Association between Periodontitis and HbA1c Levels in Non-Diabetic Patients: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Search Results
3.2. Study Characteristics
3.3. Methodological Quality
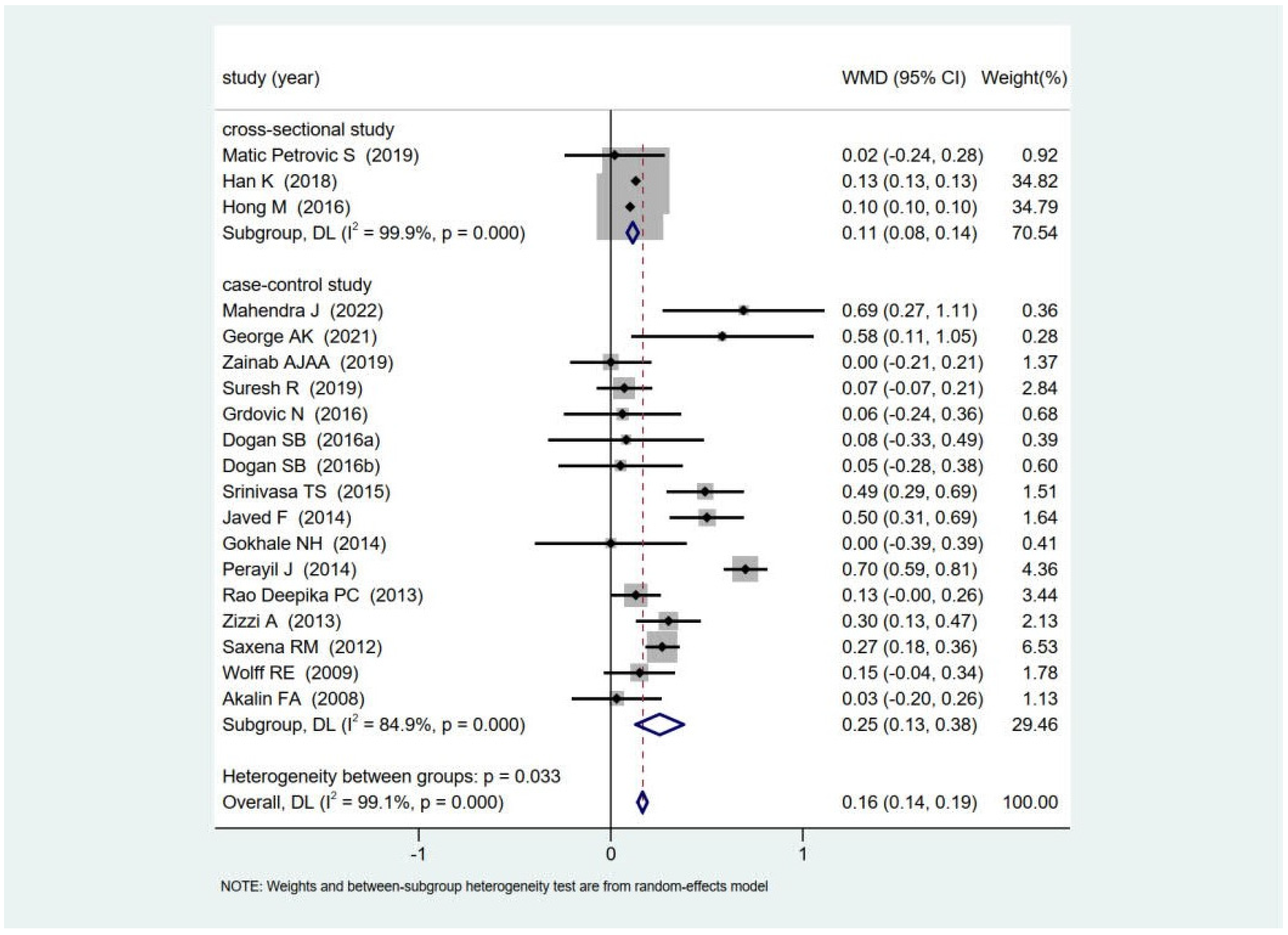
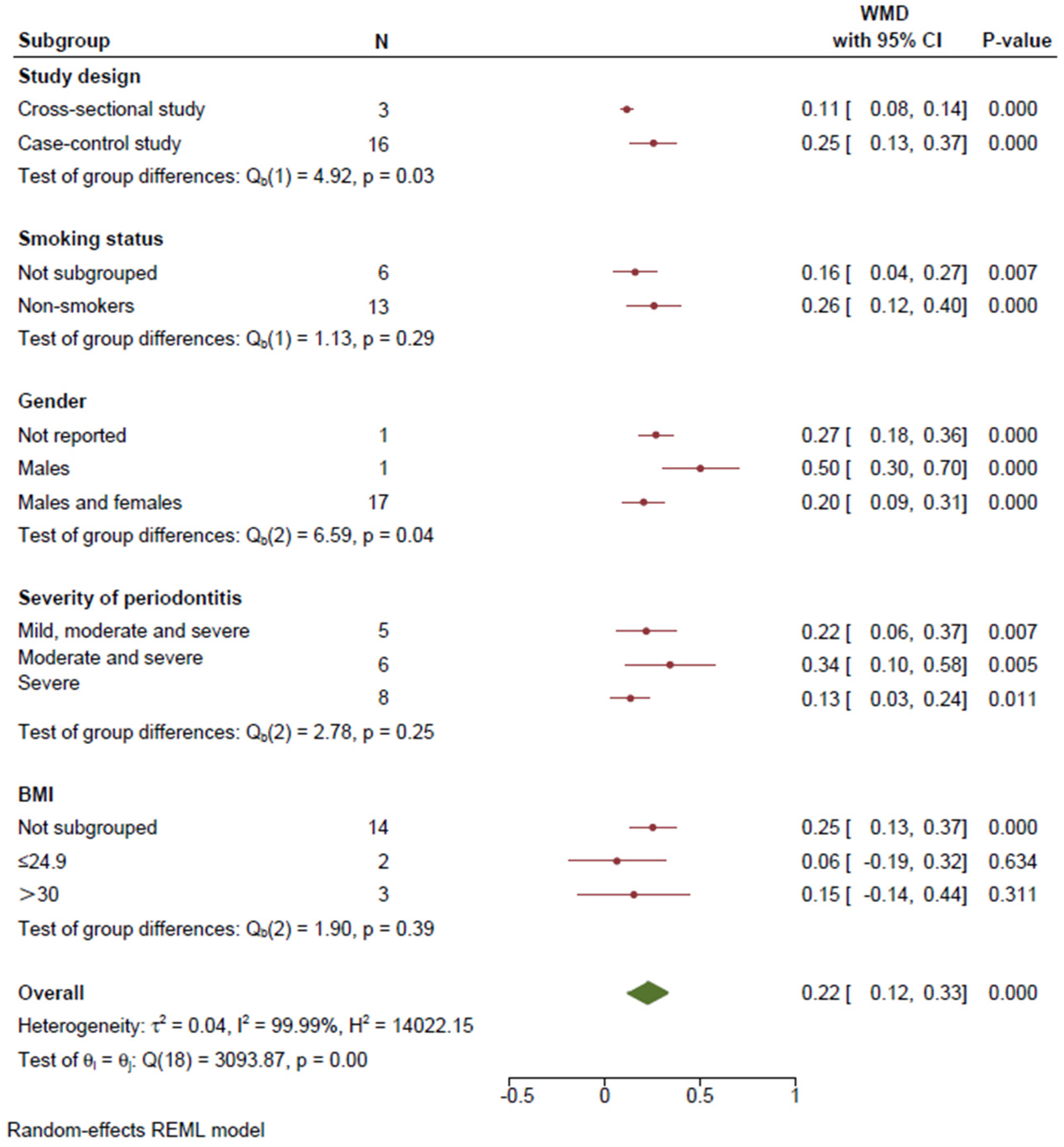
3.4. Meta-Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hajishengallis, G.L.J. Complement and dysbiosis in periodontal disease. Immunobiology 2012, 217, 1111–1116. [Google Scholar] [CrossRef] [PubMed]
- Spahr, A.; Divnic-Resnik, T. Impact of health and lifestyle food supplements on periodontal tissues and health. Periodontology 2000 2022, 90, 146–175. [Google Scholar] [CrossRef] [PubMed]
- Peres, M.A.; Macpherson, L.M.D.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreno, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef]
- Diseases, G.B.D.; Injuries, C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Luo, L.S.; Luan, H.H.; Jiang, J.F.; Wu, L.; Li, C.; Leng, W.D.; Zeng, X.T. The spatial and temporal trends of severe periodontitis burden in Asia, 1990–2019: A population-based epidemiological study. J. Periodontol. 2022, 93, 1615–1625. [Google Scholar] [CrossRef]
- Hajishengallis, G.; Chavakis, T. Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities. Nat. Rev. Immunol. 2021, 21, 426–440. [Google Scholar] [CrossRef]
- Genco, R.J.; Sanz, M. Clinical and public health implications of periodontal and systemic diseases: An overview. Periodontology 2000 2020, 83, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Garcia, M.; Hernandez-Lemus, E. Periodontal Inflammation and Systemic Diseases: An Overview. Front. Physiol. 2021, 12, 709438. [Google Scholar] [CrossRef]
- Bui, F.Q.; Almeida-da-Silva, C.L.C.; Huynh, B.; Trinh, A.; Liu, J.; Woodward, J.; Asadi, H.; Ojcius, D.M. Association between periodontal pathogens and systemic disease. Biomed. J. 2019, 42, 27–35. [Google Scholar] [CrossRef]
- Beck, J.D.; Papapanou, P.N.; Philips, K.H.; Offenbacher, S. Periodontal Medicine: 100 Years of Progress. J. Dent. Res. 2019, 98, 1053–1062. [Google Scholar] [CrossRef]
- Shoelson, S.E.; Lee, J.; Goldfine, A.B. Inflammation and insulin resistance. J. Clin. Investig. 2006, 116, 1793–1801. [Google Scholar] [CrossRef] [PubMed]
- Loos, B.G.; Craandijk, J.; Hoek, F.J.; Wertheim-van Dillen, P.M.; van der Velden, U. Elevation of systemic markers related to cardiovascular diseases in the peripheral blood of periodontitis patients. J. Periodontol. 2000, 71, 1528–1534. [Google Scholar] [CrossRef]
- Tonetti, M.S.; D’Aiuto, F.; Nibali, L.; Donald, A.; Storry, C.; Parkar, M.; Suvan, J.; Hingorani, A.D.; Vallance, P.; Deanfield, J. Treatment of periodontitis and endothelial function. N. Engl. J. Med. 2007, 356, 911–920. [Google Scholar] [CrossRef] [PubMed]
- Genco, R.J.; Genco, F.D. Common risk factors in the management of periodontal and associated systemic diseases: The dental setting and interprofessional collaboration. J. Evid. Based Dent. Pract. 2014, 14, 4–16. [Google Scholar] [CrossRef] [PubMed]
- Stanko, P.; Izakovicova Holla, L. Bidirectional association between diabetes mellitus and inflammatory periodontal disease. A review. Biomed. Pap. Med. Fac. Univ. Palacky. Olomouc. Czechoslov. 2014, 158, 35–38. [Google Scholar] [CrossRef]
