Do Differences Exist in Impact Test Domains between Youth Athletes with and without an Anterior Cruciate Ligament Injury?
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Subjects
2.3. Statistical Analysis
3. Results
3.1. Demographics
3.2. Outcomes
4. Discussion
4.1. Conclusions
4.2. Alternative Factors Contributing to Injury in Youth Athletes
4.3. Limitations
4.4. Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- NFHS. NFHS Releases First High School Sports Participation Survey in Three Years. 2022. Available online: https://www.nfhs.org/articles/nfhs-releases-first-high-school-sports-participation-survey-in-three-years/ (accessed on 13 September 2023).
- NCAA Media Center. NCAA Student-Athletes Surpass 520,000, Set New Record. 2022. Available online: https://www.ncaa.org/news/2022/12/5/media-center-ncaa-student-athletes-surpass-520-000-set-new-record.aspx (accessed on 13 September 2023).
- Tirabassi, J.; Brou, L.; Khodaee, M.; Lefort, R.; Fields, S.K.; Comstock, R.D. Epidemiology of High School Sports-Related Injuries Resulting in Medical Disqualification: 2005–2006 through 2013–2014 Academic Years. Am. J. Sports Med. 2016, 44, 2925–2932. [Google Scholar] [CrossRef] [PubMed]
- Bram, J.T.; Magee, L.C.; Mehta, N.N.; Patel, N.M.; Ganley, T.J. Anterior Cruciate Ligament Injury Incidence in Adolescent Athletes: A Systematic Review and Meta-Analysis. Am. J. Sports Med. 2021, 49, 1962–1972. [Google Scholar] [CrossRef] [PubMed]
- Yoo, H.; Marappa-Ganeshan, R. Anatomy, Bony Pelvis and Lower Limb, Knee Anterior Cruciate Ligament. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Domnick, C.; Raschke, M.J.; Herbort, M. Biomechanics of the Anterior Cruciate Ligament: Physiology, Rupture and Reconstruction Techniques. World J. Orthop. 2016, 7, 82–93. [Google Scholar] [CrossRef] [PubMed]
- Griffin, L.Y.; Agel, J.; Albohm, M.J.; Arendt, E.A.; Dick, R.W.; Garrett, W.E.; Garrick, J.G.; Hewett, T.E.; Huston, L.; Ireland, M.L.; et al. Noncontact Anterior Cruciate Ligament Injuries: Risk Factors and Prevention Strategies. J. Am. Acad. Orthop. Surg. 2000, 8, 141–150. [Google Scholar] [CrossRef]
