Beyond Hypoglossal Hype: Social Media Perspectives on the Inspire Upper Airway Stimulation System
Abstract
:1. Introduction
2. Materials and Methods
2.1. Multimedia Classification
2.2. Authorship Demographics
2.3. Subject Categorization
- Advertisement: Strategically oriented posts promoting the Inspire® device, affiliated medical procedures, or ancillary resources.
- Educational: Scholarly content delving deep into the device’s mechanism, indications, therapeutic potential, or expansive knowledge pertinent to the Inspire® Sleep Apnea Hypoglossal Nerve Stimulator.
- Patient Experience: In-depth chronicles delineating subjective encounters with the Inspire® device, encompassing both the procedure and post-procedural experiences.
- Media Coverage: Analytical content highlighting the portrayal of or discourse on the Inspire® modality within the broader media echelons, encapsulating news, documentaries, and similar channels.
2.4. Engagement Metrics
2.5. Data Collection Standards
3. Results
3.1. Multimedia Classification
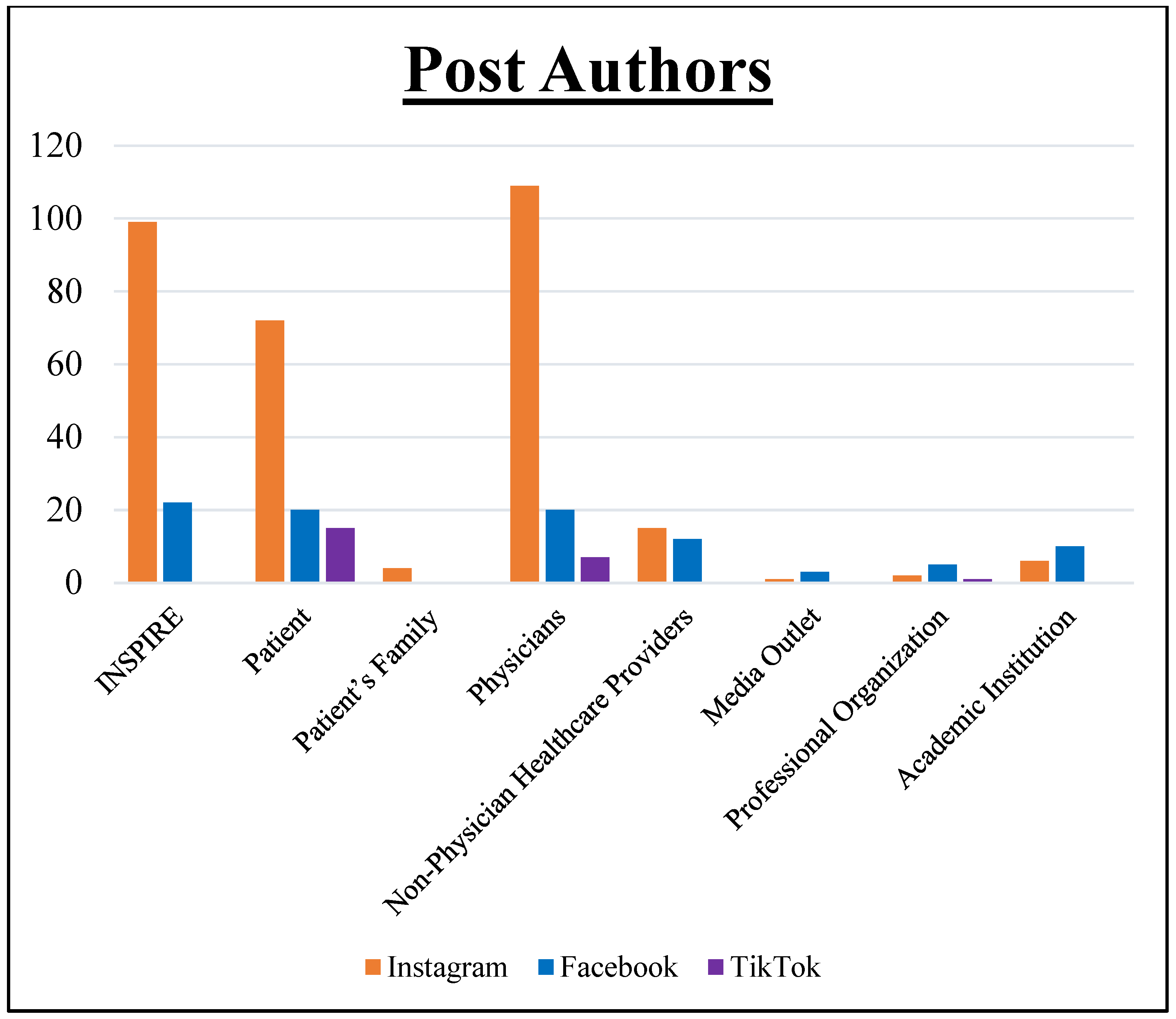
3.2. Authorship Demographics
3.3. Subject Categorization
3.4. Engagement Metrics
3.5. Hashtag Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Strollo, P.J., Jr.; Soose, R.J.; Maurer, J.T.; De Vries, N.; Cornelius, J.; Froymovich, O.; Hanson, R.D.; Padhya, T.A.; Steward, D.L.; Gillespie, M.B.; et al. Upper-Airway Stimulation for Obstructive Sleep Apnea. N. Eng. J. Med. 2014, 370, 139–149. [Google Scholar] [CrossRef] [PubMed]
- Dedhia, R.C.; Strollo, P.J.; Soose, R.J. Upper Airway Stimulation for Obstructive Sleep Apnea: Past, Present, and Future. Sleep 2015, 38, 899–906. [Google Scholar] [CrossRef] [PubMed]
- Baptista, P.; Di Frisco, I.M.; Urrestarazu, E.; Alcalde, J.; Alegre, M.; Sanchez, I.; O’Connor-Reina, C.; Plaza, G. Quality of Life Impact of Hypoglossal Nerve Stimulation with Inspire(®) Device in Patients with Obstructive Sleep Apnea Intolerant to Continuous Positive Airway Pressure Therapy. Life 2022, 12, 1737. [Google Scholar] [CrossRef] [PubMed]
- Costantino, A.; Rinaldi, V.; Moffa, A.; Luccarelli, V.; Bressi, F.; Cassano, M.; Casale, M.; Baptista, P. Hypoglossal nerve stimulation long-term clinical outcomes: A systematic review and meta-analysis. Sleep Breath 2020, 24, 399–411. [Google Scholar] [CrossRef] [PubMed]
- Mashaqi, S.; Patel, S.I.; Combs, D.; Estep, L.; Helmick, S.; Machamer, J.; Parthasarathy, S. The Hypoglossal Nerve Stimulation as a Novel Therapy for Treating Obstructive Sleep Apnea-A Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 1642. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Wang, Y. Social Media Use for Health Purposes: Systematic Review. J. Med. Internet Res. 2021, 23, e17917. [Google Scholar] [CrossRef] [PubMed]
