Responsiveness and Minimal Important Change of the Arabic Disabilities of the Arm, Shoulder and Hand (DASH) in Patients with Upper Extremity Musculoskeletal Disorders
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Participants
2.2. Procedure
2.3. Outcome Measures
2.3.1. Disabilities of the Arm, Shoulder and Hand (DASH)
2.3.2. Numeric Pain Rating Scale (NPRS)
2.3.3. Global Assessment of Function (GAF)
2.3.4. Global Rating of Change Scale (GRC)
2.3.5. Statistical Analysis
2.4. Sample Size Estimation
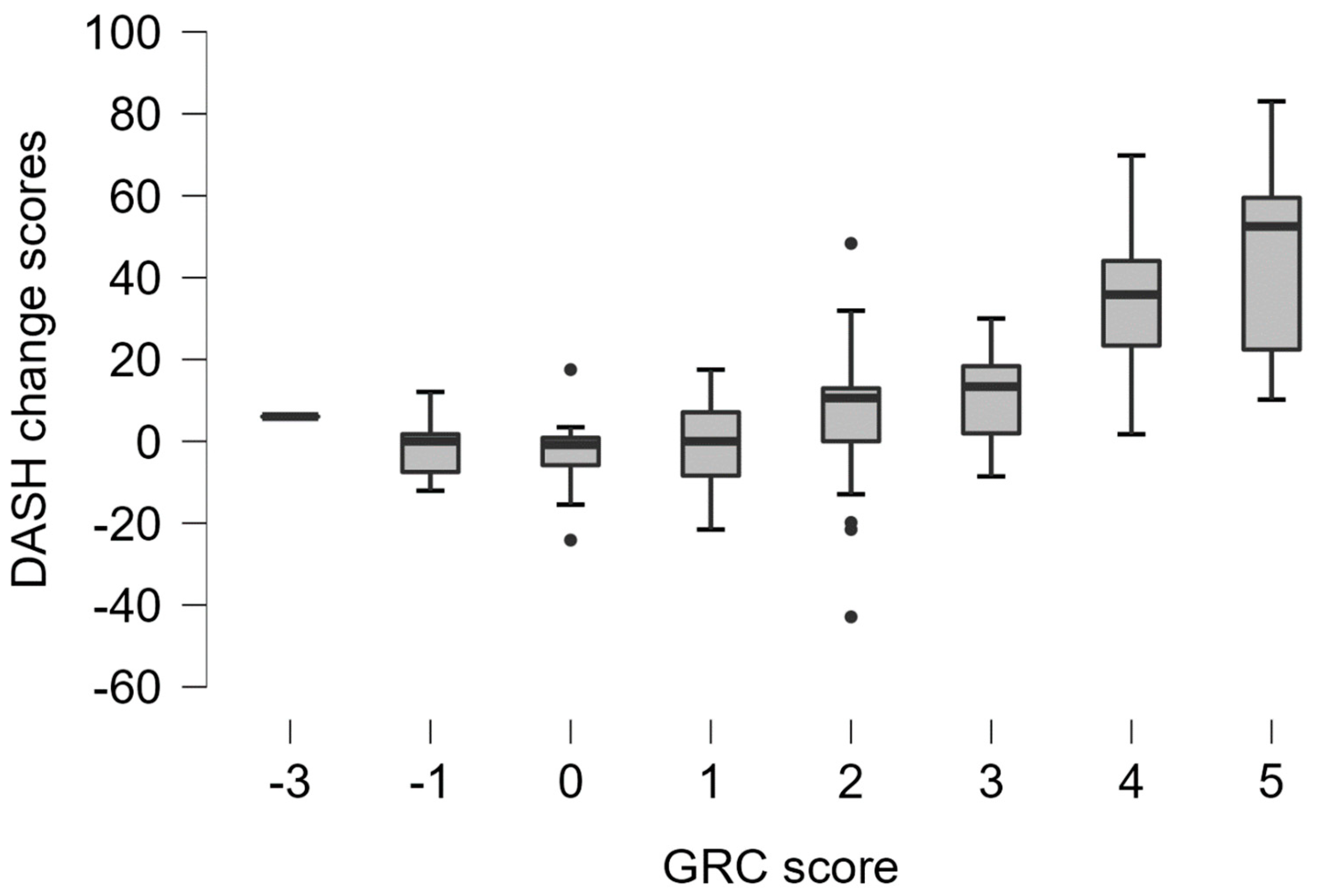
3. Results
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hudak, P.L.; Amadio, P.C.; Bombardier, C. Development of an upper extremity outcome measure: The DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am. J. Ind. Med. 1996, 29, 602–608. [Google Scholar] [CrossRef]
- Beaton, D.E.; Katz, J.N.; Fossel, A.H.; Wright, J.G.; Tarasuk, V.; Bombardier, C. Measuring the whole or the parts? Validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J. Hand Ther. 2001, 14, 128–146. [Google Scholar] [CrossRef]
- de Klerk, S.; Buchanan, H.; Jerosch-Herold, C. The validity and clinical utility of the Disabilities of the Arm Shoulder and Hand questionnaire for hand injuries in developing country contexts: A systematic review. J. Hand Ther. 2018, 31, 80–90.e1. [Google Scholar] [CrossRef]
- Wajngarten, D.; Campos, J.; Garcia, P. The Disabilities of the Arm, Shoulder and Hand scale in the evaluation of disability—A literature review. Med. Lav. 2017, 108, 314–323. [Google Scholar]
- Sigirtmac, I.C.; Oksuz, C. Systematic review of the quality of the cross-cultural adaptations of Disabilities of the Arm, Shoulder and Hand (DASH). Med. Lav. 2021, 112, 279–291. [Google Scholar]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; de Vet, H.C. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J. Clin. Epidemiol. 2010, 63, 737–745. [Google Scholar] [CrossRef]
- Mokkink, L.B.; Terwee, C.B.; Knol, D.L.; Stratford, P.W.; Alonso, J.; Patrick, D.L.; Bouter, L.M.; de Vet, H.C. The COSMIN checklist for evaluating the methodological quality of studies on measurement properties: A clarification of its content. BMC Med. Res. Methodol. 2010, 10, 22. [Google Scholar] [CrossRef] [PubMed]
- Prinsen, C.A.C.; Mokkink, L.B.; Bouter, L.M.; Alonso, J.; Patrick, D.L.; de Vet, H.C.W.; Terwee, C.B. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual. Life Res. 2018, 27, 1147–1157. [Google Scholar] [CrossRef] [PubMed]
- Alotaibi, N.M.; Aljadi, S.H.; Alrowayeh, H.N. Reliability, validity and responsiveness of the Arabic version of the Disability of Arm, Shoulder and Hand (DASH-Arabic). Disabil. Rehabil. 2016, 38, 2469–2478. [Google Scholar] [CrossRef] [PubMed]