- Stanley, L.E.; Kerr, Z.Y.; Dompier, T.P.; Padua, D.A. Sex Differences in the Incidence of Anterior Cruciate Ligament, Medial Collateral Ligament, and Meniscal Injuries in Collegiate and High School Sports: 2009–2010 Through 2013–2014. Am. J. Sports Med. 2016, 44, 1565–1572. [Google Scholar] [CrossRef]
- Sutton, K.M.; Bullock, J.M. Anterior Cruciate Ligament Rupture: Differences between Males and Females. J. Am. Acad. Orthop. Surg. 2013, 21, 41–50. [Google Scholar] [CrossRef]
- Wiggins, A.J.; Grandhi, R.K.; Schneider, D.K.; Stanfield, D.; Webster, K.E.; Myer, G.D. Risk of Secondary Injury in Younger Athletes After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. Am. J. Sports Med. 2016, 44, 1861–1876. [Google Scholar] [CrossRef]
- Gans, I.; Retzky, J.S.; Jones, L.C.; Tanaka, M.J. Epidemiology of Recurrent Anterior Cruciate Ligament Injuries in National Collegiate Athletic Association Sports: The Injury Surveillance Program, 2004–2014. Orthop. J. Sports Med. 2018, 6, 2325967118777823. [Google Scholar] [CrossRef]
- Sepúlveda, F.; Sánchez, L.; Amy, E.; Micheo, W. Anterior Cruciate Ligament Injury: Return to Play, Function and Long-Term Considerations. Curr. Sports Med. Rep. 2017, 16, 172–178. [Google Scholar] [CrossRef]
- Lee, J.; Guzek, R.H.; Shah, N.S.; Lawrence, J.T.R.; Ganley, T.J.; Shah, A.S. How Much Will My Child’s ACL Reconstruction Cost? Availability and Variability of Price Estimates for Anterior Cruciate Ligament Reconstruction in the United States. J. Pediatr. Orthop. 2022, 42, 614–620. [Google Scholar] [CrossRef]
- Piskin, D.; Benjaminse, A.; Dimitrakis, P.; Gokeler, A. Neurocognitive and Neurophysiological Functions Related to ACL Injury: A Framework for Neurocognitive Approaches in Rehabilitation and Return-to-Sports Tests. Sports Health 2022, 14, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Herman, D.C.; Barth, J.T. Drop-Jump Landing Varies With Baseline Neurocognition: Implications for Anterior Cruciate Ligament Injury Risk and Prevention. Am. J. Sports Med. 2016, 44, 2347–2353. [Google Scholar] [CrossRef] [PubMed]
- Swanik, C.B. Brains and Sprains: The Brain’s Role in Noncontact Anterior Cruciate Ligament Injuries. J. Athl. Train. 2015, 50, 1100–1102. [Google Scholar] [CrossRef]
