The Role of Physiotherapists in Smoking Cessation Management: A Scoping Review
Abstract
1. Introduction
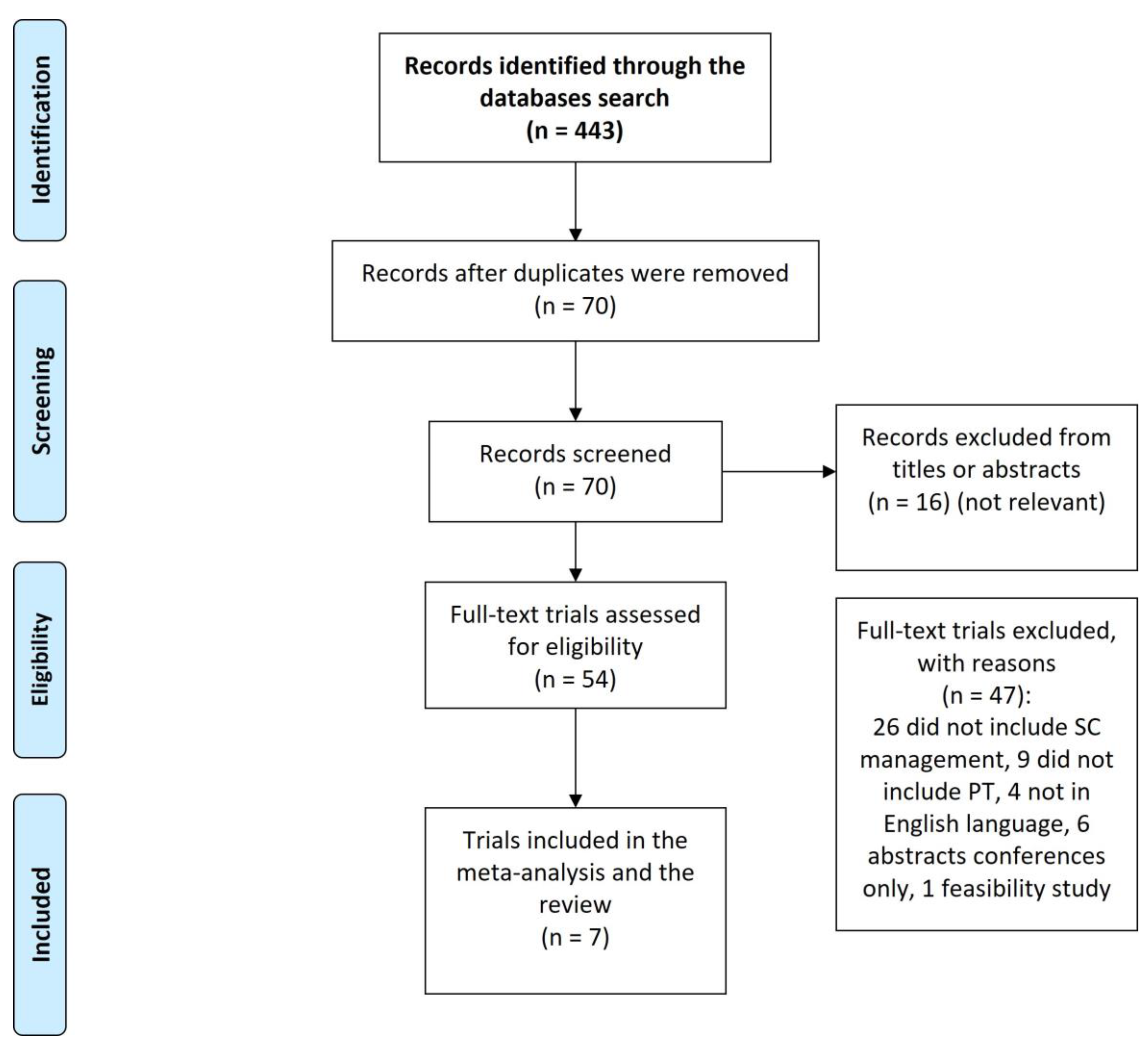
2. Method
2.1. Design
2.2. Study Protocol
2.3. Search Strategy
2.3.1. Keywords Used
2.3.2. Inclusion/Exclusion Criteria for the Articles
2.3.3. Study Selection
2.3.4. Data Extraction
3. Results
3.1. Opinions of PTs about Including SC Counselling in Their Practice
3.2. Prevalence of SC Counselling in Physiotherapy Practice
3.3. Barriers to Including SC Counselling in PTs Practice
3.3.1. Lack of Knowledge
3.3.2. Lack of Training
3.3.3. Lack of Time
3.3.4. Other Barriers
4. Discussion
5. Limitation
6. Conclusions
Authors’ Contribution
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. WHO Report on the Global Tobacco Epidemic, 2021: Addressing New and Emerging Products; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Office of National Statistics. Adult Smoking Habits in the UK: 2017. Office of National Statistics Accessed, 2018. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandlifeexpectancies/bulletins/adultsmokinghabitsingreatbritain/2017 (accessed on 30 December 2018).
