COVID-19 Continues to Burden General Practitioners: Impact on Workload, Provision of Care, and Intention to Leave
Abstract
1. Introduction
2. Methods
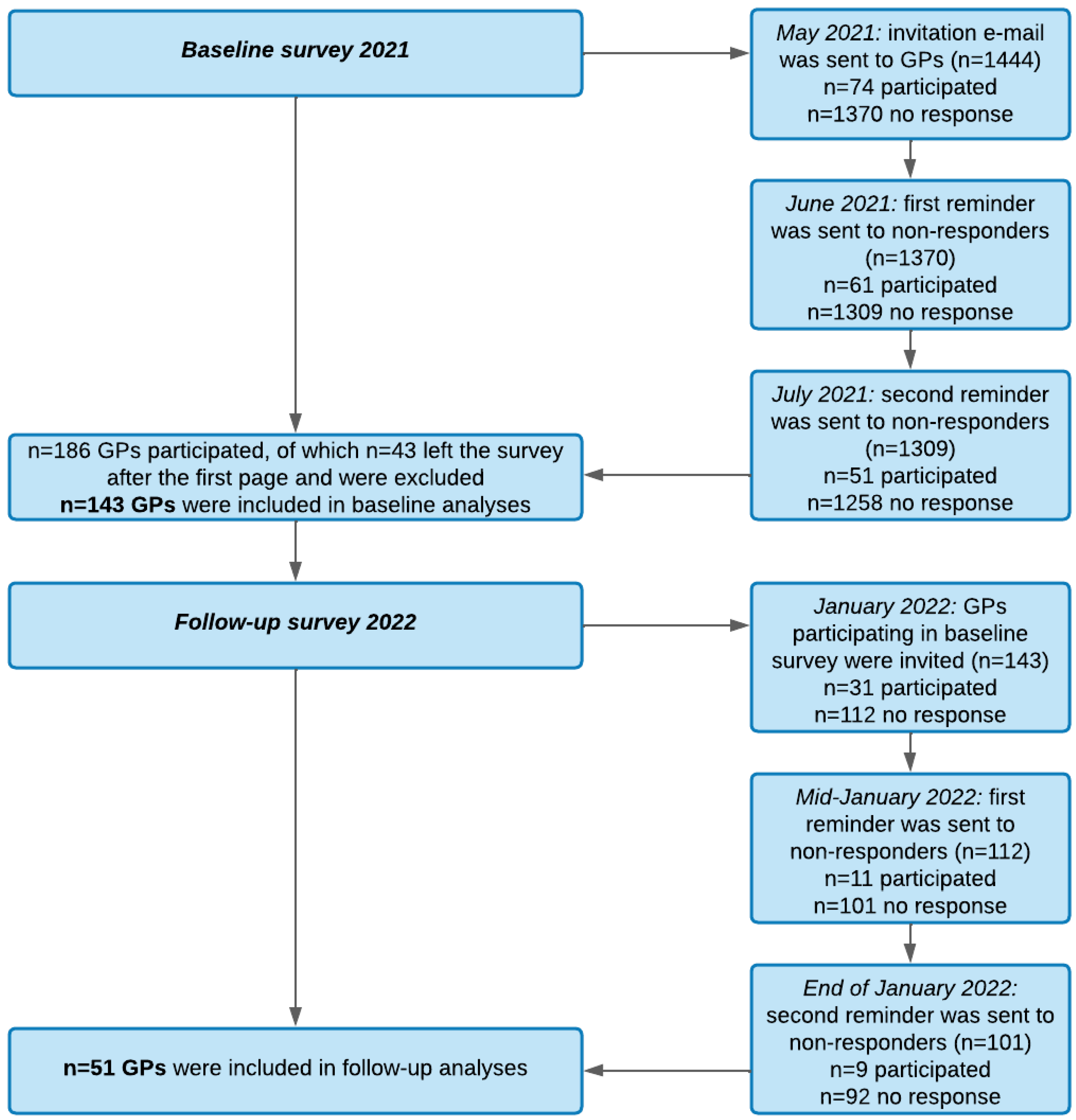
2.1. Recruitment Procedure
2.2. Survey
2.3. Coding of Free Text Entries
2.4. Statistical Analyses
3. Results
3.1. Sample Characteristics
3.2. Workload since the Outbreak of the Pandemic
3.3. Consultations Related to COVID-19 in GP Practices
3.4. Provision of Care for Patients with Long COVID: Identified Problems and Need for Support
3.5. Provision of Care for Other Patients since the Outbreak of the Pandemic
3.6. Intention to Leave
3.7. Additional Comments and Wishes
“It is difficult to get a rehabilitation place (which is also time-consuming and help is needed). The same applies to initiating psychological co-treatment. The health insurance companies do not support me as a doctor and my patients (e.g., I went through depressing written disputes about quarantine/AU [certificate of incapacity for work]).”(female GP, 49 years old)
“Direct and timely access to rehabilitation and specialist care must be organized! The best way is via a central coordination office. It is essential to set up a quota for psychotherapy for these patients!”(female GP, 42 years old)
“In my patients I see predominantly psychological impairments, especially an increase in anxiety/neurotic symptoms accompanied by physical and cognitive stress insufficiency. It is difficult to differentiate whether the physical limitations are a consequence of the psychological impairments.”(female GP, 45 years old)
“I am concerned that this disease is drifting more into the psychosomatic domain. Apart from a long feeling of illness, there is no tangible value and no recovery criterion except for the patient’s subjective statements.“(male GP, 59 years old)
“More than genuine “post/long COVID symptoms”, we observe an aggravation of already psychologically pre-altered patients in connection with COVID-19 without objectifiable pathological organic findings.”(male GP, 39 years old)
“The extensive “nocebo education” provided by the media and the constant change of information are counterproductive for physical and psychological convalescence.”(male GP, 39 years old)
“The state has failed and these polls are far too late. Last year’s discussions [2020] were a disgrace to the academy. Germany is stuck in the Middle Ages when it comes to communication between the university and the front.”(male GP, 35 years old)
“At the moment, I am only 50% GP and 50% practices organizer. Bureaucracy is not diminishing, since Corona, it massively increased (through constant change of billing codes, diagnosis codes and combinations, official orders).”(male GP, 54 years old)
“Planning security. A reasonable, comprehensible, and not constantly changing strategy in pandemic control and vaccine supply. Relief through sufficient vaccination services outside the practice. We can well and safely secure the infection event and the outpatient care of patients suffering from COVID-19 if we are not responsible for the quarantine regulations and we also receive the ordered vaccine. Compulsory vaccination of staff in our facilities will lead to staff shortages and I worry that, then at the latest, we will only be able to provide minimal patient care and the quality of care can no longer be guaranteed due to overwork of the remaining staff.”(female GP, 36 years old)
“The IT innovations are justified, plausible, and at some point perhaps also facilitating/helpful. Currently, however, these things represent an additional burden! It would therefore be helpful to postpone them or to implement simplified processes!”(male GP, 43 years old)
“It would help to be released from the burdensome and largely pointless expansion of digitization applications. I am not an opponent of digitization, but the currently planned measures such as e-prescription, e-AU [certificate of incapacity for work], and e-PA [patient file] predominantly cost time, money, non-existent mental reserves without visible practicability for the general public.”(female GP, 46 years old)