- Lundquist, C.B.; Dossing, K.; Christiansen, D.H. Responsiveness of a Danish version of the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire. Dan. Med. J. 2014, 61, A4813. [Google Scholar] [PubMed]
- Chanthana, P.; Atthakomol, P.; Manosroi, W.; Wongpakaran, T.; Kraisarin, J.; Sananpanich, K. Comparison of patient preferences and responsiveness among common patient-reported outcome measures for hand/wrist injuries or disorders. J. Orthop. Traumatol. 2023, 24, 2. [Google Scholar] [CrossRef]
- Gummesson, C.; Atroshi, I.; Ekdahl, C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: Longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet. Disord. 2003, 4, 11. [Google Scholar] [CrossRef] [PubMed]
- Greenslade, J.R.; Mehta, R.L.; Belward, P.; Warwick, D.J. Dash and Boston questionnaire assessment of carpal tunnel syndrome outcome: What is the responsiveness of an outcome questionnaire? J. Hand Surg. Br. 2004, 29, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Schonnemann, J.O.; Larsen, K.; Hansen, T.B.; Soballe, K. Reliability and validity of the Danish version of the disabilities of arm, shoulder, and hand questionnaire in patients with fractured wrists. J. Plast. Surg. Hand Surg. 2011, 45, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.P.; Tiruttani, R.; Kaur, M.N.; MacDermid, J.; Karim, R. Psychometric Properties of the Hindi Version of the Disabilities of Arm, Shoulder, and Hand: A Pilot Study. Rehabil. Res. Pract. 2015, 2015, 482378. [Google Scholar] [CrossRef]
- Imaeda, T.; Toh, S.; Nakao, Y.; Nishida, J.; Hirata, H.; Ijichi, M.; Kohri, C.; Nagano, A. Validation of the Japanese Society for Surgery of the Hand version of the Disability of the Arm, Shoulder, and Hand questionnaire. J. Orthop. Sci. 2005, 10, 353–359. [Google Scholar] [CrossRef]
- De Vet, H.C.; Terwee, C.B.; Mokkink, L.B.; Knol, D.L. Measurement in Medicine: A Practical Guide; Cambridge University Press: Cambridge, UK, 2011. [Google Scholar]
- Revicki, D.; Hays, R.D.; Cella, D.; Sloan, J. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J. Clin. Epidemiol. 2008, 61, 102–109. [Google Scholar] [CrossRef]
- Terwee, C.B.; Peipert, J.D.; Chapman, R.; Lai, J.-S.; Terluin, B.; Cella, D.; Griffith, P.; Mokkink, L.B. Minimal important change (MIC): A conceptual clarification and systematic review of MIC estimates of PROMIS measures. Qual. Life Res. 2021, 30, 2729–2754. [Google Scholar] [CrossRef]
- Franchignoni, F.; Vercelli, S.; Giordano, A.; Sartorio, F.; Bravini, E.; Ferriero, G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH). J. Orthop. Sports Phys. Ther. 2014, 44, 30–39. [Google Scholar] [CrossRef]
