Technology-Assisted Upper Limb Therapy (TAULT): Evaluation of Clinical Practice at a Specialised Centre for Spinal Cord Injury in Switzerland
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Sample
2.2. Technology-Assisted Upper Limb Therapy (TAULT)
2.3. Goals
2.3.1. Body Function
2.3.2. ADL Goals
2.4. Manual Muscle Testing
2.5. Data Analysis
3. Results
3.1. Demographics
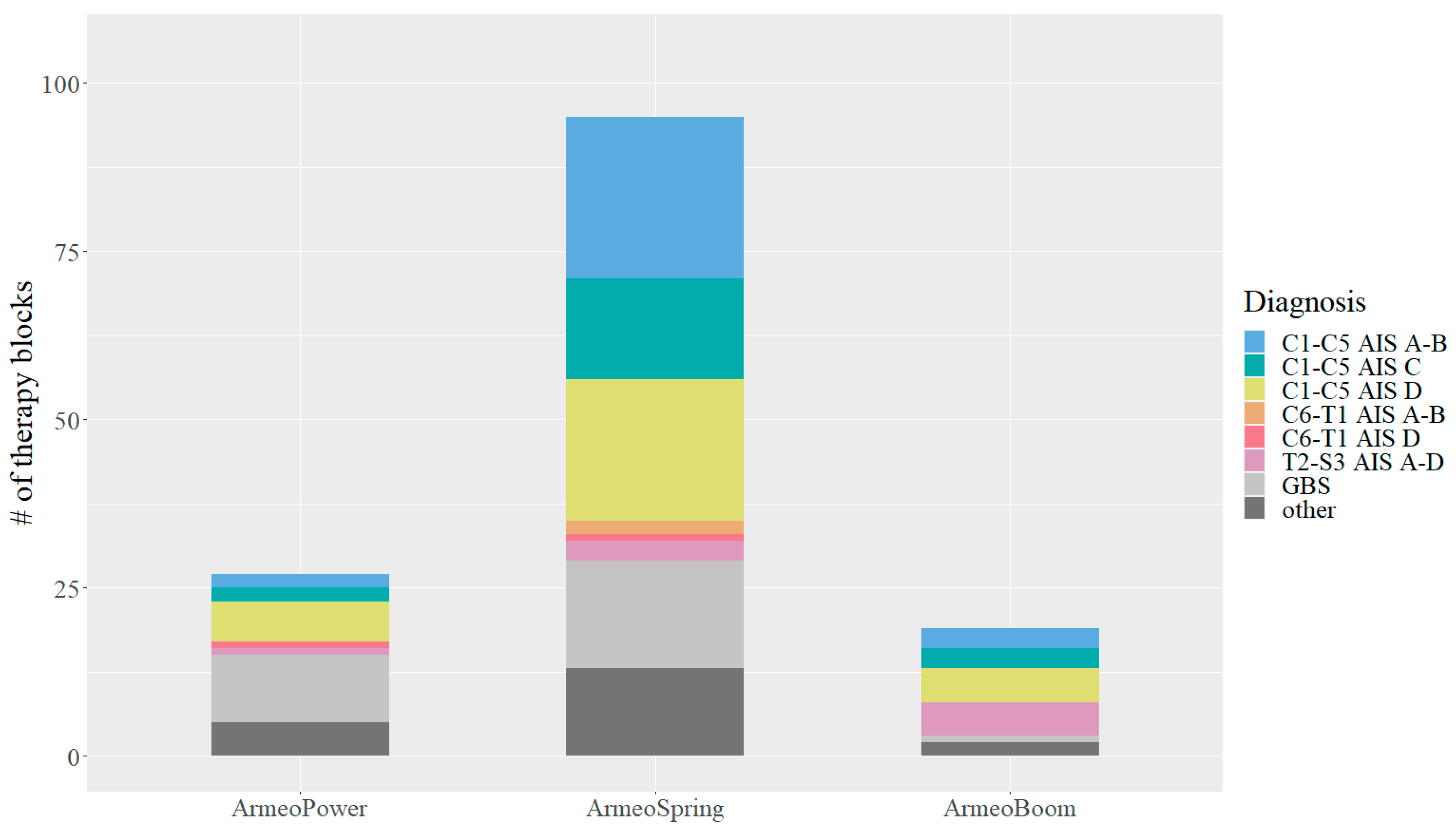
3.2. Technology-Assisted Upper Limb Therapy (TAULT)
3.3. Goals
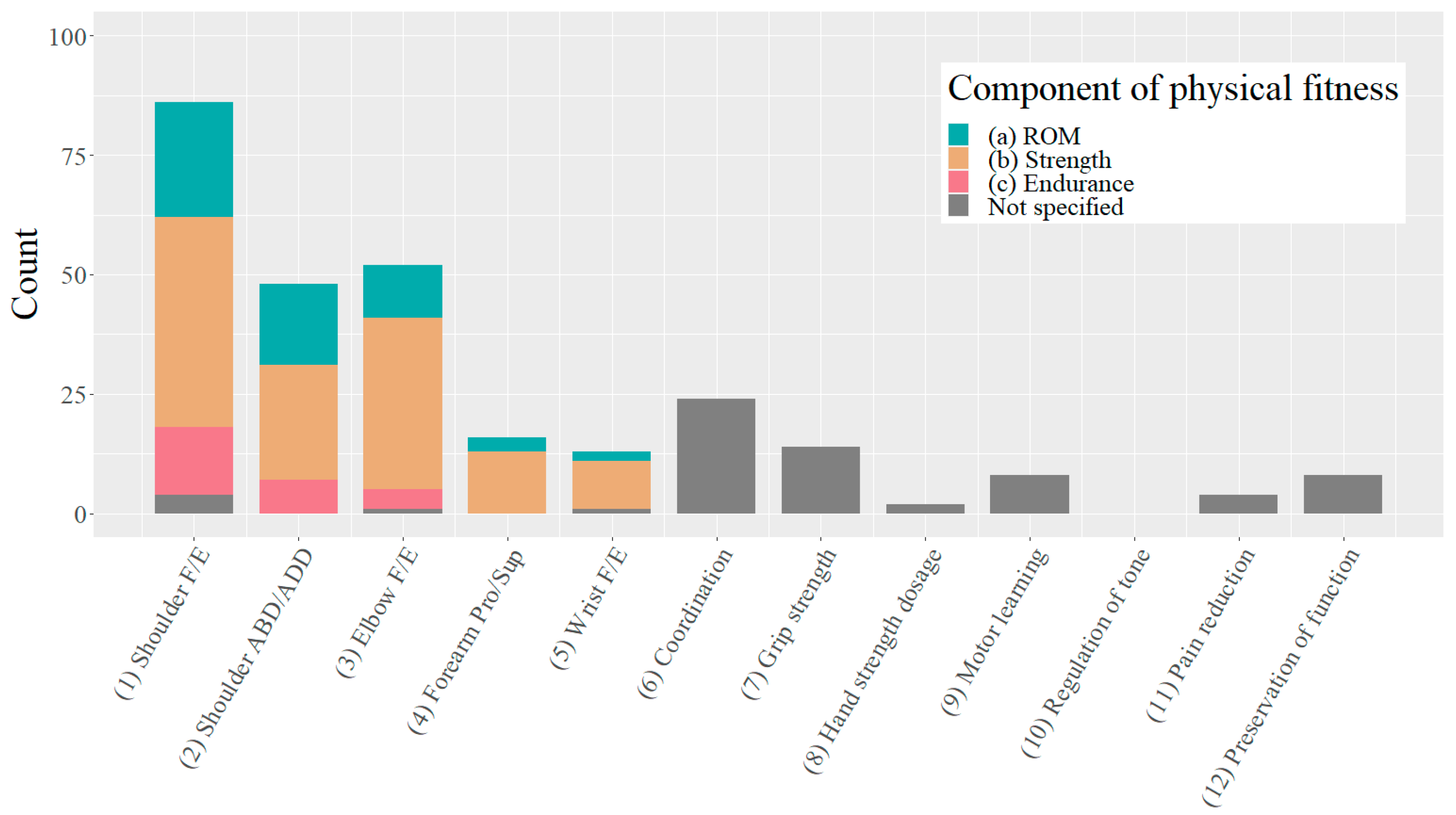
3.3.1. Body Functions
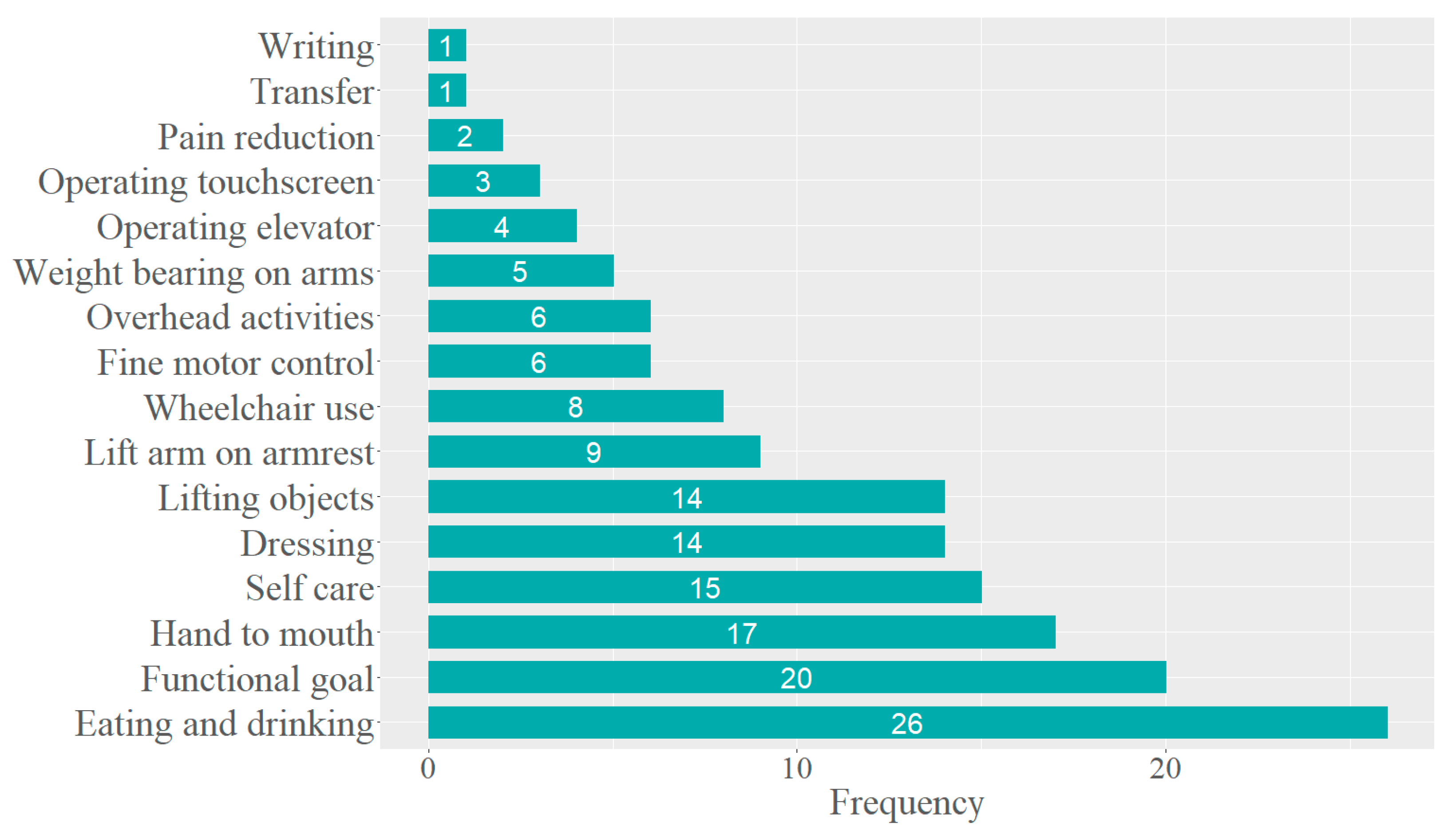
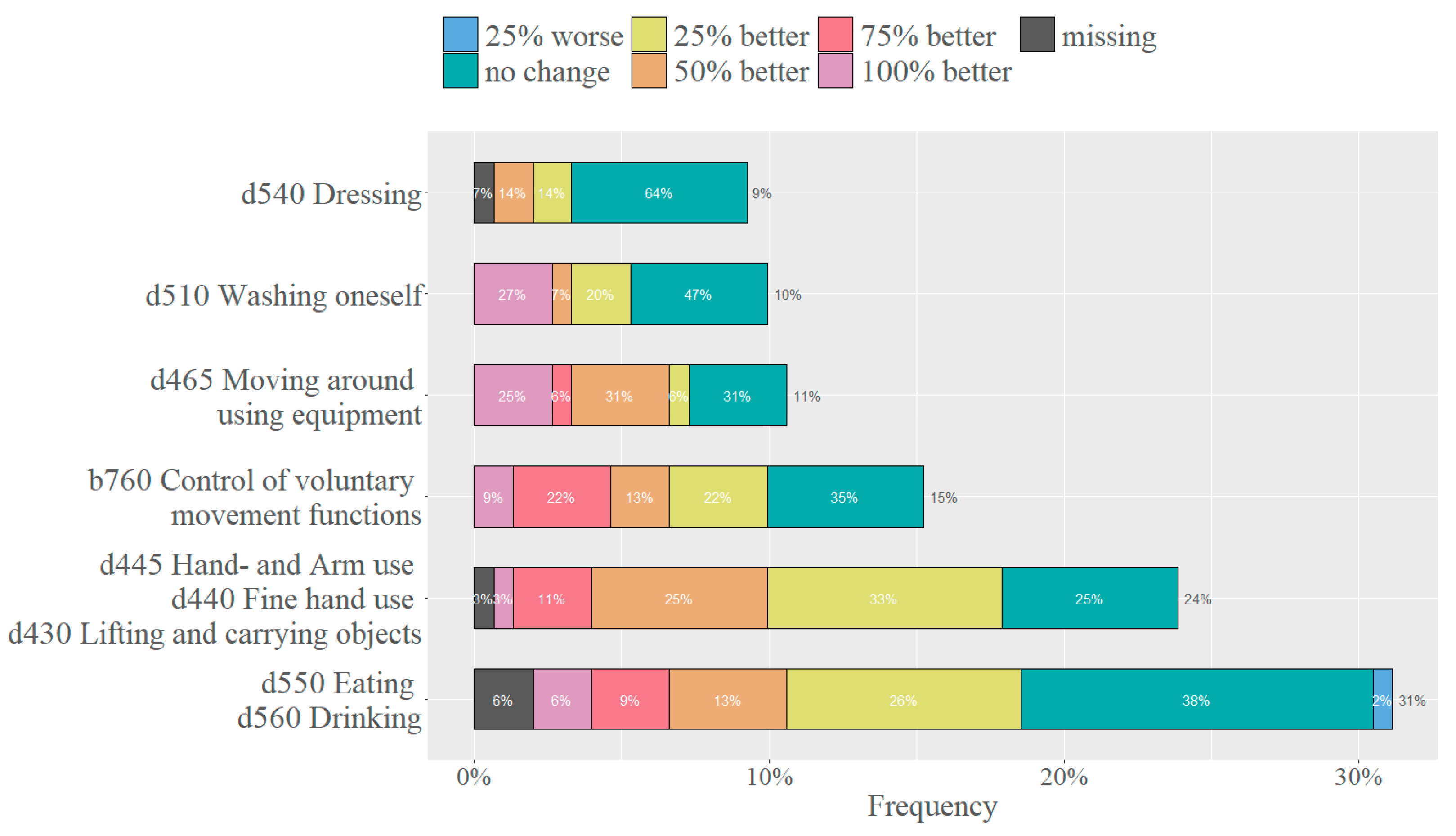
3.3.2. ADL Goals
3.4. Manual Muscle Testing
4. Discussion
4.1. Sample
4.2. Technology-Assisted Upper Limb Therapy (TAULT)
4.3. Goals
4.3.1. Body Functions
4.3.2. ADL Goals
4.4. Manual Muscle Testing
4.5. Personnel