| Major Category | Subcategory | n * | % ** |
|---|---|---|---|
| General public and politics | 30 | 78.9 | |
| Reduction of bureaucracy | 12 | 31.6 | |
| Reduction of short-notice decisions/changes | 9 | 23.7 | |
| Reliable policy announcements | 7 | 18.4 | |
| Improvement of remuneration and budgeting | 6 | 15.8 | |
| Scientifically transparent recommendations | 4 | 10.5 | |
| Easy-to-understand regulations regarding quarantine and masks | 4 | 10.5 | |
| Improved collaboration with health authorities | 3 | 7.9 | |
| Consistent regulations for quarantine | 2 | 5.3 | |
| Unburdening of the reporting system for infectious diseases | 2 | 5.3 | |
| Coverage of non-medical COVID-19 counseling services by (health) authorities | 2 | 5.3 | |
| Anticipatory and responsible media communication | 2 | 5.3 | |
| GPs included in political committees and advisory boards | 2 | 5.3 | |
| Organizational system for scarce resources | 1 | 2.6 | |
| Actions against vaccination opponents and misinformation | 1 | 2.6 | |
| Reduction of mandatory health insurance services | 1 | 2.6 | |
| Protection of the health system from investors and shareholders | 1 | 2.6 | |
| Everyday practice | 22 | 57.9 | |
| More time for digital implementations | 5 | 13.2 | |
| No mandatory digitalization | 5 | 13.2 | |
| Increased time for patients (with chronic conditions) | 3 | 7.9 | |
| Improved availability of psychotherapists | 3 | 7.9 | |
| Preservation of therapeutic freedom | 2 | 5.3 | |
| Working without masks and/or tests | 2 | 5.3 | |
| Short hand-outs with information (on treatment of patients with COVID-19/long COVID, COVID-19 testing) | 2 | 5.3 | |
| Local meetings with other physicians | 1 | 2.6 | |
| Increased digitalization (e-vaccination card, e-prescription) | 1 | 2.6 | |
| Improved appointment options in long COVID outpatient clinics | 1 | 2.6 | |
| Vaccination | 18 | 47.4 | |
| Reliability of vaccine dose orders | 10 | 26.3 | |
| Constant offers for testing and vaccination outside the practice (test and vaccine centers) | 5 | 13.2 | |
| No compulsory vaccination | 5 | 13.2 | |
| Consistent regulations for COVID-19 vaccinations | 2 | 5.3 | |
| SARS-CoV-2 vaccines in single vials | 1 | 2.6 | |
| Compulsory vaccination | 1 | 2.6 | |
| Staff and colleagues | 13 | 34.2 | |
| Improvement of staffing situation | 4 | 10.5 | |
| Financial and societal upgrading of the medical staff | 4 | 10.5 | |
| Protection of staff from insults, threats, and misinformation | 2 | 5.3 | |
| Better medical cooperation in outpatient and inpatient areas | 2 | 5.3 | |
| Promotion of training and professional profile of physician assistants | 2 | 5.3 | |
| Physician assistant for administrative tasks | 1 | 2.6 | |
| Ensured provision of child care | 1 | 2.6 | |
| Recruitment of medical staff through health insurances | 1 | 2.6 | |
| Better work-life balance | 1 | 2.6 | |
| Possibility to delegate more non-medical tasks to staff | 1 | 2.6 | |
| Clear regulations regarding unvaccinated staff | 1 | 2.6 |
4. Discussion
4.1. Pandemic’s Influence on Workload
4.2. Consultations Related to COVID-19 and Other Services
4.3. Pandemic’s Influence on the Provision of Patient Care
4.4. Intention to Leave
4.5. Perceived Burdens and Need for Support
4.6. Limitations
4.7. Implications
- (1)
- The primary care sector carries the main quantitative burden of care for patients with acute COVID-19 and long COVID as well as SARS-CoV-2 vaccinations. GPs would therefore potentially benefit from extended treatment options, including additional external vaccination offers and referral options for patients with acute COVID-19 or long COVID to specialists or rehabilitation to increase time for non-COVID-19-related healthcare. Information and updates on these additional local specialized care offers should be easily available for GPs. In addition, multidisciplinary teams and the possibility to allocate tasks to practice nurses might further reduce GPs’ burden.