- Rysstad, T.; Røe, Y.; Haldorsen, B.; Svege, I.; Strand, L.I. Responsiveness and minimal important change of the Norwegian version of the Disabilities of the Arm, Shoulder and Hand questionnaire (DASH) in patients with subacromial pain syndrome. BMC Musculoskelet. Disord. 2017, 18, 248. [Google Scholar] [CrossRef]
- Mahabier, K.C.; Hartog, D.D.; Theyskens, N.; Verhofstad, M.H.; Van Lieshout, E.M.; Bos, P.K.; Bronkhorst, M.W.; Bruijninckx, M.M.; De Haan, J.; Hoed, P.T.D.; et al. Reliability, validity, responsiveness, and minimal important change of the Disabilities of the Arm, Shoulder and Hand and Constant-Murley scores in patients with a humeral shaft fracture. J. Shoulder Elb. Surg. 2017, 26, e1–e12. [Google Scholar]
- Negahban, H.; Behtash, Z.; Sohani, S.M.; Salehi, R. Responsiveness of two Persian-versions of shoulder outcome measures following physiotherapy intervention in patients with shoulder disorders. Disabil. Rehabil. 2015, 37, 2300–2304. [Google Scholar] [CrossRef]
- Farzad, M.; MacDermid, J.C.; Shafiee, E.; Beygi, A.S.; Vafaei, A.; Varahra, A.; Beikpour, H. Clinimetric testing of the Persian version of the Patient-Rated Tennis Elbow Evaluation (PRTEE) and the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaires in patients with lateral elbow tendinopathy. Disabil. Rehabil. 2022, 44, 2902–2907. [Google Scholar] [CrossRef]
- Kc, S.; Sharma, S.; Ginn, K.; Almadi, T.; Subedi, H.; Reed, D. Cross-cultural adaptation and measurement properties of the Nepali version of the DASH (disability of arm, shoulder and hand) in patients with shoulder pain. Health Qual. Life Outcomes 2019, 17, 51. [Google Scholar]
- Terluin, B.; Eekhout, I.; Terwee, C.B.; de Vet, H.C. Minimal important change (MIC) based on a predictive modeling approach was more precise than MIC based on ROC analysis. J. Clin. Epidemiol. 2015, 68, 1388–1396. [Google Scholar] [CrossRef]
- Terluin, B.; Eekhout, I.; Terwee, C.B. The anchor-based minimal important change, based on receiver operating characteristic analysis or predictive modeling, may need to be adjusted for the proportion of improved patients. J. Clin. Epidemiol. 2017, 83, 90–100. [Google Scholar] [CrossRef]
- Alghadir, A.H.; Anwer, S.; Iqbal, Z.A. The psychometric properties of an Arabic numeric pain rating scale for measuring osteoarthritis knee pain. Disabil. Rehabil. 2016, 38, 2392–2397. [Google Scholar] [CrossRef]
- Alnahdi, A.H.; Alrashid, G.I.; Alkhaldi, H.A.; Aldali, A.Z. Cross-cultural adaptation, validity and reliability of the Arabic version of the Lower Extremity Functional Scale. Disabil. Rehabil. 2016, 38, 897–904. [Google Scholar] [CrossRef]
