Acupuncture Treatment for Emotional Problems in Women with Infertility: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Data Sources and Searches
2.2.1. Data Sources
2.2.2. Search Strategy
2.3. Eligibility Criteria for Study Selection
2.3.1. Types of Studies
2.3.2. Participants
2.3.3. Types of Interventions
2.3.4. Types of Comparisons
2.3.5. Types of Outcome Measures
Primary Outcomes
- (1)
- Emotion-related assessment scales (e.g., State-Trait Anxiety Inventory (STAI), Self-rating Anxiety Scale (SAS), Amsterdam Preoperative Anxiety and Information Scale (APAIS), Hamilton Anxiety-rating Scale (HAS), Self-rating Depression Scale (SDS), Hamilton Depression Rating Scale (HAM-D), Infertility Self-Efficacy scale (ISE), and Fertility Problem Inventory (FPI))
Secondary Outcomes
- (1)
- Total effectiveness rate for emotional problems
- (2)
- Quality of life
- (3)
- Clinical pregnancy rate
- (4)
- Adverse events
2.4. Data Collection and Analysis
2.4.1. Selection of Studies
2.4.2. Data Extraction
2.4.3. Assessment of Risk of Bias
2.4.4. Data Synthesis
3. Results
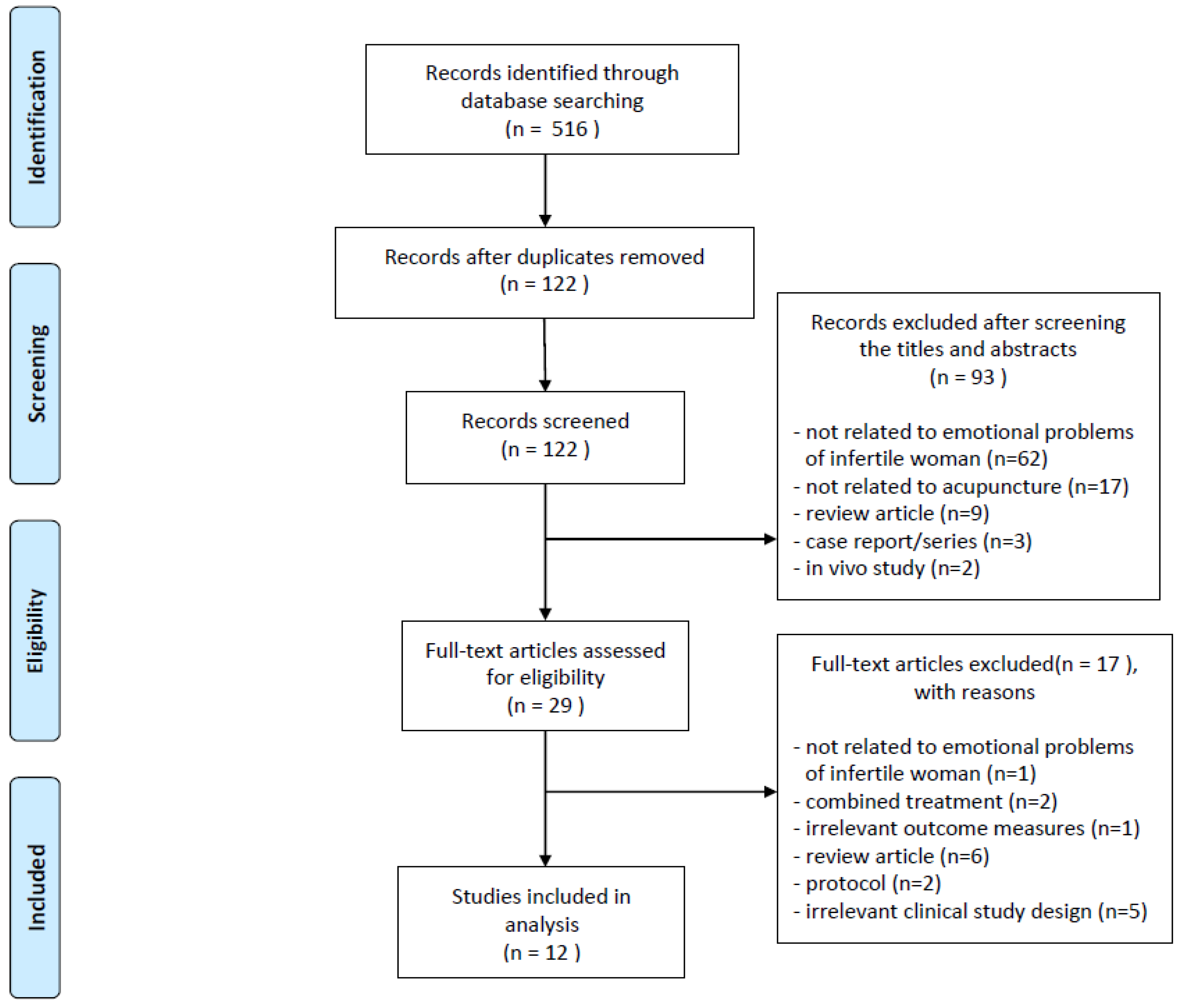
3.1. Study Selection
3.2. Main Characteristics of the Included Studies
3.3. Interventions
3.4. Control Intervention
3.5. Outcomes
3.5.1. Anxiety-Related Assessment Scales
State–Trait Anxiety Inventory (STAI)
- Acupuncture treatment versus no treatment
- 2.
- Acupuncture treatment versus sham acupuncture treatment
Self-Rating Anxiety Scale (SAS)
- Acupuncture treatment versus no treatment
- 2.
- Acupuncture treatment versus sham acupuncture treatment
Amsterdam Preoperative Anxiety and Information Scale (APAIS)
- Acupuncture treatment versus no treatment
- 2.
- Acupuncture treatment versus sham acupuncture treatment
Hamilton Anxiety-Rating Scale (HAS)
- Acupuncture treatment versus sham acupuncture treatment
3.5.2. Depression-Related Assessment Scales
Self-Rating Depression Scale (SDS)
- Acupuncture treatment versus no treatment
- 2.
- Acupuncture treatment versus sham acupuncture treatment
Hamilton Depression Rating Scale (HAM-D)
- Acupuncture plus conventional treatment versus conventional treatment
3.5.3. Low Self-Efficacy-Related Assessment Scales
Infertility Self-Efficacy Scale
- Acupuncture treatment versus no treatment
- 2.
- Acupuncture treatment versus sham acupuncture treatment
3.5.4. Infertility-Related Stress Assessment Scales
Fertility Problem Inventory (FPI)
- Acupuncture treatment versus no treatment
3.5.5. Total Effectiveness Rate
Acupuncture Plus Conventional Treatment Versus Conventional Treatment
3.5.6. Quality of Life
Acupuncture Treatment Versus Sham Acupuncture Treatment
3.5.7. Clinical Pregnancy Rate
Acupuncture Treatment Versus No Treatment
Acupuncture Treatment Versus Sham Acupuncture Treatment
3.5.8. Adverse Events
3.6. Assessment for ROB
4. Discussion
4.1. Main Findings