- (2)
- In the course of this pandemic or in future pandemics, GPs can be supported by revisiting, suspending, or outsourcing pandemic-related documentational and administrative work.
- (3)
- Changes in official regulations and legislation should be reduced to a minimum to increase compliance.
- (4)
- Practices should be able to postpone the implementation of obligatory changes in practices’ structures during times of extraordinarily high workload, such as telematics infrastructures. These implementations should also be fully developed and should not cause additional workload.
- (5)
- Finally, feeling valued for the daily responsibilities as well as financial incentives could further increase satisfaction for staff working in general practices and might compensate for the higher workload, as has also been reported previously [58].
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lal, A.; Lim, C.; Almeida, G.; Fitzgerald, J. Minimizing COVID-19 disruption: Ensuring the supply of essential health products for health emergencies and routine health services. Lancet Reg. Health-Am. 2022, 6, 100129. [Google Scholar] [CrossRef] [PubMed]
- Tuczyńska, M.; Matthews-Kozanecka, M.; Baum, E. Accessibility to non-COVID health services in the world during the COVID-19 pandemic: Review. Front. Public Health 2021, 9, 760795. [Google Scholar] [CrossRef] [PubMed]
- Webb, E.; Hernández-Quevedo, C.; Williams, G.; Scarpetti, G.; Reed, S.; Panteli, D. Providing health services effectively during the first wave of COVID-19: A cross-country comparison on planning services, managing cases, and maintaining essential services. Health Policy 2022, 126, 382–390. [Google Scholar] [CrossRef]
- Hoffmann, K.; Wojczewski, S.; George, A.; Schäfer, W.L.A.; Maier, M. Stressed and overworked? A cross-sectional study of the working situation of urban and rural general practitioners in Austria in the framework of the QUALICOPC project. Croat. Med. J. 2015, 56, 366–374. [Google Scholar] [CrossRef]
- Cohidon, C.; Wild, P.; Senn, N. Practice organization characteristics related to job satisfaction among general practitioners in 11 countries. Ann. Fam. Med. 2019, 17, 510–517. [Google Scholar] [CrossRef] [PubMed]
- Mahase, E. General practice needs rescue package to prevent burnout and preserve care, warns RCGP. BMJ 2021, 374, n1913. [Google Scholar] [CrossRef]
- Sudre, C.H.; Murray, B.; Varsavsky, T.; Graham, M.S.; Penfold, R.S.; Bowyer, R.C.; Pujol, J.C.; Klaser, K.; Antonelli, M.; Canas, L.S.; et al. Attributes and predictors of long COVID. Nat. Med. 2021, 27, 626–631. [Google Scholar] [CrossRef] [PubMed]
- Förster, C.; Colombo, M.G.; Wetzel, A.-J.; Martus, P.; Joos, S. Persisting symptoms after COVID-19. Dtsch. Arztebl. Int. 2022, 119, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Schrimpf, A.; Braesigk, A.; Lippmann, S.; Bleckwenn, M. Management and treatment of long COVID symptoms in general practices: An online-based survey. Front. Public Health 2022, 10, 937100. [Google Scholar] [CrossRef]
- Pavli, A.; Theodoridou, M.; Maltezou, H.C. Post-COVID syndrome: Incidence, clinical spectrum, and challenges for primary healthcare professionals. Arch. Med. Res. 2021, 52, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, T.; Knight, M.; A’Court, C.; Buxton, M.; Husain, L. Management of post-acute covid-19 in primary care. BMJ 2020, 370, m3026. [Google Scholar] [CrossRef] [PubMed]
- Borek, A.J.; Pilbeam, C.; Mableson, H.; Wanat, M.; Atkinson, P.; Sheard, S.; Martindale, A.M.; Solomon, T.; Butler, C.C.; Gobat, N.; et al. Experiences and concerns of health workers throughout the first year of the COVID-19 pandemic in the UK: A longitudinal qualitative interview study. PLoS ONE 2022, 17, e0264906. [Google Scholar] [CrossRef] [PubMed]
- Steiger, E.; Rass, S.; Seidel, A.; Kroll, L.; Czihal, T. COVID-19 vaccination in medical practices in Germany. Dtsch. Ärzteblatt Int. 2021, 118, 756–757. [Google Scholar] [CrossRef]
- Mojtahedzadeh, N.; Wirth, T.; Nienhaus, A.; Harth, V.; Mache, S. Job demands, resources and strains of outpatient caregivers during the covid-19 pandemic in Germany: A qualitative study. Int. J. Environ. Res. Public Health 2021, 18, 3684. [Google Scholar] [CrossRef] [PubMed]
- Hoernke, K.; Djellouli, N.; Andrews, L.; Lewis-Jackson, S.; Manby, L.; Martin, S.; Vanderslott, S.; Vindrola-Padros, C. Frontline healthcare workers’ experiences with personal protective equipment during the COVID-19 pandemic in the UK: A rapid qualitative appraisal. BMJ Open 2021, 11, e046199. [Google Scholar] [CrossRef]