- Preshaw, P.M.; Alba, A.L.; Herrera, D.; Jepsen, S.; Konstantinidis, A.; Makrilakis, K.; Taylor, R. Periodontitis and diabetes: A two-way relationship. Diabetologia 2012, 55, 21–31. [Google Scholar] [CrossRef]
- Taylor, G.W.; Burt, B.A.; Becker, M.P.; Genco, R.J.; Shlossman, M.; Knowler, W.C.; Pettitt, D.J. Severe periodontitis and risk for poor glycemic control in patients with non-insulin-dependent diabetes mellitus. J. Periodontol. 1996, 67, 1085–1093. [Google Scholar] [CrossRef]
- Grossi, S.G.; Genco, R.J. Periodontal disease and diabetes mellitus: A two-way relationship. Ann. Periodontol. 1998, 3, 51–61. [Google Scholar] [CrossRef]
- Mealey, B.L.; Ocampo, G.L. Diabetes mellitus and periodontal disease. Periodontology 2000 2007, 44, 127–153. [Google Scholar] [CrossRef]
- Lang, N.P.; Suvan, J.E.; Tonetti, M.S. Risk factor assessment tools for the prevention of periodontitis progression a systematic review. J. Clin. Periodontol. 2015, 42 (Suppl. S16), S59–S70. [Google Scholar] [CrossRef]
- Rapone, B.; Ferrara, E.; Corsalini, M.; Qorri, E.; Converti, I.; Lorusso, F.; Delvecchio, M.; Gnoni, A.; Scacco, S.; Scarano, A. Inflammatory Status and Glycemic Control Level of Patients with Type 2 Diabetes and Periodontitis: A Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2021, 18, 3018. [Google Scholar] [CrossRef] [PubMed]
- Rapone, B.; Ferrara, E.; Corsalini, M.; Converti, I.; Grassi, F.R.; Santacroce, L.; Topi, S.; Gnoni, A.; Scacco, S.; Scarano, A.; et al. The Effect of Gaseous Ozone Therapy in Conjunction with Periodontal Treatment on Glycated Hemoglobin Level in Subjects with Type 2 Diabetes Mellitus: An Unmasked Randomized Controlled Trial. Int. J. Environ. Res. Public. Health 2020, 17, 5467. [Google Scholar] [CrossRef] [PubMed]
- Faggion, C.M., Jr.; Cullinan, M.P.; Atieh, M. An overview of systematic reviews on the effectiveness of periodontal treatment to improve glycaemic control. J. Periodontal. Res. 2016, 51, 716–725. [Google Scholar] [CrossRef] [PubMed]
- Teshome, A.; Yitayeh, A. The effect of periodontal therapy on glycemic control and fasting plasma glucose level in type 2 diabetic patients: Systematic review and meta-analysis. BMC Oral. Health 2016, 17, 31. [Google Scholar] [CrossRef]
- Stohr, J.; Barbaresko, J.; Neuenschwander, M.; Schlesinger, S. Bidirectional association between periodontal disease and diabetes mellitus: A systematic review and meta-analysis of cohort studies. Sci. Rep. 2021, 11, 13686. [Google Scholar] [CrossRef]
- Nguyen, A.T.M.; Akhter, R.; Garde, S.; Scott, C.; Twigg, S.M.; Colagiuri, S.; Ajwani, S.; Eberhard, J. The association of periodontal disease with the complications of diabetes mellitus. A Syst. Rev. Diabetes Res. Clin. Pr. Pract. 2020, 165, 108244. [Google Scholar] [CrossRef]
- Kocher, T.; König, J.; Borgnakke, W.S.; Pink, C.; Meisel, P. Periodontal complications of hyperglycemia/diabetes mellitus: Epidemiologic complexity and clinical challenge. Periodontology 2000 2018, 78, 59–97. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef]
- Wells, G.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses; Department of Epidemiology and Community Medicine, University of Ottawa: Ottawa, Canada, 2014; Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 3 August 2023).
