Factors Influencing the Aged in the Use of Mobile Healthcare Applications: An Empirical Study in China
Abstract
:1. Introduction
1.1. Background
1.2. Research Purpose
2. Literature Research
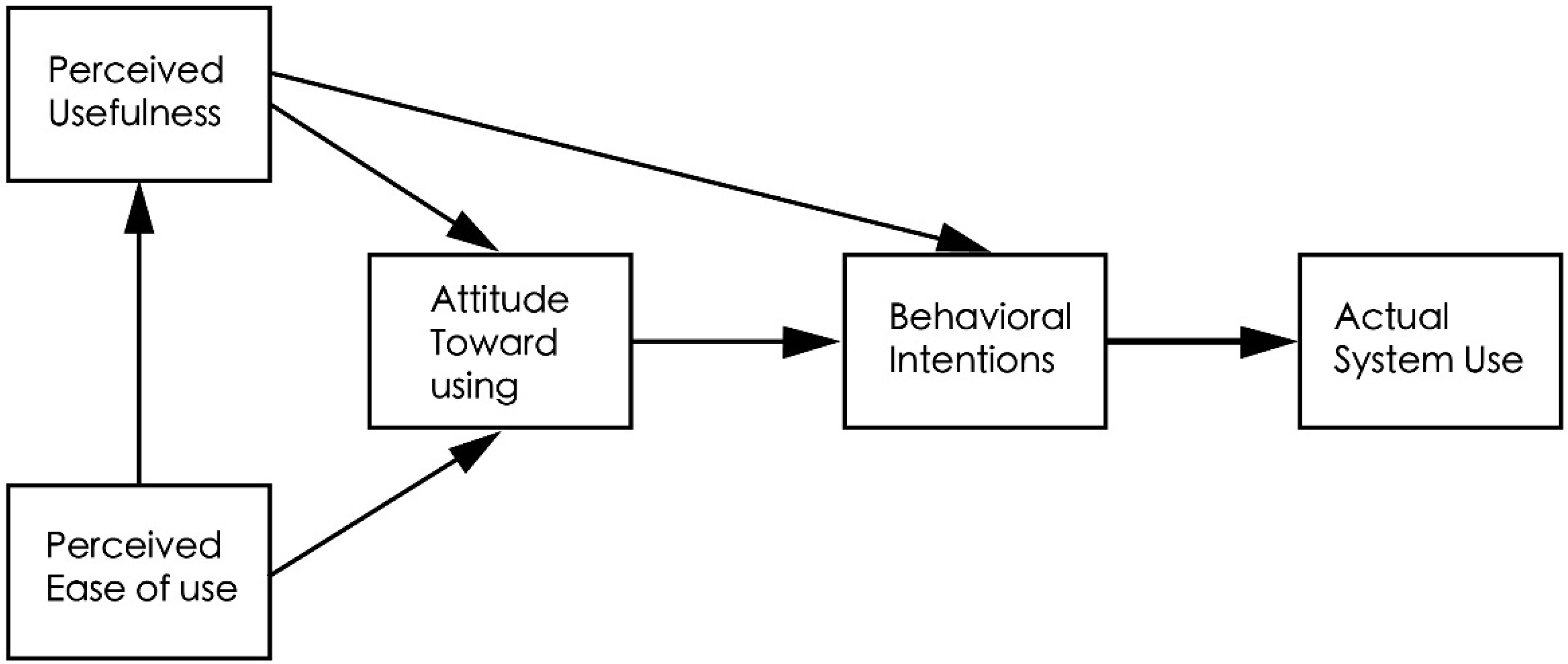
2.1. Technology Acceptance Model (TAM)
2.2. Protection Motivation Theory (PMT)
2.3. Perceived Risk Theory
3. Model Building and Hypotheses
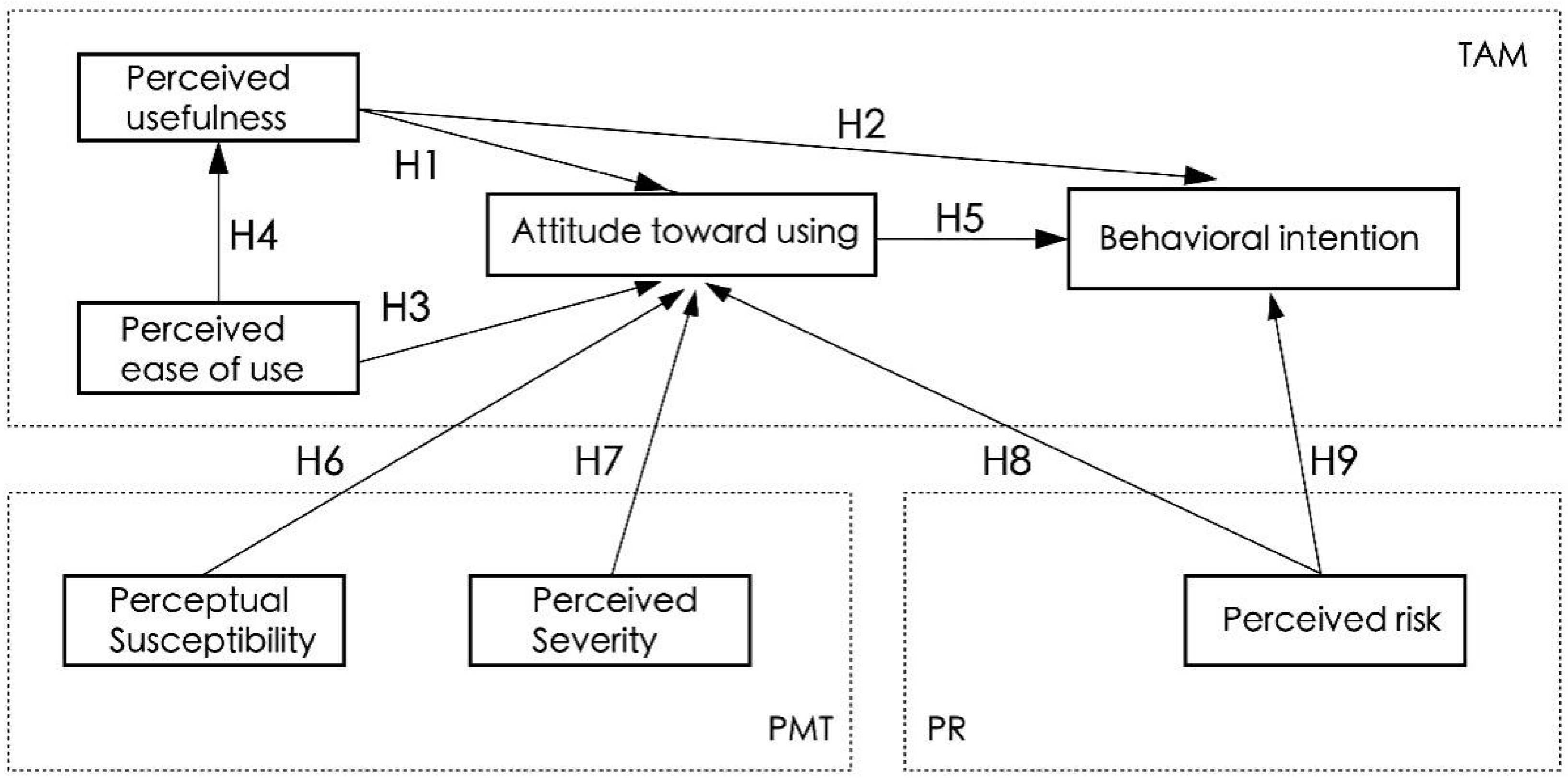
3.1. Research Hypotheses
3.1.1. Relation among Perceived Usefulness, Attitude toward Using Mobile Healthcare Applications, and Behavioral Intention
3.1.2. Relation between Perceived Ease of Use and Attitude toward Using Mobile Healthcare Applications
3.1.3. Relation between Perceived Ease of Use and Perceived Usefulness
3.1.4. Relation between Attitude toward Using Mobile Healthcare Applications and Behavioral Intention
3.1.5. Relation among Perceived Susceptibility, Perceived Severity, and Attitude toward Using Mobile Healthcare Applications
3.1.6. Relation between Perceived Risk and Attitude toward Using Mobile Healthcare Applications
3.2. Model Building
3.3. Variable Definition and Measurement
4. Empirical Analysis
4.1. Questionnaire Design
4.2. Descriptive Statistics
4.3. Scale Reliability Analysis
4.4. Scale Validity Analysis
4.4.1. KMO and Bartlett Tests
4.4.2. Exploratory Factor Analysis
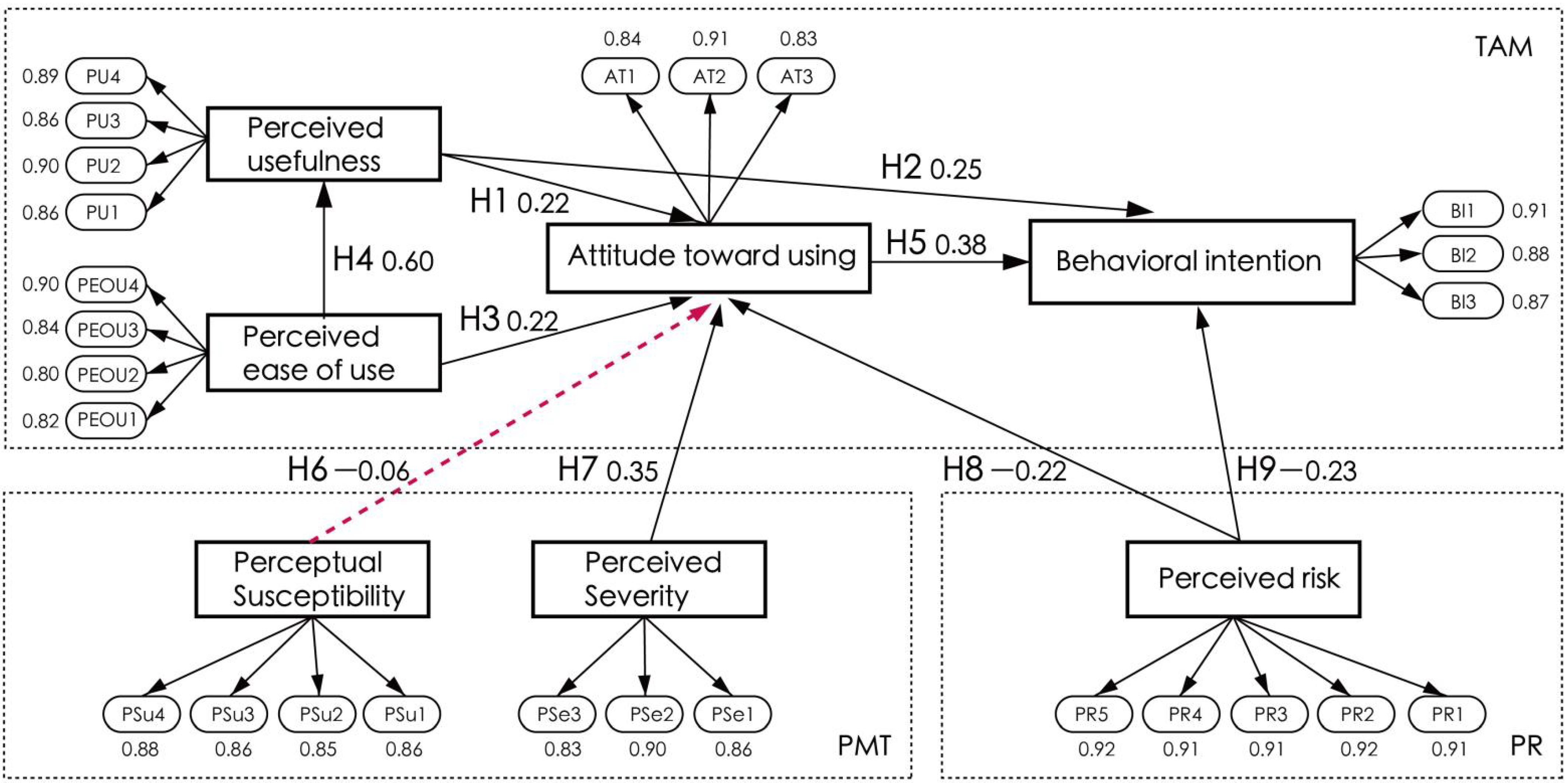
4.5. Measurement Model
4.5.1. Convergent Validity
4.5.2. Discriminant Validity
4.6. Structural Model Analysis
4.6.1. Model Fit Criteria
4.6.2. Path Analysis
4.7. Hypothesis Explanation
5. Results and Discussion
6. Suggestions and Conclusions
6.1. Suggestions
6.1.1. Promote the Usefulness and Ease of Use of mHealthcare Apps
6.1.2. Strengthen the Efforts on the Publicity of mHealthcare Apps
6.1.3. Reduce the Risks of Using mHealthcare Apps
6.2. Conclusions
7. Limitations and Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tong, Y.F. The latest developments and trends of China’s population—Analysis combined with the data of the seventh national census. J. China Inst. Labor Relat. 2021, 35, 15–25. [Google Scholar]
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development; General Assembly: Vienna, Austria, 2015. [Google Scholar]
- Gu, Y. Research on the Design of Mobile Health Care Platform for the Elderly. Master’s Thesis, Jiangnan University, Wuxi, China, 2014. [Google Scholar]
- Han, X.D.; Jin, X.Z. Research on mobile health service demand of urban elderly. Smart Heal. 2016, 12, 7–12. [Google Scholar]
- Qin, M.D.; Wang, K.Y.; Chen, C.X. Analysis on the status quo of demand for mobile health services for the elderly. Mod. Hosp. 2022, 6, 935–937. [Google Scholar]
- Office of the State Council. Guiding Opinions of the General Office of the State Council on Promoting the Healthy Development of the Pharmaceutical Industry. Available online: http://www.gov.cn/zhengce/content/2016-03/11/content_5052267.htm (accessed on 16 December 2022).
- Guo, X.Y.; Gong, M.S.; Shu, H.M. Mobile health app design strategy for the elderly with chronic diseases. Design 2017, 15, 128–130. [Google Scholar]
- Junaid, S.B.; Imam, A.A.; Balogun, A.O.; De Silva, L.C.; Surakat, Y.A.; Kumar, G.; Abdulkarim, M.; Shuaibu, A.N.; Garba, A.; Sahalu, Y. Recent advancements in emerging technologies for healthcare management systems: A survey. Healthcare 2022, 10, 1940. [Google Scholar] [CrossRef]
- Istepanian, R.S. Mobile health (m-health) in retrospect: The known unknowns. Int. J. Environ. Res. Public Health. 2022, 19, 3747. [Google Scholar] [CrossRef]
- Liu, Y.; Liang, Z.; Li, C.; Guo, J.; Zhao, G. An investigation into the adoption behavior of mhealth users: From the perspective of the push-pull-mooring framework. Sustainability 2022, 14, 14372. [Google Scholar] [CrossRef]