- Frenkel, M.O.; Pollak, K.M.; Schilling, O.; Voigt, L.; Fritzsching, B.; Wrzus, C.; Egger-Lampl, S.; Merle, U.; Weigand, M.A.; Mohr, S. Stressors faced by healthcare professionals and coping strategies during the early stage of the COVID-19 pandemic in Germany. PLoS ONE 2022, 17, e0261502. [Google Scholar] [CrossRef]
- Jefferson, L.; Golder, S.; Heathcote, C.; Avila, A.C.; Dale, V.; Essex, H.; van der Feltz Cornelis, C.; McHugh, E.; Moe-Byrne, T.; Bloor, K. GP wellbeing during the COVID-19 pandemic: A systematic review. Br. J. Gen. Pract. 2022, 72, e325–e333. [Google Scholar] [CrossRef]
- Verhoeven, V.; Tsakitzidis, G.; Philips, H.; Van Royen, P. Impact of the COVID-19 pandemic on the core functions of primary care: Will the cure be worse than the disease? A qualitative interview study in Flemish GPs. BMJ Open 2020, 10, e039674. [Google Scholar] [CrossRef]
- Kumpunen, S.; Webb, E.; Permanand, G.; Zheleznyakov, E.; Edwards, N.; van Ginneken, E.; Jakab, M. Transformations in the landscape of primary health care during COVID-19: Themes from the European region. Health Policy 2022, 126, 391–397. [Google Scholar] [CrossRef]
- Saint-Lary, O.; Gautier, S.; Le Breton, J.; Gilberg, S.; Frappé, P.; Schuers, M.; Bourgueil, Y.; Renard, V. How GPs adapted their practices and organisations at the beginning of COVID-19 outbreak: A French national observational survey. BMJ Open 2020, 10, e042119. [Google Scholar] [CrossRef]
- Scheidt-Nave, C.; Barnes, B.; Beyer, A.-K.; Busch, M.A.; Hapke, U.; Heidemann, C.; Imhoff, M.; Mumm, R.; Paprott, R.; Steppuhn, H.; et al. Care for the chronically ill in Germany—The challenges during the COVID-19 pandemic. J. Health Monit. 2021, 5, 2–27. [Google Scholar] [CrossRef] [PubMed]
- Jacob, L.; Kalder, M.; Kostev, K. Decrease in the number of patients diagnosed with cancer during the COVID-19 pandemic in Germany. J. Cancer Res. Clin. Oncol. 2022, 148, 3117–3123. [Google Scholar] [CrossRef]
- Schäfer, I.; Hansen, H.; Menzel, A.; Eisele, M.; Tajdar, D.; Lühmann, D.; Scherer, M. The effect of COVID-19 pandemic and lockdown on consultation numbers, consultation reasons and performed services in primary care: Results of a longitudinal observational study. BMC Fam. Pract. 2021, 22, 125. [Google Scholar] [CrossRef]
- Tuppin, P.; Lesuffleur, T.; Constantinou, P.; Atramont, A.; Coatsaliou, C.; Ferrat, E.; Canouï-Poitrine, F.; Debeugny, G.; Rachas, A. Underuse of primary healthcare in France during the COVID-19 epidemic in 2020 according to individual characteristics: A national observational study. BMC Prim. Care 2022, 23, 200. [Google Scholar] [CrossRef] [PubMed]
- Archer, S.; Calanzani, N.; Honey, S.; Johnson, M.; Neal, R.; Scott, S.E.; Walter, F.M. Impact of the COVID-19 pandemic on cancer assessment in primary care: A qualitative study of GP views. BJGP Open 2021, 5, 56. [Google Scholar] [CrossRef]
- Maehl, N.; Bleckwenn, M.; Riedel-Heller, S.G.; Mehlhorn, S.; Lippmann, S.; Deutsch, T.; Schrimpf, A. The impact of the COVID-19 pandemic on avoidance of health care, symptom severity, and mental well-being in patients with coronary artery disease. Front. Med. 2021, 8, 760265. [Google Scholar] [CrossRef]
- Deml, M.J.; Minnema, J.; Dubois, J.; Senn, O.; Streit, S.; Rachamin, Y.; Jungo, K.T. The impact of the COVID-19 pandemic on the continuity of care for at-risk patients in Swiss primary care settings: A mixed-methods study. Soc. Sci. Med. 2022, 298, 114858. [Google Scholar] [CrossRef]
- Homeniuk, R.; Collins, C. How COVID-19 has affected general practice consultations and income: General practitioner cross-sectional population survey evidence from Ireland. BMJ Open 2021, 11, e044685. [Google Scholar] [CrossRef]
- Roth, C.; Breckner, A.; Moellinger, S.; Schwill, S.; Peters-Klimm, F.; Szecsenyi, J.; Stengel, S.; Wensing, M. Beliefs and practices among primary care physicians during the first wave of the COVID-19 pandemic in Baden-Wuerttemberg (Germany): An observational study. BMC Fam. Pract. 2021, 22, 86. [Google Scholar] [CrossRef] [PubMed]
- Alrawashdeh, H.M.; Al-Tammemi, A.A.B.; Alzawahreh, M.K.; Al-Tamimi, A.; Elkholy, M.; Al Sarireh, F.; Abusamak, M.; Elehamer, N.M.K.; Malkawi, A.; Al-Dolat, W.; et al. Occupational burnout and job satisfaction among physicians in times of COVID-19 crisis: A convergent parallel mixed-method study. BMC Public Health 2021, 21, 811. [Google Scholar] [CrossRef]