- Elyasi, M.; Abreu, L.G.; Badri, P.; Saltaji, H.; Flores-Mir, C.; Amin, M. Impact of Sense of Coherence on Oral Health Behaviors: A Systematic Review. PLoS ONE 2015, 10, e0133918. [Google Scholar] [CrossRef]
- Ferreira, M.C.; Dias-Pereira, A.C.; Branco-de-Almeida, L.S.; Martins, C.C.; Paiva, S.M. Impact of periodontal disease on quality of life: A systematic review. J. Periodontal. Res. 2017, 52, 651–665. [Google Scholar] [CrossRef]
- Chambrone, L.; Foz, A.M.; Guglielmetti, M.R.; Pannuti, C.M.; Artese, H.P.; Feres, M.; Romito, G.A. Periodontitis and chronic kidney disease: A systematic review of the association of diseases and the effect of periodontal treatment on estimated glomerular filtration rate. J. Clin. Periodontol. 2013, 40, 443–456. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Begg, C.B.; Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, D.; Topcu, A.O.; Akcay, E.U.; Altındis, M.; Gursoy, U.K. Salivary human beta-defensins and cathelicidin levels in relation to periodontitis and type 2 diabetes mellitus. Acta Odontol. Scand. 2020, 78, 327–331. [Google Scholar] [CrossRef]
- Matic Petrovic, S.; Radunovic, M.; Barac, M.; Kuzmanovic Pficer, J.; Pavlica, D.; Arsic Arsenijevic, V.; Pucar, A. Subgingival areas as potential reservoirs of different Candida spp in type 2 diabetes patients and healthy subjects. PLoS ONE 2019, 14, e0210527. [Google Scholar] [CrossRef]
- Han, K.; Park, J.-B. Clinical implication of fasting glucose and systolic/diastolic blood p ressure on the prevalence of periodontitis in non-diabetic and non-hyp ertensive adults using nationally representative data. Exp. Ther. Med. 2018, 16, 671–678. [Google Scholar] [CrossRef]
- Hong, M.; Kim, H.Y.; Seok, H.; Yeo, C.D.; Kim, Y.S.; Song, J.Y.; Lee, Y.B.; Lee, D.H.; Lee, J.I.; Lee, T.K.; et al. Prevalence and risk factors of periodontitis among adults with or without diabetes mellitus. Korean J. Intern. Med. 2016, 31, 910–919. [Google Scholar] [CrossRef]
- Lappin, D.F.; Robertson, D.; Hodge, P.; Treagus, D.; Awang, R.A.; Ramage, G.; Nile, C.J. The Influence of Glycated Hemoglobin on the Cross Susceptibility Between Type 1 Diabetes Mellitus and Periodontal Disease. J. Periodontol. 2015, 86, 1249–1259. [Google Scholar] [CrossRef]
- Javed, F.; Ahmed, H.B.; Saeed, A.; Mehmood, A.; Bain, C. Whole salivary interleukin-6 and matrix metalloproteinase-8 levels in patients with chronic periodontitis with and without prediabetes. J. Periodontol. 2014, 85, e130–e135. [Google Scholar] [CrossRef]
- Wolff, R.E.; Wolff, L.F.; Michalowicz, B.S. A pilot study of glycosylated hemoglobin levels in periodontitis cases and healthy controls. J. Periodontol. 2009, 80, 1057–1061. [Google Scholar] [CrossRef]
- Perayil, J.; Suresh, N.; Fenol, A.; Vyloppillil, R.; Bhaskar, A.; Menon, S. Comparison of glycated hemoglobin levels in individuals without diabetes and with and without periodontitis before and after non-surgical periodontal therapy. J. Periodontol. 2014, 85, 1658–1666. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, A.A.; Kolte, A.P.; Kolte, R.A.; Chari, S.; Gupta, M.; Pakhmode, R. Evaluation and comparison of serum vitamin D and calcium levels in periodontally healthy, chronic gingivitis and chronic periodontitis in patients with and without diabetes mellitus—a cross-sectional study. Acta Odontol. Scand. 2019, 77, 592–599. [Google Scholar] [CrossRef] [PubMed]
- Vaghani, H.; Mehta, R.; Desai, K.; Duseja, S.; Mehta, T. Effect of Non-surgical Periodontal Therapy on Glycosylated Haemoglobin Levels in Diabetics and Non-diabetic Healthy Controls with Periodontitis. Adv. Hum. Human. Biol. May Aug. 2016, 6, 95–98. [Google Scholar] [CrossRef]
- Muthu, J.; Muthanandam, S.; Mahendra, J.; Namasivayam, A.; John, L.; Logaranjini, A. Effect of Nonsurgical Periodontal Therapy on the Glycaemic Control of Nondiabetic Periodontitis Patients: A Clinical Biochemical Study. Oral. Health Prev. Dent. 2015, 13, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Acharya, A.B.; Thakur, S.; Muddapur, M.V. Effect of scaling and root planing on serum interleukin-10 levels and glycemic control in chronic periodontitis and type 2 diabetes mellitus. J. Ind. Soc. Periodontol. 2015, 19, 188–193. [Google Scholar] [CrossRef]
- Saxena, R.M.; Deepika, P.C. Comparison of glycosylated hemoglobin levels in periodontitis patients and healthy controls: A pilot study in Indian population. Ind. J. Dent. Res. Off. Publ. Ind. Soc. Dent. Res. 2012, 23, 368–372. [Google Scholar] [CrossRef] [PubMed]
- Doğan, Ş.B.; Ballı, U.; Dede, F.; Sertoğlu, E.; Tazegül, K. Chemerin as a Novel Crevicular Fluid Marker of Patients With Periodontitis and Type 2 Diabetes Mellitus. J. Periodontol. 2016, 87, 923–933. [Google Scholar] [CrossRef] [PubMed]
- Bozkurt Doğan, Ş.; Öngöz Dede, F.; Ballı, U.; Sertoğlu, E. Levels of vaspin and omentin-1 in gingival crevicular fluid as potential markers of inflammation in patients with chronic periodontitis and type 2 diabetes mellitus. J. Oral. Sci. 2016, 58, 379–389. [Google Scholar] [CrossRef]
- George, A.K.; Narayan, V.; Kurian, N.; Joseph, A.E.; Anil, S. A pilot study on glycemia and insulin resistance in patients with severe periodontitis. J. Ind. Soc. Periodontol. 2021, 25, 393–398. [Google Scholar] [CrossRef]
- Zainab, A.; Ashish, N.; Ragnath, V. Salivary Levels of Antimicrobial Peptides in Chronic Periodontitis Patients with Type 2 Diabetes. J. Int. Acad. Periodontol. 2019, 21, 36–44. [Google Scholar]
- Acharya, A.B.; Thakur, S.; Muddapur, M.V.; Kulkarni, R.D. Systemic Cytokines in Type 2 Diabetes Mellitus and Chronic Periodontitis. Curr. Diabetes Rev. 2018, 14, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Grdović, N.; Rajić, J.; Petrović, S.M.; Dinić, S.; Uskoković, A.; Mihailović, M.; Jovanović, J.A.; Tolić, A.; Pucar, A.; Milašin, J.; et al. Association of CXCL12 gene promoter methylation with periodontitis in patients with diabetes mellitus type 2. Arch. Oral. Biol. 2016, 72, 124–133. [Google Scholar] [CrossRef] [PubMed]
- Srinivasa, T.S.; Agrawal, P.; Goyal, P.; Farista, S.; Sowmya, N.K.; Deonani, S. Comparative clinical evaluation of glycosylated haemoglobin level in healthy and chronic periodontitis patients: A chairside diagnostic method. Ind. J. Dent. Res. Off. Publ. Ind. Soc. Dent. Res. 2015, 26, 504–507. [Google Scholar] [CrossRef]
