Development of a Set of Assessment Tools for Health Professionals to Design a Tailored Rehabilitation Exercise and Sports Program for People with Stroke in South Korea: A Delphi Study
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Development of a Set of Assessment Tools
2.2.1. Step 1. Literature Review
2.2.2. Step 2. Building a Draft Version of the Hierarchical Structure for Evaluation Factors and Determining Corresponding Assessment Tools for Each Evaluation Factor
2.2.3. Step 3. Determination of Evaluation Factors
2.2.4. Step 4. Determination of Assessment Tools
2.3. Expert Panel Selection
2.4. Data Analysis
3. Results
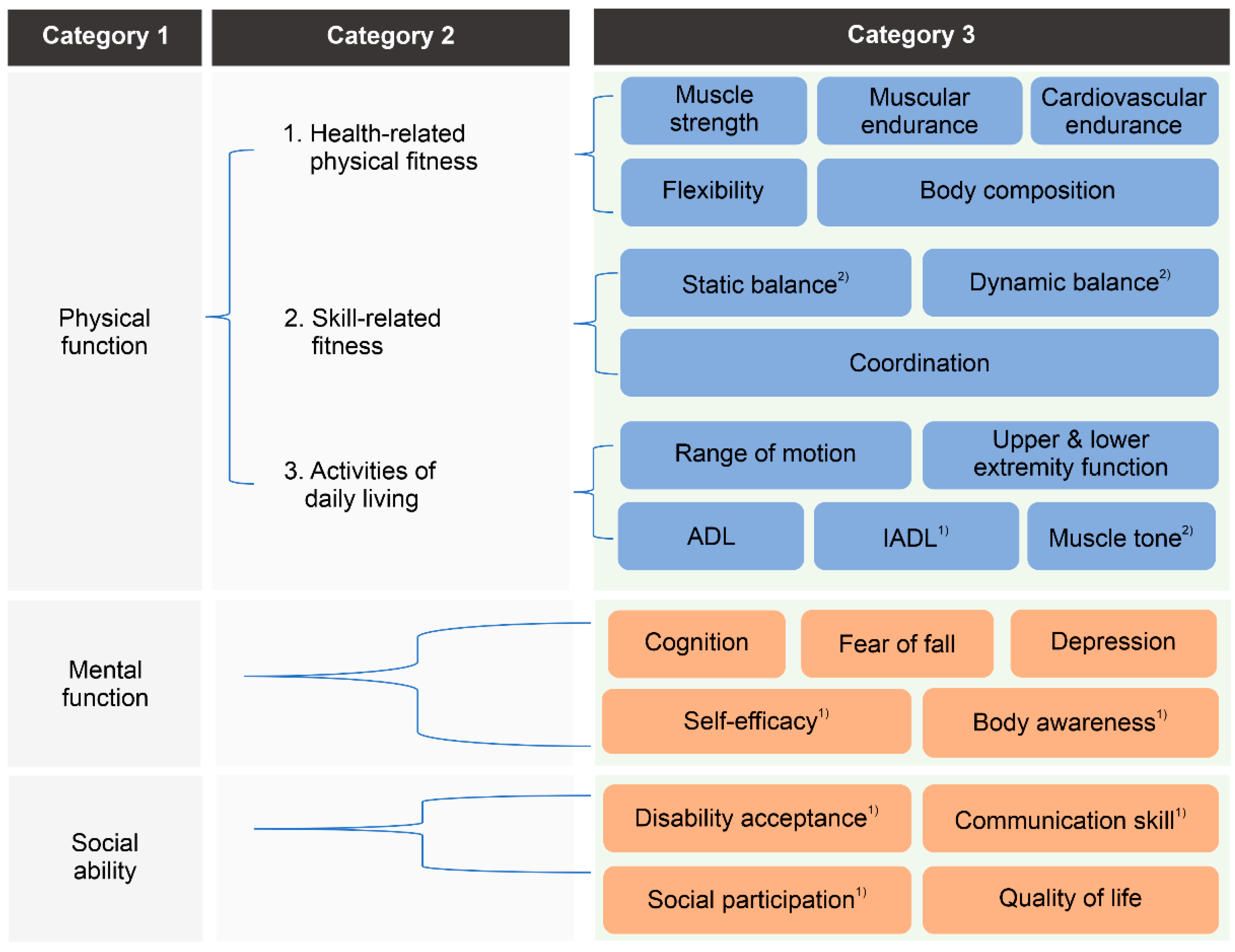
3.1. Development of a Hierarchical Structure for Evaluation Factors
3.2. Delphi Survey for the Determination of Evaluation Factors
3.3. Delphi Survey for the Determination of Assessment Tools
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Rehabilitation Center. Healthcare Project for People with Disabilities; National Rehabilitation Center: Seoul, Republic of Korea, 2017.
