Contrast-Enhanced Ultrasound Follow-Up for Acute Pyelonephritis Patients
Abstract
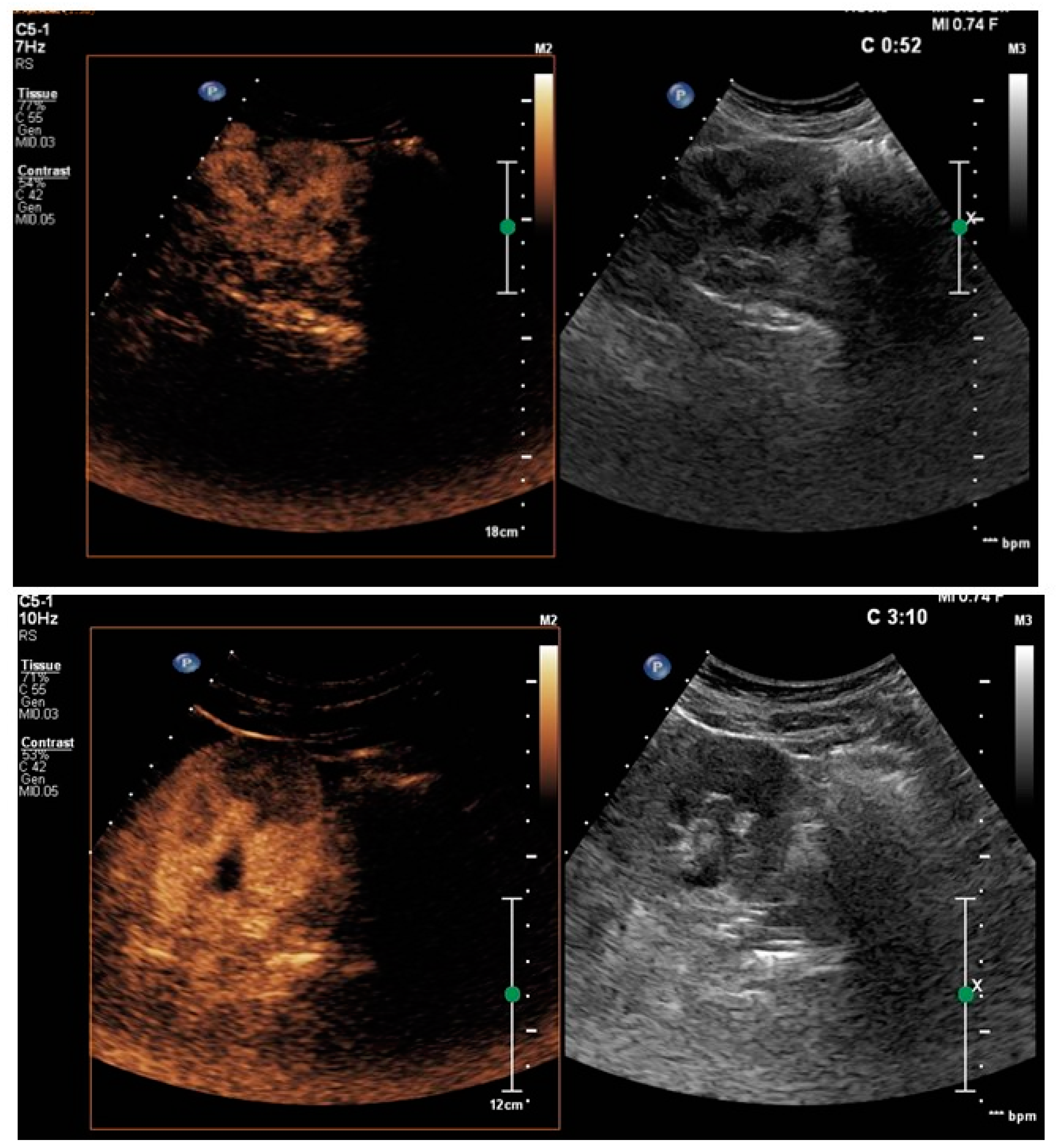
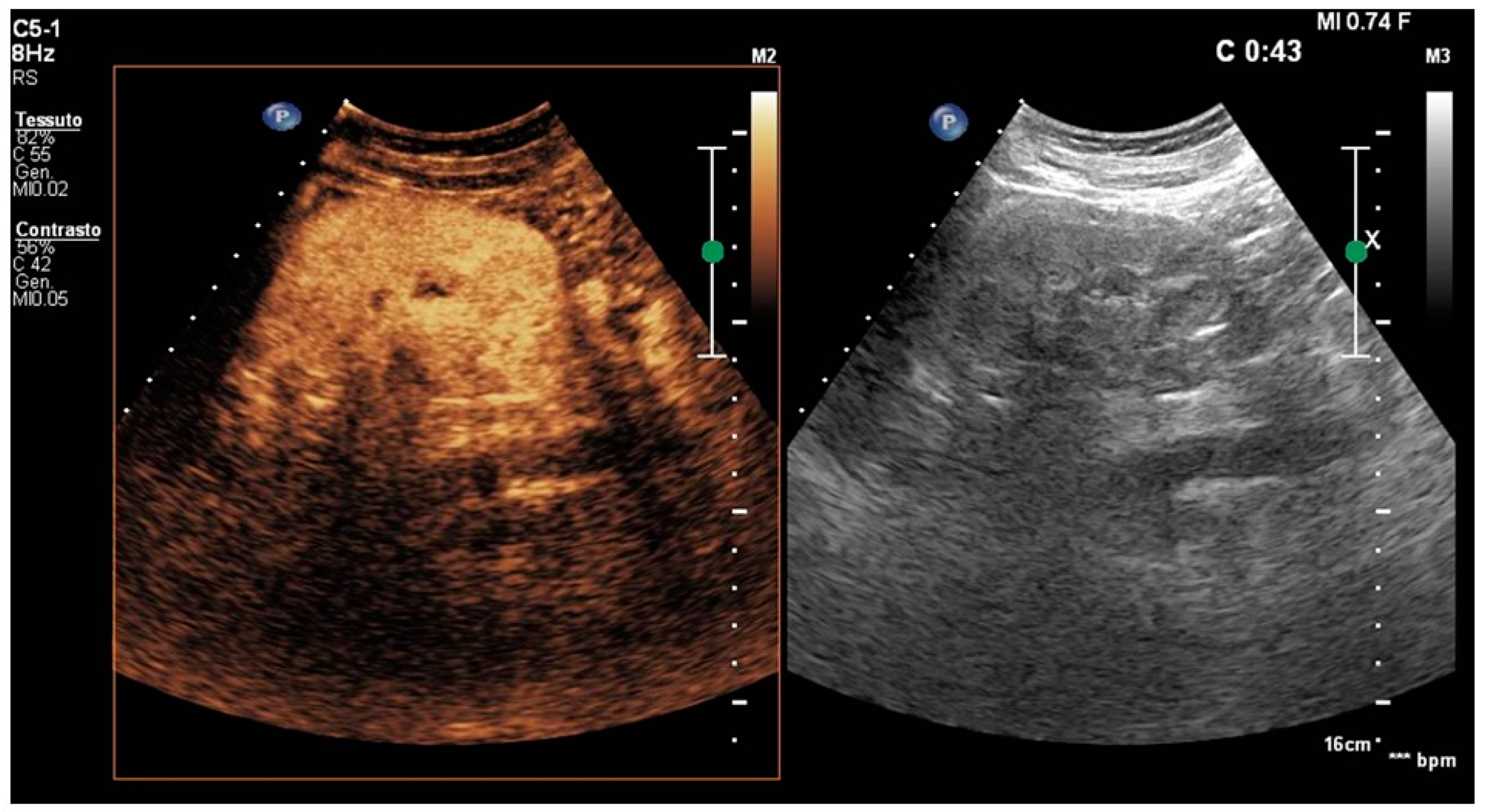
:1. Introduction
2. Materials and Methods
2.1. Ultrasound and CEUS Technique
2.2. Statistical Analysis
3. Results
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gupta, K.; Grigoryan, L.; Trautner, B. Urinary Tract Infection. Ann. Intern. Med. 2017, 167, ITC49–ITC64. [Google Scholar] [CrossRef] [PubMed]
- Foxman, B. Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. Disease-a-Month 2003, 49, 53–70. [Google Scholar] [CrossRef]
- Flores-Mireles, A.L.; Walker, J.N.; Caparon, M.; Hultgren, S.J. Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nat. Rev. Microbiol. 2015, 13, 269–284. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.R.; Russo, T.A. Acute Pyelonephritis in Adults. N. Engl. J. Med. 2018, 378, 48–59. [Google Scholar] [CrossRef] [PubMed]
- Sriman, R.; Venkatesh, K.; Mathew, C.; Pankaj, M.; Shankar, R. Validity of diffusion-weighted magnetic resonance imaging in the evaluation of acute pyelonephritis in comparison with contrast-enhanced computed tomography. Pol. J. Radiol. 2020, 85, e137–e143. [Google Scholar] [CrossRef]
- Browne, R.F.; Zwirewich, C.; Torreggiani, W.C. Imaging of urinary tract infection in the adult. Eur. Radiol. Suppl. 2004, 14 (Suppl. S3), E168–E183. [Google Scholar] [CrossRef]
- Das, C.J.; Ahmad, Z.; Sharma, S.; Gupta, A.K. Multimodality imaging of renal inflammatory lesions. World J. Radiol. 2014, 6, 865–873. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.B.; Lee, S.; Choi, Y.H.; Cheon, J.E.; Lee, S.B.; Cho, Y.J.; Ahn, Y.H.; Lim, S.H. Contrast-enhanced ultrasound for the diagnosis of acute pyelonephritis in pediatric patients with urinary tract infection: A feasibility study. PLoS ONE 2023, 18, e0284016. [Google Scholar] [CrossRef]