- Matić Petrović, S.; Cimbaljević, M.; Radunović, M.; Kuzmanović Pfićer, J.; Jotić, A.; Pucar, A. Detection and sampling methods for isolation of Candida spp. from oral cavities in diabetics and non-diabetics. Braz. Oral. Res. 2015, 29. [Google Scholar] [CrossRef] [PubMed]
- Gokhale, N.H.; Acharya, A.B.; Patil, V.S.; Trivedi, D.J.; Setty, S.; Thakur, S.L. Resistin levels in gingival crevicular fluid of patients with chronic periodontitis and type 2 diabetes mellitus. J. Periodontol. 2014, 85, 610–617. [Google Scholar] [CrossRef]
- Zizzi, A.; Tirabassi, G.; Aspriello, S.D.; Piemontese, M.; Rubini, C.; Lucarini, G. Gingival advanced glycation end-products in diabetes mellitus-associated chronic periodontitis: An immunohistochemical study. J. Periodontal. Res. 2013, 48, 293–301. [Google Scholar] [CrossRef]
- Gd, G.S.G.; Sudhakar, U.; Raghavan, A.; Narayan, K.V. Effects of Non-surgical Periodontal Therapy on Saliva and Gingival Crevicular Fluid Levels of Chemerin in Periodontitis Subjects with and without Type 2 Diabetes Mellitus. Cureus 2023, 15, e33388. [Google Scholar] [CrossRef]
- Mahendra, J.; Palathingal, P.; Mahendra, L.; Alzahrani, K.J.; Banjer, H.J.; Alsharif, K.F.; Halawani, I.F.; Muralidharan, J.; Annamalai, P.T.; Verma, S.S.; et al. Impact of Red Complex Bacteria and TNF-α Levels on the Diabetic and Renal Status of Chronic Kidney Disease Patients in the Presence and Absence of Periodontitis. Biology 2022, 11, 451. [Google Scholar] [CrossRef]
- Akram, Z.; Alqahtani, F.; Alqahtani, M.; Al-Kheraif, A.A.; Javed, F. Levels of advanced glycation end products in gingival crevicular fluid of chronic periodontitis patients with and without type-2 diabetes mellitus. J. Periodontol. 2020, 91, 396–402. [Google Scholar] [CrossRef]
- Altıngöz, S.M.; Kurgan, Ş.; Önder, C.; Serdar, M.A.; Ünlütürk, U.; Uyanık, M.; Başkal, N.; Tatakis, D.N.; Günhan, M. Salivary and serum oxidative stress biomarkers and advanced glycation end products in periodontitis patients with or without diabetes: A cross-sectional study. J. Periodontol. 2020, 92, 1274–1285. [Google Scholar] [CrossRef]
- Suresh, R.; Jayachandran, P.; Fenol, A.; Biswas, R.; Krishnan, S.; Kumar, K.A.; Divakar, D.D.; Vellappally, S. Effect of Non-Surgical Periodontal Therapy on the Serum Sialic Acid Levels in Diabetic Patients with Periodontitis. Acta Med. 2019, 62, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Mishra, V.; Shettar, L.; Bajaj, M.; Math, A.S.; Thakur, S.L. Interlinking Periodontitis and Type 2 Diabetes Mellitus by Assessment of Crevicular Visfatin Levels in Health and in Disease before and after Initial Periodontal Therapy. J. Clin. Diagn. Res. 2016, 10, ZC67–ZC71. [Google Scholar] [CrossRef] [PubMed]
- Corbi, S.C.; Bastos, A.S.; Orrico, S.R.; Secolin, R.; Dos Santos, R.A.; Takahashi, C.S.; Scarel-Caminaga, R.M. Elevated micronucleus frequency in patients with type 2 diabetes, dyslipidemia and periodontitis. Mutagenesis 2014, 29, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Rajan, P.; Nera, M.; Pavalura, A.K.; Medandrao, N.; Kumar, S.C. Comparison of glycosylated hemoglobin (HbA1C) levels in patients with chronic periodontitis and healthy controls. Dent. Res. J. 2013, 10, 389–393. [Google Scholar]
- Rao Deepika, P.C.; Saxena, R.M. Comparison of glycosylated hemoglobin levels in severe periodontitis patients and healthy controls: A study in an Indian population. Quintessence Int. 2013, 44, 319–325. [Google Scholar] [CrossRef]
- Pan, Z.; Guzeldemir, E.; Toygar, H.U.; Bal, N.; Bulut, S. Nitric oxide synthase in gingival tissues of patients with chronic periodontitis and with and without diabetes. J. Periodontol. 2010, 81, 109–120. [Google Scholar] [CrossRef]
- Akalin, F.A.; Işiksal, E.; Baltacioğlu, E.; Renda, N.; Karabulut, E. Superoxide dismutase activity in gingiva in type-2 diabetes mellitus patients with chronic periodontitis. Arch. Oral. Biol. 2008, 53, 44–52. [Google Scholar] [CrossRef]
- Needleman, I.; Warnakulasuriya, S.; Sutherland, G.; Bornstein, M.M.; Casals, E.; Dietrich, T.; Suvan, J. Evaluation of tobacco use cessation (TUC) counselling in the dental office. Oral. Health Prev. Dent. 2006, 4, 27–47. [Google Scholar]
- Sackett, D.L. Rules of evidence and clinical recommendations for the management of patients. Can. J. Cardiol. 1993, 9, 487–489. [Google Scholar]
- Selvin, E.; Crainiceanu, C.M.; Brancati, F.L.; Coresh, J. Short-term variability in measures of glycemia and implications for th e classification of diabetes. Arch. Intern. Med. 2007, 167, 1545–1551. [Google Scholar] [CrossRef]
- Gillett, M.J. International Expert Committee report on the role of the A1c assay in the diagnosis of diabetes: Diabetes Care 2009, 32, 1327–1334. Clin. Biochem. Rev. 2009, 30, 197–200. [Google Scholar]
- Little, R.R.; Rohlfing, C.L.; Sacks, D.B. Status of hemoglobin A1c measurement and goals for improvement: From chaos to order for improving diabetes care. Clin. Chem. 2011, 57, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Association, A.D. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care 2020, 43, S14–S31. [Google Scholar] [CrossRef] [PubMed]
- Schulz, K.F.; Grimes, D.A. Case-control studies: Research in reverse. Lancet 2002, 359, 431–434. [Google Scholar] [CrossRef] [PubMed]
- Zelig, R.; Samavat, H.; Duda, P.; Singer, S.R.; Feldman, C.; LaSalle, P.; Muhammad, E.; Touger-Decker, R. Screening for diabetes risk using the diabetes risk test and point-of-care hemoglobin A1C values in adults seen in a dental clinic. Quintessence Int. 2023, 54, 500–509. [Google Scholar] [CrossRef]

| First Author (Publication Year) | Study Design * | Sample Size | Demographic Data of Subjects | Description of Subjects without DM | Definition of Periodontitis | Glycemic State |
|---|---|---|---|---|---|---|
| Gomathi GD (2023) [58] | Case–control study, convenience sample | Stage II periodontitis group and periodontal health group: 15 vs. 15 | Non-tobacco chewers and non-smokers | The ADA criteria. | AAP/EFP 2017 classification. | In periodontitis group and periodontal health group, HbA1c (%, mean ± SD): 5.54 ± 0.29 vs. 5.3 ± 0.26, p > 0.05; FPG (mg/dL, mean ± SD): 92.3 ± 5.76 vs. 92.0 ± 4.85, p > 0.05; by one-way ANOVA. |