- National Rehabilitation Center. Healthcare Project for People with Disabilities; National Rehabilitation Center: Seoul, Republic of Korea, 2020.
- Statistics Korea. Annual Report on the Causes of Death Statistics; Statistics Korea: Daejeon, Republic of Korea, 2019.
- Mohan, K.M.; Wolfe, C.D.; Rudd, A.G.; Heuschmann, P.U.; Kolominsky-Rabas, P.L.; Grieve, A.P. Risk and cumulative risk of stroke recurrence: A systematic review and meta-analysis. Stroke 2011, 42, 1489–1494. [Google Scholar] [CrossRef] [PubMed]
- Furie, K.L.; Kasner, S.E.; Adams, R.J.; Albers, G.W.; Bush, R.L.; Fagan, S.C.; Halperin, J.L.; Johnston, S.C.; Katzan, I.; Kernan, W.N.; et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011, 42, 227–276. [Google Scholar] [CrossRef] [PubMed]
- Kopunek, S.P.; Michael, K.M.; Shaughnessy, M.; Resnick, B.; Nahm, E.S.; Whitall, J.; Goldberg, A.; Macko, R.F. Cardiovascular risk in survivors of stroke. Am. J. Prev. Med. 2007, 32, 408–412. [Google Scholar] [CrossRef] [PubMed]
- D’Isabella, N.T.; Shkredova, D.A.; Richardson, J.A.; Tang, A. Effects of exercise on cardiovascular risk factors following stroke or transient ischemic attack: A systematic review and meta-analysis. Clin. Rehabil. 2017, 31, 1561–1572. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.A.; Hallsworth, K.; Jakovljevic, D.G.; Blamire, A.M.; He, J.; Ford, G.A.; Rochester, L.; Trenell, M.I. Effects of community exercise therapy on metabolic, brain, physical, and cognitive function following stroke: A randomized controlled pilot trial. Neurorehabil. Neural Repair. 2015, 29, 623–635. [Google Scholar] [CrossRef] [PubMed]
- Ramas, J.; Courbon, A.; Roche, F.; Bethoux, F.; Calmels, P. Effect of training programs and exercise in adult stroke patients: Literature review. Ann. Readapt. Med. Phys. 2007, 50, 438–444. [Google Scholar] [CrossRef]
- Cramp, M.C.; Greenwood, R.J.; Gill, M.; Lehmann, A.; Rothwell, J.C.; Scott, O.M. Effectiveness of a community-based low intensity exercise programme for ambulatory stroke survivors. Disabil. Rehabil. 2010, 32, 239–247. [Google Scholar] [CrossRef]
- Pang, M.Y.C.; Eng, J.J.; Dawson, A.S.; McKay, H.A.; Harris, J.E. A community-based fitness and mobility exercise program for older adults with chronic stroke: A randomized, controlled trial. J. Am. Geriatr. Soc. 2005, 53, 1667–1674. [Google Scholar] [CrossRef]
- Dean, C.M.; Rissel, C.; Sherrington, C.; Sharkey, M.; Cumming, R.G.; Lord, S.R.; Barker, R.N.; Kirkham, C.; O’Rourke, S. Exercise to enhance mobility and prevent falls after stroke: The community stroke club randomized trial. Neurorehabil. Neural Repair. 2012, 26, 1046–1057. [Google Scholar] [CrossRef]
- Mudge, S.; Barber, P.A.; Stott, N.S. Circuit-based rehabilitation improves gait endurance but not usual walking activity in chronic stroke: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2009, 90, 1989–1996. [Google Scholar] [CrossRef]
- Liu-Ambrose, T.; Eng, J.J. Exercise training and recreational activities to promote executive functions in chronic stroke: A proof-of-concept study. J. Stroke Cerebrovasc. Dis. 2015, 24, 130–137. [Google Scholar] [CrossRef]
- Ministry of Culture, Sports and Tourism. National Sport Participation Survey in Korea 2021. Available online: https://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=1658 (accessed on 16 December 2022).