- Alnahdi, A.H. Validity and reliability of the Arabic quick disabilities of the arm, Shoulder and Hand (QuickDASH-Arabic). Musculoskelet. Sci. Pract. 2021, 53, 102372. [Google Scholar]
- Aljathlani, M.F.; Alshammari, M.O.; Alsuwaygh, M.A.; Al-Mutairi, M.S.; Aljassir, F.F.; Bindawas, S.M.; Alnahdi, A.H. Cross-cultural adaptation and validation of the Arabic version of the upper extremity functional index. Disabil. Rehabil. 2022, 44, 5656–5662. [Google Scholar]
- Kamper, S.J.; Maher, C.G.; Mackay, G. Global rating of change scales: A review of strengths and weaknesses and considerations for design. J. Man. Manip. Ther. 2009, 17, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Hawker, G.A.; Mian, S.; Kendzerska, T.; French, M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. 2011, 63 (Suppl. S11), S240–S252. [Google Scholar]
- Alnahdi, A.H. Measurement properties of the 15-item Arabic lower extremity functional scale. Disabil. Rehabil. 2021, 43, 3839–3844. [Google Scholar] [CrossRef] [PubMed]
- Mokkink, L.B.; De Vet, H.C.W.; Prinsen, C.A.C.; Patrick, D.L.; Alonso, J.; Bouter, L.M.; Terwee, C.B. COSMIN Risk of Bias checklist for systematic reviews of Patient-Reported Outcome Measures. Qual. Life Res. 2018, 27, 1171–1179. [Google Scholar] [CrossRef] [PubMed]
- Prinsen, C.A.C.; Vohra, S.; Rose, M.R.; Boers, M.; Tugwell, P.; Clarke, M.; Williamson, P.R.; Terwee, C.B. How to select outcome measurement instruments for outcomes included in a “Core Outcome Set”—A practical guideline. Trials 2016, 17, 449. [Google Scholar] [CrossRef] [PubMed]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice, 3rd ed.; Pearson/Prentice Hall: Upper Saddle River, NJ, USA, 2009. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: London, UK, 2013. [Google Scholar]
- Deyo, R.A.; Centor, R.M. Assessing the responsiveness of functional scales to clinical change: An analogy to diagnostic test performance. J. Chronic Dis. 1986, 39, 897–906. [Google Scholar] [CrossRef]
- Terluin, B.; Roos, E.M.; Terwee, C.B.; Thorlund, J.B.; Ingelsrud, L.H. Assessing baseline dependency of anchor-based minimal important change (MIC): Don’t stratify on the baseline score! Qual. Life Res. 2021, 30, 2773–2782. [Google Scholar] [CrossRef]
- Terwee, C.B.; Mokkink, L.B.; Knol, D.L.; Ostelo, R.W.J.G.; Bouter, L.M.; de Vet, H.C.W. Rating the methodological quality in systematic reviews of studies on measurement properties: A scoring system for the COSMIN checklist. Qual. Life Res. 2012, 21, 651–657. [Google Scholar] [CrossRef]
- Schmitt, J.; Di Fabio, R.P. The validity of prospective and retrospective global change criterion measures. Arch. Phys. Med. Rehabil. 2005, 86, 2270–2276. [Google Scholar] [CrossRef]