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lo, C.; Tran, Y.; Anderson, K.; Craig, A.; Middleton, J. Functional Priorities in Persons with Spinal Cord Injury: Using Discrete Choice Experiments to Determine Preferences. J. Neurotrauma 2016, 33, 1958–1968. [Google Scholar] [CrossRef] [PubMed]
- Lynskey, J.V.; Belanger, A.; Jung, R. Activity-dependent plasticity in spinal cord injury. J. Rehabil. Res. Dev. 2008, 45, 229–240. [Google Scholar] [CrossRef] [PubMed]
- Gassert, R.; Dietz, V. Rehabilitation robots for the treatment of sensorimotor deficits: A neurophysiological perspective. J. Neuroeng. Rehabil. 2018, 15, 46. [Google Scholar] [CrossRef] [PubMed]
- Wade, D.T. Goal setting in rehabilitation: An overview of what, why and how. Clin. Rehabil. 2009, 23, 291–295. [Google Scholar] [CrossRef] [PubMed]
- WHO. How to Use the ICF: A Practical Manual for Using the International Classification of Functioning, Disability and Health (ICF); Exposure Draft for Comment; WHO: Geneva, Switzerland, 2013.
- Mittrach, R.; Grill, E.; Walchner-Bonjean, M.; Scheuringer, M.; Boldt, C.; Huber, E.O.; Stucki, G. Goals of physiotherapy interventions can be described using the International Classification of Functioning, Disability and Health. Physiotherapy 2008, 94, 150–157. [Google Scholar] [CrossRef]
- Finger, M.E.; Cieza, A.; Stoll, J.; Stucki, G.; Huber, E.O. Identification of intervention categories for physical therapy, based on the international classification of functioning, disability and health: A Delphi exercise. Phys. Ther. 2006, 86, 1203–1220. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Singh, H.; Unger, J.; Zariffa, J.; Pakosh, M.; Jaglal, S.; Craven, B.C.; Musselman, K.E. Robot-assisted upper extremity rehabilitation for cervical spinal cord injuries: A systematic scoping review. Disabil. Rehabil. Assist. Technol. 2018, 13, 704–715. [Google Scholar] [CrossRef]