4.2. Strength and Limitation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zegers-Hochschild, F.; Adamson, G.D.; de Mouzon, J.; Ishihara, O.; Mansour, R.; Nygren, K.; Sullivan, E.; Vanderpoel, S. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology. Fertil. Steril. 2009, 92, 1520–1524. [Google Scholar] [CrossRef] [PubMed]
- Gerrits, T.; Van Rooij, F.; Esho, T.; Ndegwa, W.; Goossens, J.; Bilajbegovic, A.; Jansen, A.; Kioko, B.; Koppen, L.; Kemunto Migiro, S.; et al. Infertility in the Global South: Raising awareness and generating insights for policy and practice. Facts Views Vis. Obgyn 2017, 9, 39–44. [Google Scholar] [PubMed]
- Carson, S.A.; Kallen, A.N. Diagnosis and Management of Infertility: A Review. JAMA 2021, 326, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Phillips, K.; Olanrewaju, R.A.; Omole, F. Infertility: Evaluation and Management. Am. Fam. Physician 2023, 107, 623–630. [Google Scholar]
- Zhou, Z.; Zheng, D.; Wu, H.; Li, R.; Xu, S.; Kang, Y.; Cao, Y.; Chen, X.; Zhu, Y.; Xu, S.; et al. Epidemiology of infertility in China: A population-based study. BJOG 2018, 125, 432–441. [Google Scholar] [CrossRef]
- Sun, H.; Gong, T.T.; Jiang, Y.T.; Zhang, S.; Zhao, Y.H.; Wu, Q.J. Global, regional, and national prevalence and disability-adjusted life-years for infertility in 195 countries and territories, 1990–2017: Results from a global burden of disease study, 2017. Aging 2019, 11, 10952–10991. [Google Scholar] [CrossRef]
- Cwikel, J.; Gidron, Y.; Sheiner, E. Psychological interactions with infertility among women. Eur. J. Obstet. Gynecol. Reprod. Biol. 2004, 117, 126–131. [Google Scholar] [CrossRef]
- Sharma, A.; Shrivastava, D. Psychological Problems Related to Infertility. Cureus 2022, 14, e30320. [Google Scholar] [CrossRef]
- Ogawa, M.; Takamatsu, K.; Horiguchi, F. Evaluation of factors associated with the anxiety and depression of female infertility patients. Biopsychosoc. Med. 2011, 5, 15. [Google Scholar] [CrossRef]
- Deka, P.K.; Sarma, S. Psychological Aspects of Infertility. BJMP 2010, 3, a336. [Google Scholar]
- Fallahzadeh, H.; Zareei Mahmood Abadi, H.; Momayyezi, M.; Malaki Moghadam, H.; Keyghobadi, N. The comparison of depression and anxiety between fertile and infertile couples: A meta-analysis study. Int. J. Reprod. Biomed. 2019, 17, 153–162. [Google Scholar] [CrossRef] [PubMed]
- De Berardis, D.; Mazza, M.; Marini, S.; Del Nibletto, L.; Serroni, N.; Pino, M.C.; Valchera, A.; Ortolani, C.; Ciarrocchi, F.; Martinotti, G.; et al. Psychopathology, emotional aspects and psychological counselling in infertility: A review. Clin. Ther. 2014, 165, 163–169. [Google Scholar] [PubMed]
- Matthiesen, S.M.; Frederiksen, Y.; Ingerslev, H.J.; Zachariae, R. Stress, distress and outcome of assisted reproductive technology (ART): A meta-analysis. Hum. Reprod. 2011, 26, 2763–2776. [Google Scholar] [CrossRef] [PubMed]