- Xiang, J.; Zhao, A.; Tian, G.Y.; Woo, W.; Liu, L.; Li, H. Prospective RFID sensors for the IoT healthcare system. J. Sens. 2022, 2022, 1–19. [Google Scholar] [CrossRef]
- Garnweidner-Holme, L.M.; Borgen, I.; Garitano, I.; Noll, J.; Lukasse, M. Designing and Developing a Mobile Smartphone Application for Women with Gestational Diabetes Mellitus Followed-Up at Diabetes Outpatient Clinics in Norway. Healthcare 2015, 3, 310–323. [Google Scholar] [CrossRef] [Green Version]
- Cano-de-la-Cuerda, R.; Jiménez-Antona, C.; Melián-Ortiz, A.; Molero-Sánchez, A.; Gil-de Miguel, Á.; Lizcano-Álvarez, Á.; Hernández-Barrera, V.; Varillas-Delgado, D.; Laguarta-Val, S. Construct Validity and Test–Retest Reliability of a Free Mobile Application to Evaluate Aerobic Capacity and Endurance in Post-COVID-19 Syndrome Patients—A Pilot Study. J. Clin. Med. 2023, 12, 131. [Google Scholar] [CrossRef]
- Chaudhry, B.M.; Islam, A. A Mobile Application-Based Relational Agent as a Health Professional for COVID-19 Patients: Design, Approach, and Implications. Int. J. Environ. Res. Public Health 2022, 19, 13794. [Google Scholar] [CrossRef]
- Athaya, T.; Choi, S. Real-Time Cuffless Continuous Blood Pressure Estimation Using 1D Squeeze U-Net Model: A Progress toward mHealth. Biosensors 2022, 12, 655. [Google Scholar] [CrossRef]
- De Michele, R.; Furini, M. Iot healthcare: Benefits, issues and challenges. In Proceedings of the 5th EAI International Conference on Smart Objects and Technologies for Social Good, New York, NY, USA, 25 September 2019; pp. 160–164. [Google Scholar]
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 13, 319–339. [Google Scholar] [CrossRef] [Green Version]
- Jing, M.; Zhou, Y. Research on consumer online purchase behavior based on TAM model and perceived risk. Shanghai Manag. Sci. 2005, 5, 5–7. [Google Scholar]
- Zhu, D.G.; Guo, J.H. Research on user satisfaction of mobile government affairs based on TAM model. Inf. Sci. 2016, 34, 141–146. [Google Scholar] [CrossRef]
- Li, D.H.; Zhang, L.X. Research on influencing factors of tourism app download and use behavior based on TAM. Tour. J. 2015, 30, 26–34. [Google Scholar]
- Holden, R.J.; Karsh, B.T. The technology acceptance model: Its past and its future in health care. J. Biomed. Inform. 2010, 43, 159–172. [Google Scholar] [CrossRef] [Green Version]
- Tian, B.H. Research on Influencing Factors of Continuous Behavior Intention of “Chunyu Doctor” App Users. Master’s Thesis, Shanghai University of Finance and Economics, Shanghai, China, 2020. [Google Scholar]
- Yu, J.; Wang, Z.T.; Li, B. Analysis and prospect of information technology user acceptance research. J. Suihua Univ. 2011, 31, 60–61. [Google Scholar]
- Prentice-Dunn, S.; Rogers, R.W. Protection motivation theory and preventive health: Beyond the health belief model. Health Educ. Res. 1986, 1, 153–161. [Google Scholar] [CrossRef]
- Rogers, R.W. A protection motivation theory of fear appeals and attitude change. J. Psychol. 1975, 91, 93–114. [Google Scholar] [CrossRef]
- Johnston, A.C.; Warkentin, M. Fear appeals and information s ecurity behaviors: An empirical study. MIS Q. 2010, 34, 549–566. [Google Scholar] [CrossRef]
- Wang, Y.; Xiao, X.; Zheng, P.P.; Abdullah, A.; Fu, H. Application and development of conservation motivation theory in individual behavior change. China Health Educ. 2009, 25, 853–855+870. [Google Scholar]
- Anderson, C.L.; Agarwal, R. Practicing safe computing: A multimethod empirical examination of home computer user security behavioral intentions. MIS Q. 2010, 34, 613–643. [Google Scholar] [CrossRef] [Green Version]