| Mahendra J (2022) [59] | Case–control study, convenience sample | Periodontitis group and control group: 30 vs. 30 | Patients with periodontitis mean aged 54.03 ± 9.10 years with 6/30 (20.6%) males, healthy controls mean aged 37.63 ± 10.26 years with 7/30 (22.2%) males | With systemic health and without systemic conditions. | AAP/EFP 2017 classification. Periodontitis: interdental CAL was detectable at >2 nonadjacent teeth with CAL ≥ 3 mm and PD > 3 mm present in >2 teeth. | In periodontitis group and control group, HbA1c (%, mean ± SD): 5.97 ± 1.16 vs. 5.28 ± 0.22; FBS (mg/dL, mean ± SD): 111.17 ± 48.08 vs. 89.43 ± 9.72; by ANOVA. The difference of periodontitis group with control group was not compared. |
| George AK (2021) [50] | Case–control study, convenience sample | Severe periodontitis group and control group: 37 vs. 37 | Patients with periodontitis mean aged 43.35 ± 7.70 years with 20/37 (54.1%) males, healthy controls mean aged 40.70 ± 6.19 years with 13/37 (35.1%) males. Non-smokers; non-obese (BMI < 30 kg/m2) | FBS < 126 mg/dL, HbA1c < 6.5%. | CDC/AAP 2013 case definition. Severe periodontitis: ≥2 interproximal sites with CAL ≥ 6 mm (not on the same tooth) and ≥1 interproximal site with PD ≥ 5 mm. | In periodontitis group and control group, HbA1c (%, mean ± SD): 5.87 ± 1.46 vs. 5.29 ± 0.20, p = 0.021; FBS (mg/dL, mean ± SD): 96.81 ± 23.59 vs. 83.27 ± 8.28, p = 0.002; by unpaired t-test. |
| Akram Z (2020) [60] | Case–control study, convenience sample | Periodontitis group and periodontal health group: 31 vs. 31 | Patients with periodontitis mean aged 51.5 (42–54) years with 25/31 (80.6%) males, healthy controls mean aged 50.7 (46–58) years with 27/31 (87.1%) males. Non-smokers (including electronic cigarettes) | Self-reported systemically healthy individuals. | AAP 1999. Periodontitis: PI, BOP, PD ≥ 4 mm, CAL ≥ 3 mm and marginal BL ≥ 3 mm in at least 30% of sites. Periodontal health group: subjects without chronic periodontitis. | In periodontitis group and periodontal health group, mean (range) of HbA1c (%): 4.7 (4.2–5.1) vs. 4.2 (4.1–4.5), p > 0.05; FPG (mg/dL, mean ± SD): 97.2 ± 11.7 vs. 94.9 ± 6.7, p > 0.05; by one-way ANOVA and Bonferroni post hoc adjustment tests. |
| Altingoz SM (2020) [61] | Case–control study, convenience sample | Stage III periodontitis group and periodontal health group: 26 vs. 28 | Patients with periodontitis mean aged 46.1 ± 5.3 years with 8/26 (30.8%) males, healthy controls mean aged 44.8 ± 11.5 years (in the text) and 44.8 ± 6.5 years (in Table 1) with 10/28 (35.7%) males | No definition; for reference, Type 2 DM: diagnosed by physicians for at least the past 5 years and 6.5% ≤ HbA1c < 12%. | AAP/EFP 2017 classification. Periodontitis: ≥ 8 sites with PD ≥ 6 mm, ≥4 sites with CAL ≥ 5 mm, distributed in at least 2 different quadrants. Periodontal health group: negative periodontal disease history, PD ≤ 3 mm and CAL ≤ 1 mm, without clinical signs of gingival inflammation and with good oral hygiene. | In periodontitis group and periodontal health group, HbA1c (%, mean ± SD): 4.8 ± 0.3 vs. 4.7 ± 0.2, p > 0.05; FPG (mg/dL, mean ± SD): 97.2 ± 11.7 vs. 94.9 ± 6.7, p > 0.05, by the ANOVA test with a Bonferroni correction. |
| Yilmaz D (2020) [35] | Cross-sectional study, convenience sample | Periodontitis group and periodontal health group: 29 vs. 28 | Patients with periodontitis mean aged 45.4 ± 12.9 years and 84.7% were males, healthy controls mean aged 43.9 ± 14.4 years and 82.7% of 28 healthy subjects were males. Non-smokers | Metabolic health: FPG <126 mg/dL (7.0 mmol/L, fasting is defined as no caloric intake for at least 8 h) and HbA1c <6.5% (48 mmol/mol) based on ADA 2018 guideline. | AAP/EFP 2017 classification. Periodontitis: BOP ≥ 10% and interdental CAL was detectable at ≥2 non-adjacent teeth with PD ≥ 4 mm. Periodontal health: BOP ˂ 10% of the surfaces and no sites with PD > 3 mm besides no CAL or BL. | In periodontitis group and periodontal health group, HbA1c (%, mean ± SD): 5.41 ± 0.54 vs. 5.56 ± 0.45; FPG (mg/dL, mean ± SD): 97.8 ± 12.1 vs. 95.6 ± 10.1. The difference between two groups was not compared. |
| Agrawal AA (2019) [43] | Case–control study, convenience sample | Chronic periodontitis group, chronic gingivitis group, and periodontal health group: 20 | Patients with periodontitis mean aged 39.29 years, with gingivitis mean aged 41.45 years, with healthy periodontal status mean aged 44.65 years. Non-tobacco chewers and non-smokers | HbA1c levels < 6.5%, RBS levels ≤ 200 mg/dL. | AAP 1999. Periodontitis: GI ≥ 1, PI ≥ 1, PD ≥ 5 mm and CAL ≥ 5 mm. Gingivitis: GI ≥ 1, PI ≥ 1, PD ≤ 3 mm. Periodontal health: GI < 1, PI < 1, PD ≤ 3 mm. | HbA1c (%, mean ± SD) in periodontitis group was 6.60 ± 1.66; in gingivitis group was 4.67 ± 0.37; in periodontal health group was 4.63 ± 0.36, p < 0.05. RBS (mg/dL, mean ± SD) in periodontitis group was 169.76 ± 41.59; in gingivitis group was 180.35 ± 22.27; in periodontal health group was 97.65 ± 47.47, p > 0.05; by Student’s unpaired t-test. |
| Matic Petrovic S (2019) [36] | Cross-sectional study, convenience sample | Chronic periodontitis group and periodontal health group: 42 vs. 36 | Patients with periodontitis mean aged 48 ± 11 years with 17/42 (40.5%) males, healthy controls mean aged 43 ± 4 years with 15/36 (41.7%) males | Free of systemic diseases. | Periodontitis: CAL ≥ 1 mm and PD > 3 mm at > 30% of sites. periodontal health group: PD < 3 mm, CAL = 0 mm, BOP < 25%. | In periodontitis group and periodontal health group, HbA1c (%, mean ± SD): 4.82 ± 0.561 vs. 4.80 ± 0.607, p > 0.05; FPG (mmol/L, mean ± SD): 4.97 ± 0.578 vs. 4.64 ± 0.534, p < 0.05; by Mann–Whitney U test. |
| Suresh R (2019) [62] | Case–control study, convenience sample | Chronic moderate periodontitis group and periodontal health group: 20 vs. 20 | Patients with periodontitis mean aged 44 ± 7.20 years with 16/20 (80.0%) males, healthy controls mean aged 48 ± 7.13 years with 10/20 (50.0%) males. Non-smokers | Without non-insulin dependent DM, RBS levels < 140 mg/dL. | AAP 1999. Periodontitis: CAL 3–4 mm, OHI-S score 1.3 to 3, GI score 1.1 to 2, PD ≥ 3 to ≤5 mm, CAL ≥ 3 to ≤4 mm in 5 or more teeth. Periodontal health group: OHI-S score 0.8 to 1, GI score 0.1 to 1, PD ≤ 3 mm and with no CAL. | In periodontitis group and periodontal health group, HbA1c (%, mean ± SD): 5.74 ± 0.19 vs. 5.67 ± 0.27, p > 0.05, by ANOVA. |