- Halcomb, E.; McInnes, S.; Williams, A.; Ashley, C.; James, S.; Fernandez, R.; Stephen, C.; Calma, K. The experiences of primary healthcare nurses during the COVID-19 pandemic in Australia. J. Nurs. Scholarsh. 2020, 52, 553–563. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.; Ripp, J.; Trockel, M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA 2020, 323, 2133–2134. [Google Scholar] [CrossRef] [PubMed]
- Wanat, M.; Hoste, M.; Gobat, N.; Anastasaki, M.; Böhmer, F.; Chlabicz, S.; Colliers, A.; Farrell, K.; Karkana, M.-N.; Kinsman, J.; et al. Supporting primary care professionals to stay in work during the COVID-19 pandemic: Views on personal risk and access to testing during the first wave of pandemic in Europe. Front. Med. 2021, 8, 726319. [Google Scholar] [CrossRef] [PubMed]
- Giusti, E.M.; Pedroli, E.; D’Aniello, G.E.; Stramba Badiale, C.; Pietrabissa, G.; Manna, C.; Stramba Badiale, M.; Riva, G.; Castelnuovo, G.; Molinari, E. The psychological impact of the COVID-19 outbreak on health professionals: A cross-sectional study. Front. Psychol. 2020, 11, 1684. [Google Scholar] [CrossRef] [PubMed]
- Naldi, A.; Vallelonga, F.; Di Liberto, A.; Cavallo, R.; Agnesone, M.; Gonella, M.; Sauta, M.D.; Lochner, P.; Tondo, G.; Bragazzi, N.L.; et al. COVID-19 pandemic-related anxiety, distress and burnout: Prevalence and associated factors in healthcare workers of North-West Italy. BJPsych Open 2021, 7, e27. [Google Scholar] [CrossRef]
- Savitsky, B.; Radomislensky, I.; Hendel, T. Nurses’ occupational satisfaction during Covid-19 pandemic. Appl. Nurs. Res. 2021, 59, 151416. [Google Scholar] [CrossRef]
- Fernemark, H.; Skagerström, J.; Seing, I.; Hårdstedt, M.; Schildmeijer, K.; Nilsen, P. Working conditions in primary healthcare during the COVID-19 pandemic: An interview study with physicians in Sweden. BMJ Open 2022, 12, e055035. [Google Scholar] [CrossRef]
- Copp, T.; Isautier, J.M.J.; Nickel, B.; Pickles, K.; Tracy, M.; Doust, J.; Bonner, C.; Dodd, R.H.; Ayre, J.; Cvejic, E.; et al. COVID-19 challenges faced by general practitioners in Australia: A survey study conducted in March 2021. Aust. J. Prim. Health 2021, 27, 357–363. [Google Scholar] [CrossRef]
- Willis, K.; Ezer, P.; Lewis, S.; Bismark, M.; Smallwood, N. Covid just amplified the cracks of the system’: Working as a frontline health worker during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 10178. [Google Scholar] [CrossRef]
- Groenewegen, P.; Van Poel, E.; Spreeuwenberg, P.; Batenburg, R.; Mallen, C.; Murauskiene, L.; Peris, A.; Pétré, B.; Schaubroeck, E.; Stark, S.; et al. Has the COVID-19 pandemic led to changes in the tasks of the primary care workforce? An international survey among general practices in 38 countries (PRICOV-19). Int. J. Environ. Res. Public Health 2022, 19, 15329. [Google Scholar] [CrossRef]
- Hoerold, M.; Gottschalk, M.; Debbeler, C.M.; Heytens, H.; Ehrentreich, S.; Braun-Dullaeus, R.C.; Apfelbacher, C. Healthcare professionals’ perceptions of impacts of the Covid-19-pandemic on outpatient care in rural areas: A qualitative study. BMC Health Serv. Res. 2021, 21, 1298. [Google Scholar] [CrossRef]
- Wanat, M.; Hoste, M.; Gobat, N.; Anastasaki, M.; Böhmer, F.; Chlabicz, S.; Colliers, A.; Farrell, K.; Karkana, M.N.; Kinsman, J.; et al. Transformation of primary care during the COVID-19 pandemic: Experiences of healthcare professionals in eight European countries. Br. J. Gen. Pract. 2021, 71, e634–e642. [Google Scholar] [CrossRef]
- Chudasama, Y.V.; Gillies, C.L.; Zaccardi, F.; Coles, B.; Davies, M.J.; Seidu, S.; Khunti, K. Impact of COVID-19 on routine care for chronic diseases: A global survey of views from healthcare professionals. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 965–967. [Google Scholar] [CrossRef]
- Carr, M.J.; Wright, A.K.; Leelarathna, L.; Thabit, H.; Milne, N.; Kanumilli, N.; Ashcroft, D.M.; Rutter, M.K. Impact of COVID-19 restrictions on diabetes health checks and prescribing for people with type 2 diabetes: A UK-wide cohort study involving 618 161 people in primary care. BMJ Qual. Saf. 2022, 31, 503–514. [Google Scholar] [CrossRef]
- Cunningham, A.T.; Felter, J.; Smith, K.R.; Sifri, R.; Arenson, C.; Patel, A.; Kelly, E.L. Burnout and commitment after 18 months of the COVID-19 pandemic: A follow-up qualitative study with primary care teams. J. Am. Board Fam. Med. 2023, 35, 220226R1. [Google Scholar] [CrossRef]
- Richter-Kuhlmann, E. Coronapandemie: Das Ende der Impfzentren. Dtsch. Ärzteblatt Int. 2021, 118, A-1854. Available online: https://www.aerzteblatt.de/int/article.asp?id=221601 (accessed on 30 November 2022).