- Gameiro, S.; Boivin, J.; Peronace, L.; Verhaak, C.M. Why do patients discontinue fertility treatment? A systematic review of reasons and predictors of discontinuation in fertility treatment. Hum. Reprod. Update 2012, 18, 652–669. [Google Scholar] [CrossRef] [PubMed]
- Lynch, C.D.; Prasad, M.R. Association between infertility treatment and symptoms of postpartum depression. Fertil. Steril. 2014, 102, 1416–1421. [Google Scholar] [CrossRef]
- Lee, J.Y.; Hwang, J.Y. A study on postpartum symptoms and their related factors in Korea. Taiwan J. Obstet. Gynecol. 2015, 54, 355–363. [Google Scholar] [CrossRef]
- Li, C.C.; Hwang, J.L.; Ko, Y.L.; Chen, H.H.; Chien, L.Y. Factors associated with postpartum depressive symptoms among women who conceived with infertility treatment. Acta Psychol. 2023, 238, 103987. [Google Scholar] [CrossRef]
- Hammerli, K.; Znoj, H.; Burri, S.; Graf, P.; Wunder, D.; Perrig-Chiello, P. Psychological interventions for infertile patients: A review of existing research and a new comprehensive approach. Counsel. Psychother. Res. 2008, 8, 246–252. [Google Scholar] [CrossRef]
- Maleki-Saghooni, N.; Amirian, M.; Sadeghi, R.; Latifnejad Roudsari, R. Effectiveness of infertility counseling on pregnancy rate in infertile patients undergoing assisted reproductive technologies: A systematic review and meta-analysis. Int. J. Reprod. Biomed. 2017, 15, 391–402. [Google Scholar] [CrossRef]
- Sniezek, D.P.; Siddiqui, I.J. Acupuncture for Treating Anxiety and Depression in Women: A Clinical Systematic Review. Med. Acupunct. 2013, 25, 164–172. [Google Scholar] [CrossRef]
- Pilkington, K. Anxiety, depression and acupuncture: A review of the clinical research. Auton. Neurosci. 2010, 157, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Pilkington, K.; Kirkwood, G.; Rampes, H.; Cummings, M.; Richardson, J. Acupuncture for anxiety and anxiety disorders—A systematic literature review. Acupunct. Med. 2007, 25, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Armour, M.; Smith, C.A.; Wang, L.Q.; Naidoo, D.; Yang, G.Y.; MacPherson, H.; Lee, M.S.; Hay, P. Acupuncture for Depression: A Systematic Review and Meta-Analysis. J. Clin. Med. 2019, 8, 1140. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Lee, M.S.; Choi, J.Y.; Lee, S.W.; Jeong, S.Y.; Ernst, E. Acupuncture and heart rate variability: A systematic review. Auton. Neurosci. 2010, 155, 5–13. [Google Scholar] [CrossRef]
- Shen, C.; Wu, M.; Shu, D.; Zhao, X.; Gao, Y. The role of acupuncture in in vitro fertilization: A systematic review and meta-analysis. Gynecol. Obstet. Investig. 2015, 79, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Qian, Y.; Xia, X.R.; Ochin, H.; Huang, C.; Gao, C.; Gao, L.; Cui, Y.G.; Liu, J.Y.; Meng, Y. Therapeutic effect of acupuncture on the outcomes of in vitro fertilization: A systematic review and meta-analysis. Arch. Gynecol. Obstet. 2017, 295, 543–558. [Google Scholar] [CrossRef]