- Bulgurcu, B.; Cavusoglu, H.; Benbasat, I. Information security policy compliance: An empirical study of rationality-based beliefs and information security awareness. MIS Q. 2010, 34, 523–548. [Google Scholar] [CrossRef] [Green Version]
- Yin, M.; Li, Q. Research on the use of health app users based on the theory of protection motivation. Mod. Intell. 2016, 36, 63–70. [Google Scholar]
- Bauer, R.A. Consumer behavior as risk-taking. In Dynamic Marketing for A Changing World; Hancock, R.S., Ed.; American Marketing Association: Chicago, IL, USA, 1960; pp. 389–398. [Google Scholar]
- Klaver, N.S.; Van de Klundert, J.; Askari, M. Relationship between perceived risks of using mHealth applications and the intention to use them among older adults in the Netherlands: Cross-sectional study. JMIR Mhealth Uhealth 2021, 9, e26845. [Google Scholar] [CrossRef]
- Sinha, M.; Fukey, L.; Balasubramanian, K.; Hanafiah, M.H.; Kunasekaran, P.; Ragavan, N.A. Acceptance of consumer-oriented health information technologies (CHITs): Integrating technology acceptance model with perceived risk. Informatica 2021, 45, 45–52. [Google Scholar] [CrossRef]
- Laili, F.N.; Wahyudi, L. Perceived Risk of Covid-19 and Trust on m-Health Transaction Intention. J. Bus. Manag. Stud. 2021, 3, 231–240. [Google Scholar] [CrossRef]
- Wu, J.; Li, S.S. A study on users’ willingness to use information services in online health communities. Inf. Sci. 2017, 35, 119–125. [Google Scholar] [CrossRef]
- Wang, Y.R.; Wang, Q.; Li, L.N.; Wang, K.; Liu, S.Q.; He, Q.; Zhang, R.Y. Survey on willingness to use mobile medical services and its influencing factors among diabetic patients. Chin. Gen. Pract. 2017, 20, 1619–1625. [Google Scholar]
- Wu, Y.M.; Zhang, M. Empirical research on sticky behavior of medical and health app users. Mod. Prev. Med. 2017, 44, 1083–1087. [Google Scholar]
- He, M.G.; Long, X.D. Research on the influence of perceived risk and trust on continuous use of mobile medical app——Based on ECM-ISC model. J. Commun. Rev. 2016, 1, 152–165. [Google Scholar]
- Pan, L. A Study on Tourists’ Adoption Behavior of Mobile Tourism Applications. Ph.D. Thesis, Xiamen University, Xiamen, China, 2017. [Google Scholar]
- Jiang, Q.Q.; Zhang, Z.H.; Xiong, J.J.; Zhu, J.F. Research on patients’ willingness to adopt “Internet + nursing service” based on technology acceptance model and planned behavior theory. PLA Nurs. J. 2022, 39, 42–45+50. [Google Scholar]
- Yu, Q.Z.; Ye, S.M.; Li, Y.; Zhong, Y.Y. Empirical research on behavioral intention of two-dimensional code based on TAM. Technol. Manag. Res. 2014, 9, 180–185. [Google Scholar]
- Luo, C.L.; Zhu, X.D. An empirical study on influencing factors of Yu’e Bao’s behavior intention based on TAM/TPB and perceived risk. Mod. Intell. 2015, 2, 143–149. [Google Scholar]
- Liu, L.L. Research on Influencing Factors of College Students’ E-learning Platform Intention Based on Technology Acceptance Model. Master’s Thesis, Zhejiang Normal University, Hangzhou, China, 2013. [Google Scholar]
- Huang, R. New retail consumption purchase decision-making intention——Based on TAM model research. J. Wuhan Bus. Univ. 2020, 34, 34–39. [Google Scholar] [CrossRef]
- Liu, C.J.; Chen, X.Q. An empirical study on the acceptance of staff information system of high star hotel based on DTPB model. Tour. J. 2010, 25, 79–85. [Google Scholar]
- Sun, Y.M.; Cao, S.Q. Analysis of college students’ BIM technology learning willingness based on technology acceptance model. Proj. Manag. Technol. 2021, 19, 70–76. [Google Scholar]
- Maddux, J.E.; Rogers, R.W. Protection motivation and self-efficacy: A revised theory of fear appeals and attitude change. J. Exp. Soc. Psychol. 1983, 19, 469–479. [Google Scholar] [CrossRef]