- Yozbatiran, N.; Francisco, G.E. Robot-assisted Therapy for the Upper Limb after Cervical Spinal Cord Injury. Phys. Med. Rehabil. Clin. N. Am. 2019, 30, 367–384. [Google Scholar] [CrossRef]
- Hess, D.R. Retrospective studies and chart reviews. Respir. Care 2004, 49, 1171–1174. [Google Scholar]
- Kirshblum, S.C.; Waring, W.; Biering-Sorensen, F.; Burns, S.P.; Johansen, M.; Schmidt-Read, M.; Donovan, W.; Graves, D.; Jha, A.; Jones, L.; et al. Reference for the 2011 revision of the International Standards for Neurological Classification of Spinal Cord Injury. J. Spinal Cord Med. 2011, 34, 547–554. [Google Scholar] [CrossRef]
- Turner-Stokes, L. Goal attainment scaling (GAS) in rehabilitation: A practical guide. Clin. Rehabil. 2009, 23, 362–370. [Google Scholar] [CrossRef]
- Bovend’Eerdt, T.J.; Botell, R.E.; Wade, D.T. Writing SMART rehabilitation goals and achieving goal attainment scaling: A practical guide. Clin. Rehabil. 2009, 23, 352–361. [Google Scholar] [CrossRef]
- Hurn, J.; Kneebone, I.; Cropley, M. Goal setting as an outcome measure: A systematic review. Clin. Rehabil. 2006, 20, 756–772. [Google Scholar] [CrossRef]
- Kiresuk, T.J.; Sherman, R.E. Goal attainment scaling: A general method for evaluating comprehensive community mental health programs. Community Ment. Health J. 1968, 4, 443–453. [Google Scholar] [CrossRef]
- Cieza, A.; Brockow, T.; Ewert, T.; Amman, E.; Kollerits, B.; Chatterji, S.; Ustun, T.B.; Stucki, G. Linking health-status measurements to the international classification of functioning, disability and health. J. Rehabil. Med. 2002, 34, 205–210. [Google Scholar] [CrossRef]
- Hislop, H.J.; Montgomery, J. Daniels & Worthingham’s Muscle Testing: Techniques of Manual Examination, 8th ed.; Saunders Elsevier: St. Louis, MI, USA, 2007. [Google Scholar]
- WHO. International Classification of Functioning, Disability and Health; WHO: Geneva, Switzerland, 2001.