- Grooms, D.R.; Onate, J.A. Neuroscience Application to Noncontact Anterior Cruciate Ligament Injury Prevention. Sports Health 2016, 8, 149–152. [Google Scholar] [CrossRef] [PubMed]
- Alsalaheen, B.; Stockdale, K.; Pechumer, D.; Broglio, S.P. Validity of the Immediate Post Concussion Assessment and Cognitive Testing (ImPACT). Sports Med. Auckl. N. Z. 2016, 46, 1487–1501. [Google Scholar] [CrossRef]
- Swanik, C.B.; Covassin, T.; Stearne, D.J.; Schatz, P. The Relationship between Neurocognitive Function and Noncontact Anterior Cruciate Ligament Injuries. Am. J. Sports Med. 2007, 35, 943–948. [Google Scholar] [CrossRef]
- Wilkerson, G.B. Neurocognitive Reaction Time Predicts Lower Extremity Sprains and Strains. Int. J. Athl. Ther. Train. 2012, 17, 4–9. [Google Scholar] [CrossRef]
- Iverson, G.L.; Lovell, M.R.; Collins, M.W. Interpreting Change on ImPACT Following Sport Concussion. Clin. Neuropsychol. 2003, 17, 460–467. [Google Scholar] [CrossRef]
- Specker, S.M.; Carlson, G.A.; Christenson, G.A.; Marcotte, M. Impulse Control Disorders and Attention Deficit Disorder in Pathological Gamblers. Ann. Clin. Psychiatry Off. J. Am. Acad. Clin. Psychiatr. 1995, 7, 175–179. [Google Scholar] [CrossRef]
- Almonroeder, T.G.; Kernozek, T.; Cobb, S.; Slavens, B.; Wang, J.; Huddleston, W. Divided Attention during Cutting Influences Lower Extremity Mechanics in Female Athletes. Sports Biomech. 2019, 18, 264–276. [Google Scholar] [CrossRef]
- Shultz, S.J.; Schmitz, R.J.; Benjaminse, A.; Collins, M.; Ford, K.; Kulas, A.S. ACL Research Retreat VII: An Update on Anterior Cruciate Ligament Injury Risk Factor Identification, Screening, and Prevention. J. Athl. Train. 2015, 50, 1076–1093. [Google Scholar] [CrossRef] [PubMed]
- Park, S.H.; Yi, C.W.; Shin, J.Y.; Ryu, Y.U. Effects of External Focus of Attention on Balance: A Short Review. J. Phys. Ther. Sci. 2015, 27, 3929–3931. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Zhang, L.; Yue, X.; Memmert, D.; Zhang, Y. Effect of Attentional Focus on Sprint Performance: A Meta-Analysis. Int. J. Environ. Res. Public. Health 2022, 19, 6254. [Google Scholar] [CrossRef] [PubMed]