- Ma, Q.; Jing, K.J.; Liu, Y.Y. Construction of structural equation model of health beliefs affecting self-management behavior of diabetic patients. Nurs. Res. 2019, 33, 4294–4298. [Google Scholar]
- Yang, Q. Empirical Research on User Acceptance Behavior of Health Wechat Public Accounts. Master’s Thesis, Ji’nan University, Guangzhou, China, 2017. [Google Scholar]
- Sun, Z.M. Research on the Influencing Factors of Social Media Health Information Adoption. Ph.D. Thesis, Nanjing University, Nanjing, China, 2018. [Google Scholar]
- Guo, X.A.; Wang, T.Y. New media exposure, health beliefs and HPV vaccination intention. J. Commun. Stud. 2020, 27, 58–74+127. [Google Scholar]
- Taylor, J.W. The role of risk in consumer behavior. J. Mark. 1974, 38, 54–60. [Google Scholar] [CrossRef]
- Schnall, R.; Higgins, T.; Brown, W.; Carballo-Dieguez, A.; Bakken, S. Trust, perceived risk, perceived ease of use and perceived usefulness as factors related to mHealth technology use. Stud. Health Technol. Inform. 2015, 216, 467. [Google Scholar] [PubMed]
- Said, G.R.E. Factors Affecting mHealth Technology Adoption in Developing Countries: The Case of Egypt. Computers 2023, 12, 9. [Google Scholar] [CrossRef]
- Zhao, Y.; Ni, Q.; Zhou, R. What factors influence the mobile health service adoption? A meta-analysis and the moderating role of age. Int. J. Inf. Manag. 2018, 43, 342–350. [Google Scholar] [CrossRef]
- Zhang, B.W.; Jin, L.; Jin, X.Z. Empirical research on behavior willingness of mobile health service users. Smart Heal. 2017, 3, 6–12+17. [Google Scholar] [CrossRef]
- Ren, C.; Deng, C. Mobile health service user acceptance model and its empirical research. China Health Stat. 2014, 6, 1015–1018+1022. [Google Scholar]
- Stone, R.N.; Grønhaug, K. Perceived risk: Further considerations for the marketing discipline. Eur. J. Mark. 1993, 27, 39–50. [Google Scholar] [CrossRef]
- Wu, J.H.; Wang, S.C. What drives mobile commerce? An empirical evaluation of the revised technology acceptance model. Inf. Manag. 2005, 42, 719–729. [Google Scholar] [CrossRef]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Jackson, D.L.; Gillaspy, J.A.; Purc-Stephenson, R. Reporting practices in confirmatory factor analysis: An overview and some recommendations. Psychol. Methods 2009, 14, 6–23. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling; Guilford Publications: New York, NY, USA, 2015. [Google Scholar]
- Whittaker, T.A. A Beginner‘s Guide to Structural Equation Modeling; Taylor & Francis: Milton Park, UK, 2011. [Google Scholar]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Mohamed, A.H.H.; Tawfik, H.; Al-Jumeily, D.; Norton, L. MoHTAM: A technology acceptance model for mobile health applications. In 2011 Developments in E-systems Engineering; IEEE: Piscataway, NJ, USA, 2011; pp. 13–18. [Google Scholar]
- Saare, M.A.; Hussain, A.; Yue, W.S. Conceptualizing Mobile Health Application Use Intention and Adoption Among Iraqian Older Adults: From the Perspective of Expanded Technology Acceptance Model. Int. J. Interact. Mob. Technol. 2019, 13, 28–41. [Google Scholar] [CrossRef]
- Wildenbos, G.A.; Peute, L.; Jaspers, M. Aging barriers influencing mobile health usability for older adults: A literature based framework (MOLD-US). Int. J. Med. Inform. 2018, 114, 66–75. [Google Scholar] [CrossRef]
- Wang, L. Research on Mobile Health Service Users’ Behavioral Willingness from the Perspective of TPB and PMT. Master’s Thesis, Wuhan Textile University, Wuhan, China, 2016. [Google Scholar]
