Prevalence and Factors Associated with Maternal Postpartum Depression among Mothers in Saudi Arabia: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Setting, and Population
2.2. Sampling Procedure
2.3. Data Collection and Study Tool
2.4. Data Analysis
2.5. Ethical Considerations
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zinga, D.; Phillips, S.D.; Born, L. Postpartum depression: We know the risks, can it be prevented? Braz. J. Psychiatry 2005, 27, s56–s64. [Google Scholar] [CrossRef] [PubMed]
- O’Hara, M.W. Postpartum depression: What we know. J. Clin. Psychol. 2009, 65, 1258–1269. [Google Scholar] [CrossRef] [PubMed]
- Epperson, C.N.; Huang, M.-Y.; Cook, K.; Gupta, D.; Chawla, A.; Greenberg, P.E.; Eldar-Lissai, A. Healthcare resource utilization and costs associated with postpartum depression among commercially insured households. Curr. Med. Res. Opin. 2020, 36, 1707–1716. [Google Scholar] [CrossRef] [PubMed]
- Stewart, D.E.; Robertson, E.; Dennis, C.-L.; Grace, S.L.; Wallington, T. Postpartum Depression: Literature Review of Risk Factors and Interventions; Program for Toronto Public Health. University Health Network Women’s Health: Toronto, ON, Canada, 2003; pp. 1–289. [Google Scholar]
- Lobel, M.; Ibrahim, S.M. Emotions and mental health during pregnancy and postpartum. Women’s Reprod. Health 2018, 5, 13–19. [Google Scholar] [CrossRef]
- Alasoom, L.I.; Koura, M.R. Predictors of postpartum depression in the eastern province capital of Saudi Arabia. J. Fam. Med. Prim. Care 2014, 3, 146. [Google Scholar]
- Bina, R. The impact of cultural factors upon postpartum depression: A literature review. Health Care Women Int. 2008, 29, 568–592. [Google Scholar] [CrossRef]
- Upadhyay, R.P.; Chowdhury, R.; Salehi, A.; Sarkar, K.; Singh, S.K.; Sinha, B.; Pawar, A.; Rajalakshmi, A.K.; Kumar, A. Postpartum depression in India: A systematic review and meta-analysis. Bull. World Health Organ. 2017, 95, 706. [Google Scholar] [CrossRef]
- Mathisen, S.E.; Glavin, K.; Lien, L.; Lagerløv, P. Prevalence and risk factors for postpartum depressive symptoms in Argentina: A cross-sectional study. Int. J. Women’s Health 2013, 5, 787. [Google Scholar] [CrossRef]
- Klainin, P.; Arthur, D.G. Postpartum depression in Asian cultures: A literature review. Int. J. Nurs. Stud. 2009, 46, 1355–1373. [Google Scholar] [CrossRef]
- Agoub, M.; Moussaoui, D.; Battas, O. Prevalence of postpartum depression in a Moroccan sample. Arch. Women’s Ment. Health 2005, 8, 37–43. [Google Scholar] [CrossRef]
- Chaaya, M.; Campbell, O.; El Kak, F.; Shaar, D.; Harb, H.; Kaddour, A. Postpartum depression: Prevalence and determinants in Lebanon. Arch. Women’s Ment. Health 2002, 5, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, K.; Gamble, J.; Creedy, D. Prevalence and factors associated with the development of antenatal and postnatal depression among Jordanian women. Midwifery 2011, 27, e238–e245. [Google Scholar] [CrossRef] [PubMed]