- Kang, J.H.; Bae, H.J.; Choi, Y.A.; Lee, S.H.; Shin, H.I. Length of hospital stay after stroke: A Korean nationwide study. Ann. Rehabil. Med. 2016, 40, 675–681. [Google Scholar] [CrossRef] [PubMed]
- Korean Law Information Center. Act on the Guarantee of Health Rights and Access To. Medical Care for Disabled Persons. 2021. Available online: https://www.law.go.kr/lsInfoP.do?lsiSeq=249313&efYd=20230929#0000 (accessed on 20 November 2023).
- Sekhar, P.K.C.; Madhavi, K.; Srikumari, V. Efficacy of isokinetic strength training and balance exercises on lower limb muscles in subjects with stroke. Int. J. Physiother. Res. 2013, 7, 25–29. [Google Scholar] [CrossRef]
- Denissen, S.; Staring, W.; Kunkel, D.; Pickering, R.M.; Lennon, S.; Geurts, A.C.; Weerdesteyn, V.; Verheyden, G.S. Interventions for preventing falls in people after stroke. Cochrane Database Syst. Rev. 2019. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.; Tabassum, D.; Baig, S.S.; Moyle, B.; Redgrave, J.; Nichols, S.; McGregor, G.; Evans, K.; Totton, N.; Cooper, C.; et al. Effect of exercise interventions on health-related quality of life after stroke and transient ischemic attack: A systematic review and meta-analysis. Stroke 2021, 52, 2445–2455. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.B.; Kang, K.Y. The effects of isokinetic eccentric resistance exercise for the hip joint on functional gait of stroke patients. J. Phys. Ther. Sci. 2013, 25, 1177–1179. [Google Scholar] [CrossRef] [PubMed]
- Marzolini, S.; Tang, A.; McIlroy, W.; Oh, P.I.; Brooks, D. Outcomes in people after stroke attending an adapted cardiac rehabilitation exercise program: Does time from stroke make a difference? J. Stroke Cerebrovasc. Dis. 2014, 23, 1648–1656. [Google Scholar] [CrossRef]
- Vanderbeken, I.; Kerckhofs, E. A systematic review of the effect of physical exercise on cognition in stroke and traumatic brain injury patients. NeuroRehabilitation 2017, 40, 33–48. [Google Scholar] [CrossRef] [PubMed]
- Sherrington, C.; Fairhall, N.J.; Wallbank, G.K.; Tiedemann, A.; Michaleff, Z.A.; Howard, K.; Clemson, L.; Hopewell, S.; Lamb, S.E. Exercise for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2019, 1, CD012424. [Google Scholar] [CrossRef]
- Alhwoaimel, N.; Turk, R.; Warner, M.; Verheyden, G.; Thijs, L.; Wee, S.K.; Hughes, A.M. Do trunk exercises improve trunk and upper extremity performance, post stroke? A systematic review and meta-analysis. NeuroRehabilitation 2018, 43, 395–412. [Google Scholar] [CrossRef]
- Bastos, V.S.; Martins, J.C.; de Morais Faria, C.D.C. Preferência de exercícios de indivíduos acometidos pelo acidente vascular cerebral usuários da atenção básica de saúde. Fisioter. Pesqui. 2021, 28, 261–266. [Google Scholar] [CrossRef]
- Lee, J.; Jeon, J.; Lee, D.; Hong, J.; Yu, J.; Kim, J. Effect of trunk stabilization exercise on abdominal muscle thickness, balance and gait abilities of patients with hemiplegic stroke: A randomized controlled trial. NeuroRehabilitation 2020, 47, 435–442. [Google Scholar] [CrossRef]