- Abdollahipour, R.; Wulf, G.; Psotta, R.; Palomo Nieto, M. Performance of Gymnastics Skill Benefits from an External Focus of Attention. J. Sports Sci. 2015, 33, 1807–1813. [Google Scholar] [CrossRef]
- Neumann, D.L. A Systematic Review of Attentional Focus Strategies in Weightlifting. Front. Sports Act. Living 2019, 1, 7. [Google Scholar] [CrossRef]
- McNicholas, K.; Comyns, T.M. Attentional Focus and the Effect on Change-of-Direction and Acceleration Performance. J. Strength Cond. Res. 2020, 34, 1860–1866. [Google Scholar] [CrossRef]
- Uslu, S.; Çetin Özdoğan, E. External Focus Reduces Accuracy and Increases Antagonist Muscle Activation in Novice Adolescent Soccer Players. Mot. Control 2023, 27, 228–241. [Google Scholar] [CrossRef]
- Bencke, J.; Aagaard, P.; Zebis, M.K. Muscle Activation During ACL Injury Risk Movements in Young Female Athletes: A Narrative Review. Front. Physiol. 2018, 9, 445. [Google Scholar] [CrossRef]
- Winstanley, C.A.; Eagle, D.M.; Robbins, T.W. Behavioral Models of Impulsivity in Relation to ADHD: Translation between Clinical and Preclinical Studies. Clin. Psychol. Rev. 2006, 26, 379–395. [Google Scholar] [CrossRef]
- Alosco, M.L.; Fedor, A.F.; Gunstad, J. Attention Deficit Hyperactivity Disorder as a Risk Factor for Concussions in NCAA Division-I Athletes. Brain Inj. 2014, 28, 472–474. [Google Scholar] [CrossRef]
- Brophy, R.H.; Silvers, H.J.; Mandelbaum, B.R. Anterior Cruciate Ligament Injuries: Etiology and Prevention. Sports Med. Arthrosc. Rev. 2010, 18, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Devana, S.K.; Solorzano, C.; Nwachukwu, B.; Jones, K.J. Disparities in ACL Reconstruction: The Influence of Gender and Race on Incidence, Treatment, and Outcomes. Curr. Rev. Musculoskelet. Med. 2022, 15, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Myer, G.D.; Quatman, C.E.; Khoury, J.; Wall, E.J.; Hewett, T.E. Youth versus Adult “Weightlifting” Injuries Presenting to United States Emergency Rooms: Accidental versus Nonaccidental Injury Mechanisms. J. Strength Cond. Res. 2009, 23, 2054–2060. [Google Scholar] [CrossRef] [PubMed]
- Schweizer, N.; Strutzenberger, G.; Franchi, M.V.; Farshad, M.; Scherr, J.; Spörri, J. Screening Tests for Assessing Athletes at Risk of ACL Injury or Reinjury-A Scoping Review. Int. J. Environ. Res. Public. Health 2022, 19, 2864. [Google Scholar] [CrossRef]