- Edwards, P.J.; Roberts, I.; Clarke, M.J.; DiGuiseppi, C.; Wentz, R.; Kwan, I.; Cooper, R.; Felix, L.M.; Pratap, S. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst. Rev. 2009, 3, MR000008. [Google Scholar] [CrossRef] [PubMed]
- Drennan, J. Cognitive interviewing: Verbal data in the design and pretesting of questionnaires. J. Adv. Nurs. 2003, 42, 57–63. [Google Scholar] [CrossRef]
- Mahlknecht, A.; Barbieri, V.; Engl, A.; Piccoliori, G.; Wiedermann, C.J. Challenges and experiences of general practitioners during the course of the Covid-19 pandemic: A northern Italian observational study—Cross-sectional analysis and comparison of a two-time survey in primary care. Fam. Pract. 2022, 39, 1009–1016. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, J. Study highlights effects of COVID-19 burnout on primary care physicians in 10 high-income countries. JAMA Health Forum 2022, 3, e225101. [Google Scholar] [CrossRef]
- Platen, M.; Bohlken, J.; Hoffmann, W.; Kostev, K.; Michalowsky, B. The long-term impact of the COVID-19 pandemic on primary and specialized care provision and disease recognition in Germany. Front. Public Health 2022, 10, 1006578. [Google Scholar] [CrossRef] [PubMed]
- Williams, R.; Jenkins, D.A.; Ashcroft, D.M.; Brown, B.; Campbell, S.; Carr, M.J.; Cheraghi-Sohi, S.; Kapur, N.; Thomas, O.; Webb, R.T.; et al. Diagnosis of physical and mental health conditions in primary care during the COVID-19 pandemic: A retrospective cohort study. Lancet Public Health 2020, 5, e543–e550. [Google Scholar] [CrossRef]
- Matenge, S.; Sturgiss, E.; Desborough, J.; Hall Dykgraaf, S.; Dut, G.; Kidd, M. Ensuring the continuation of routine primary care during the COVID-19 pandemic: A review of the international literature. Fam. Pract. 2022, 39, 747–761. [Google Scholar] [CrossRef]
- Hangartner, N.; Di Gangi, S.; Elbl, C.; Senn, O.; Bisatz, F.; Fehr, T. Impact of the COVID-19 pandemic on emergency outpatient consultations and admissions of non-COVID-19 patients (ECCO)—A cross-sectional study. PLoS ONE 2022, 17, e0269724. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.F.; Nicholson, B.D.; Hirst, Y.; Fleming, S.; Bankhead, C.R. Primary care practice and cancer suspicion during the first three COVID-19 lockdowns in the UK: A qualitative study. Br. J. Gen. Pract. 2022, 72, e713–e721. [Google Scholar] [CrossRef] [PubMed]
- Jentzsch, A.; Geier, A.-K.; Bleckwenn, M.; Schrimpf, A. Differences in demographics of vaccinees, access to, and satisfaction with SARS-CoV-2 vaccination procedures between German general practices and mass vaccination centers. Vaccines 2022, 10, 1823. [Google Scholar] [CrossRef] [PubMed]
- Robert Koch-Institut. Monitoring des COVID-19-Impfgeschehens in Deutschland. Monatsbericht vom 29.09.2022. 2022. Available online: www.rki.de/covid-19-impfbericht (accessed on 22 November 2022).
- Sinsky, C.A.; Brown, R.L.; Stillman, M.J.; Linzer, M. COVID-related stress and work intentions in a sample of US health care workers. Mayo Clin. Proc. Innov. Qual. Outcomes 2021, 5, 1165–1173. [Google Scholar] [CrossRef] [PubMed]
- Jung, F.U.; Bodendieck, E.; Bleckwenn, M.; Hussenöder, F.; Luppa, M.; Riedel-Heller, S.G. Views on Retirement by General Practitioners. Gesundh. EFirst 2022, 70, e1–e2. [Google Scholar] [CrossRef]
- Békési, D.; Teker, I.; Torzsa, P.; Kalabay, L.; Rózsa, S.; Eőry, A. To prevent being stressed-out: Allostatic overload and resilience of general practitioners in the era of COVID-19. A cross-sectional observational study. Eur. J. Gen. Pract. 2021, 27, 277–285. [Google Scholar] [CrossRef]
- Hann, M.; Reeves, D.; Sibbald, B. Relationships between job satisfaction, intentions to leave family practice and actually leaving among family physicians in England. Eur. J. Public Health 2011, 21, 499–503. [Google Scholar] [CrossRef]
- Stengel, S.; Hoffmann, M.; Koetsenruijter, J.; Peters-Klimm, F.; Wensing, M.; Merle, U.; Szecsenyi, J. Long COVID: Care and support needs from the perspective of “long-haul” patients and primary care practitioners—A mixed-methods study from Baden-Wuerttemberg. Z. Evidenz Fortbild. Qual. Gesundh. 2022, 172, 61–70. [Google Scholar] [CrossRef]
- Parkin, A.; Davison, J.; Tarrant, R.; Ross, D.; Halpin, S.; Simms, A.; Salman, R.; Sivan, M. A multidisciplinary NHS COVID-19 service to manage post-COVID-19 syndrome in the community. J. Prim. Care Community Health 2021, 12, 21501327211010994. [Google Scholar] [CrossRef] [PubMed]
- Panchyrz, I.; Pohl, S.; Hoffmann, J.; Gatermann, C.; Walther, F.; Harst, L.; Held, H.-C.; Kleber, C.; Albrecht, M.; Schmitt, J. The role of university hospitals in regional health care management for coping with the COVID-19 pandemic. Z. Evidenz Fortbild. Qual. Gesundh. 2021, 167, 68–77. [Google Scholar] [CrossRef]