- Fekete, C.; Brach, M.; Ehrmann, C.; Post, M.W.M.; InSci; Stucki, G. Cohort Profile of the International Spinal Cord Injury Community Survey Implemented in 22 Countries. Arch. Phys. Med. Rehabil. 2020, 101, 2103–2111. [Google Scholar] [CrossRef]
- Doets, A.Y.; Verboon, C.; van den Berg, B.; Harbo, T.; Cornblath, D.R.; Willison, H.J.; Islam, Z.; Attarian, S.; Barroso, F.A.; Bateman, K.; et al. Regional variation of Guillain-Barre syndrome. Brain 2018, 141, 2866–2877. [Google Scholar] [CrossRef]
- DeVivo, M.J.; Biering-Sorensen, F.; New, P.; Chen, Y.; International Spinal Cord Injury Data, S. Standardization of data analysis and reporting of results from the International Spinal Cord Injury Core Data Set. Spinal Cord. 2011, 49, 596–599. [Google Scholar] [CrossRef]
- Wuennemann, M.J.; Mackenzie, S.W.; Lane, H.P.; Peltz, A.R.; Ma, X.; Gerber, L.M.; Edwards, D.J.; Kitago, T. Dose and staffing comparison study of upper limb device-assisted therapy. NeuroRehabilitation 2020, 46, 287–297. [Google Scholar] [CrossRef]
- Kirshblum, S.; Snider, B.; Eren, F.; Guest, J. Characterizing Natural Recovery after Traumatic Spinal Cord Injury. J. Neurotrauma 2021, 38, 1267–1284. [Google Scholar] [CrossRef]
- Langer, J.S.; Sueoka, S.S.; Wang, A.A. The importance of shoulder external rotation in activities of daily living: Improving outcomes in traumatic brachial plexus palsy. J. Hand Surg. Am. 2012, 37, 1430–1436. [Google Scholar] [CrossRef]
- Velstra, I.M.; Curt, A.; Frotzler, A.; Abel, R.; Kalsi-Ryan, S.; Rietman, J.S.; Bolliger, M. Changes in Strength, Sensation, and Prehension in Acute Cervical Spinal Cord Injury: European Multicenter Responsiveness Study of the GRASSP. Neurorehabil Neural Repair. 2015, 29, 755–766. [Google Scholar] [CrossRef]
- Jung, J.H.; Lee, H.J.; Cho, D.Y.; Lim, J.E.; Lee, B.S.; Kwon, S.H.; Kim, H.Y.; Lee, S.J. Effects of Combined Upper Limb Robotic Therapy in Patients with Tetraplegic Spinal Cord Injury. Ann. Rehabil. Med. 2019, 43, 445–457. [Google Scholar] [CrossRef]
- Simpson, L.A.; Eng, J.J.; Hsieh, J.T.; Wolfe, D.L.; Spinal Cord Injury Rehabilitation Evidence Scire Research, T. The health and life priorities of individuals with spinal cord injury: A systematic review. J. Neurotrauma 2012, 29, 1548–1555. [Google Scholar] [CrossRef]
- Snoek, G.J.; MJ, I.J.; Hermens, H.J.; Maxwell, D.; Biering-Sorensen, F. Survey of the needs of patients with spinal cord injury: Impact and priority for improvement in hand function in tetraplegics. Spinal Cord. 2004, 42, 526–532. [Google Scholar] [CrossRef]