- Jeyaraman, M.; Ramasubramanian, S.; Kumar, S.; Jeyaraman, N.; Selvaraj, P.; Nallakumarasamy, A.; Bondili, S.K.; Yadav, S.; Shanmugapriya, A.; Arulkumar, N. Multifaceted Role of Social Media in Healthcare: Opportunities, Challenges, and the Need for Quality Control. Cureus 2023, 15, e39111. [Google Scholar] [CrossRef]
- Chirumamilla, S.; Gulati, M. Patient Education and Engagement through Social Media. Curr. Cardiol. Rev. 2021, 17, 137–143. [Google Scholar] [CrossRef]
- García-Méndez, C.; García-Padilla, F.M.; Romero-Martín, M.; Sosa-Cordobés, E.; Domínguez-Pérez, M.D.M.; Robles-Romero, J.M. Social networks: A quality tool for health dissemination? J. Educ. Health Promot. 2022, 11, 355. [Google Scholar] [CrossRef]
- Suarez-Lledo, V.; Alvarez-Galvez, J. Prevalence of Health Misinformation on Social Media: Systematic Review. J. Med. Internet Res. 2021, 23, e17187. [Google Scholar] [CrossRef]
- Bestourous, D.E.; Pasick, L.J.; Benito, D.A.; Zapanta, P.E. Adverse events associated with the Inspire implantable hypoglossal nerve stimulator: A MAUDE database review. Am. J. Otolaryngol. 2020, 41, 102616. [Google Scholar] [CrossRef]
- Yeung, A.W.K.; Tosevska, A.; Klager, E.; Eibensteiner, F.; Tsagkaris, C.; Parvanov, E.D.; Nawaz, F.A.; Völkl-Kernstock, S.; Schaden, E.; Kletecka-Pulker, M.; et al. Medical and Health-Related Misinformation on Social Media: Bibliometric Study of the Scientific Literature. J. Med. Internet Res. 2022, 24, e28152. [Google Scholar] [CrossRef]
- Joseph, A.M.; Fernandez, V.; Kritzman, S.; Eaddy, I.; Cook, O.M.; Lambros, S.; Silva, C.E.J.; Arguelles, D.; Abraham, C.; Dorgham, N.; et al. COVID-19 Misinformation on Social Media: A Scoping Review. Cureus 2022, 14, e24601. [Google Scholar] [CrossRef] [PubMed]
- Ventola, C.L. Social media and health care professionals: Benefits, risks, and best practices. Pharm. Ther. 2014, 39, 491–520. [Google Scholar]
- Neely, S.; Eldredge, C.; Sanders, R. Health Information Seeking Behaviors on Social Media During the COVID-19 Pandemic Among American Social Networking Site Users: Survey Study. J. Med. Internet Res. 2021, 23, e29802. [Google Scholar] [CrossRef] [PubMed]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef] [PubMed]
- Patrick, M.; Venkatesh, R.D.; Stukus, D.R. Social media and its impact on health care. Ann. Allergy Asthma Immunol. 2022, 128, 139–145. [Google Scholar] [CrossRef]
- Tan, S.S.; Goonawardene, N. Internet Health Information Seeking and the Patient-Physician Relationship: A Systematic Review. J. Med. Internet Res. 2017, 19, e9. [Google Scholar] [CrossRef]
- Rossi, N.A.; George, S.S.; Patel, K.P.; Reddy, D.N.; Ohlstein, J.F.; McKinnon, B.J.; Siddiqui, F.N.; Lees, K.A. Qualitative analysis of sinus surgery posts on popular social media platforms. Am. J. Otolaryngol. 2022, 43, 103388. [Google Scholar] [CrossRef]