- Bushman, T.T.; Grier, T.L.; Canham-Chervak, M.; Anderson, M.K.; North, W.J.; Jones, B.H. The Functional Movement Screen and Injury Risk: Association and Predictive Value in Active Men. Am. J. Sports Med. 2016, 44, 297–304. [Google Scholar] [CrossRef]
- Bring, B.V.; Chan, M.; Devine, R.C.; Collins, C.L.; Diehl, J.; Burkam, B. Functional Movement Screening and Injury Rates in High School and Collegiate Runners: A Retrospective Analysis of 3 Prospective Observational Studies. Clin. J. Sport Med. Off. J. Can. Acad. Sport Med. 2018, 28, 358–363. [Google Scholar] [CrossRef]
- Avedesian, J.M.; McPherson, A.L.; Diekfuss, J.A.; Barber Foss, K.D.; Hogg, J.A.; Zuleger, T.M.; Dufek, J.S.; Myer, G.D. Visual-Spatial Attentional Performance Identifies Lower Extremity Injury Risk in Adolescent Athletes. Clin. J. Sport Med. Off. J. Can. Acad. Sport Med. 2022, 32, 574–579. [Google Scholar] [CrossRef]
- Sainsbury, D.; Downs, J.; Nettoi, K. Leanda McKenna Factors Associated With Sports Injuries in Adolescents Who Play Team Sports at a Nonelite Level: A Scoping Review. J. Orthop. Sports Phys. Ther. 2023, 1, 1–15. [Google Scholar]
- von Rosen, P.; Frohm, A.; Kottorp, A.; Fridén, C.; Heijne, A. Multiple Factors Explain Injury Risk in Adolescent Elite Athletes: Applying a Biopsychosocial Perspective. Scand. J. Med. Sci. Sports 2017, 27, 2059–2069. [Google Scholar] [CrossRef]
- Manderino, L.; Gunstad, J. Collegiate Student Athletes With History of ADHD or Academic Difficulties Are More Likely to Produce an Invalid Protocol on Baseline ImPACT Testing. Clin. J. Sport Med. Off. J. Can. Acad. Sport Med. 2018, 28, 111–116. [Google Scholar] [CrossRef]
- Maietta, J.E.; Barchard, K.A.; Kuwabara, H.C.; Donohue, B.D.; Ross, S.R.; Kinsora, T.F.; Allen, D.N. Influence of Special Education, ADHD, Autism, and Learning Disorders on ImPACT Validity Scores in High School Athletes. J. Int. Neuropsychol. Soc. JINS 2021, 27, 461–471. [Google Scholar] [CrossRef] [PubMed]
- Thoma, R.J.; Cook, J.A.; McGrew, C.; King, J.H.; Pulsipher, D.T.; Yeo, R.A.; Monnig, M.A.; Mayer, A.; Pommy, J.; Campbell, R.A. Convergent and Discriminant Validity of the ImPACT with Traditional Neuropsychological Measures. Cogent Psychol. 2018, 5, 1430199. [Google Scholar] [CrossRef] [PubMed]