- Cuthbert, S.C.; Goodheart, G.J., Jr. On the reliability and validity of manual muscle testing: A literature review. Chiropr. Osteopat. 2007, 15, 4. [Google Scholar] [CrossRef]
- Noreau, L.; Vachon, J. Comparison of three methods to assess muscular strength in individuals with spinal cord injury. Spinal Cord. 1998, 36, 716–723. [Google Scholar] [CrossRef]
- Morin, M.; Hebert, L.J.; Perron, M.; Petitclerc, E.; Lake, S.R.; Duchesne, E. Psychometric properties of a standardized protocol of muscle strength assessment by hand-held dynamometry in healthy adults: A reliability study. BMC Musculoskelet. Disord. 2023, 24, 294. [Google Scholar] [CrossRef]


| Characteristics | SCI | GBS | Other | Total |
|---|---|---|---|---|
| Number (%) | 42 (68.9) | 8 (13.1) | 11 (18.0) | 61 (100) |
| Age: median (IQR) (years) | 58.0 (47.0–66.3) | 70.0 (63.5–77.3) | 43.0 (27.5–60.5) | 58.0 (45.0–69.0) |
| Time since disease onset: median (IQR) (days) | 105 (70.8–137.5) | 162 (114.8–188.8) | 222 (81–2181) | 118 (76–221) |
| Time since admission: median (IQR) (days) | 72.5 (35.3–106.3) | 106 (67.0–144.8) | 47 (17.5–119.0) | 73 (31–114) |
| SCI group, n (%) | 42 (100) | |||
| C1–C5 AIS A–B | 13 (30.6) | |||
| C1–C5 AIS C | 7 (16.7) | |||
| C1–C5 AIS D | 13 (30.6) | |||
| C6–T1 AIS A–B | 1 (2.4) | |||
| C6–T1 AIS C | 0 (0) | |||
| C6–T1 AIS D | 4 (9.5) | |||
| T2–S3 AIS A–D | 6 (14.3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuchen, D.B.; Hubacher, B.; Ladner, A.; Velstra, I.-M.; Widmer, M. Technology-Assisted Upper Limb Therapy (TAULT): Evaluation of Clinical Practice at a Specialised Centre for Spinal Cord Injury in Switzerland. Healthcare 2023, 11, 3055. https://doi.org/10.3390/healthcare11233055
Kuchen DB, Hubacher B, Ladner A, Velstra I-M, Widmer M. Technology-Assisted Upper Limb Therapy (TAULT): Evaluation of Clinical Practice at a Specialised Centre for Spinal Cord Injury in Switzerland. Healthcare. 2023; 11(23):3055. https://doi.org/10.3390/healthcare11233055
Chicago/Turabian StyleKuchen, Daniela B., Beatrice Hubacher, Andris Ladner, Inge-Marie Velstra, and Mario Widmer. 2023. "Technology-Assisted Upper Limb Therapy (TAULT): Evaluation of Clinical Practice at a Specialised Centre for Spinal Cord Injury in Switzerland" Healthcare 11, no. 23: 3055. https://doi.org/10.3390/healthcare11233055
APA StyleKuchen, D. B., Hubacher, B., Ladner, A., Velstra, I.-M., & Widmer, M. (2023). Technology-Assisted Upper Limb Therapy (TAULT): Evaluation of Clinical Practice at a Specialised Centre for Spinal Cord Injury in Switzerland. Healthcare, 11(23), 3055. https://doi.org/10.3390/healthcare11233055