- Marzolini, S.; Oh, P.; Corbett, D.; Dooks, D.; Calouro, M.; MacIntosh, B.J.; Goodman, R.; Brooks, D. Prescribing aerobic exercise intensity without a cardiopulmonary exercise test post stroke: Utility of the six-minute walk test. J. Stroke Cerebrovasc. Dis. 2016, 25, 2222–2231. [Google Scholar] [CrossRef]
- Park, J.S.; Lee, G.; Choi, J.B.; Hwang, N.K.; Jung, Y.J. Game-based hand resistance exercise versus traditional manual hand exercises for improving hand strength, motor function, and compliance in stroke patients: A multi-center randomized controlled study. NeuroRehabilitation 2019, 45, 221–227. [Google Scholar] [CrossRef]
- Wonsetler, E.C.; Bowden, M.G. A systematic review of mechanisms of gait speed change post-stroke. Part 2: Exercise capacity, muscle activation, kinetics, and kinematics. Top. Stroke Rehabil. 2017, 24, 394–403. [Google Scholar] [CrossRef] [PubMed]
- English, C.; Hillier, S.L.; Lynch, E.A. Circuit class therapy for improving mobility after stroke. Cochrane Database Syst. Rev. 2017, 6, CD007513. [Google Scholar] [CrossRef] [PubMed]
- Pollock, A.; Gray, C.; Culham, E.; Durward, B.R.; Langhorne, P. Interventions for improving sit-to-stand ability following stroke. Cochrane Database Syst. Rev. 2014, 2014, CD007232. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Gonzalo, R.; Fernandez-Gonzalo, S.; Turon, M.; Prieto, C.; Tesch, P.A.; García-Carreira, M.d.C. Muscle, functional and cognitive adaptations after flywheel resistance training in stroke patients: A pilot randomized controlled trial. J. Neuroeng. Rehabil. 2016, 13, 37. [Google Scholar] [CrossRef]
- Ghasemi, E.; Khademi-Kalantari, K.; Khalkhali-Zavieh, M.; Rezasoltani, A.; Ghasemi, M.; Baghban, A.A.; Ghasemi, M. The effect of functional stretching exercises on functional outcomes in spastic stroke patients: A randomized controlled clinical trial. J. Bodyw. Mov. Ther. 2018, 22, 1004–1012. [Google Scholar] [CrossRef]
- Haruyama, K.; Kawakami, M.; Otsuka, T. Effect of core stability training on trunk function, standing balance, and mobility in stroke patients. Neurorehabil. Neural Repair. 2017, 31, 240–249. [Google Scholar] [CrossRef]
- Johar, M.N.; Mohd Nordin, N.A.; Abdul Aziz, A.F. The effect of game-based in comparison to conventional circuit exercise on functions, motivation level, self-efficacy and quality of life among stroke survivors. Medicine 2022, 101, e28580. [Google Scholar] [CrossRef] [PubMed]
- Rose, D.K.; Nadeau, S.E.; Wu, S.S.; Tilson, J.K.; Dobkin, B.H.; Pei, Q.; Duncan, P.W. Locomotor training and strength and balance exercises for walking recovery after stroke: Response to number of training sessions. Phys. Ther. 2017, 97, 1066–1074. [Google Scholar] [CrossRef] [PubMed]
- van Duijnhoven, H.J.; Heeren, A.; Peters, M.A.; Veerbeek, J.M.; Kwakkel, G.; Geurts, A.C.; Weerdesteyn, V. Effects of exercise therapy on balance capacity in chronic stroke: Systematic review and meta-analysis. Stroke 2016, 47, 2603–2610. [Google Scholar] [CrossRef]
- Treger, I.; Landesman, C.; Tabacaru, E.; Kalichman, L. Influence of home-based exercises on walking ability and function of post-stroke individuals. Int. J. Ther. Rehabil. 2014, 21, 441–446. [Google Scholar] [CrossRef]