| Zainab AJAA (2019) [51] | Case–control study, convenience sample, with equal number of males and females | Chronic periodontitis group and periodontal health group: 20 vs. 20 | Patients with periodontitis mean aged 43.5 ± 4.81 years with 10/20 (50.0%) males, healthy controls mean aged 40.05 ± 5.56 years with 10/20 (50.0%) males. Never-smokers; non-obese | Without DM or any other systemic disease. | AAP 1999. Periodontitis: ≥5 mm of CAL present at more than 30% of the sites and BL radiographically. Periodontal health group: PD ≤ 3 mm, no CAL, absence of BOP, no radiographic BL. | In periodontitis group and periodontal health group, HbA1c (%, mean ± SD): 4.85 ± 0.39 vs. 4.85 ± 0.29, p > 0.05; FPG (mg/dL, mean ± SD): 107.00 ± 9.28 vs. 106.35 ± 8.22, p > 0.05, by ANOVA. |
| Acharya AB (2018) [52] | Case–control study, convenience sample | Chronic periodontitis group and periodontal health group: 20 vs. 20 | Patients with periodontitis mean aged 42.09 ± 6.45 years with 12/20 (60.0%) males, healthy controls mean aged 42.80 ± 4.81 years with 10/20 (50.0%) males. Non-tobacco users; BMI < 30 kg/m2 and lipid profile in normal limits | Not previously diagnosed with DM. | Periodontitis: generalized BOP, PD of ≥ 5 mm, CAL ≥ 2 mm supplemented by radiographic confirmation of alveolar BL. | In periodontitis group and periodontal health group, HbA1c (%, mean ± SD): 5.72 ± 0.33 vs. 4.87 ± 0.42, p > 0.05; RBS (mg/dL, mean ± SD): 116.80 ± 15.98 vs. 105.85 ± 11.398, p > 0.05; by Wilcoxon sign–rank tests. |
| Han K (2018) [37] | Cross-sectional study, nationally representative community sample from multi-centers | Periodontitis group and periodontal health group: 1968 vs. 6373 | Patients with periodontitis mean aged 49.29 ± 0.37 years and 56.24% were males, healthy controls mean aged 37.94 ± 0.23 years and 44.65% were males | Without diagnosis of DM. | Periodontitis: CPI ≥ 3. | In periodontitis group and periodontal health group, HbA1c (%, mean ± SD): 5.59 ± 0.01 vs. 5.46 ± 0.01, p < 0.05; FPG (mg/dL, mean ± SD): 94.88 ± 0.24 vs. 91.66 ± 0.15, p < 0.05; by independent t-test. Multivariate logistic regression: adjusted age, gender, smoking, drinking, education, income, and BMI, HbA1c was not significantly different in periodontitis group and periodontal health group. |
| Dogan SB (2016a) [49] | Case–control study, convenience sample | Chronic periodontitis group and periodontal health group: 15 vs. 15 | Patients with periodontitis median aged 48.00 years with 8/15 (53.3%) males, healthy controls median aged 52.00 years with 7/15 (46.7%) males. Never-smokers; BMI ≤ 24.9 kg/m2 | HbA1c levels < 6.5%. | AAP 1999. Periodontitis: Radiographic signs of BL and CAL, at least 6 teeth with a PD ≥ 5 mm. These teeth showed BOP across a minimum of 2 separate quadrants, and had GI > 1. Periodontal health group: PD ≤ 3 mm, GI = 0, and no indication of CAL or radiographic evidence of alveolar BL (i.e., the gap between the CEJ and bone crest was <3 mm at > 95% of the proximal tooth sites). | In periodontitis group and periodontal health group, HbA1c (%, median): 5.30 vs. 5.10, p > 0.05; by Kruskal–Wallis nonparametric test. |
| Dogan SB (2016b) [48] | Case–control study, convenience sample | Chronic periodontitis group and periodontal health group: 20 vs. 20 | Patients with periodontitis median aged 49.50 years with 10/20 (50.0%) males, healthy controls mean aged 50.50 years with 11/20 (55.0%) males. Never-smokers; BMI ≤ 24.9 kg/m2 | HbA1c <6% and FPG < 100 mg/dL. | AAP 1999. Periodontitis: At least 6 teeth with CAL and a PD ≥ 5 mm. positive BOP within multiple regions. BL affected >30% of existing teeth on clinical and radiographic examination. GI ≥ 2. Periodontal health group: PD ≤ 3 mm, GI = 0, and no indication of CAL or radiographic evidence of alveolar BL (i.e., the gap between the CEJ and bone crest was <3 mm at >95% of the proximal tooth sites). | In periodontitis group and periodontal health group, HbA1c (%, median): 5.10 vs.5.00, p > 0.05; FPG (mg/dL, median): 87.00 vs. 87.50, p > 0.05; by Kruskal–Wallis non-parametric test. |
| Grdovic N (2016) [53] | Case–control study, convenience sample | Chronic periodontitis group and periodontal health group: 29 vs. 21 | Patients with periodontitis mean aged 48.17 ± 13.48 years with 16/29 (55.2%) males, healthy controls mean aged 33.43 ± 5.28 years with 8/21 (38.1%) males. BMI 19–30 kg/m2 | Normal parameters on OGTT and HbA1c < 6.5%. | AAP 1999. Periodontitis: CAL > 1 mm and PD > 3 mm at least at three sites in two different quadrants. Periodontal health group: PD < 3 mm, CAL = 0 mm on all examined teeth. | In periodontitis group and periodontal health group, HbA1c (%, mean ± SD): 4.75 ± 0.47 vs. 4.69 ± 0.59, p > 0.05; Glucose (mmol/L, mean ± SD): 4.96 ± 0.59 vs. 4.65 ± 0.43, p > 0.05; by one-way ANOVA followed by Fisher’s LSD test. |
| Hong M (2016) [38] | Cross-sectional study, nationally representative community sample from multi-centers | Periodontitis group and non-periodontitis group: 1005 vs. 2855 | Patients with periodontitis mean aged 53.5 ± 0.6 years and 60.9% were males, without periodontitis mean aged 46.9 ± 0.3 years and 45.6% were males | FPG < 126 mg/dL, not self-reported diagnosed with DM and not current use of oral hypoglycemic agents and/or insulin. | Periodontitis: CPI ≥ 3. | In periodontitis group and non-periodontitis group, HbA1c (%, mean ± SD): 5.6 ± 0.02 vs. 5.5 ± 0.0, p < 0.05; by one-way ANOVA. |
| Mishra V (2016) [63] | Case–control study, convenience sample | Chronic periodontitis group and periodontal health group: 14 vs. 14 | Patients with periodontitis mean aged 41.71 ± 8.06 years with 8/14 (57.14%) males, healthy controls mean aged 32.43 ± 2.03 years with 3/14 (21.43%) males. Non-smokers | No signs and symptoms of systemic disease. | Periodontitis: AAP 1999. Periodontal health: clinically healthy periodontium. | In periodontitis group and control group, HbA1c (%, mean ± SD): 4.71 ± 0.59 vs. 4.78 ± 0.52, p > 0.05; by one-way ANOVA and Tukey’s multiple post hoc procedures. |