- Haeberle, H.S.; Bartschat, N.I.; Navarro, S.M.; Rooney, P.W.; Rosneck, J.; Westermann, R.W.; Ramkumar, P.N. Hip Arthroscopy: A Social Media Analysis of Patient Perception. Orthop. J. Sports Med. 2019, 7, 2325967119854188. [Google Scholar] [CrossRef]
- Haeberle, H.S.; Egger, A.C.; Navarro, S.M.; Cornaghie, M.M.; Ramkumar, P.N.; Goodwin, R.C.; Mont, M.A. Social Media and Pediatric Scoliosis: An Analysis of Patient and Surgeon Use. Surg. Technol. Int. 2017, 31, 189–196. [Google Scholar]
- Khansa, I.; Khansa, L.; Pearson, G.D. Patient Satisfaction After Rhinoplasty: A Social Media Analysis. Aesthet. Surg. J. 2016, 36, NP1–NP5. [Google Scholar] [CrossRef] [PubMed]
- Hairston, T.K.; Links, A.R.; Harris, V.; Tunkel, D.E.; Walsh, J.; Beach, M.C.; Boss, E.F. Evaluation of Parental Perspectives and Concerns About Pediatric Tonsillectomy in Social Media. JAMA Otolaryngol. Head. Neck Surg. 2019, 145, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Rossi, N.A.; Devarajan, K.; Chokshi, S.N.; Ochoa, V.J.; Benavidez, M.; Malaya, L.T.; Ohlstein, J.F.; Young, D.L.; McKinnon, B.J. Social Media Depictions of Cochlear Implants: An Instagram and TikTok Analysis. Otol. Neurotol. 2023, 44, e13–e21. [Google Scholar] [CrossRef] [PubMed]
- Green, K.K.; Woodson, B.T. Upper Airway Stimulation Therapy. Otolaryngol. Clin. North. Am. 2016, 49, 1425–1431. [Google Scholar] [CrossRef] [PubMed]
- Inspire for obstructive sleep apnea. Med. Lett. Drugs Ther. 2023, 65, 118–120. [CrossRef] [PubMed]
- Liu, P.; Kong, W.; Fang, C.; Zhu, K.; Dai, X.; Meng, X. Hypoglossal nerve stimulation in adolescents with down syndrome and obstructive sleep apnea: A systematic review and meta-analysis. Front. Neurol. 2022, 13, 1037926. [Google Scholar] [CrossRef]
- Moffatt, D.C.; Lahaye, J.J.; Corona, K.K.; Rossi, N.A.; Joshi, R.; Resto, V.; McKinnon, B.J.; Coblens, O.M. Laryngectomy: Social media analysis of patient perception. Head Neck 2023, 45, 464–472. [Google Scholar] [CrossRef]
- Rossi, N.A.; French, K.R.; Evans, C.L.; Ohlstein, J.F.; Neve, L.D.; Daram, S.; Young, D.L.; McKinnon, B.J.; Pine, H.S. Trending Tubes: A Social Media Analysis of Tympanostomy Tubes in Children. OTO Open 2022, 6, 2473974x221086964. [Google Scholar] [CrossRef]
- Yu, J.L.; Thaler, E.R. Hypoglossal Nerve (Cranial Nerve XII) Stimulation. Otolaryngol. Clin. N. Am. 2020, 53, 157–169. [Google Scholar] [CrossRef]
- Basch, C.H.; Hillyer, G.C.; Jaime, C. COVID-19 on TikTok: Harnessing an emerging social media platform to convey important public health messages. Int. J. Adolesc. Med. Health 2020, 34, 367–369. [Google Scholar] [CrossRef] [PubMed]
- McCashin, D.; Murphy, C.M. Using TikTok for public and youth mental health—A systematic review and content analysis. Clin. Child Psychol. Psychiatry 2023, 28, 279–306. [Google Scholar] [CrossRef] [PubMed]