- Al Dallal, F.; Grant, I. Postnatal depression among Bahraini women: Prevalence of symptoms and psychosocial risk factors. East. Mediterr. Health J. 2012, 18, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Bener, A.; Burgut, F.T.; Ghuloum, S.; Sheikh, J. A study of postpartum depression in a fast developing country: Prevalence and related factors. Int. J. Psychiatry Med. 2012, 43, 325–337. [Google Scholar] [CrossRef]
- Pataky, E.A.; Ehlert, U. Longitudinal assessment of symptoms of postpartum mood disorder in women with and without a history of depression. Arch. Women’s Ment. Health 2020, 23, 391–399. [Google Scholar] [CrossRef]
- Taherifard, P.; Delpisheh, A.; Shirali, R.; Afkhamzadeh, A.; Veisani, Y. Socioeconomic, psychiatric and materiality determinants and risk of postpartum depression in border city of Ilam, Western Iran. Depress. Res. Treat. 2013, 2013, 653471. [Google Scholar] [CrossRef]
- Josefsson, A.; Angelsiöö, L.; Berg, G.; Ekström, C.-M.; Gunnervik, C.; Nordin, C.; Sydsjö, G. Obstetric, somatic, and demographic risk factors for postpartum depressive symptoms. Obstet. Gynecol. 2002, 99, 223–228. [Google Scholar] [PubMed]
- Alharbi, A.A.; Abdulghani, H.M. Risk factors associated with postpartum depression in the Saudi population. Neuropsychiatr. Dis. Treat. 2014, 10, 311–316. [Google Scholar] [PubMed]
- Corrigan, C.P.; Kwasky, A.N.; Groh, C.J. Social support, postpartum depression, and professional assistance: A survey of mothers in the Midwestern United States. J. Perinat. Educ. 2015, 24, 48–60. [Google Scholar] [CrossRef] [PubMed]
- Reid, K.M.; Taylor, M.G. Social support, stress, and maternal postpartum depression: A comparison of supportive relationships. Soc. Sci. Res. 2015, 54, 246–262. [Google Scholar] [CrossRef]
- Azale, T.; Fekadu, A.; Hanlon, C. Treatment gap and help-seeking for postpartum depression in a rural African setting. BMC Psychiatry 2016, 16, 196. [Google Scholar] [CrossRef] [PubMed]
- Sword, W.; Busser, D.; Ganann, R.; McMillan, T.; Swinton, M. Women’s care-seeking experiences after referral for postpartum depression. Qual. Health Res. 2008, 18, 1161–1173. [Google Scholar] [CrossRef] [PubMed]
- Chrzan-Dętkoś, M.; Murawska, N.; Walczak-Kozłowska, T. ‘Next Stop: Mum’: Evaluation of a Postpartum Depression Prevention Strategy in Poland. Int. J. Environ. Res. Public Health 2022, 19, 11731. [Google Scholar] [CrossRef] [PubMed]
- Ochsenwald, W.L.; Teitelbaum, J. “Saudi Arabia”. Encyclopedia Britannica. Available online: https://www.britannica.com/place/Saudi-Arabia (accessed on 22 November 2022).
- Almutairi, A.F.; Salam, M.; Alanazi, S.; Alweldawi, M.; Alsomali, N.; Alotaibi, N. Impact of help-seeking behavior and partner support on postpartum depression among Saudi women. Neuropsychiatr. Dis. Treat. 2017, 13, 1929–1936. [Google Scholar] [CrossRef] [PubMed]