- Schmitt, J.S.; Di Fabio, R.P. Reliable change and minimum important difference (MID) proportions facilitated group responsiveness comparisons using individual threshold criteria. J. Clin. Epidemiol. 2004, 57, 1008–1018. [Google Scholar] [CrossRef]
- MacDermid, J.C.; Tottenham, V. Responsiveness of the disability of the arm, shoulder, and hand (DASH) and patient-rated wrist/hand evaluation (PRWHE) in evaluating change after hand therapy. J. Hand Ther. 2004, 17, 18–23. [Google Scholar] [CrossRef]
- Terwee, C.B.; Bot, S.D.M.; de Boer, M.R.; van der Windt, D.A.W.M.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C.W. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Hao, Q.; Devji, T.; Zeraatkar, D.; Wang, Y.; Qasim, A.; Siemieniuk, R.A.; Vandvik, P.O.; Lähdeoja, T.; Carrasco-Labra, A.; Agoritsas, T.; et al. Minimal important differences for improvement in shoulder condition patient-reported outcomes: A systematic review to inform a BMJ Rapid Recommendation. BMJ Open 2019, 9, e028777. [Google Scholar] [CrossRef] [PubMed]
- Wojnicz, W.; Sobierajska-Rek, A.; Zagrodny, B.; Ludwicki, M.; Jabłońska-Brudło, J.; Forysiak, K. A New Approach to Assess Quality of Motion in Functional Task of Upper Limb in Duchenne Muscular Dystrophy. Appl. Sci. 2022, 12, 12247. [Google Scholar] [CrossRef]

| Pre-Defined Hypotheses | Hypothesis Supported |
|---|---|
| 1. DASH change scores demonstrate a positive correlation with GAF change scores (≥0.4). | Yes |
| 2. DASH change scores demonstrate a positive correlation with NPRS change scores (≥0.4). | Yes |
| 3. DASH change scores demonstrate a positive correlation with GRC scores (≥0.4). | Yes |
| 4. The DASH demonstrates an effect size (ES, SRM) of at least 0.5 in participants with a reported improvement in upper extremity function (GRC ≥ 3). | Yes |
| 5. DASH change scores differentiate between participants with a reported improvement in upper extremity function and those with no improvement (area under the ROC curve (AUC) ≥ 0.70). | Yes |
| Variable | Mean ± SD or N (%) |
|---|---|
| Age (year) | 38.18 ± 13.98 |
| Sex | |
| Male | 72 (62.6) |
| Female | 43 (37.4) |
| Height (m) | 1.68 ± 0.09 |
| Mass (kg) | 76.39 ±16.56 |
| Body mass index (kg/m2) | 27.26 ± 5.99 |
| Site of dysfunction | |
| Shoulder and arm | 50 (43.5) |
| Elbow and forearm | 21 (18.3) |
| Wrist and hand | 44 (38.3) |
| Upper extremity surgery | |
| Yes | 51 (44.3) |
| Time after surgery (months) | 1.84 (2.76) * |
| No | 64 (55.7) |
| Duration of symptoms (months) | 2.99 (7.71) * |
| Variable | Baseline Scores Mean ± SD | Follow-Up Scores Mean ± SD | Change Scores Mean ± SD | ES | SRM | Baseline | Follow-Up | ||