- Jung, H.J.; Choi, M.H.; Pai, K.S.; Kim, H.G. Diagnostic performance of contrast-enhanced ultrasound for acute pyelonephritis in children. Sci. Rep. 2020, 10, 10715. [Google Scholar] [CrossRef]
- Rinaldo, C.; Grimaldi, D.; Di Serafino, M.; Iacobellis, F.; Verde, F.; Caruso, M.; Sabatino, V.; Orabona, G.D.; Schillirò, M.L.; Vallone, G.; et al. An update on pyelonephritis: Role of contrast enhancement ultrasound (CEUS). J. Ultrasound 2023, 26, 333–342. [Google Scholar] [CrossRef]
- Granata, A.; Floccari, F.; Insalaco, M.; Clementi, A.; Di Lullo, L.; D’Amelio, A.; Zamboli, P.; Logias, F.; Romano, M.; Fiorini, F. [Ultrasound assessment in renal infections]. G. Ital. Di Nefrol. Organo Uff. Della Soc. Ital. Di Nefrol. 2012, 29 (Suppl. S57), S47–S57. [Google Scholar]
- Mitterberger, M.; Pinggera, G.M.; Colleselli, D.; Bartsch, G.; Strasser, H.; Steppan, I.; Pallwein, L.; Friedrich, A.; Gradl, J.; Frauscher, F. Acute pyelonephritis: Comparison of diagnosis with computed tomography and contrast-enhanced ultrasonography. BJU Int. 2008, 101, 341–344. [Google Scholar] [CrossRef]
- Sidhu, P.S.; Cantisani, V.; Dietrich, C.F.; Gilja, O.H.; Saftoiu, A.; Bartels, E.; Bertolotto, M.; Calliada, F.; Clevert, D.A.; Cosgrove, D.; et al. The EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound (CEUS) in Non-Hepatic Applications: Update 2017 (Long Version). Ultraschall Med.-Eur. J. Ultrasound 2018, 39, e2–e44. [Google Scholar] [CrossRef]
- Claudon, M.; Cosgrove, D.; Albrecht, T.; Bolondi, L.; Bosio, M.; Calliada, F.; Correas, J.M.; Darge, K.; Dietrich, C.; D’Onofrio, M.; et al. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS)—Update 2008. Ultraschall Med.-Eur. J. Ultrasound 2008, 29, 28–44. [Google Scholar] [CrossRef] [PubMed]