- Abdollahi, F.; Etemadinezhad, S.; Lye, M.-S. Postpartum mental health in relation to sociocultural practices. Taiwan. J. Obstet. Gynecol. 2016, 55, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Schleyer, T.K.; Forrest, J.L. Methods for the design and administration of web-based surveys. J. Am. Med. Inform. Assoc. 2000, 7, 416–425. [Google Scholar] [CrossRef]
- Wyatt, J.C. When to use web-based surveys. J. Am. Med. Inform. Assoc. 2000, 7, 426–430. [Google Scholar] [CrossRef]
- Dankner, R.; Goldberg, R.P.; Fisch, R.Z.; Crum, R.M. Cultural elements of postpartum depression. A study of 327 Jewish Jerusalem women. J. Reprod. Med. 2000, 45, 97–104. [Google Scholar]
- Halbreich, U.; Karkun, S. Cross-cultural and social diversity of prevalence of postpartum depression and depressive symptoms. J. Affect. Disord. 2006, 91, 97–111. [Google Scholar] [CrossRef]
- Ing, H.; Fellmeth, G.; White, J.; Stein, A.; Simpson, J.A.; McGready, R. Validation of the Edinburgh Postnatal Depression Scale (EPDS) on the Thai-Myanmar border. Trop. Doctor 2017, 47, 339–347. [Google Scholar] [CrossRef]
- Ta Park, V.M.; Goyal, D.; Nguyen, T.; Lien, H.; Rosidi, D. Postpartum traditions, mental health, and help-seeking considerations among Vietnamese American women: A mixed-methods pilot study. J. Behav. Health Serv. Res. 2017, 44, 428–441. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Categories | Frequency | % |
|---|---|---|---|
| Nationality | Saudi | 439 | 98.9 |
| Non-Saudi | 5 | 1.1 | |
| Marital status | Married | 430 | 96.8 |
| Divorced | 8 | 1.8 | |
| Widow | 6 | 1.4 | |
| Age group (years) | 24 or less | 129 | 29.1 |
| 25–39 | 267 | 60.1 | |
| 40–54 | 48 | 10.8 | |
| Number of deliveries | 1 | 140 | 31.5 |
| 2 | 115 | 25.9 | |
| 3 | 75 | 16.9 | |
| 4 | 47 | 10.6 | |
| 5 | 34 | 7.7 | |
| More than 5 | 33 | 7.4 | |
| Last delivery | <1 month | 38 | 8.6 |
| <6 months | 117 | 26.4 | |
| <12 months | 289 | 65.1 | |
| Working status | Housewife | 292 | 65.8 |
| Working outside | 152 | 34.2 | |
| Monthly income | less than 5000 | 178 | 40.1 |
| 5000–9999 | 168 | 37.8 | |
| 10,000–14,999 | 79 | 17.8 | |
| 15,000–19,999 | 11 | 2.5 | |
| 20,000 or more | 8 | 1.8 |
| Variables | Categories | N | % |
|---|---|---|---|
| Prevalence of PPD using EPDS | Having the symptoms | 336 | 75.7 |
| Free of the symptoms | 108 | 24.3 | |
| Thought of harming self | Never | 359 | 80.9 |
| Hardly ever | 35 | 7.9 | |
| Sometimes | 22 | 4.95 | |
| Yes, quite often | 28 | 6.3 | |
| Duration of PPD symptoms among mothers | less than month | 150 | 34.8 |
| less than 6 months | 92 | 20.8 | |
| less than 1 year | 58 | 13.1 | |
| None | 144 | 32.4 | |
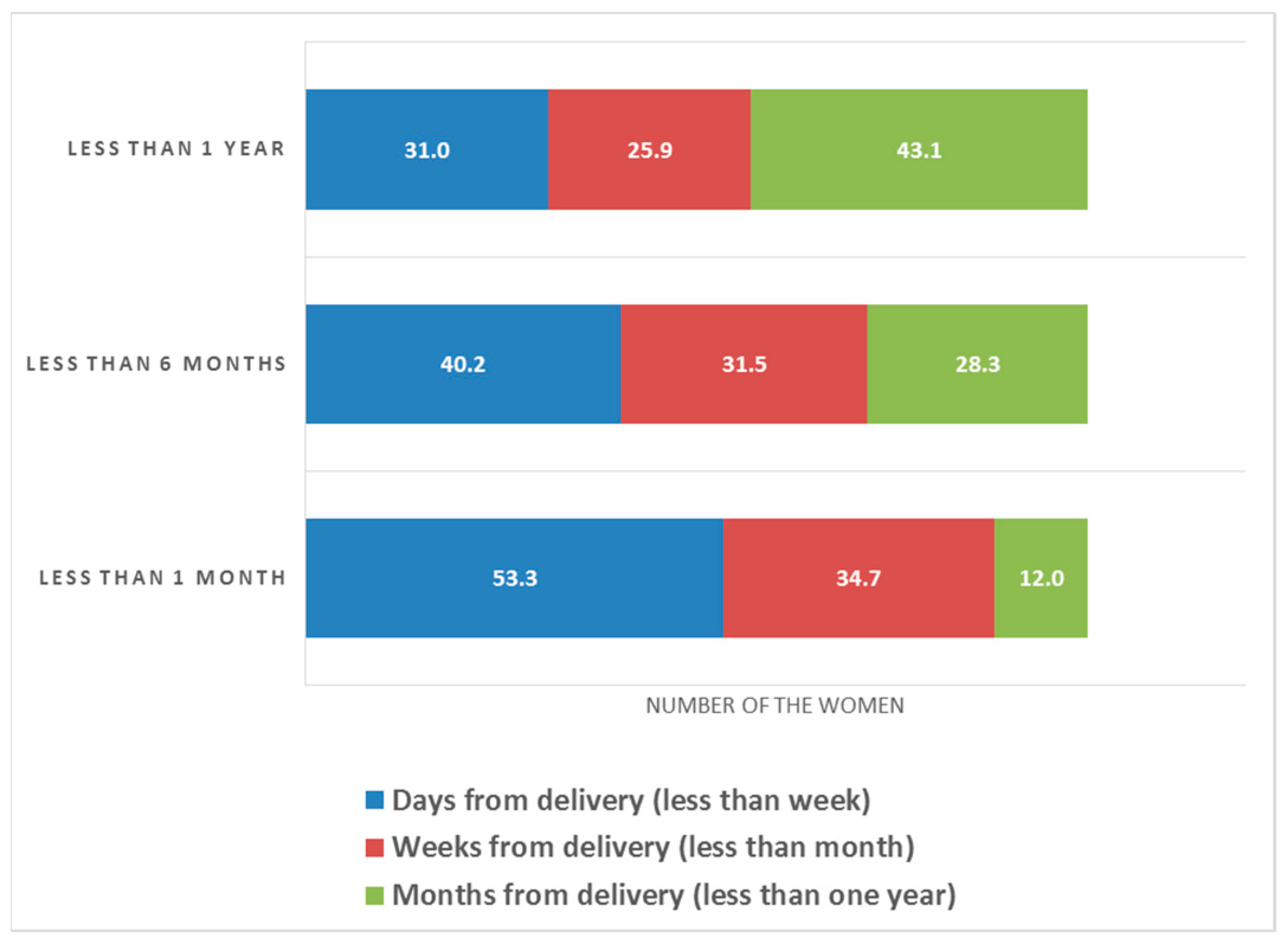
| Onset of symptoms | Days from delivery (less than a week) | 135 | 30.4 |
| Weeks from delivery (less than a month) | 96 | 21.6 | |
| Months from delivery (less than one year) | 69 | 15.5 | |
| Had the symptoms previously after delivery | Yes | 227 | 51.1 |
| No | 217 | 48.9 | |
| More than 5 | 12 | 2.6 | |