- Xie, Z.Y.; Peng, Z.H.; Yao, B.; Chen, L.; Mu, Y.Y.; Cheng, J.; Li, Q.; Luo, X.; Yang, P.Y.; Xia, Y.B. The effects of acupuncture on pregnancy outcomes of in vitro fertilization: A systematic review and meta-analysis. BMC Complement. Altern. Med. 2019, 19, 131. [Google Scholar] [CrossRef]
- Hassanzadeh Bashtian, M.; Latifnejad Roudsari, R.; Sadeghi, R. Effects of Acupuncture on Anxiety in Infertile Women: A Systematic Review of the Literature. J. Midwifery Women’s Health 2017, 5, 842–848. [Google Scholar]
- Hwang, S.I.; Sung, S.H.; Yoon, Y.J.; Park, J.K. Acupuncture treatment for emotional problems in infertile women: A protocol for systematic review and meta-analysis. Medicine 2021, 100, e26306. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- MacPherson, H.; Altman, D.G.; Hammerschlag, R.; Youping, L.; Taixiang, W.; White, A.; Moher, D. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): Extending the CONSORT statement. J. Evid. Based Med. 2010, 3, 140–155. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savovi´c, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.C. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Domar, A.D.; Meshay, I.; Kelliher, J.; Alper, M.; Powers, R.D. The impact of acupuncture on in vitro fertilization outcome. Fertil. Steril. 2009, 91, 723–726. [Google Scholar] [CrossRef]
- Smith, C.A.; Ussher, J.M.; Perz, J.; Carmady, B.; de Lacey, S. The effect of acupuncture on psychosocial outcomes for women experiencing infertility: A pilot randomized controlled trial. J. Altern. Complement. Med. 2011, 17, 923–930. [Google Scholar] [CrossRef] [PubMed]
- Guo, Q. The Initial Study of Bushen-Shugan Therapy to Improve the Embryo Implantation Rate of Invitro Fertilization and Embryo Transfer by Ameliorating Resistence Index of Theca Blood. Master’s Thesis, Shandong University of Traditional Chinese Medicine, Jinan, China, 2011. [Google Scholar]
- Isoyama, D.; Cordts, E.B.; de Souza van Niewegen, A.M.; de Almeida Pereira de Carvalho, W.; Matsumura, S.T.; Barbosa, C.P. Effect of acupuncture on symptoms of anxiety in women undergoing in vitro fertilisation: A prospective randomised controlled study. Acupunct. Med. 2012, 30, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Qu, F.; Zhang, D.; Chen, L.T.; Wang, F.F.; Pan, J.X.; Zhu, Y.M.; Ma, C.M.; Huang, Y.T.; Ye, X.Q.; Sun, S.J.; et al. Auricular Acupressure Reduces Anxiety Levels and Improves Outcomes of in Vitro Fertilization: A Prospective, Randomized and Controlled Study. Sci. Rep. 2014, 4, 5028. [Google Scholar] [CrossRef]
- Fang, Z. Effects of TEAS on affecting Oxytocin and Vasopressin Levels and Improving the Pregnancy Outcome in Patients with Anxiety and Depression. Master’s Thesis, Shandong University of Traditional Chinese Medicine, Jinan, China, 2016. [Google Scholar]