- Park, J.H.; Shin, J.H.; Lee, H.; Roh, J.; Park, H.S. Alterations in intermuscular coordination underlying isokinetic exercise after a stroke and their implications on neurorehabilitation. J. Neuroeng. Rehabil. 2021, 18, 110. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.C.; Chuang, C.Y.; Leong, C.P.; Wang, L.; Chen, H.L.; Chiang, C.W. Effect of comprehensive postural instructions and range of motion exercises via educational videos on motor function and shoulder injury in stroke patients with hemiplegia: A preliminary study. J. Manip. Physiol. Ther. 2018, 41, 665–671. [Google Scholar] [CrossRef]
- Zondervan, D.K.; Friedman, N.; Chang, E.; Zhao, X.; Augsburger, R.; Reinkensmeyer, D.J.; Cramer, S.C. Home-based hand rehabilitation after chronic stroke: Randomized, controlled single-blind trial comparing the MusicGlove with a conventional exercise program. J. Rehabil. Res. Dev. 2016, 53, 457–472. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Liu, Y.; Yu, J.; Zhang, Q.; Wang, X.; Zhang, Y.; Gao, Y.; Ye, L. Exercise interventions for post-stroke depression: A protocol for systematic review and meta-analysis. Medicine 2021, 100, e24945. [Google Scholar] [CrossRef]
- Grau-Pellicer, M.; Chamarro-Lusar, A.; Medina-Casanovas, J.; Serdà Ferrer, B.C. Walking speed as a predictor of community mobility and quality of life after stroke. Top. Stroke Rehabil. 2019, 26, 349–358. [Google Scholar] [CrossRef]
- Yousuf, M.I. Using experts’ opinions through Delphi technique. Pract. Assess. Res. Eval. 2007, 12, 4. [Google Scholar]
- Chesbrough, H. Open Business Models: How to Thrive in the New Innovation Landscape; Harvard Business Press: Boston, MA, USA, 2006. [Google Scholar]
- Baek, S.; Kim, S. Participatory public service design by Gov.3.0 Design Group. Sustainability 2018, 10, 245. [Google Scholar] [CrossRef]
- Palinkas, L.A.; Horwitz, S.M.; Green, C.A.; Wisdom, J.P.; Duan, N.; Hoagwood, K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation Research. Adm. Policy Ment. Health 2015, 42, 533–544. [Google Scholar] [CrossRef] [PubMed]
- Corbin, C.B.; Pangrazi, R.P.; Franks, B.D. Definitions: Health, Fitness, and Physical Activity; President’s Council on Physical Fitness and Sports Research Digest: Washington, DC, USA, 2000. [Google Scholar]
- World Health Organization. Towards a Common Language for Functioning, Disability, and Health ICF; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Stier-Jarmer, M.; Grill, E.; Ewert, T.; Bartholomeyczik, S.; Finger, M.; Mokrusch, T.; Kostanjsek, N.; Stucki, G. ICF Core Set for patients with neurological conditions in early post-acute rehabilitation facilities. Disabil. Rehabil. 2009, 27, 1464–5165. [Google Scholar] [CrossRef]
- Hong, S.J.; Goh, E.Y.; Chua, S.Y.; Ng, S.S. Reliability and Validity of Step Test Scores in Subjects With Chronic Stroke. Arch. Phys. Med. Rehabil. 2012, 93, 1065–1071. [Google Scholar] [CrossRef] [PubMed]
- Tsang, Y.L.; Mak, M.K. Sit-and-reach test can predict mobility of patients recovering from acute stroke. Arch. Phys. Med. Rehabil. 2004, 85, 94–98. [Google Scholar] [CrossRef]
- Hafsteinsdottir, T.B.; Rensink, M.; Schuurmans, M. Clinimetric Properties of the Timed Up and Go Test for Patients With Stroke: A Systematic Review. Top. Stroke Rehabil. 2014, 21, 197–210. [Google Scholar] [CrossRef]