- Cornish, D.; Brookman, A.; Horton, M.; Scanlon, S. Adult Smoking Habits in the UK: 2018; Office For National Statistics: Office For National Statistics: London, UK, 2019.
- Jamal, A.; King, B.A.; Neff, L.J.; Whitmill, J.; Babb, S.D.; Graffunder, C.M. Current cigarette smoking among adults—United States, 2005–2015. Morb. Mortal. Wkly. Rep. 2016, 65, 1205–1211. [Google Scholar] [CrossRef] [PubMed]
- US Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General; US Department of Health and Human Services, Centers for Disease: Atlanta, GA, USA, 2014.
- Darabseh, M.Z.; Selfe, J.; Morse, C.I.; Degens, H. Impact of vaping and smoking on maximum respiratory pressures and respiratory function. Int. J. Adolesc. Youth 2021, 26, 421–431. [Google Scholar] [CrossRef]
- Misigoj-Durakovic, M.; Bok, D.; Soric, M.; Dizdar, D.; Durakovic, Z.; Jukic, I. The effect of cigarette smoking history on muscular and cardiorespiratory endurance. J. Addict. Dis. 2012, 31, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Lauria, V.T.; Sperandio, E.F.; De Sousa TL, W.; de Oliveira Vieira, W.; Romiti, M.; de Toledo Gagliardi, A.R.; AraNtes, R.L.; Dourado, V.Z. Evaluation of dose–response relationship between smoking load and cardiopulmonary fitness in adult smokers: A cross-sectional study. Rev. Port. Pneumol. 2006 2017, 23, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Groppelli, A.; Giorgi, D.; Omboni, S.; Parati, G.; Mancia, G. Persistent blood pressure increase induced by heavy smoking. J. Hypertens. 1992, 10, 495–499. [Google Scholar] [CrossRef]
- Young, R.P.; Hopkins, R.J.; Smith, M.; Hogarth, D.K. Smoking cessation: The potential role of risk assessment tools as motivational triggers. Postgrad. Med. J. 2010, 86, 26–33. [Google Scholar] [CrossRef]
- Cahill, K.; Lindson-Hawley, N.; Thomas, K.H.; Fanshawe, T.R.; Lancaster, T. Nicotine receptor partial agonists for smoking cessation. Cochrane Database Syst. Rev. 2016, 5, 78–169. [Google Scholar] [CrossRef]
- Guilmette, T.J.; Motta, S.I.; Shadel, W.G.; Mukand, J.; Niaura, R. Promoting smoking cessation in the rehabilitation setting. Am. J. Phys. Med. Rehabil. 2001, 80, 560–562. [Google Scholar] [CrossRef]
- Hughes, J.R. How confident should we be that smoking cessation treatments work? Addiction 2009, 104, 1637–1640. [Google Scholar] [CrossRef]
- US Department of Health and Human Services. The Health Consequences of Smoking: A Report of the Surgeon General; US Department of Health and Human Services, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2004.