- Xing, L.F.; Wu, Y.; Wang, F.F.; Zhu, Y.H.; Ma, C.M.; Yan, Y.Y.; Sun, S.J.; Pan, J.X.; Robinson, N.; Hardiman, P.; et al. Transcutaneous electrical acupoint stimulation alleviates the anxiety levels of IVF: A prospective, randomized and controlled study. Eur. J. Integr. Med. 2018, 20, 126–130. [Google Scholar] [CrossRef]
- Bashtian, M.H.; Khadivzadeh, T.; Aval, S.B.; Esmaily, H. Evaluation of acupressure effects on self-efficacy and pregnancy rate in infertile women under in vitro fertilization/intracytoplasmic sperm injection treatment: A randomized controlled trial. J. Educ. Health Promot. 2018, 7, 84. [Google Scholar]
- Yuan, S.; Pan, C. Clinical Observation on Pulse Acupuncture in the Treatment of Infertile Women with Depression State. Clin. Med. Eng. 2018, 25, 877–878. [Google Scholar]
- Smith, C.A.; de Lacey, S.; Chapman, M.; Ratcliffe, J.; Norman, R.J.; Johnson, N.P.; Fahey, P. The effects of acupuncture on the secondary outcomes of anxiety and quality of life for women undergoing IVF: A randomized controlled trial. Acta Obstet. Gynecol. Scand. 2019, 98, 460–469. [Google Scholar] [CrossRef]
- Ma, J.; Zhang, Q. Clinical study of acupuncture on improving endometrial receptivity, emotion of anxiety and depression, and pregnancy outcome in IVF-ET repeated implantation failure patients with syndrome of kidney deficiency and liver stagnation. Acad. J. Shanghai Univ. Tradit. Chin. 2019, 33, 32–38. [Google Scholar]
- Guven, P.G.; Cayir, Y.; Borekci, B. Effectiveness of acupuncture on pregnancy success rates for women undergoing in vitro fertilization: A randomized controlled trial. Taiwan J. Obstet. Gynecol. 2020, 59, 282–286. [Google Scholar] [CrossRef]
- Kim, H.; Park, H.J.; Han, S.M.; Hahm, D.H.; Lee, H.J.; Kim, K.S.; Shim, I. The effects of acupuncture stimulation at PC6 (Neiguan) on chronic mild stress-induced biochemical and behavioral responses. Neurosci. Lett. 2009, 460, 56–60. [Google Scholar] [CrossRef]
- Zhu, C.; Wang, X.Y.; Zhao, J.; Long, B.; Xiao, X.; Pan, L.Y.; Yuan, T.F.; Chen, J.H. Effect of transdermal drug delivery therapy on anxiety symptoms in schizophrenic patients. Front. Neurosci. 2023, 17, 1177214. [Google Scholar] [CrossRef]
- Kwon, S.; Lee, B.; Yeom, M.; Sur, B.J.; Kim, M.; Kim, S.T.; Park, H.J.; Lee, H.; Hahm, D.H. Modulatory effects of acupuncture on murine depression-like behavior following chronic systemic inflammation. Brain Res. 2012, 1472, 149–160. [Google Scholar] [CrossRef]










| First Author (Year) | Country | Sample Size (EG:CG) | Mean Age (±SD) | Mean Duration of Infertility (±SD, yr) | Emotional Problem(s) | Interventions | Outcome Measurement | Main Results | AEs | |
|---|---|---|---|---|---|---|---|---|---|---|
| EG | CG | |||||||||
