3.70 (1.69–8.10) ** | 0.001 |
| Urinary incontinence | ||||
| No | ||||
| Yes | 7.98 (3.15–20.23) *** | <0.001 | 5.61 (2.10–15.02) ** | 0.001 |
| Variable | Unadjusted HR 1 | Adjusted HR 2 | ||
|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | |
| MFS 3 | ||||
| No risk (0–24) | ||||
| Low risk (25–50) | 1.48 (0.86–2.53) | 0.154 | 1.52 (0.88–2.63) | 0.135 |
| High risk (≥51) | 3.85 (1.99–7.46) *** | <0.001 | 4.56 (2.31–9.00) *** | <0.001 |
| Length of stay 4 | 1.00 (0.96–1.04) | 0.927 | 0.94 (0.91–0.97) *** | <0.001 |
| Sleep disorder | ||||
| No | ||||
| Yes | 3.84 (2.11–6.98) *** | <0.001 | 2.23 (1.41–3.54) ** | 0.001 |
| Urinary incontinence | ||||
| No | ||||
| Yes | 2.24 (1.41–3.56) ** | 0.001 | 2.22 (1.36–3.63) ** | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, M.-J.; Seo, B.-J.; Kim, M.-Y. Time-Varying Hazard of Patient Falls in Hospital: A Retrospective Case–Control Study. Healthcare 2023, 11, 2194. https://doi.org/10.3390/healthcare11152194
Lee M-J, Seo B-J, Kim M-Y. Time-Varying Hazard of Patient Falls in Hospital: A Retrospective Case–Control Study. Healthcare. 2023; 11(15):2194. https://doi.org/10.3390/healthcare11152194
Chicago/Turabian StyleLee, Mi-Joon, Bum-Jeun Seo, and Myo-Youn Kim. 2023. "Time-Varying Hazard of Patient Falls in Hospital: A Retrospective Case–Control Study" Healthcare 11, no. 15: 2194. https://doi.org/10.3390/healthcare11152194
APA StyleLee, M.-J., Seo, B.-J., & Kim, M.-Y. (2023). Time-Varying Hazard of Patient Falls in Hospital: A Retrospective Case–Control Study. Healthcare, 11(15), 2194. https://doi.org/10.3390/healthcare11152194