- Norman, G.J.; Velicer, W.F.; Fava, J.L.; Prochaska, J.O. Dynamic typology clustering within the stages of change for smoking cessation. Addict. Behav. 1998, 23, 139–153. [Google Scholar] [CrossRef]
- Prochaska, J.O.; Goldstein, M.G. Process of smoking cessation: Implications for clinicians. Clin. Chest Med. 1991, 12, 727–735. [Google Scholar] [CrossRef] [PubMed]
- Chase, E.C.; McMenamin, S.B.; Halpin, H.A. Medicaid provider delivery of the 5A’s for smoking cessation counseling. N& T. 2007, 9, 1095–1101. [Google Scholar]
- US Department of Health and Human Services. A Report of the Surgeon General, Editor the Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General; Citeseer: Princeton, NJ, USA, 2014.
- Powell, J.T. Vascular damage from smoking: Disease mechanisms at the arterial wall. Vasc. Med. 1998, 3, 21–28. [Google Scholar] [CrossRef]
- Leow, Y.-H.; Maibach, H.I. Cigarette smoking, cutaneous vasculature, and tissue oxygen. Clin. Dermatol. 1998, 16, 579–584. [Google Scholar] [CrossRef]
- Everson, E.S.; Taylor, A.H.; Ussher, M. Determinants of physical activity promotion by smoking cessation advisors as an aid for quitting: Support for the Transtheoretical Model. Patient Educ. Couns. 2010, 78, 53–56. [Google Scholar] [CrossRef]
- Bodner, M.E.; Miller, W.C.; Rhodes, R.E.; Dean, E. Smoking Cessation and Counseling: Knowledge and Views of Canadian Physical Therapists. Phys. Ther. 2011, 91, 1051–1062. [Google Scholar] [CrossRef]
- Luxton, N.; Redfern, J. The Role of Physiotherapists in Smoking Cessation; Elsevier: Amsterdam, The Netherlands, 2020. [Google Scholar]
- Lein, D.H., Jr.; Clark, D.; Graham, C.; Perez, P.; Morris, D. A model to integrate health promotion and wellness in physical therapist practice: Development and validation. Phys. Ther. 2017, 97, 1169–1181. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Schardt, C.; Adams, M.B.; Owens, T.; Keitz, S.; Fontelo, P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med. Inform. Decis. Mak. 2007, 7, 16. [Google Scholar] [CrossRef]
- Balfour, C. Physiotherapists and smoking cessation. Physiotherapy 1993, 79, 247–250. [Google Scholar] [CrossRef]
- Bodner, M.E.; Rhodes, R.E.; Miller, W.C.; Dean, E. Smoking cessation and counseling: Practices of Canadian physical therapists. Am. J. Prev. Med. 2012, 43, 67–71. [Google Scholar] [CrossRef] [PubMed]
- McCleary, R.E.; Johnson, G.M.; Skinner, M. Physiotherapists’ knowledge and uptake of the ABC approach to smoking cessation. N. Zealand J. Physiother. 2012, 40, 71–75. [Google Scholar]
- Pignataro, R.M.; Gurka, M.J.; Jones, D.L.; Kershner, R.E.; Ohtake, P.J.; Stauber, W.T.; Swisher, A.K. Tobacco Cessation Counseling Training in US Entry-Level Physical Therapist Education Curricula: Prevalence, Content, and Associated Factors. Phys. Ther. 2014, 94, 1294–1305. [Google Scholar] [CrossRef] [PubMed]
- Pignataro, R.M. Tobacco cessation counseling within physical therapist practice: Results of a statewide survey of Florida physical therapists. Physiother. Theory Pract. 2017, 33, 131–137. [Google Scholar] [CrossRef]
- Bodner, M.E.P.; Rhodes, R.E.P.; Miller, W.C.O.T.P.; Dean, E.P.T.P. Predictors of physical therapists’ intentions to counsel for smoking cessation: Implications for practice and professional education. Physiother. Theory Pract. 2020, 36, 628–637. [Google Scholar] [CrossRef]
- Gorin, S.S.; Heck, J.E. Meta-analysis of the efficacy of tobacco counseling by health care providers. Cancer Epidemiol. Biomark. Prev. 2004, 13, 2012–2022. [Google Scholar] [CrossRef]
- Charlesworth, L.; Hutton, D.; Hussain, H. Therapeutic Radiographers’ perceptions of the barriers and enablers to effective smoking cessation support. Radiography 2019, 25, 121–128. [Google Scholar] [CrossRef]
- Fiore, M. Smoking Cessation; US Department of Health and Human Services, Public Health Service, Agency: Washington, DC, USA, 1996.