|---|---|---|---|---|---|---|---|---|---|
| Floor | Ceiling | Floor | Ceiling | ||||||
| DASH (0–100) | 47.47 ± 21.17 | 30.33 ± 23.66 | 17.14 ± 24.73 | 0.81 | 0.69 | 0% | 0% | 0% | 10.4% |
| Improved (N = 56) | 52.52 ± 21.50 | 19.53 ± 20.46 | 32.99 ± 23.23 | 1.53 | 1.42 | ||||
| Unchanged (N = 58) | 42.25 ± 19.77 | 40.22 ± 22.03 | 2.03 ± 14.88 | 0.10 | 0.14 | ||||
| GAF (0–100) | 58.70 ± 19.65 | 75.83 ± 20.74 | 17.14 ± 22.16 | 0.87 | 0.77 | 0% | 0% | 0% | 12.2% |
| NPRS (0–10) | 5.00 ± 2.41 | 3.17 ± 2.81 | 1.84 ± 2.90 | 0.76 | 0.63 | 2.6% | 3.5% | 1.7% | 25.2% |
| Variable | N (%) |
|---|---|
| GRC | |
| 5 (Very great deal better) | 25 (21.7) |
| 4 (Great deal better) | 15 (13.0) |
| 3 (Moderately better) | 16 (13.9) |
| 2 (Little bit better) | 26 (22.6) |
| 1 (A tiny bit better, almost the same) | 14 (12.2) |
| 0 (No change) | 13 (11.3) |
| −1 (Tiny bit worse, almost the same) | 5 (4.3) |
| −2 (Little bit worse) | 0 (0.0) |
| −3 (Moderately worse) | 1 (0.9) |
| −4 (Great deal worse) | 0 (0.0) |
| −5 (Very great deal worse) | 0 (0.0) |
| Change over time status according to GRC score | |
| Unchanged vs. Improved vs. Worsened | |
| Unchanged (GRC −2 to 2) | 58 (50.4) |
| Improved (GRC ≥ 3) | 56 (48.7) |
| Worsened (GRC ≤ -3) | 1 (0.9) |
| Improved vs. Not improved | |
| Improved (GRC ≥ 3) | 56 (48.7) |
| Not improved (GRC ≤ 2) | 59 (51.3) |
| Variable | r (95% CI) | p |
|---|---|---|
| GAF change | 0.69 (0.55 to 0.81) | <0.001 |
| NPRS change | 0.68 (0.57 to 0.77) | <0.001 |
| GRC | 0.73 (0.64 to 0.80) * | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alnahdi, A.H. Responsiveness and Minimal Important Change of the Arabic Disabilities of the Arm, Shoulder and Hand (DASH) in Patients with Upper Extremity Musculoskeletal Disorders. Healthcare 2023, 11, 2623. https://doi.org/10.3390/healthcare11192623
Alnahdi AH. Responsiveness and Minimal Important Change of the Arabic Disabilities of the Arm, Shoulder and Hand (DASH) in Patients with Upper Extremity Musculoskeletal Disorders. Healthcare. 2023; 11(19):2623. https://doi.org/10.3390/healthcare11192623
Chicago/Turabian StyleAlnahdi, Ali H. 2023. "Responsiveness and Minimal Important Change of the Arabic Disabilities of the Arm, Shoulder and Hand (DASH) in Patients with Upper Extremity Musculoskeletal Disorders" Healthcare 11, no. 19: 2623. https://doi.org/10.3390/healthcare11192623
APA StyleAlnahdi, A. H. (2023). Responsiveness and Minimal Important Change of the Arabic Disabilities of the Arm, Shoulder and Hand (DASH) in Patients with Upper Extremity Musculoskeletal Disorders. Healthcare, 11(19), 2623. https://doi.org/10.3390/healthcare11192623