- Zenone, M.; Ow, N.; Barbic, S. TikTok and public health: A proposed research agenda. BMJ Glob. Health 2021, 6, e007648. [Google Scholar] [CrossRef]
- Afful-Dadzie, E.; Afful-Dadzie, A.; Egala, S.B. Social media in health communication: A literature review of information quality. Health Inf. Manag. 2023, 52, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Kanchan, S.; Gaidhane, A. Social Media Role and Its Impact on Public Health: A Narrative Review. Cureus 2023, 15, e33737. [Google Scholar] [CrossRef] [PubMed]
- Kite, J.; Chan, L.; MacKay, K.; Corbett, L.; Reyes-Marcelino, G.; Nguyen, B.; Bellew, W.; Freeman, B. A Model of Social Media Effects in Public Health Communication Campaigns: Systematic Review. J. Med. Internet Res. 2023, 25, e46345. [Google Scholar] [CrossRef]
- LaHaye, J.J.; Moffatt, D.C.; Dunmire, A.; Corona, K.K.; Rossi, N.A.; Siddiqui, F.N. A social media analysis examining new-age devices of the rhinology industry. Int. Forum Allergy Rhinol. 2023, 13, 2092–2095. [Google Scholar] [CrossRef]
- Zhu, C.; Xu, X.; Zhang, W.; Chen, J.; Evans, R. How Health Communication via Tik Tok Makes a Difference: A Content Analysis of Tik Tok Accounts Run by Chinese Provincial Health Committees. Int. J. Environ. Res. Public. Health 2019, 17, 192. [Google Scholar] [CrossRef]
- Eppes, E.V.; Augustyn, M.; Gross, S.M.; Vernon, P.; Caulfield, L.E.; Paige, D.M. Engagement with and Acceptability of Digital Media Platforms for Use in Improving Health Behaviors Among Vulnerable Families: Systematic Review. J. Med. Internet Res. 2023, 25, e40934. [Google Scholar] [CrossRef]
- Ramkumar, P.N.; Navarro, S.M.; Haeberle, H.S.; Chughtai, M.; Demetriades, C.; Piuzzi, N.S.; Mont, M.A.; Bauer, T.W.; Muschler, G.F. Cellular therapy injections in today’s orthopedic market: A social media analysis. Cytotherapy 2017, 19, 1392–1399. [Google Scholar] [CrossRef]
- Ramkumar, P.N.; Navarro, S.M.; Haeberle, H.S.; Chughtai, M.; Flynn, M.E.; Mont, M.A. Social Media and Total Joint Arthroplasty: An Analysis of Patient Utilization on Instagram. J. Arthroplast. 2017, 32, 2694–2700. [Google Scholar] [CrossRef]
- Ramkumar, P.N.; Navarro, S.M.; Cornaghie, M.M.; Haeberle, H.S.; Hameed, H.; Schickendantz, M.S.; Ricchetti, E.T.; Iannotti, J.P. Social Media in Shoulder & Elbow Surgery: An Analysis of Twitter and Instagram. Int. J. Sports Med. 2018, 39, 564–570. [Google Scholar] [CrossRef] [PubMed]
- Győrffy, Z.; Radó, N.; Mesko, B. Digitally engaged physicians about the digital health transition. PLoS ONE 2020, 15, e0238658. [Google Scholar] [CrossRef] [PubMed]
- Navarro Martínez, O.; Igual García, J.; Traver Salcedo, V. Transferring Healthcare Professional’s Digital Competencies to the Workplace and Patients: A Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 13187. [Google Scholar] [CrossRef] [PubMed]