- Abbaspur-Behbahani, S.; Monaghesh, E.; Hajizadeh, A.; Fehresti, S. Application of mobile health to support the elderly during the COVID-19 outbreak: A systematic review. Health Policy Technol. 2022, 11, 100595. [Google Scholar] [CrossRef]
- Zhang, X.; Liu, S.; Wang, L.; Zhang, Y.; Wang, J. Mobile health service adoption in China: Integration of theory of planned behavior, protection motivation theory and personal health differences. Online Inf. Rev. 2019, 44, 1–23. [Google Scholar] [CrossRef]
- Guo, X.; Han, X.; Zhang, X.; Dang, Y.; Chen, C. Investigating m-health acceptance from a protection motivation theory perspective: Gender and age differences. Telemed. E-Health 2015, 21, 661–669. [Google Scholar] [CrossRef]
- Zhang, L.; McDowell, W.C. Am I really at risk? Determinants of online users’ intentions to use strong passwords. J. Internet Commer. 2009, 8, 180–197. [Google Scholar] [CrossRef]
- Lee, Y. Understanding anti-plagiarism software adoption: An extended protection motivation theory perspective. Decis. Support Syst. 2011, 50, 361–369. [Google Scholar] [CrossRef]
- Liu, Z. Research on User-Centered Network Interface Design. Master’s Thesis, Nanjing University of Aeronautics and Astronautics, Nanjing, China, 2007. [Google Scholar]
- Zhu, D.; Wang, D.; Huang, R.; Jing, Y.; Qiao, L.; Liu, W. User interface (UI) design and user experience questionnaire (UEQ) evaluation of a to-do list mobile application to support day-to-day life of older adults. Healthcare 2022, 10, 2068. [Google Scholar] [CrossRef]
- Norman, D.A. Emotional Design: Why We Love (or Hate) Everyday Things; Basic Books: New York, NY, USA, 2005. [Google Scholar]
- Dang, Y.Y. Research on User Participation Value and Incentive Mechanism of Mobile Medical APP for Chronic Diseases. Ph.D. Thesis, Harbin Institute of Technology, Harbin, China, 2020. [Google Scholar]
- Xu, H.; Sun, S.H.; Lin, W.S.; Yang, Y. Feasibility analysis of promoting mobile health based on smartphones to middle-aged and elderly people in cities. J. Prev. Med. Inf. 2018, 34, 745–749. [Google Scholar]
| Category | Research Variables | Definition of Operability | Code | Measurement Item | Sources |
|---|---|---|---|---|---|
| TAM | Perceived ease of use (PEOU) | The easier the aged find the use of mHealthcare apps, the more likely they are to have a positive attitude toward using them | PEOU1 | 1. MHealthcarecare Apps can upgrade our health quality | [17,56,57] |
| PEOU2 | 2. I think mHealthcare Apps have made my daily life safer | ||||
| PEOU3 | 3. MHealthcare services have enriched my access for disease prevention and treatment | ||||
| PEOU4 | 4. I think mHealthcare Apps are useful | ||||
| Perceived usefulness (PU) | When the aged feel helped during the use of mHealthcare apps, they will enhance their perceived usefulness toward the apps, thus forming a positive attitude toward using them | PU1 | 1. I think it’s easy to use mHealthcare Apps | [17,56,57] | |
| PU2 | 2. I thinks it’s easy to learn how to operate the mHealthcare Apps | ||||
| PU3 | 3. I think the mHealthcare Apps are simple and easy to use | ||||
| PU4 | 4. In general, mHealthcare Apps are easy to use | ||||
| Attitude toward using (AT) | The more active the aged are during the use of mHealthcare apps, the more likely they will be to access the platform | AT1 | 1. It’s a good idea to use mHealthcare service for health management | [17,56,57] | |
| AT2 | 2. I think my health status can be improved by using mHealthcare services | ||||
| AT3 | 3. I think mHealthcare services are very valuable | ||||
| Behavioral intention (BI) | The more positive the attitude of the aged toward using mHealthcare apps, the more positive the behavior trend will be, which will lead to the use of such apps | BI1 | 1. I’d love to use mHealthcare services for health management | [17,56,57] | |