| n | Major | Position | ID | Degree | Major Field Experience (Year) |
|---|---|---|---|---|---|
| 1 | Rehabilitation Medicine | Professor | W1 | MD | 27 |
| 2 | Rehabilitation Medicine | Professor | W2 | MD | 24 |
| 3 | Rehabilitation Medicine | Professor | W3 | MD | 16 |
| 4 | Sports Medicine | Professor | W4 | PhD | 25 |
| 5 | Sports Medicine | Instructor | W5 | MS | 18 |
| 6 | Kinesiology | Professor | W6 | PhD | 30 |
| 7 | Kinesiology | Professor | W7 | PhD | 23 |
| 8 | Kinesiology | Professor | W8 | PhD | 18 |
| 9 | Kinesiology | Professor | W9 | PhD | 25 |
| 10 | Kinesiology | Professor | W10 | PhD | 15 |
| 11 | Kinesiology | Professor | W11 | PhD | 27 |
| 12 | Kinesiology | Instructor | W12 | MS | 25 |
| 13 | Kinesiology | Instructor | W13 | MS | 24 |
| 14 | Special Physical Education | Professor | W14 | PhD | 32 |
| 15 | Special Physical Education | Professor | W15 | PhD | 20 |
| 16 | Special Physical Education | Professor | W16 | PhD | 25 |
| 17 | Special Physical Education | Senior researcher | W17 | PhD | 20 |
| 18 | Physical Therapy | Professor | W18 | PhD | 15 |
| 19 | Physical Therapy | Professor | W19 | PhD | 20 |
| 20 | Physical Therapy | Professor | W20 | PhD | 40 |
| Evaluation Factors | Mean | SD | I-CVI | CV | ||
|---|---|---|---|---|---|---|
| Physical function | Health-related factors | Muscle strength | 4.6 | 0.49 | 1 | 0.11 |
| Muscular endurance | 4.3 | 0.56 | 0.95 | 0.13 | ||
| Cardiovascular endurance | 4.1 | 0.62 | 0.85 | 0.15 | ||
| Flexibility | 4.35 | 0.73 | 0.85 | 0.17 | ||
| Body composition | 4.1 | 0.70 | 0.8 | 0.17 | ||
| Skill-related factors | Static balance | 4.6 | 0.49 | 1 | 0.11 | |
| Dynamic balance | 4.8 | 0.40 | 1 | 0.08 | ||
| Coordination | 4.7 | 0.46 | 1 | 0.10 | ||
| ADL-related factors | Range of motion | 4.55 | 0.50 | 1 | 0.11 | |
| Upper & lower extremity function | 4.75 | 0.43 | 1 | 0.09 | ||
| Muscle tone | 4.3 | 0.71 | 0.85 | 0.17 | ||
| ADL | 4.7 | 0.46 | 1 | 0.10 | ||
| IADL | 4.35 | 0.57 | 0.95 | 0.13 | ||
| Mental function | Cognition | 4.5 | 0.67 | 0.9 | 0.15 | |
| Depression | 4.15 | 0.65 | 0.85 | 0.16 | ||
| Fear of falling | 4.45 | 0.67 | 0.9 | 0.15 | ||
| Self -efficacy | 4.45 | 0.74 | 0.85 | 0.17 | ||
| Body awareness | 4.4 | 0.73 | 0.85 | 0.17 | ||
| Social ability | Disability acceptance | 4.4 | 0.58 | 0.95 | 0.13 | |
| Communication skill | 4.4 | 0.66 | 0.9 | 0.15 | ||
| Social participation | 4.45 | 0.59 | 0.95 | 0.13 | ||
| Quality of life | 4.65 | 0.57 | 0.95 | 0.12 | ||
| Evaluation Factors | Assessment Tools | Mean | SD | I-CVI | CV | ||||
|---|---|---|---|---|---|---|---|---|---|
| Importance | Feasibility | Importance | Feasibility | Importance | Feasibility | Importance | Feasibility | ||
| I. Physical function: Health-related factors | |||||||||
| 1. Muscle strength | [M] Manual muscle test | 4.42 | 4.26 | 0.67 | 0.64 | 0.85 | 0.85 | 0.15 | 0.15 |
| [M] Isometric muscle test | 3.26 | 3.11 | 0.71 | 0.64 | 0.4 | 0.25 | 0.22 | 0.21 | |
| [I] Dynamometer | 3.53 | 3.47 | 0.68 | 0.68 | 0.6 | 0.55 | 0.19 | 0.20 | |
| [I] Back muscle dynamometer | 2.89 | 2.68 | 0.55 | 0.46 | 0.1 | 0 | 0.19 | 0.17 | |