- Demertzis, J.; Menias, C.O. State of the art: Imaging of renal infections. Emerg. Radiol. 2007, 14, 13–22. [Google Scholar] [CrossRef]
- Craig, W.D.; Wagner, B.J.; Travis, M.D. Pyelonephritis: Radiologic-pathologic review. Radiographics 2008, 28, 255–277, quiz 327–328. [Google Scholar] [CrossRef] [PubMed]
- Fontanilla, T.; Minaya, J.; Cortés, C.; Hernando, C.G.; Arangüena, R.P.; Arriaga, J.; Carmona, M.S.; Alcolado, A. Acute complicated pyelonephritis: Contrast-enhanced ultrasound. Abdom. Imaging 2012, 37, 639–646. [Google Scholar] [CrossRef]
- Shigemura, K.; Ishikawa, K. AAUS guideline for acute uncomplicated pyelonephritis. J. Infect. Chemother. 2022, 28, 1092–1097. [Google Scholar] [CrossRef]
- Kang, C.I.; Kim, J.; Park, D.W.; Kim, B.N.; Ha, U.S.; Lee, S.J.; Yeo, J.K.; Min, S.K.; Lee, H.; Wie, S.H. Clinical Practice Guidelines for the Antibiotic Treatment of Community-Acquired Urinary Tract Infections. Infect. Chemother. 2018, 50, 67–100. [Google Scholar] [CrossRef]
- Yoon, C.; Park, S.Y.; Kim, B.; Kwon, K.T.; Ryu, S.Y.; Wie, S.H.; Jo, H.U.; Kim, J.; Hong, K.W.; Kim, H.I.; et al. Relationship between the appropriateness of antibiotic treatment and clinical outcomes/medical costs of patients with community-acquired acute pyelonephritis: A multicenter prospective cohort study. BMC Infect. Dis. 2022, 22, 112. [Google Scholar] [CrossRef]
- Pšeničny, E.; Glušič, M.; Pokorn, M.; Ključevšek, D. Contrast-enhanced ultrasound in detection and follow-up of focal renal infections in children. Br. J. Radiol. 2022, 95, 20220290. [Google Scholar] [CrossRef] [PubMed]

| Clinical Characteristics | Value |
|---|---|
| Age (years) | 49.2 ± 21.4 |
| Female sex | 17 (73.9%) |
| Ultrasound follow-up (days) | 23.7 ± 18.6 |