| Vaghani H (2016) [44] | Case–control study, convenience sample | Periodontitis group and non-periodontitis group: 30 vs. 30 | 35–65 years; non-smokers | Not diagnosed with DM, FBS < 110 mg/dL and without clinical history of DM. | Periodontitis: PD ≥ 5 mm and CAL > 3 mm in five or more teeth. Non-periodontitis group: no BOP, no PD > 3 mm and no CAL. | In periodontitis group and control group, HbA1c (%, mean ± SD): 6.17 ± 0.22 vs. 5.62 ± 0.24, the difference was statistically significant; by ANOVA test. |
| Acharya AB (2015) [46] | Case–control study, convenience sample | Moderate-severe chronic periodontitis group and periodontal health group: 15 vs. 15 | 35–55 years; non-smokers; BMI < 30 kg/m2 | Systemically healthy subjects. | AAP 1999. Periodontitis: at least 4 teeth with PD ≥5 mm, CAL and alveolar BL as evidenced in prescribed radiographs. | In periodontitis group and periodontal health group, HbA1c (%, mean ± SD): 5.78 ± 0.28 vs. 4.86 ± 0.48, p = 0.001; RBS (mg/dL, mean ± SD): 103.73 ± 12.47 vs. 114.86 ± 17.76; by one-way ANOVA and Tukey’s multiple post hoc procedures. |
| Lappin DF (2015) [39] | Cross-sectional study, convenience sample | Periodontitis group and healthy volunteers: 23 vs. 19 | Patients with periodontitis mean aged 40 ± 11 years and 46% were males, healthy volunteers mean aged 33 ± 8 years and 63% were males. No history of smoking within the past five years | Healthy volunteers. | Periodontitis: at least two sites with PD and CAL ≥ 5 mm. | In periodontitis group and healthy volunteers, HbA1c (mmol/mol, mean ± SD): 33.3 ± 1.1 vs. 32.2 ± 1.1; blood glucose (mmol/L, mean ± SD): 5.7 ± 0.1 vs.5.6 ± 0.1. The difference between two groups was not compared. |
| Matic Petrovic S (2015) [55] | Case–control study, convenience sample | Chronic periodontitis group and periodontal health group: 30 vs. 35 | Patients with periodontitis mean aged 47.07 ± 10.869 years with 14/30 (40.0%) males, healthy controls mean aged 43.57 ± 3.389 years with 14/35 (28.6%) males | Normal parameters on OGTT and HbA1c < 6.5%. | AAP 1999. Periodontitis: CAL > 1 mm and PD > 3 mm at least at three sites in two quadrants. Control group: PD < 3 mm and CAL = 0 mm. | In periodontitis group and periodontal health group, HbA1c (%, mean ± SD): 4.86 ± 0.635 vs. 4.81 ± 0.623; FPG (mg/dL, mean ± SD): 4.73 ± 0.624 vs. 4.65 ± 0.539. Not reported median. There was no statistical significance between groups using non-parametric test. |
| Muthu J (2015) [45] | Case–control study, convenience sample | Periodontitis group and control group: 130 vs. 90 | 96 women and 124 men aged 35–50 years; non-smokers | Nondiabetic patients. | AAP 1999. Periodontitis: ≥ 5 teeth with PD ≥ 5 mm and CAL > 3 mm or radiographic BL, a mSBI ≥ 2 in at least 15% of sites. Control group: No PD ≥ 4 mm, BOP ≤ 15% of tooth sites. | In periodontitis group and control group, HbA1c (%, mean ± SD): 3.40 ± 0.58 vs. 2.23 ± 0.47, p < 0.001; by Student’s independent t-test. |
| Srinivasa TS (2015) [54] | Case–control study, convenience sample | Chronic periodontitis group and control group: 20 vs. 20 | Patients with periodontitis mean aged 38.9 ± 13.4 years with 12/20 (60.0%) males, healthy controls mean aged 40.1 ± 14.4 years with 10/20 (50.0%) males | No severe systemic diseases. | AAP 1999. Periodontitis: at least five teeth with PD ≥ 5 mm, BOP and CAL > 1 mm on > 5 teeth or radiographic BL. Control group: PD ≤ 4 mm, BOP ≤ 15% and no CAL. | In periodontitis group and control group, HbA1c (%, mean ± SD): 5.66 ± 0.35 vs. 5.17 ± 0.3, p = 0.003; by t-test. |
| Corbi SCT (2014) [64] | Case–control study, convenience sample | Chronic periodontitis group and control group: 30 vs. 30 | Patients with periodontitis mean aged 45.9 ± 5.9 years with 19/30 (63.3%) males, healthy controls mean aged 39.3 ± 3.6 years with 18/30 (60.0%) males. Never-smokers | Systemically healthy individuals. | AAP 1999. Periodontitis: PD ≥ 6 mm and CAL ≥ 4 mm in ≥4 non-adjacent teeth. | In periodontitis group and control group, HbA1c (%, mean ± SD): 5.1 ± 0.6 vs. 5.4 ± 0.21; fasting glucose (mg/dL, mean ± SD): 90.8 ± 7.3 vs. 85.9 ± 6.5. Not reported median. There was no statistical siginificance between groups using Kruskal–Wallis test and Dunn’s post hoc test. |
| Gokhale NH (2014) [56] | Case–control study, convenience sample | Chronic periodontitis group and control group: 15 vs. 15 | Patients with periodontitis consisted of 3/15 (20.0%) males, healthy controls consisted of 7/15 (46.7%) males. Non-smokers | HbA1c levels <6.5%, and RBS levels <200 mg/dL. | Periodontitis: GI > 1, minimum of three teeth with PD ≥ 5 mm that were positive for BOP and radiographic evidence of BL. Control group: GI ≤ 1, no teeth with PD ≥ 5 mm. | In periodontitis group and control group, HbA1c (%, mean ± SD): 4.75 ± 0.59 vs. 4.75 ± 0.51, p > 0.05; RBS (mg/dL, mean ± SD): 127.20 ± 17.37 vs. 126.33 ± 20.36, p > 0.05; by one-way ANOVA and Tukey multiple post hoc procedures. |
| Javed F (2014) [40] | Case–control study, convenience sample | Chronic periodontitis group and control group: 30 vs. 28 | Patients with periodontitis mean aged 42.2 ± 1.8 years, healthy controls mean aged 42.7 ± 3.2 years. Only males included. Non-smokers | Self-reported systemically healthy individuals | AAP 1999. Periodontitis: CAL ≥ 3 mm, PD ≥ 5 mm, and marginal BL ≥ 3 mm in >30% of the sites. | In periodontitis group and control group, HbA1c (%, mean ± SD): 4.8 ± 0.5 vs. 4.3 ± 0.2, p > 0.05; FPG (mg/dL, mean ± SD): 80.1 ± 3.5 vs. 75.3 ± 2.2, p > 0.05; by one-way ANOVA. |
| Perayil J (2014) [42] | Case–control study, convenience sample | Calculated, periodontitis group and control group: 30 vs. 30 | Patients with periodontitis mean aged 45.24 ± 8.50 years with 16/30 (53.3%) males, healthy controls mean aged 40.77 ± 8.29 years with 10/30 (33.3%) males. Non-smokers | FBS levels <110 mg/dL. | AAP 1999. Periodontitis: PD ≥ 5 mm and CAL > 3 mm in ≥5 teeth. Control group: no BOP, no PD > 3 mm, no CAL. | In periodontitis group and control group, HbA1c (%, mean ± SD): 6.08 ± 0.23 vs. 5.38 ± 0.22, p = 0.001, by independent sample t-tests. |