| [I] 1-repetition maximum | 2.68 | 2.63 | 0.73 | 0.67 | 0.1 | 0.05 | 0.27 | 0.25 | |
| 2. Muscular endurance | [M] Step test | 3.32 | 3.21 | 0.73 | 0.69 | 0.45 | 0.35 | 0.22 | 0.22 |
| [M] Step-box test | 2.84 | 2.53 | 0.49 | 0.50 | 0.05 | 0 | 0.17 | 0.20 | |
| [M] 30 s chair stand test | 3.79 | 3.53 | 0.69 | 0.60 | 0.7 | 0.55 | 0.18 | 0.17 | |
| 3. Cardiovascular endurance | [M] 6 min walk test | 3.68 | 3.58 | 0.73 | 0.75 | 0.6 | 0.5 | 0.20 | 0.21 |
| [M] Pacer test (20 m) | 2.68 | 2.42 | 0.57 | 0.67 | 0 | 0 | 0.21 | 0.28 | |
| [I] Treadmill test | 2.79 | 2.53 | 0.77 | 0.68 | 0.15 | 0.05 | 0.27 | 0.27 | |
| [I] Ergometer test | 3.11 | 2.89 | 0.72 | 0.55 | 0.3 | 0.1 | 0.23 | 0.19 | |
| [I] FVC, FEV1 | 4.05 | 4.00 | 0.51 | 0.46 | 0.85 | 0.85 | 0.13 | 0.11 | |
| [I] Power breathe | 3.79 | 3.74 | 0.52 | 0.55 | 0.7 | 0.65 | 0.14 | 0.15 | |
| 4. Flexibility | [M] Sit-and-reach test | 3.37 | 3.32 | 0.67 | 0.65 | 0.45 | 0.4 | 0.20 | 0.20 |
| [M] Trunk forward flexion test | 2.84 | 2.63 | 0.81 | 0.74 | 0.2 | 0.1 | 0.29 | 0.28 | |
| [M] Shoulder flexibility test | 3.74 | 3.68 | 0.55 | 0.65 | 0.65 | 0.55 | 0.15 | 0.18 | |
| 5. Body composition | [I] Skinfold technique | 3.21 | 3.21 | 0.83 | 0.83 | 0.3 | 0.3 | 0.26 | 0.26 |
| [I] Body composition analyzer | 4.11 | 4.21 | 0.55 | 0.61 | 0.85 | 0.85 | 0.13 | 0.15 | |
| [M] Body mass index | 3.79 | 3.89 | 0.61 | 0.64 | 0.65 | 0.7 | 0.16 | 0.16 | |
| I. Physical function: Skill-related factors | |||||||||
| 6. Static balance | [M] Functional reach test | 4.37 | 4.32 | 0.58 | 0.57 | 0.9 | 0.9 | 0.13 | 0.13 |
| 7. Dynamic balance | [M] Timed up and go | 4.37 | 4.26 | 0.81 | 0.78 | 0.75 | 0.75 | 0.19 | 0.18 |
| [M] Berg balance scale | 4.32 | 4.21 | 0.65 | 0.69 | 0.85 | 0.8 | 0.15 | 0.16 | |
| [M] Tinetti test | 3.68 | 3.63 | 0.73 | 0.67 | 0.6 | 0.5 | 0.20 | 0.18 | |
| [M] Short physical performance battery | 3.79 | 3.68 | 0.61 | 0.65 | 0.65 | 0.55 | 0.16 | 0.18 | |
| [M] 4-square step test | 3.21 | 3.21 | 0.61 | 0.61 | 0.3 | 0.3 | 0.19 | 0.19 | |
| 8. Coordination | [M] Trunk impairment scale | 4.21 | 4.05 | 0.52 | 0.51 | 0.9 | 0.85 | 0.12 | 0.13 |
| [I] Force plate measurements | 4.00 | 3.84 | 0.56 | 0.67 | 0.8 | 0.75 | 0.14 | 0.17 | |
| [M] Postural assessment scale for stroke | 4.21 | 4.11 | 0.69 | 0.55 | 0.8 | 0.85 | 0.16 | 0.13 | |
| I. Physical function: ADL-related factors | |||||||||
| 9. Range of motion | [I] Goniometer | 4.58 | 4.47 | 0.49 | 0.50 | 0.95 | 0.95 | 0.11 | 0.11 |
| 10. Upper & lower extremity function | [M] Motor assessment scale | 4.42 | 4.32 | 0.67 | 0.65 | 0.85 | 0.85 | 0.15 | 0.15 |
| [I] Jebsen—Taylor hand function test | 4.32 | 3.89 | 0.57 | 0.64 | 0.9 | 0.7 | 0.13 | 0.16 | |
| [M] Manual function test | 4.26 | 4.21 | 0.55 | 0.52 | 0.9 | 0.9 | 0.13 | 0.12 | |
| [I] Grooved pegboard test | 3.63 | 3.47 | 0.67 | 0.68 | 0.5 | 0.35 | 0.18 | 0.20 | |
| [I] Box and block test | 4.05 | 4.00 | 0.76 | 0.79 | 0.7 | 0.65 | 0.19 | 0.20 | |
| [M] Fugl—Meyer assessment | 4.16 | 3.58 | 0.67 | 0.82 | 0.8 | 0.55 | 0.16 | 0.23 | |
| 11. Muscle tone | [M] Modified Ashworth scale | 4.53 | 4.21 | 0.50 | 0.69 | 0.95 | 0.9 | 0.11 | 0.16 |