| Domar (2009) [33] | U.S.A. | 146 (78:68) | EG: 36.1 CG: 36.1 | NR | anxiety | Acupuncture | No treatment | 1. STAI 2. CPR | 1. positive a 2. NS | NR |
| Smith (2011) [34] | Australia | 32 (16:16) | EG: 35.1 ± 4.2 CG: 34.1 ± 5.2 | EG: 4.50 ± 3.5 CG: 3.57 ± 2.4 | anxiety, self-efficacy, infertility-related stress | Acupuncture | No treatment | 1. STAI 2. FPI (1) Social concern (2) Sexual concern (3) Relationship concern (4) Rejection of childfree lifestyle (5) Need for parenthood 3. ISE | 1. NS 2. (1) NS (2) NS (3) positive a (4) NS (5) NS 3. NS | NR |
| Guo (2011) [35] | China | 64 (33:31) | EG: 31.49 ± 2.96 CG: 30.93 ± 3.39 | EG: 4.02 ± 2.13 CG: 3.86 ± 1.74 | anxiety, depression | Acupuncture | No treatment | 1. SAS 2. SDS 3. CPR | 1. positive b 2. positive b 3. NS | NR |
| Isoyama (2012) [36] | Brazil | 43 (22:21) | EG: 34.1 ± 4.6 CG: 34.3 ± 4.6 | EG: 3.4 ± 1.5 CG: 4.7 ± 2.8 | anxiety | Acupuncture | Sham Acupuncture | 1. HAS 2. CPR | 1. positive c 2. positive b 3. NS | NR |
| Qu (2014) [37] | China | 305 (101:102:102) | EG: 31.65 ± 4.30 CG1: 30.87 ± 4.12 CG2: 30.95 ± 4.78 | EG: 5.19 ± 3.39 CG1: 4.16 ± 3.21 CG2: 4.97 ± 4.17 | anxiety | Acupressure | CG1: Sham Acupressure CG2: No treatment | 1. STAI 2. APAIS 3. CPR | 1. positive a(d,e) 2. positive a(d,e) 3. positive b(d,e) | None |
| Fang (2016) [38] | China | 180 (60:60:60) | EG: 29.69 ± 0.47 CG1: 29.53 ± 0.48 CG2: 30.39 ± 0.55 | NR | anxiety, depression | TEAS | CG1: Sham TEAS CG2: No treatment | 1. SAS 2. SDS 3. CPR | 1. positive a(d,e) 2. positive a(d,e) 3. positive a(d,e) | NR |
| Xing (2018) [39] | China | 180 (90:90) | EG: 31.99 ± 4.56 CG: 31.24 ± 4.91 | EG: 5.55 ± 4.42 CG: 5.32 ± 3.91 | anxiety | TEAS | No Treatment | 1. STAI 2. APAIS | 1. positive a 2. positive a | None |
| Bashtian (2018) [40] | Iran | 132 (45:45:42) | EG: 30.20 ± 2.56 CG: 31.08 ± 2.87 | 3.89 ± 3.80 | self-efficacy | Acupressure | CG1: Sham Acupressure CG2: No treatment | 1. ISE 2. CPR | 1. NS (d,e) 2. NS (d,e) | NR |
| Yuan (2018) [41] | China | 98 (49:49) | EG: 35.7 ± 4.3 CG: 35.7 ± 4.2 | EG: 15.87 ± 2.16(mo) CG: 16.33 ± 1.81(mo) | depression | Acupuncture + CG Treatment | Fluoxetine 20 mg | 1. HAM-D 2. TER | 1. positive a 2. positive b | NR |
| Smith (2019) [42] | Australia, New Zealand | 608 (301:307) | EG: 30.04 ± 2.98 CG: 30.55 ± 3.71 | NR | anxiety | Acupuncture | Sham Acupuncture | 1. STAI 2. SF-36 | 1. positive a 2. NS | NR |
| Ma (2019) [43] | China | 70 (35:35) | EG 30.70 ± 5.14 CG 29.98 ± 4.95 | EG: 4.4 ± 1.8 CG: 4.9 ± 1.5 | anxiety, depression | Acupuncture | No treatment | 1. SAS 2. SDS 3. CPR | 1. positive a 2. NS 3. positive a | NR |
| Guven (2020) [44] | Turkey | 72 (36:36) | EG: 30.3 ± 3.4 CG: 31.5 ± 4 | NR | anxiety | Acupuncture | No treatment | 1. STAI 2. CPR | 1. positive c 2. positive b | None |