- Stoumpos, A.I.; Kitsios, F.; Talias, M.A. Digital Transformation in Healthcare: Technology Acceptance and Its Applications. Int. J. Environ. Res. Public Health 2023, 20, 3407. [Google Scholar] [CrossRef] [PubMed]
- Moses, R.E.; McNeese, L.G.; Feld, L.D.; Feld, A.D. Social media in the health-care setting: Benefits but also a minefield of compliance and other legal issues. Am. J. Gastroenterol. 2014, 109, 1128–1132. [Google Scholar] [CrossRef] [PubMed]
- Katz, M.; Nandi, N. Social Media and Medical Education in the Context of the COVID-19 Pandemic: Scoping Review. JMIR Med. Educ. 2021, 7, e25892. [Google Scholar] [CrossRef] [PubMed]
- Giroux, C.M.; Moreau, K.A. Leveraging social media for medical education: Learning from patients in online spaces. Med. Teach. 2020, 42, 970–972. [Google Scholar] [CrossRef]
- Lee, P.B.; Miano, D.I.; Sesselmann, M.; Johnson, J.; Chung, M.T.; Abboud, M.; Johnson, A.P.; Zuliani, G.F. RealSelf Social Media Analysis of Rhinoplasty Patient Reviews. J. Plast. Reconstr. Aesthet. Surg. 2022, 75, 2368–2374. [Google Scholar] [CrossRef]
- Xiao, K.; Campbell, D.; Mastrolonardo, E.; Boon, M.; Huntley, C. Evaluating YouTube Videos on Hypoglossal Nerve Stimulation as a Resource for Patients. Laryngoscope 2021, 131, E2827–E2832. [Google Scholar] [CrossRef]
- Park, E.; Forhan, M.; Jones, C.A. The use of digital storytelling of patients’ stories as an approach to translating knowledge: A scoping review. Res. Involv. Engagem. 2021, 7, 58. [Google Scholar] [CrossRef] [PubMed]
- Kington, R.S.; Arnesen, S.; Chou, W.S.; Curry, S.J.; Lazer, D.; Villarruel, A.M. Identifying Credible Sources of Health Information in Social Media: Principles and Attributes. National Academy of Medicine, 16 July 2021. [Google Scholar] [CrossRef]
- Alpert, J.M. Evaluating the Content of Family Physician Websites in the United States. J. Healthc. Qual. 2015, 37, 311–318. [Google Scholar] [CrossRef]
- Panahi, S.; Watson, J.; Partridge, H. Social media and physicians: Exploring the benefits and challenges. Health Inform. J. 2016, 22, 99–112. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Baxter, S.L.; Xu, J.; Zhou, X.; Zhang, K. The practical implementation of artificial intelligence technologies in medicine. Nat. Med. 2019, 25, 30–36. [Google Scholar] [CrossRef]
- Mesko, B.; Győrffy, Z.; Kollár, J. Digital Literacy in the Medical Curriculum: A Course with Social Media Tools and Gamification. JMIR Med. Educ. 2015, 1, e6. [Google Scholar] [CrossRef]
- Wong, B.L.; Khurana, M.P.; Smith, R.D.; El-Omrani, O.; Pold, A.; Lotfi, A.; O’Leary, C.A.; Saminarsih, D.S. Harnessing the digital potential of the next generation of health professionals. Hum. Resour. Health 2021, 19, 50. [Google Scholar] [CrossRef] [PubMed]