| Number of deliveries with symptoms | First delivery | 131 | 29.6 |
| Others | 128 | 28.8 | |
| First delivery + other | 185 | 41.6 | |
| Had the symptoms previously after delivery and now depressed | Yes | 389 | 87.7 |
| No | 280 | 63.1 | |
| Ask for health care (psychology) | Yes | 30 | 6.8 |
| No | 414 | 93.2 | |
| Follow-up of therapy | Yes | 311 | 70.0 |
| No | 133 | 30.0 | |
| Compliance with follow-up visiting | Yes | 252 | 56.7 |
| No | 192 | 43.3 | |
| Type of health institutions visited | Primary Health Care Centre (PHC) | 119 | 26.7 |
| General hospital | 119 | 26.7 | |
| Private clinic | 207 | 46.7 |
| Risk Factors | Variable | % | PPD Symptoms (%) EPDS ≥ 10 | OR | p-Value |
|---|---|---|---|---|---|
| Delivery type | Normal | 77.25 | 74.6 | 1.3 | 0.347 |
| Cesarean | 22.75 | 79.2 | |||
| Severe complications during delivery | Yes | 11 | 83.7 | 0.5 | 0.167 |
| No | 89 | 74.7 | |||
| Gestational diabetes | Yes | 7.21 | 81.3 | 0.7 | 0.441 |
| No | 92.79 | 75.0 | |||
| Anemia during pregnancy | Yes | 34.68 | 79.2 | 0.7 | 0.191 |
| No | 65.32 | 73.1 | |||
| Family support | Yes | 81.98 | 71.7 | 5.9 | <0.001 |
| No | 18.02 | 93.8 | |||
| Unexpected pregnancy | Yes | 52.03 | 68.0 | 2.5 | <0.001 |
| No | 47.97 | 84.0 | |||
| Un-expected gender | Yes | 41.00 | 72.0 | 1.4 | 0.112 |
| No | 59.00 | 78.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdelmola, A.O.; Bahari, A.; Gosadi, I.; Aburasain, K.S.; Osaisi, N.A.; Jilan, N.S.; Alsanosy, S.R.; Mahnashi, H.A.; Gadri, H.F.; Khobrani, A.A.; et al. Prevalence and Factors Associated with Maternal Postpartum Depression among Mothers in Saudi Arabia: A Cross-Sectional Study. Healthcare 2023, 11, 343. https://doi.org/10.3390/healthcare11030343
Abdelmola AO, Bahari A, Gosadi I, Aburasain KS, Osaisi NA, Jilan NS, Alsanosy SR, Mahnashi HA, Gadri HF, Khobrani AA, et al. Prevalence and Factors Associated with Maternal Postpartum Depression among Mothers in Saudi Arabia: A Cross-Sectional Study. Healthcare. 2023; 11(3):343. https://doi.org/10.3390/healthcare11030343
Chicago/Turabian StyleAbdelmola, Amani Osman, Ahmed Bahari, Ibrahim Gosadi, Khdeeja Shami Aburasain, Njoud Ali Osaisi, Nidaa Sameer Jilan, Sarah Rashad Alsanosy, Haneen Ali Mahnashi, Hadeel Fuad Gadri, Amnah Ahmad Khobrani, and et al. 2023. "Prevalence and Factors Associated with Maternal Postpartum Depression among Mothers in Saudi Arabia: A Cross-Sectional Study" Healthcare 11, no. 3: 343. https://doi.org/10.3390/healthcare11030343
APA StyleAbdelmola, A. O., Bahari, A., Gosadi, I., Aburasain, K. S., Osaisi, N. A., Jilan, N. S., Alsanosy, S. R., Mahnashi, H. A., Gadri, H. F., Khobrani, A. A., Darraj, A. A., Mahfouz, M. S., Kariri, H. D. H., & Abdelwahab, S. I. (2023). Prevalence and Factors Associated with Maternal Postpartum Depression among Mothers in Saudi Arabia: A Cross-Sectional Study. Healthcare, 11(3), 343. https://doi.org/10.3390/healthcare11030343