| First Author (Year) | TYPE of Acupuncture | Regimen | Number of Needle Insertions | Acupuncture Points | Depth of Insertion | Response Sought | Needle Stimulation (Frequency) | Needle Retention Time | Types of Needle (Diameter, Length) | Co-Interventions |
|---|---|---|---|---|---|---|---|---|---|---|
| Domar (2009) [33] | Acupuncture | 2 sessions (① before ET, ② after ET) | 12–13 | ① PC6, SP8, LR3, GV20, ST29, Ear points (TF4, CO18, TF2, AT3) (uni) ② ST36, SP6, SP10, LI4, Ear points (TF4, CO18, TF2, AT3) (uni) | 10–20 mm | de qi | manual | 25 min | 0.25 mm, 25 mm/ 0.2 mm, 13 mm (ear points) | none |
| Smith (2011) [34] | Acupuncture | 6 sessions (8 weeks) | 3–11 | usually PC5, PC6, HT5, HT7 (points selected in response to emotional complaints) | NR | de qi | manual | 45 min | 0.2 mm, 30 mm | none |
| Guo (2011) [35] | Acupuncture | NR (from the day of downregulation until the HCG injection) | 7 | CV3, LR3, EX-CA1, SP6 | CV3(1–1.5 cun), LR3(1–1.5 cun), EX-CA1 (1.5–2 cun), SP6(0.5–1.0 cun) | de qi | manual | NR | NR, 40 mm | none |
| Isoyama (2012) [36] | Acupuncture | 4–6 sessions (once a week, during the process from ovulation induction to the result of β-hcG) | 7 | HT7, PC6, CV17, GV20, EX-HN3 | NR | de qi | manual | 25 min | 0.25 mm, 40 mm | none |
| Qu (2014) [37] | Acupressure | 24 sessions (4 times/day, 6 days (from 1 day before TVOR to the next day of ET)) | 6 | Ear points (TF4, CO18, TF2) | NR | NR | NR | 15 min | NR | none |
| Fang (2016) [38] | TEAS | NR (from the day of downregulation until the HCG injection) | 8 | HT7, PC6, ST36, SP6 | NR | NR | electrical (2/15 Hz) | 30 min | NR | none |
| Xing (2018) [39] | TEAS | 2 sessions (① 24 h before TVOR ② 2 h before ET) | 6–8 | ① SP10, SP8, LR3, ST36 ② EX-CA1, RN4, PC6, CV12 | NR | visible muscle contraction response | electrical (2/100 Hz) | 30 min | NR | none |
| Bashtian (2018) [40] | Acupressure | 12 sessions (4 sessions/week, until the day before ET) | 4 | PC6, HT7 | NR | feeling of heaviness | NR | 3 min | NR | none |
| Yuan (2018) [41] | Acupuncture | 28 sessions (daily, 28 days) | 10–14 | GV20, EX-HN3, PC6, SP6, CV3, CV4, EX-CA1 (Deficiency of both the heart and spleen: add ST36, HT7/ Liver-qi stagnation: add LR3, LI4) | NR | NR | manual | 30 min | NR | CG Treatment (Fluoxetine 20 mg) |
| Smith (2019) [42] | Acupuncture | 3 sessions (① between day 6 and 8 of ovarian stimulation ② 1 h before ET ③ following ET) | 8–13 | ① ST29, CV4, CV6, SP6 SP10 ② ST29, SP8, SP10, LR3, CV4, ear point (TF2), one of three (HT7, PC6 or EX-HN3) ③ GV20, KI3, ST36, SP6, PC6, ear point (TF4) | NR | de qi | manual | 25 min | 0.35 mm, 70 mm | none |
| Ma (2019) [43] | Acupuncture | NR (① every other day (from the 2nd day of menstruation until the day of ET) ② 30 min after ET) | 12–18 | ① ST25, CV4, CV6, ST29, ST36, SP8, EX-CA1, SP6, LR3, GV20, EX-HN3 ② ST25, CV4, CV6, ST29, ST36, SP8, KI3 | NR | de qi | manual | 30 min | 0.25 mm, 40 mm | none |