- Ngenzi, J.L.; Scott, R.E.; Mars, M. Information and communication technology to enhance continuing professional development (CPD) and continuing medical education (CME) for Rwanda: A scoping review of reviews. BMC Med. Educ. 2021, 21, 245. [Google Scholar] [CrossRef]
- Saiyad, S.; Virk, A.; Mahajan, R.; Singh, T. Online Teaching in Medical Training: Establishing Good Online Teaching Practices from Cumulative Experience. Int. J. Appl. Basic Med. Res. 2020, 10, 149–155. [Google Scholar] [CrossRef]
- Appel, G.; Grewal, L.; Hadi, R.; Stephen, A.T. The future of social media in marketing. J. Acad. Mark. Sci. 2020, 48, 79–95. [Google Scholar] [CrossRef]
- Barry, C.T.; Moran-Miller, K.; Levy, H.F.; Gray, T. Social media engagement, perceptions of social media costs and benefits, and well-being in college student-athletes. J. Am. Coll. Health 2022. [Google Scholar] [CrossRef]
- Hagg, E.; Dahinten, V.S.; Currie, L.M. The emerging use of social media for health-related purposes in low and middle-income countries: A scoping review. Int. J. Med. Inform. 2018, 115, 92–105. [Google Scholar] [CrossRef]
- Ulvi, O.; Karamehic-Muratovic, A.; Baghbanzadeh, M.; Bashir, A.; Smith, J.; Haque, U. Social Media Use and Mental Health: A Global Analysis. Epidemiologia 2022, 3, 11–25. [Google Scholar] [CrossRef]
- O’Sullivan, E.; Cutts, E.; Kavikondala, S.; Salcedo, A.; D’Souza, K.; Hernandez-Torre, M.; Anderson, C.; Tiwari, A.; Ho, K.; Last, J. Social Media in Health Science Education: An International Survey. JMIR Med. Educ. 2017, 3, e1. [Google Scholar] [CrossRef] [PubMed]
- Al-Dmour, H.; Masa’deh, R.; Salman, A.; Abuhashesh, M.; Al-Dmour, R. Influence of Social Media Platforms on Public Health Protection Against the COVID-19 Pandemic via the Mediating Effects of Public Health Awareness and Behavioral Changes: Integrated Model. J. Med. Internet Res. 2020, 22, e19996. [Google Scholar] [CrossRef] [PubMed]
- Farsi, D. Social Media and Health Care, Part I: Literature Review of Social Media Use by Health Care Providers. J. Med. Internet Res. 2021, 23, e23205. [Google Scholar] [CrossRef] [PubMed]
- De Vere Hunt, I.; Linos, E. Social Media for Public Health: Framework for Social Media-Based Public Health Campaigns. J. Med. Internet Res. 2022, 24, e42179. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Zhang, D.; Yang, C.; Wang, Y. Harnessing Social Media for Health Information Management. Electron. Commer. Res. Appl. 2018, 27, 139–151. [Google Scholar] [CrossRef] [PubMed]
- Auxier, B.; Anderson, M. Social Media Use in 2021; Pew Research Center: Washington, DC, USA, 2021. [Google Scholar]
- Yoon, S.; Wee, S.; Lee, V.S.Y.; Lin, J.; Thumboo, J. Patterns of use and perceived value of social media for population health among population health stakeholders: A cross-sectional web-based survey. BMC Public Health 2021, 21, 1312. [Google Scholar] [CrossRef] [PubMed]