- Fleetham, J.A. Introduction. Thorax 1998, 53 (Suppl. 3), S1. [Google Scholar] [CrossRef]
- Fiore, M.C.; Bailey, W.C.; Cohen, S.J. Treating Tobacco Use and Dependence: Clinical Practice Guideline; US Department of Health and Human Services, Public Health Service: Rockville, MD, USA, 2000.
- World Health Organization. Toolkit for Delivering the 5A’s and 5R’s Brief Tobacco Interventions to TB Patients in Primary Care; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Dean, E.; Jones, A.; Yu, H.P.-M.; Gosselink, R.; Skinner, M. Translating COVID-19 Evidence to Maximize Physical Therapists’ Impact and Public Health Response. Phys. Ther. 2020, 100, 1458–1464. [Google Scholar] [CrossRef]
- World Health Organization. WHO Global Report on Trends in Prevalence of Tobacco Use 2000–2025; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
| Population | Intervention | Comparison | Outcome Measures |
|---|---|---|---|
| “Physiotherapy” OR “physiotherapist” OR “physiotherapists” OR “physical therapy” OR “Physical therapists” OR “Physical therapist” | “Smoking cessation” OR “smoking cessation interventions” OR “quit smoking” OR “stop smoking” OR “tobacco cessation” OR “smoking abstinence” OR “vape” OR “vaping” OR “e-cigarette” OR “e-cig” OR “electronic cigarette”. | No physiotherapy intervention | Success of cessation |
| Author (Year) | Sample Size | Study Design | Study Goals | Key Findings |
|---|---|---|---|---|
| Balfour (1993) [27] | 63 PTs | Cross-sectional postal survey |
|
|
| Bonder et al. (2011) [22] | 738 PTs | Cross-sectional postal survey |
|
|
| Bonder et al. (2012) [28] | 738 PTs | Cross-sectional postal survey |
|
|
| McCleary et al. (2012) [29] | 602 PTs | Cross-sectional postal survey |
|
|
| Pignataro et al. (2014) [30] | 146 PT programme directors | Cross-sectional online survey |
|
|
| Pignataro et al. (2017) [31] | 212 PTs | Cross-sectional online survey |
|
|
| Bonder et al. (2020) [32] | 738 PTs | Cross-sectional postal survey |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Darabseh, M.Z.; Aburub, A.; Fayed, E.E. The Role of Physiotherapists in Smoking Cessation Management: A Scoping Review. Healthcare 2023, 11, 336. https://doi.org/10.3390/healthcare11030336
Darabseh MZ, Aburub A, Fayed EE. The Role of Physiotherapists in Smoking Cessation Management: A Scoping Review. Healthcare. 2023; 11(3):336. https://doi.org/10.3390/healthcare11030336
Chicago/Turabian StyleDarabseh, Mohammad Z., Aseel Aburub, and Eman E. Fayed. 2023. "The Role of Physiotherapists in Smoking Cessation Management: A Scoping Review" Healthcare 11, no. 3: 336. https://doi.org/10.3390/healthcare11030336
APA StyleDarabseh, M. Z., Aburub, A., & Fayed, E. E. (2023). The Role of Physiotherapists in Smoking Cessation Management: A Scoping Review. Healthcare, 11(3), 336. https://doi.org/10.3390/healthcare11030336