| BI2 | 2. I’m planning to learn how to use mHealthcare services | ||||
| BI3 | 3. I prefer mHealthcare services to other forms of health management | ||||
| PMT | Perceived susceptibility (PSu) | Individual judgment of probability of occurrence of threat events from which they may suffer | PSu1 | 1. I think I’m more susceptible to illness than other people | [24,57] |
| PSu2 | 2. I feel that I am likely to have chronic diseases such as high blood pressure/heart disease/diabetes in the future | ||||
| PSu3 | 3. I find my physical condition is getting worse | ||||
| PSu4 | 4. I find myself in a state of sub-health | ||||
| Perceived severity (PSe) | Severity of threat events’ consequences or degree of harmfulness to them upon individual judgment | PSe1 | 1. I think the chronic diseases in elderly such as high blood pressure and heart disease may endanger my life | [24,57] | |
| PSe2 | 2. I think the deficient knowledge about the aged care may cause me to miss the optimal treatment | ||||
| PSe3 | 3. I think my life and work will be disturbed by any disease | ||||
| Perceived risk | Perceived risk (PR) | The aged perceive the use of mobile health apps as risky | PR1 | 1. I think the adoption of mHealthcare services may lead to privacy disclosure | [55,58,59] |
| PR2 | 2. I think the adoption of mHealthcare services may fail to meet my original expectation | ||||
| PR3 | 3. There may be security issues such as function disorders/system breakdown during the use of mHealthcare services | ||||
| PR4 | 4. Adoption of mHealthcare services may lead to financial losses, such as additional unknown paid services in the service system | ||||
| PR5 | 5. Adoption of mHealthcare services makes me nervous or anxious |
| Frequency Analysis Results | ||||
|---|---|---|---|---|
| Item | Option | Frequency | Percentage (%) | Cumulative Percentage (%) |
| Gender | Male | 160 | 43.84 | 43.84 |
| Female | 205 | 56.16 | 100.00 | |
| Age | 60–65 years old | 157 | 43.01 | 43.01 |
| 66–70 years old | 108 | 29.59 | 72.60 | |
| 71–75 years old | 65 | 17.81 | 90.41 | |
| Over 76 years old | 35 | 9.59 | 100.00 | |
| Educational background | Junior high school and under | 178 | 48.77 | 48.77 |
| Senior high school | 82 | 22.47 | 71.24 | |
| Junior college | 48 | 13.15 | 84.39 | |
| Undergraduate | 38 | 10.41 | 94.80 | |
| Master’s and above | 19 | 5.20 | 100.00 | |
| Occupation | Government departments and public institutions | 36 | 9.86 | 9.86 |
| Private business owners or managers | 25 | 6.85 | 16.71 | |
| Professionals and technical personnel | 23 | 6.30 | 23.01 | |
| Service personnel | 27 | 7.40 | 30.41 | |
| Industrial workers | 36 | 9.86 | 40.27 | |
| Agricultural laborers | 218 | 59.73 | 100.00 | |
| Monthly income | Below CNY 2000 | 58 | 15.89 | 15.89 |
| CNY 2001–3500 | 176 | 48.22 | 64.11 | |
| CNY 3501–5000 | 80 | 21.92 | 86.03 | |
| Over CNY 5000 | 51 | 13.97 | 100.00 | |
| Total | 365 | 100.00 | 100.00 | |
| Variables | Item | Corrected Item-Total Correlation (CITC) | Cronbach’s α if Item Deleted | Cronbach’s α | Total Cronbach α |
|---|---|---|---|---|---|
| PEOU | PEOU1 | 0.756 | 0.885 | 0.903 | 0.832 |
| PEOU2 | 0.750 | 0.887 | |||
| PEOU3 | 0.769 | 0.880 | |||
| PEOU4 | 0.860 | 0.847 | |||
| PU | PU1 | 0.821 | 0.916 | 0.931 | |
| PU2 | 0.858 | 0.903 | |||
| PU3 | 0.828 | 0.913 | |||
| PU4 | 0.845 | 0.907 | |||
| AT | AT1 | 0.778 | 0.861 | 0.894 | |
| AT2 | 0.827 | 0.818 | |||
| AT3 | 0.772 | 0.866 | |||
| BI | BI1 | 0.855 | 0.867 | 0.919 | |
| BI2 | 0.833 | 0.885 | |||
| BI3 | 0.818 | 0.897 | |||
| PSu | PSu1 | 0.819 | 0.901 | 0.923 | |