| Guven (2020) [44] | Acupuncture | 3 sessions (① 1 week before ET ② 30 min before ET ③ 30 min after ET) | 7–10 | ① HT7, LI4, GV20, Ear point (TF4) ② CV3, CV4, CV6, GV20, LR3, ST30, SP8 ③ LI4, SP6, SP9, ST36 | 1–2 cun | NR | none | 30 min | 0.25 mm, 25 mm | none |
| First Author (Year) | Type of Acupuncture | Regimen | Number of Needle Insertions (per Session) | Acupuncture Points | Depth of Insertion | Response Sought | Needle Stimulation (Frequency) | Needle Retention Time | Types of Needle (Diameter, Length) |
|---|---|---|---|---|---|---|---|---|---|
| Isoyama (2012) [36] | Sham Acupuncture | 4–6 sessions (once a week, during the process from ovulation induction to the result of β-hcG) | 7 | located close to but not on the real acupuncture points (distance of approximately 1.5 cm in regions) | 2 mm | none | none | 25 min | 0.25 mm, 40 mm |
| Qu (2014) [37] | Sham Acupressure | 24 sessions (4 times/day, 6 days (from 1 day before TVOR to the next day of ET)) | 6 | Ear points (CO17, CO4, CO7) | NR | NR | NR | 15 min | NR |
| Fang (2016) [38] | Sham TEAS | NR (from the day of downregulation until the HCG injection) | 8 | HT7, PC6, ST36, SP6 | NR | NR | electrical (NR) | 30 min | Sham TEAS (frequency which has no therapeutic effect) |
| Bashtian (2018) [40] | Sham Acupressure | 12 sessions (4 sessions/week, until the day before ET) | 4 | 2 cm distance of the main points | NR | NR | NR | 3 min | NR |
| Smith (2019) [42] | Sham Acupuncture | 3 sessions (① between day 6 and 8 of ovarian stimulation ② 1 h before ET ③ following ET) | 6 | sham points at locations away from known acupuncture points and with no known function | NR | NR | NR | 25 min | 0.35 mm, 70 mm (sham needle (non-insertive): Park Sham Device) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, S.-I.; Yoon, Y.-J.; Sung, S.-H.; Cho, S.-J.; Park, J.-K. Acupuncture Treatment for Emotional Problems in Women with Infertility: A Systematic Review and Meta-Analysis. Healthcare 2023, 11, 2704. https://doi.org/10.3390/healthcare11202704
Hwang S-I, Yoon Y-J, Sung S-H, Cho S-J, Park J-K. Acupuncture Treatment for Emotional Problems in Women with Infertility: A Systematic Review and Meta-Analysis. Healthcare. 2023; 11(20):2704. https://doi.org/10.3390/healthcare11202704
Chicago/Turabian StyleHwang, Su-In, Young-Jin Yoon, Soo-Hyun Sung, Su-Jin Cho, and Jang-Kyung Park. 2023. "Acupuncture Treatment for Emotional Problems in Women with Infertility: A Systematic Review and Meta-Analysis" Healthcare 11, no. 20: 2704. https://doi.org/10.3390/healthcare11202704
APA StyleHwang, S.-I., Yoon, Y.-J., Sung, S.-H., Cho, S.-J., & Park, J.-K. (2023). Acupuncture Treatment for Emotional Problems in Women with Infertility: A Systematic Review and Meta-Analysis. Healthcare, 11(20), 2704. https://doi.org/10.3390/healthcare11202704