- Jefferson, L.; Heathcote, C.; Bloor, K. General practitioner wellbeing during the COVID-19 pandemic: A qualitative interview study. MedRxiv 2022. [Google Scholar]
- Kuhlmann, S.; Franzke, J. Multi-level responses to COVID-19: Crisis coordination in Germany from an intergovernmental perspective. Local Gov. Stud. 2022, 48, 312–334. [Google Scholar] [CrossRef]
- Dutour, M.; Kirchhoff, A.; Janssen, C.; Meleze, S.; Chevalier, H.; Levy-Amon, S.; Detrez, M.A.; Piet, E.; Delory, T. Family medicine practitioners’ stress during the COVID-19 pandemic: A cross-sectional survey. BMC Fam. Pract. 2021, 22, 36. [Google Scholar] [CrossRef]
- Buhlinger-Göpfarth, N.; Zander, A.; Heckmann, I.; Holzmann, T.; Lauck, K.; Stengel, S.; Nickel, S.; Peters-Klimm, F. Time spent on the vaccination process and organization of the COVID-19 vaccination in family practices. Z. Für Allg. 2022, 98, 100–105. [Google Scholar] [CrossRef]
- Koch, H.; Schmola, M. Digitalisierung und Patientensicherheit in einem Medizinischen Versorgungszentrum während der Corona-Pandemie. In Patientensicherheit: Gemeinsames Handeln als Herausforderung; Hellmann, W., Ed.; Springer Gabler: Wiesbaden, Germany, 2022; pp. 129–137. [Google Scholar] [CrossRef]
- Burmann, A.; Tischler, M.; Faßbach, M.; Schneitler, S.; Meister, S. The role of physicians in digitalizing health care provision: Web-based survey study. JMIR Med. Inform. 2021, 9, e31527. [Google Scholar] [CrossRef] [PubMed]
- Weißenfeld, M.M.; Goetz, K.; Steinhäuser, J. Facilitators and barriers for the implementation of telemedicine from a local government point of view—A cross-sectional survey in Germany. BMC Health Serv. Res. 2021, 21, 919. [Google Scholar] [CrossRef] [PubMed]
- Gardner, D.G.; Cummings, L.L.; Dunham, R.B.; Pierce, J.L. Single-item versus multiple-item measurement scales: An empirical comparison. Educ. Psychol. Meas. 1998, 58, 898–915. [Google Scholar] [CrossRef]
- Matthews, R.A.; Pineault, L.; Hong, Y.H. Normalizing the use of single-item measures: Validation of the single-item compendium for organizational psychology. J. Bus. Psychol. 2022, 37, 639–673. [Google Scholar] [CrossRef]
- Verster, J.C.; Sandalova, E.; Garssen, J.; Bruce, G. The use of single-item ratings versus traditional multiple-item questionnaires to assess mood and health. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 183–198. [Google Scholar] [CrossRef] [PubMed]
- Merrett, A.; Jones, D.; Sein, K.; Green, T.; Macleod, U. Attitudes of newly qualified doctors towards a career in general practice: A qualitative focus group study. Br. J. Gen. Pract. 2017, 67, e253–e259. [Google Scholar] [CrossRef] [PubMed]
- Selva Olid, A.; Zurro, A.M.; Villa, J.J.; Hijar, A.M.; Tuduri, X.M.; Puime, Á.O.; Dalmau, G.M.; Coello, P.A. Medical students’ perceptions and attitudes about family practice: A qualitative research synthesis. BMC Med. Educ. 2012, 12, 81. [Google Scholar] [CrossRef] [PubMed]
- Doran, N.; Fox, F.; Rodham, K.; Taylor, G.; Harris, M. Lost to the NHS: A mixed methods study of why GPs leave practice early in England. Br. J. Gen. Pract. 2016, 66, e128–e135. [Google Scholar] [CrossRef]


| Total | Practices with no Focus on COVID-19 | Practices with Focus on COVID-19 | |||
|---|---|---|---|---|---|
| p | F/χ2 | ||||
| n | 143 | 132 | 11 | ||
| Age | 50.2 ± 9.4 | 50.3 ± 9.2 | 48.5 ± 11.4 | 0.528 | 0.399 |
| Sex | 61.1% ♀ | 59.8% ♀ | 63.6% ♀ | 1.000 | 0.131 |
| Medical specialist for * | |||||
| General Medicine | 65% | 66.7% | 45.5% | 0.193 | 2.009 |
| Internal Medicine | 33.6% | 32.6% | 45.5% | 0.508 | 0.755 |
| Others | 4.9% | 4.5% | 9.1% | 0.436 | 0.451 |
| Practice structure | 0.051 | 9.153 | |||
| Single practice | 61.5% | 62.1% | 54.5% | ||
| Practice sharing | 10.5% | 11.4% | 0.0% | ||
| Joint practice | 16.1% | 13.6% | 45.5% | ||
| Medical center | 11.9% | 12.9% | 0.0% | ||
| Number of health insurance approved physicians per practice | 1.5 ± 1.0 | 1.4 ± 0.9 | 2.2 ± 1.7 | 0.018 | 5.743 |
| Number of cases per quarter | 0.102 | 7.713 | |||
| ≤700 | 7.7% | 8.3% | 0.0% | ||
| 701–1000 | 24.5% | 26.5% | 0.0% | ||
| 1001–1500 | 39.2% | 38.6% | 45.5% | ||
| ≥1501 | 26.6% | 24.2% | 54.5% | ||
| No answer | 2.1% | 2.3% | 0.0% | ||
| Catchment area of the practice * | |||||
| City | 39.2% | 38.6% | 45.5% | 0.751 | 0.198 |
| Small town | 44.8% | 45.5% | 36.4% | 0.755 | 0.339 |
| Rural | 41.3% | 41.7% | 36.4% | 1.000 | 0.118 |
| Baseline 2021 | Follow-Up 2022 | |
|---|---|---|
| n | 143 | 51 |
| Compared to pre-pandemic times, my practice is visited by patients | ||