| PSu2 | 0.817 | 0.902 | |||
| PSu3 | 0.820 | 0.901 | |||
| PSu4 | 0.833 | 0.897 | |||
| PSe | PSe1 | 0.794 | 0.861 | 0.899 | |
| PSe2 | 0.831 | 0.829 | |||
| PSe3 | 0.776 | 0.876 | |||
| PR | PR1 | 0.884 | 0.952 | 0.961 | |
| PR2 | 0.892 | 0.951 | |||
| PR3 | 0.888 | 0.952 | |||
| PR4 | 0.884 | 0.952 | |||
| PR5 | 0.897 | 0.950 |
| KMO Value | 0.9 | |
| Bartlett’s Test of Sphericity | Chi-square Approximation | 4695.093 |
| df | 325 | |
| p value | 0 | |
| Name | Factor Loading | Commonality (Common Factor Variance) | ||||||
|---|---|---|---|---|---|---|---|---|
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 | Factor 6 | Factor 7 | ||
| PEOU1 | −0.115 | 0.239 | 0.019 | 0.800 | 0.138 | 0.202 | 0.099 | 0.780 |
| PEOU2 | −0.122 | 0.222 | 0.078 | 0.763 | 0.103 | 0.173 | 0.114 | 0.706 |
| PEOU3 | −0.110 | 0.208 | 0.026 | 0.776 | 0.128 | 0.075 | 0.268 | 0.752 |
| PEOU4 | −0.074 | 0.172 | 0.048 | 0.882 | 0.153 | 0.127 | 0.134 | 0.873 |
| PU1 | −0.096 | 0.855 | 0.010 | 0.146 | 0.174 | 0.173 | 0.157 | 0.847 |
| PU2 | −0.106 | 0.857 | −0.012 | 0.249 | 0.172 | 0.177 | 0.107 | 0.880 |
| PU3 | −0.145 | 0.848 | 0.073 | 0.220 | 0.095 | 0.147 | 0.189 | 0.860 |
| PU4 | −0.067 | 0.865 | 0.000 | 0.251 | 0.101 | 0.058 | 0.183 | 0.862 |
| AT1 | −0.233 | 0.253 | 0.047 | 0.207 | 0.245 | 0.204 | 0.742 | 0.816 |
| AT2 | −0.269 | 0.247 | 0.035 | 0.248 | 0.215 | 0.172 | 0.778 | 0.877 |
| AT3 | −0.150 | 0.243 | −0.031 | 0.254 | 0.209 | 0.206 | 0.785 | 0.850 |
| BI1 | −0.262 | 0.175 | −0.042 | 0.176 | 0.241 | 0.816 | 0.204 | 0.897 |
| BI2 | −0.240 | 0.150 | −0.040 | 0.218 | 0.170 | 0.824 | 0.172 | 0.866 |
| BI3 | −0.213 | 0.249 | −0.011 | 0.221 | 0.172 | 0.810 | 0.153 | 0.866 |
| PSU1 | 0.042 | 0.068 | 0.895 | 0.006 | 0.049 | −0.050 | −0.009 | 0.812 |
| PSU2 | −0.020 | 0.019 | 0.903 | 0.022 | 0.098 | −0.046 | −0.027 | 0.829 |
| PSU3 | 0.062 | −0.027 | 0.895 | 0.037 | 0.046 | 0.037 | 0.069 | 0.816 |
| PSU4 | 0.043 | −0.003 | 0.919 | 0.074 | 0.013 | −0.002 | 0.005 | 0.853 |
| PSE1 | −0.099 | 0.158 | 0.078 | 0.170 | 0.832 | 0.134 | 0.265 | 0.851 |
| PSE2 | −0.074 | 0.111 | 0.087 | 0.168 | 0.878 | 0.160 | 0.165 | 0.877 |
| PSE3 | −0.139 | 0.226 | 0.079 | 0.146 | 0.827 | 0.206 | 0.101 | 0.835 |
| PR1 | 0.899 | −0.095 | 0.038 | −0.068 | −0.068 | −0.175 | −0.072 | 0.863 |
| PR2 | 0.914 | −0.044 | 0.017 | −0.061 | −0.100 | −0.140 | −0.114 | 0.884 |
| PR3 | 0.915 | −0.082 | 0.046 | −0.112 | −0.058 | −0.080 | −0.104 | 0.880 |
| PR4 | 0.908 | −0.085 | 0.012 | −0.100 | −0.094 | −0.113 | −0.120 | 0.877 |
| PR5 | 0.899 | −0.116 | 0.039 | −0.098 | −0.035 | −0.147 | −0.136 | 0.875 |
| Cumulative percentage of variance explained % | 84.549 | |||||||
| Item | Estimate | S.E. | C.R. | p | Std | CR | AVE | ||
|---|---|---|---|---|---|---|---|---|---|
| PEOU1 | <--- | PEOU | 1 | 0.779 | 0.910 | 0.718 | |||
| PEOU2 | <--- | PEOU | 1.065 | 0.090 | 11.889 | *** | 0.839 | ||
| PEOU3 | <--- | PEOU | 1.116 | 0.089 | 12.489 | *** | 0.872 | ||
| PEOU4 | <--- | PEOU | 1.142 | 0.089 | 12.851 | *** | 0.894 | ||
| PU1 | <--- | PU | 1 | 0.829 | 0.915 | 0.728 | |||
| PU2 | <--- | PU | 1.032 | 0.074 | 13.898 | *** | 0.876 | ||
| PU3 | <--- | PU | 0.919 | 0.072 | 12.695 | *** | 0.824 | ||
| PU4 | <--- | PU | 1 | 0.071 | 14.078 | *** | 0.883 | ||
| AT1 | <--- | AT | 1 | 0.816 | 0.875 | 0.702 | |||
| AT2 | <--- | AT | 1.187 | 0.091 | 13.104 | *** | 0.906 | ||
| AT3 | <--- | AT | 0.964 | 0.085 | 11.312 | *** | 0.786 | ||
| BI1 | <--- | BI | 1 | 0.892 | 0.909 | 0.769 | |||
| BI2 | <--- | BI | 0.943 | 0.060 | 15.809 | *** | 0.886 | ||
| BI3 | <--- | BI | 0.980 | 0.066 | 14.812 | *** | 0.852 | ||
| PSu1 | <--- | PSu | 1 | 0.866 | 0.919 | 0.739 | |||