| Pyelonephritis resolution (days) | 25.9 ± 19.3 |
| WBC admission (×109/L) [3.60–10.50] | 11.3 ± 3.3 |
| CRP admission (mg/dL) [<0.50] | 15.6 ± 7.3 |
| PCT admission (ng/mL) [<0.50] | 6.4 ± 5.5 |
| WBC discharge (×109/L) [3.60–10.50] | 6.7 ± 2.1 |
| CRP discharge (mg/dL) [<0.50] | 3.0 ± 2.3 |
| PCT discharge (ng/mL) [<0.50] | 0.7 ± 0.4 |
| Characteristics of Pyelonephritis | n (%) |
|---|---|
| Monolateral | 19 (82.6%) |
| Monofocal | 14 (60.8%) |
| Multifocal | 8 (34.7%) |
| Bilateral | 4 (17.3%) |
| Nephrolithiasis | 4 (17.3%) |
| Hydronephrosis | 6 (26%) |
| Escherichia coli + urine culture | 7 (30.4%) |
| Klebsiella pneumoniae + urine culture | 2 (8.6%) |
| First diagnosis by CEUS | 10 (35.7%) |
| First diagnosis by CT | 14 (50%) |
| First diagnosis by CEUS + CT | 4 (14.2%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boccatonda, A.; Venerato, S.; D’Ardes, D.; Cocco, G.; Schiavone, C.; Vicari, S. Contrast-Enhanced Ultrasound Follow-Up for Acute Pyelonephritis Patients. Healthcare 2023, 11, 2899. https://doi.org/10.3390/healthcare11212899
Boccatonda A, Venerato S, D’Ardes D, Cocco G, Schiavone C, Vicari S. Contrast-Enhanced Ultrasound Follow-Up for Acute Pyelonephritis Patients. Healthcare. 2023; 11(21):2899. https://doi.org/10.3390/healthcare11212899
Chicago/Turabian StyleBoccatonda, Andrea, Stefano Venerato, Damiano D’Ardes, Giulio Cocco, Cosima Schiavone, and Susanna Vicari. 2023. "Contrast-Enhanced Ultrasound Follow-Up for Acute Pyelonephritis Patients" Healthcare 11, no. 21: 2899. https://doi.org/10.3390/healthcare11212899
APA StyleBoccatonda, A., Venerato, S., D’Ardes, D., Cocco, G., Schiavone, C., & Vicari, S. (2023). Contrast-Enhanced Ultrasound Follow-Up for Acute Pyelonephritis Patients. Healthcare, 11(21), 2899. https://doi.org/10.3390/healthcare11212899