| More frequently | 47.3% | 69.4% |
| As frequently | 42% | 24.5% |
| Less frequently | 10.7% | 6.1% |
| Compared to pre-pandemic times, I need for patient consultations | ||
| More time | 67.9% | 61.2% |
| As much time | 28.2% | 32.7% |
| Less time | 3.8% | 6.1% |
| Compared to pre-pandemic times, my workload is | ||
| Higher | 91.6% | 95.9% |
| Just the same | 8.4% | 4.1% |
| Lower | 0% | 0% |
| Compared to pre-pandemic times, the economic situation of my practice | ||
| Improved | 19.8% | 44.9% |
| Did not change | 67.2% | 40.8% |
| Worsened | 13% | 14.3% |
| Have you considered quitting your job in the last 12 months? | n.a. | |
| Yes | 26.5% | |
| No | 73.5% |
| Baseline 2021 | Follow-Up 2022 | |
|---|---|---|
| n | 143 | 51 |
| Current number of patients with acute COVID-19 per GP practice | n.a. | 43.3 ± 84.2 |
| Current number of patients with long COVID (symptoms lasting between 4–12 weeks) per GP practice | 11.9 ± 11.3 | 10.0 ± 11.3 |
| Current number of patients with long COVID (symptoms lasting >12 weeks) per GP practice | 5.9 ± 6.4 | 6.8 ± 9.6 |
| Consultation of patient with acute COVID-19 in practice | n.a. | |
| Daily | 32.1% | |
| Weekly | 51.9% | |
| Monthly | 13% | |
| Less than monthly | 3% | |
| Never | 0% | |
| Consultation of patient with long COVID (symptoms lasting between 4–12 weeks) in practice | n.a. | |
| Daily | 3.8% | |
| Weekly | 44.3% | |
| Monthly | 38.9% | |
| Less than monthly | 13% | |
| Never | 0% | |
| Consultation of patient with long COVID (symptoms lasting more than 12 weeks) in practice | n.a. | |
| Daily | 2.4% | |
| Weekly | 16.9% | |
| Monthly | 44.6% | |
| Less than monthly | 24.6% | |
| Never | 11.5% | |
| How many out of 100 patients are currently visiting for the following reasons: | n.a. | |
| Acute COVID-19 infection | 9.1 ± 8.3 | |
| Long COVID (4–12 weeks after diagnosis) | 3.2 ± 3.4 | |
| Long COVID (>12 weeks after diagnosis) | 1.8 ± 1.9 | |
| Other infections | 9.3 ± 6.1 | |
| Other acute reasons | 13.7 ± 7.5 | |
| Care of chronic diseases | 33.9 ± 16.5 | |
| SARS-CoV-2 vaccinations | 15.3 ± 10.1 | |
| Other vaccinations | 5.6 ± 4.7 | |
| Other reasons | 7.9 ± 10 | |
| Number of SARS-CoV-2 vaccinations per week | n.a. | 74.5 ± 73.7 |
| Baseline 2021 | Follow-Up 2022 | |
|---|---|---|
| n | 143 | 51 |
| Problems related to treatment of patients with long COVID * | n.a. | |
| Diagnosis is difficult | 42.1% | |
| Unspecific symptoms | 78.2% | |
| Uncertainty regarding medications | 70.7% | |
| Long course of disease | 78.9% | |
| No guidelines available | 56.4% | |
| Need for support related to COVID-19 * | n.a. | |
| Specialized information on typical symptoms and their length | 53.4% | |
| Exchange with colleagues on case reports and workshops | 45.9% | |
| Online training | 37.6% | |
| Diagnostic tools | 30.8% | |
| Special therapies for patients with long COVID | 55.6% | |
| Guidelines on long COVID | 63.9% | |
| Referral options to specialized outpatient clinics | 60.9% | |
| Fewer appointments can be currently offered in the following services *: | n.a. | |
| Acute consultations | 20% | |
| Care of chronically ill patients | 40% | |
| Preventive cancer screenings | 44% | |
| Preventive health check-ups | 58% | |
| Self-payer services | 66% | |
| Home visits | 24% | |
| Nursing home visits | 22% | |
| Being able to address medical and/or psychological needs of COVID patients during consultations 1 = “not able”, 10 = “fully able” | 6.7 ± 2 | 6.7 ± 2 |
| Perceived limited provision of satisfactory medical care to other patients with chronic diseases 1 = “fully limited”, 10 = “not limited” | 6.2 ± 2.5 | 5.1 ± 2.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schrimpf, A.; Bleckwenn, M.; Braesigk, A. COVID-19 Continues to Burden General Practitioners: Impact on Workload, Provision of Care, and Intention to Leave. Healthcare 2023, 11, 320. https://doi.org/10.3390/healthcare11030320
Schrimpf A, Bleckwenn M, Braesigk A. COVID-19 Continues to Burden General Practitioners: Impact on Workload, Provision of Care, and Intention to Leave. Healthcare. 2023; 11(3):320. https://doi.org/10.3390/healthcare11030320
Chicago/Turabian StyleSchrimpf, Anne, Markus Bleckwenn, and Annett Braesigk. 2023. "COVID-19 Continues to Burden General Practitioners: Impact on Workload, Provision of Care, and Intention to Leave" Healthcare 11, no. 3: 320. https://doi.org/10.3390/healthcare11030320
APA StyleSchrimpf, A., Bleckwenn, M., & Braesigk, A. (2023). COVID-19 Continues to Burden General Practitioners: Impact on Workload, Provision of Care, and Intention to Leave. Healthcare, 11(3), 320. https://doi.org/10.3390/healthcare11030320