| PSu2 | <--- | PSu | 1.026 | 0.073 | 14.082 | *** | 0.846 | ||
| PSu3 | <--- | PSu | 1.009 | 0.068 | 14.894 | *** | 0.875 | ||
| PSu4 | <--- | PSu | 1.008 | 0.071 | 14.242 | *** | 0.852 | ||
| PSe1 | <--- | PSe | 1 | 0.831 | 0.887 | 0.724 | |||
| PSe2 | <--- | PSe | 1.029 | 0.075 | 13.654 | *** | 0.897 | ||
| PSe3 | <--- | PSe | 0.944 | 0.076 | 12.357 | *** | 0.822 | ||
| PR1 | <--- | PR | 1 | 0.906 | 0.958 | 0.819 | |||
| PR2 | <--- | PR | 0.987 | 0.052 | 19.051 | *** | 0.906 | ||
| PR3 | <--- | PR | 1.009 | 0.054 | 18.793 | *** | 0.902 | ||
| PR4 | <--- | PR | 0.951 | 0.052 | 18.168 | *** | 0.890 | ||
| PR5 | <--- | PR | 1.041 | 0.052 | 19.875 | *** | 0.921 | ||
| AVE | PEOU | PU | AT | BI | PSu | PSe | PR | |
|---|---|---|---|---|---|---|---|---|
| PEOU | 0.718 | 0.847 | ||||||
| PU | 0.728 | 0.636 *** | 0.853 | |||||
| AT | 0.702 | 0.546 *** | 0.504 *** | 0.838 | ||||
| BI | 0.769 | 0.539 *** | 0.555 *** | 0.596 *** | 0.877 | |||
| PSu | 0.739 | 0.203 * | 0.037 | 0.037 | 0.053 | 0.860 | ||
| PSe | 0.724 | 0.592 *** | 0.520 *** | 0.616 *** | 0.596 *** | 0.197* | 0.851 | |
| PR | 0.819 | −0.333 *** | −0.260 ** | −0.428 *** | −0.431 *** | −0.079 | −0.333 *** | 0.905 |
| Model Fit | Criteria | Model Fit of Research Model | Judgment |
|---|---|---|---|
| ML chi-square (MLχ2) | The smaller, the better | 345.801 | |
| Degrees of freedom (DF) | The larger, the better | 278 | |
| Normed chi-square χ2/df | <3 | 1.244 | Yes |
| Root mean square error of approximation (RMSEA) | <0.08 | 0.038 | Yes |
| Standardized root mean square residual (SRMR) | <0.08 | 0.0434 | Yes |
| Tucker–Lewis index (TLI) | >0.9 | 0.978 | Yes |
| Comparative fit index (CFI) | >0.9 | 0.981 | Yes |
| Normative fit index (NFI) | >0.9 | 0.912 | Yes |
| Parsimony goodness-of-fit index (PGFI) | >0.5 | 0.690 | Yes |
| Parsimony normed fit index (PNFI) | >0.5 | 0.780 | Yes |
| Incremental fit index (IFI) | >0.9 | 0.981 | Yes |
| Hypothesis | Route | Estimate | S.E. | C.R. | p | STD | Results | ||
|---|---|---|---|---|---|---|---|---|---|
| H1 | AT | <--- | PU | 0.184 | 0.047 | 3.882 | *** | 0.217 | Support |
| H2 | BI | <--- | PU | 0.245 | 0.052 | 4.703 | *** | 0.249 | Support |
| H3 | AT | <--- | PEOU | 0.203 | 0.061 | 3.315 | *** | 0.217 | Support |
| H4 | PU | <--- | PEOU | 0.664 | 0.06 | 10.984 | *** | 0.603 | Support |
| H5 | BI | <--- | AT | 0.443 | 0.07 | 6.34 | *** | 0.383 | Support |
| H6 | AT | <--- | PSu | −0.049 | 0.037 | −1.311 | 0.19 | −0.057 | Nonsupport |
| H7 | AT | <--- | PSe | 0.308 | 0.049 | 6.239 | *** | 0.346 | Support |
| H8 | AT | <--- | PR | −0.157 | 0.032 | −4.89 | *** | −0.223 | Support |
| H9 | BI | <--- | PR | −0.184 | 0.041 | −4.551 | *** | −0.225 | Support |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, X.; Lee, C.-F.; Jiang, J.; Zhu, X. Factors Influencing the Aged in the Use of Mobile Healthcare Applications: An Empirical Study in China. Healthcare 2023, 11, 396. https://doi.org/10.3390/healthcare11030396
Wang X, Lee C-F, Jiang J, Zhu X. Factors Influencing the Aged in the Use of Mobile Healthcare Applications: An Empirical Study in China. Healthcare. 2023; 11(3):396. https://doi.org/10.3390/healthcare11030396
Chicago/Turabian StyleWang, Xiang, Chang-Franw Lee, Jiabei Jiang, and Xiaoyang Zhu. 2023. "Factors Influencing the Aged in the Use of Mobile Healthcare Applications: An Empirical Study in China" Healthcare 11, no. 3: 396. https://doi.org/10.3390/healthcare11030396
APA StyleWang, X., Lee, C.-F., Jiang, J., & Zhu, X. (2023). Factors Influencing the Aged in the Use of Mobile Healthcare Applications: An Empirical Study in China. Healthcare, 11(3), 396. https://doi.org/10.3390/healthcare11030396