| Rajan P (2013) [65] | Case–control study, convenience sample | Chronic periodontitis group and control group: 70 vs. 70 | Patients with periodontitis mean aged 45.33 ± 6.64 years with 27/70 (38.6%) males, healthy controls mean aged 43.43 ± 6.57 years with 30/70 (42.9%) males | Previously not diagnosed with DM. | Periodontitis: ≥10 teeth with PD ≥ 5 mm and ≥15% sites with BOP and CAL > 1 mm. Control group: PD <4 mm, BOP at <15% of teeth sites. | In periodontitis group and control group, HbA1c (%, mean ± SD): using kit, 5.51 ± 0.53 vs. 5.44 ± 0.27, p > 0.05; in lab, 5.50 ± 0.74 vs. 5.48 ± 0.29, p > 0.05; by t-test. |
| Rao Deepika PC (2013) [66] | Case–control study, convenience sample | Severe periodontitis group and control group: 28 (recruited 30 subjects) vs. 30 | Patients with periodontitis mean aged 48.82 ± 7.775 years with 19/28 (67.9%) males, healthy controls mean aged 45.93 ± 5.632 years with 12/30 (40.0%) males. Non-smokers | No medical history with DM. | AAP 1999. Severe periodontitis: >30% of the sites with CAL ≥ 5 mm and BOP. Control group: PD ≤ 4 mm, BOP at ≤15% of tooth sites, no CAL. | In periodontitis group and control group, HbA1c (%, median; min and max): 5.8; 5.1 and 6.0 vs. 5.6; 5.1 and 6.0, p > 0.05. Subgroup analysis according to BMI: normal-weight subjects: In periodontitis group and control group, HbA1c (%, mean ± SD): 5.68 ± 0.25 vs. 5.62 ± 0.27, p > 0.05; overweight subjects: In periodontitis group and control group, HbA1c (%, mean ± SD): 5.89 ± 0.12 vs. 5.65 ± 0.27, p = 0.016, by t-test. |
| Zizzi A (2013) [57] | Case–control study, convenience sample | Periodontitis (generalized, severe, chronic) group and control group: 16 vs. 16 | Patients with periodontitis mean aged 56.5 ± 1.32 years with 9/16 (56.3%) males, healthy controls mean aged 55 ± 1.76 years with 12/16 (75.0%) males. Non-smokers | HbA1c levels <6.1%, plasma glucose < 100 mg/dL. | AAP 1999. Periodontitis: >30% of sites with >5 mm of CAL. Control group: PD < 3 mm, GI = 0 and CAL < 2 mm. | Median (IQR) of HbA1c (%) in periodontitis group and control group: 5.3 (5.2–5.5) vs. 5 (4.9–5.2), p < 0.05; glycemia (mg/dL): 87.5 (78.7–92) vs. 82.5 (76.2–89), p > 0.05; by the Kruskal–Wallis test followed by the Mann–Whitney U-test. |
| Saxena RM (2012) [47] | Case–control study, convenience sample | Periodontitis group and control group: 18 vs. 18 | Non-smokers | Not diagnosed with DM. | AAP 1999. Periodontitis: ≥5 teeth with PD ≥ 5 mm, and >5 teeth with CAL > 1 mm or radiographic BL and BOP. Control group: PD ≤ 4 mm, BOP at ≤15% of tooth sites, and no CAL. | In periodontitis group and control group, HbA1c (%, mean ± SD): 6.0611 ± 0.0645 vs. 5.7944 ± 0.1830, p > 0.05; subgroup analysis according to BMI: normal-weight subjects: in periodontitis group and control group, HbA1c (%, mean): 6.08 vs. 5.78, p > 0.05; overweight subjects: in periodontitis group and control group, HbA1c (%, mean): 5.7 vs. 5.87, p > 0.05, by t-test. |
| Pan Z (2010) [67] | Case–control study, convenience sample | Chronic periodontitis group and control group: 20 vs. 20 | Patients with periodontitis mean aged 43.1 ± 8.9 years with 12/20 (60.0%) males, healthy controls mean aged 29.8 ± 9.2 years with 12/20 (60.0%) males. Non-smokers | Systemically healthy subjects. | AAP 1999. Periodontitis: ≥20 teeth with >30% of measured sites with CAL > 5 mm, BOP at >50% of the proximal sites and alveolar BL > 50% in at least two quadrants. Control group: PD < 3 mm with no CAL, no obvious clinical inflammation, and no BOP. | In periodontitis group and control group, HbA1c (%, mean ± SD): 4.9 ± 0.7 vs. 5.0 ± 0.6, p > 0.05. FPG (mg/dL, mean ± SD): 87.2 ± 7.9 vs. 87.8 ± 7.3, p > 0.05; by parametric tests. |
| Wolff RE (2009) [41] | Case–control study, convenience sample | Calculated; periodontitis group and control group: 59 vs. 53 | Patients with periodontitis mean aged 51.3 ± 14.8 years with 40/59 (67.8%) males, healthy controls mean aged 50.9 ± 16.3 years with 20/53 (37.7%) males | Not diagnosed with DM. | AAP 1999. Periodontitis: ≥5 teeth with PD ≥ 5 mm and BOP and CAL > 1 mm or radiographic BL. Control group: no PD > 4 mm, BOP at ≤5% of tooth sites, and no periodontal treatment within 6 months. | In periodontitis group and control group, HbA1c (%, mean ± SD): 5.66 ± 0.56 vs. 5.51 ± 0.44, p = 0.12,by t-test. After adjustments for age, gender, BMI, and current smoking, mean HbA1c was significantly higher in cases than controls (0.21%; 95% CI 0.01% to 0.41%; p = 0.046), by multivariate linear regression. |
| Akalin FA (2008) [68] | Case–control study, convenience sample | Chronic periodontitis group and control group: 17 vs. 17 | Patients with periodontitis mean aged 49.35 ± 9.07 years with 9/17 (52.9%) males, healthy controls mean aged 44.12 ± 9.54 years with 8/17 (47.1%) males. Never-smokers | Not having systemic disease and a history of DM in the family. | AAP 1999. Periodontitis: ≥30% periodontal BL and ≥3 teeth with ≥ 5 mm periodontal pockets. Control group: no gingival inflammation, no history of any periodontal disease, with PD of <3 mm, and had good oral hygiene. | In periodontitis group and control group, HbA1c (%, median): 5.4 vs. 5.2, p > 0.05; FPG (mg/dL, median): 82 vs. 82, p > 0.05; by Kruskal–Wallis test. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, D.; Sun, Y.; Li, X.; Wang, X.; Lu, L.; Li, C.; Pan, Y.; Wang, S. Association between Periodontitis and HbA1c Levels in Non-Diabetic Patients: A Systematic Review and Meta-Analysis. Healthcare 2023, 11, 2649. https://doi.org/10.3390/healthcare11192649
Zhao D, Sun Y, Li X, Wang X, Lu L, Li C, Pan Y, Wang S. Association between Periodontitis and HbA1c Levels in Non-Diabetic Patients: A Systematic Review and Meta-Analysis. Healthcare. 2023; 11(19):2649. https://doi.org/10.3390/healthcare11192649
Chicago/Turabian StyleZhao, Dan, Yangyang Sun, Xin Li, Xiaoxiao Wang, Lijie Lu, Chen Li, Yaping Pan, and Songlin Wang. 2023. "Association between Periodontitis and HbA1c Levels in Non-Diabetic Patients: A Systematic Review and Meta-Analysis" Healthcare 11, no. 19: 2649. https://doi.org/10.3390/healthcare11192649
APA StyleZhao, D., Sun, Y., Li, X., Wang, X., Lu, L., Li, C., Pan, Y., & Wang, S. (2023). Association between Periodontitis and HbA1c Levels in Non-Diabetic Patients: A Systematic Review and Meta-Analysis. Healthcare, 11(19), 2649. https://doi.org/10.3390/healthcare11192649