| 12. ADL | [S] Functional independence measure | 4.42 | 3.79 | 0.59 | 0.77 | 0.9 | 0.75 | 0.13 | 0.20 |
| [S] Modified Bathel index | 4.32 | 4.00 | 0.57 | 0.73 | 0.9 | 0.8 | 0.13 | 0.18 | |
| 13. IADL | [S] K-IADL | 4.37 | 4.16 | 0.48 | 0.49 | 0.95 | 0.9 | 0.11 | 0.12 |
| Ⅱ. Mental function | |||||||||
| 14. Cognition | [S] Mini-mental status examination | 4.47 | 4.32 | 0.50 | 0.57 | 0.95 | 0.9 | 0.11 | 0.13 |
| [S] Korean version of Montreal cognitive assessment | 4.05 | 3.89 | 0.60 | 0.64 | 0.8 | 0.7 | 0.15 | 0.16 | |
| 15. Depression | [S] Geriatric depression scale short form | 3.74 | 3.63 | 0.71 | 0.67 | 0.55 | 0.5 | 0.19 | 0.18 |
| [S] Patient health questionnaire | 4.32 | 4.11 | 0.65 | 0.55 | 0.85 | 0.85 | 0.15 | 0.13 | |
| [S] Beck depression inventory | 4.05 | 3.79 | 0.69 | 0.69 | 0.75 | 0.6 | 0.17 | 0.18 | |
| 16. Self-efficacy | [S] Self efficacy questionnaire | 4.53 | 4.26 | 0.50 | 0.44 | 0.95 | 0.95 | 0.11 | 0.10 |
| 17. Fear of fall | [S] Fear of falling questionnaire | 4.42 | 4.26 | 0.59 | 0.55 | 0.9 | 0.9 | 0.13 | 0.13 |
| [S] Falls efficacy scale—International | 4.21 | 3.95 | 0.41 | 0.39 | 0.95 | 0.85 | 0.10 | 0.10 | |
| 18. Body awareness | [S] Body awareness questionnaire | 4.42 | 4.05 | 0.49 | 0.60 | 0.95 | 0.9 | 0.11 | 0.15 |
| Ⅲ. Social ability | |||||||||
| 19. Disability acceptance | [S] Disability acceptance scale | 4.58 | 4.32 | 0.49 | 0.46 | 0.95 | 0.95 | 0.11 | 0.11 |
| 20. Communication skill | [S] Holden communication scale | 4.47 | 4.26 | 0.60 | 0.55 | 0.9 | 0.9 | 0.13 | 0.13 |
| 21. Social participation | [S] Participation in social activities and environmental factors | 4.47 | 4.26 | 0.50 | 0.44 | 0.95 | 0.95 | 0.11 | 0.10 |
| 22. Quality of life | [S] EQ-5D | 4.26 | 4.26 | 0.78 | 0.64 | 0.75 | 0.85 | 0.18 | 0.15 |
| [S] WHO quality of life | 4.42 | 4.21 | 0.49 | 0.41 | 0.95 | 0.95 | 0.11 | 0.10 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, M.; Park, Y.; Eun, S.-D.; Ho, S.H. Development of a Set of Assessment Tools for Health Professionals to Design a Tailored Rehabilitation Exercise and Sports Program for People with Stroke in South Korea: A Delphi Study. Healthcare 2023, 11, 3031. https://doi.org/10.3390/healthcare11233031
Lee M, Park Y, Eun S-D, Ho SH. Development of a Set of Assessment Tools for Health Professionals to Design a Tailored Rehabilitation Exercise and Sports Program for People with Stroke in South Korea: A Delphi Study. Healthcare. 2023; 11(23):3031. https://doi.org/10.3390/healthcare11233031
Chicago/Turabian StyleLee, Minyoung, Yoon Park, Seon-Deok Eun, and Seung Hee Ho. 2023. "Development of a Set of Assessment Tools for Health Professionals to Design a Tailored Rehabilitation Exercise and Sports Program for People with Stroke in South Korea: A Delphi Study" Healthcare 11, no. 23: 3031. https://doi.org/10.3390/healthcare11233031
APA StyleLee, M., Park, Y., Eun, S.-D., & Ho, S. H. (2023). Development of a Set of Assessment Tools for Health Professionals to Design a Tailored Rehabilitation Exercise and Sports Program for People with Stroke in South Korea: A Delphi Study. Healthcare, 11(23), 3031. https://doi.org/10.3390/healthcare11233031