- Côrte-Real, B.; Cordeiro, C.; Pestana, P.C.; Duarte, E.S.I.; Novais, F. Addictive Potential of Social Media: A Cross Sectional Study in Portugal. Acta Med. Port. 2023, 36, 162–166. [Google Scholar] [CrossRef]


| Inspire® Social Media Post Topics | |
|---|---|
| Subject | Description |
| Inspire® |
|
| Patient |
|
| Patient’s Family |
|
| Physicians |
|
| Non-Physician Healthcare Providers |
|
| Media Outlet |
|
| Professional Organization |
|
| Academic Institution |
|
| Inspire® Social Media Data | |||||
|---|---|---|---|---|---|
| n (%) | |||||
| Platform | TikTok | Total | |||
| Included Posts | 308 | 92 | 23 | 423 | |
| Type | |||||
| Image | 221 | 64 | 0 | 285 (67.4) | |
| Video | 87 | 9 | 23 | 119 (28.1) | |
| Text | 0 | 19 | 0 | 19 (4.5) | |
| Author | |||||
| Inspire® | 99 | 22 | 0 | 121 (28.6) | |
| Patient | 72 | 20 | 15 | 107 (25.3) | |
| Patient’s Family | 4 | 0 | 0 | 4 (0.9) | |
| Physicians | 109 | 20 | 7 | 136 (32.2) | |
| Non-Physician Healthcare Providers | 15 | 12 | 0 | 27 (6.4) | |
| Media Outlet | 1 | 3 | 0 | 4 (0.9) | |
| Professional Organization | 2 | 5 | 1 | 8 (1.9) | |
| Academic Institution | 6 | 10 | 0 | 16 (3.8) | |
| Subject | |||||
| Advertisement | 133 | 34 | 2 | 169 (40.0) | |
| Educational | 73 | 23 | 8 | 104 (24.6) | |
| Patient Experience | 101 | 32 | 13 | 146 (34.5) | |
| Media Coverage | 1 | 3 | 0 | 4 (0.9) | |
| Popularity | Mean Likes Per Post | 32.7 | 41.2 | 152.9 | 41.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rossi, N.A.; Vories, B.A.; Razmi, S.E.; Momin, N.A.; Burgess, Z.S.; Pine, H.S.; Shabani, S.; Sultana, R.; McKinnon, B.J. Beyond Hypoglossal Hype: Social Media Perspectives on the Inspire Upper Airway Stimulation System. Healthcare 2023, 11, 3082. https://doi.org/10.3390/healthcare11233082
Rossi NA, Vories BA, Razmi SE, Momin NA, Burgess ZS, Pine HS, Shabani S, Sultana R, McKinnon BJ. Beyond Hypoglossal Hype: Social Media Perspectives on the Inspire Upper Airway Stimulation System. Healthcare. 2023; 11(23):3082. https://doi.org/10.3390/healthcare11233082
Chicago/Turabian StyleRossi, Nicholas A., Bridget A. Vories, Samuel E. Razmi, Nishat A. Momin, Zachary S. Burgess, Harold S. Pine, Sepehr Shabani, Rizwana Sultana, and Brian J. McKinnon. 2023. "Beyond Hypoglossal Hype: Social Media Perspectives on the Inspire Upper Airway Stimulation System" Healthcare 11, no. 23: 3082. https://doi.org/10.3390/healthcare11233082
APA StyleRossi, N. A., Vories, B. A., Razmi, S. E., Momin, N. A., Burgess, Z. S., Pine, H. S., Shabani, S., Sultana, R., & McKinnon, B. J. (2023). Beyond Hypoglossal Hype: Social Media Perspectives on the Inspire Upper Airway Stimulation System. Healthcare, 11(23), 3082. https://doi.org/10.3390/healthcare11233082