| ACL Injury (%) | No ACL Injury (%) | p-Value | |
|---|---|---|---|
| N | 70 (50) | 70 (50) | NE |
| Sex | 1.000 | ||
| Male | 32 (45.7) | 32 (45.7) | |
| Female | 38 (54.3) | 38 (54.3) | |
| Age (Years) | |||
| Mean ± SD | 15.4 ± 1.2 | 15.6 ± 1.1 | 0.461 |
| Median (IQR) | 16 (14–17) | 16 (14–17) | NE |
| ImPACT Composite | ACL Injury | No ACL Injury | p-Value | Cohen’s d |
|---|---|---|---|---|
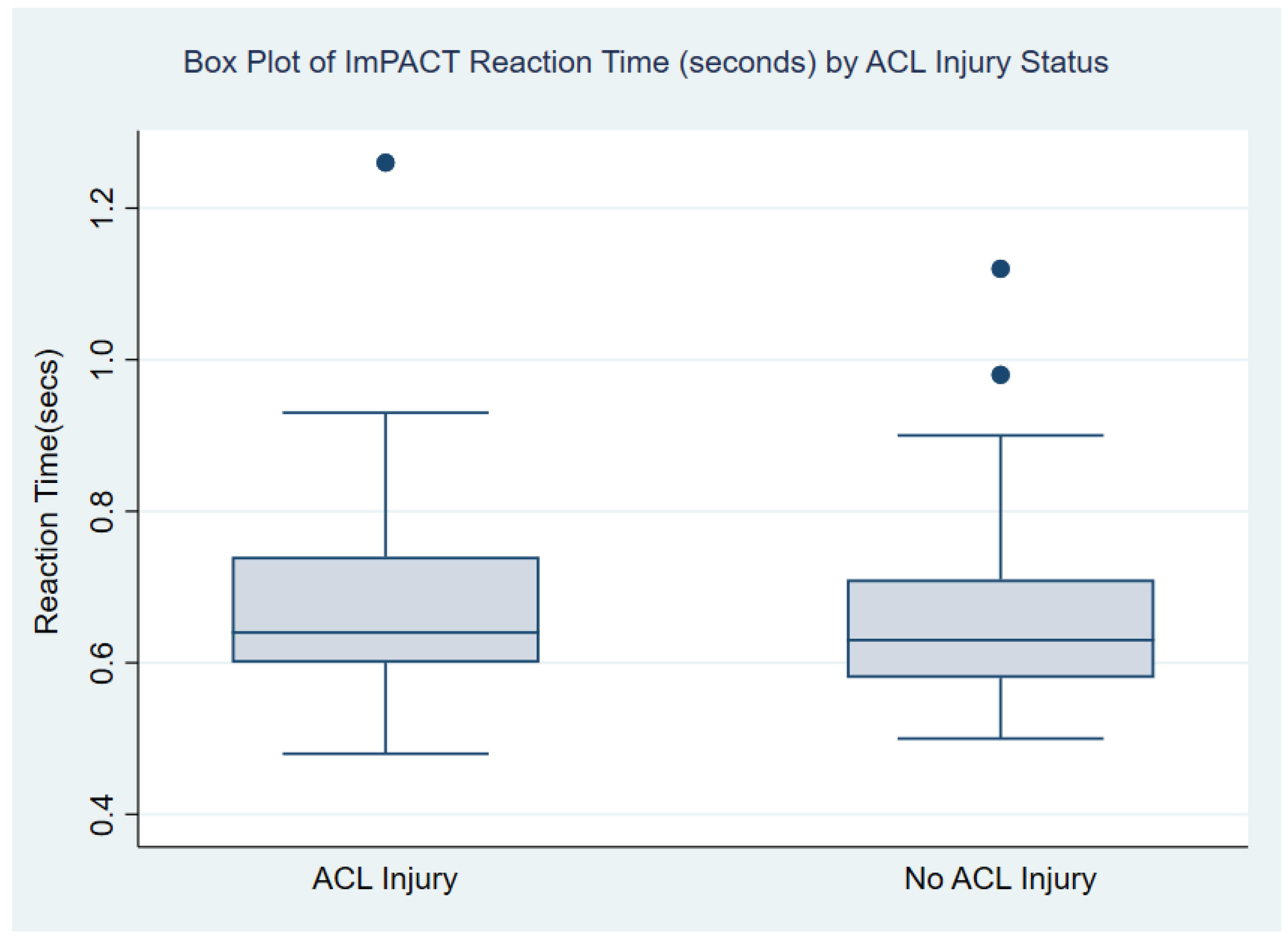
| Reaction Time | ||||
| Mean ± SD | 0.67 ± 0.12 | 0.66 ± 0.12 | 0.432 | 0.13 |
| Median (IQR) | 0.64 (0.51–0.87) | 0.63 (0.51–0.89) | NE | NE |
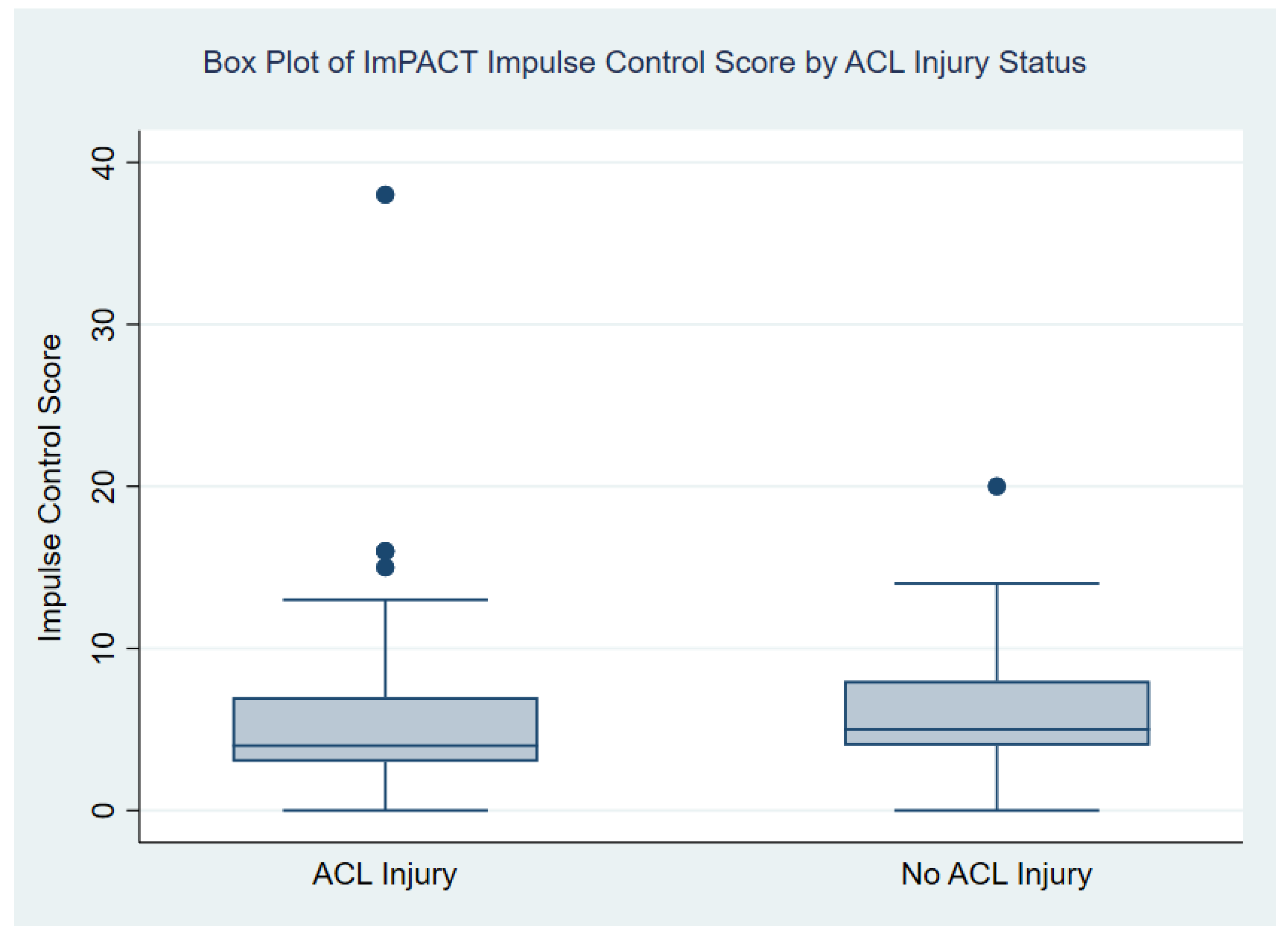
| Impulse Control | ||||
| Mean ± SD | 5.67 ± 5.38 | 6.07 ± 3.75 | 0.611 | 0.09 |
| Median (IQR) | 4 (1–15) | 5 (1–12) | NE | NE |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gureck, A.E.; Crockett, Z.; Barsky, B.W.; Samuels, S.; Frank, J.S.; Storer, S.K.; Fazekas, M.L. Do Differences Exist in Impact Test Domains between Youth Athletes with and without an Anterior Cruciate Ligament Injury? Healthcare 2023, 11, 2764. https://doi.org/10.3390/healthcare11202764
Gureck AE, Crockett Z, Barsky BW, Samuels S, Frank JS, Storer SK, Fazekas ML. Do Differences Exist in Impact Test Domains between Youth Athletes with and without an Anterior Cruciate Ligament Injury? Healthcare. 2023; 11(20):2764. https://doi.org/10.3390/healthcare11202764
Chicago/Turabian StyleGureck, Ashley E., Zack Crockett, Brandon W. Barsky, Shenae Samuels, Jeremy S. Frank, Stephen K. Storer, and Matthew L. Fazekas. 2023. "Do Differences Exist in Impact Test Domains between Youth Athletes with and without an Anterior Cruciate Ligament Injury?" Healthcare 11, no. 20: 2764. https://doi.org/10.3390/healthcare11202764
APA StyleGureck, A. E., Crockett, Z., Barsky, B. W., Samuels, S., Frank, J. S., Storer, S. K., & Fazekas, M. L. (2023). Do Differences Exist in Impact Test Domains between Youth Athletes with and without an Anterior Cruciate Ligament Injury? Healthcare, 11(20), 2764. https://doi.org/10.3390/healthcare11202764


_MD__MPH_PhD.png)



