Preferred Place of End-of-Life Care Based on Clinical Scenario: A Cross-Sectional Study of a General Japanese Population
Abstract
1. Introduction
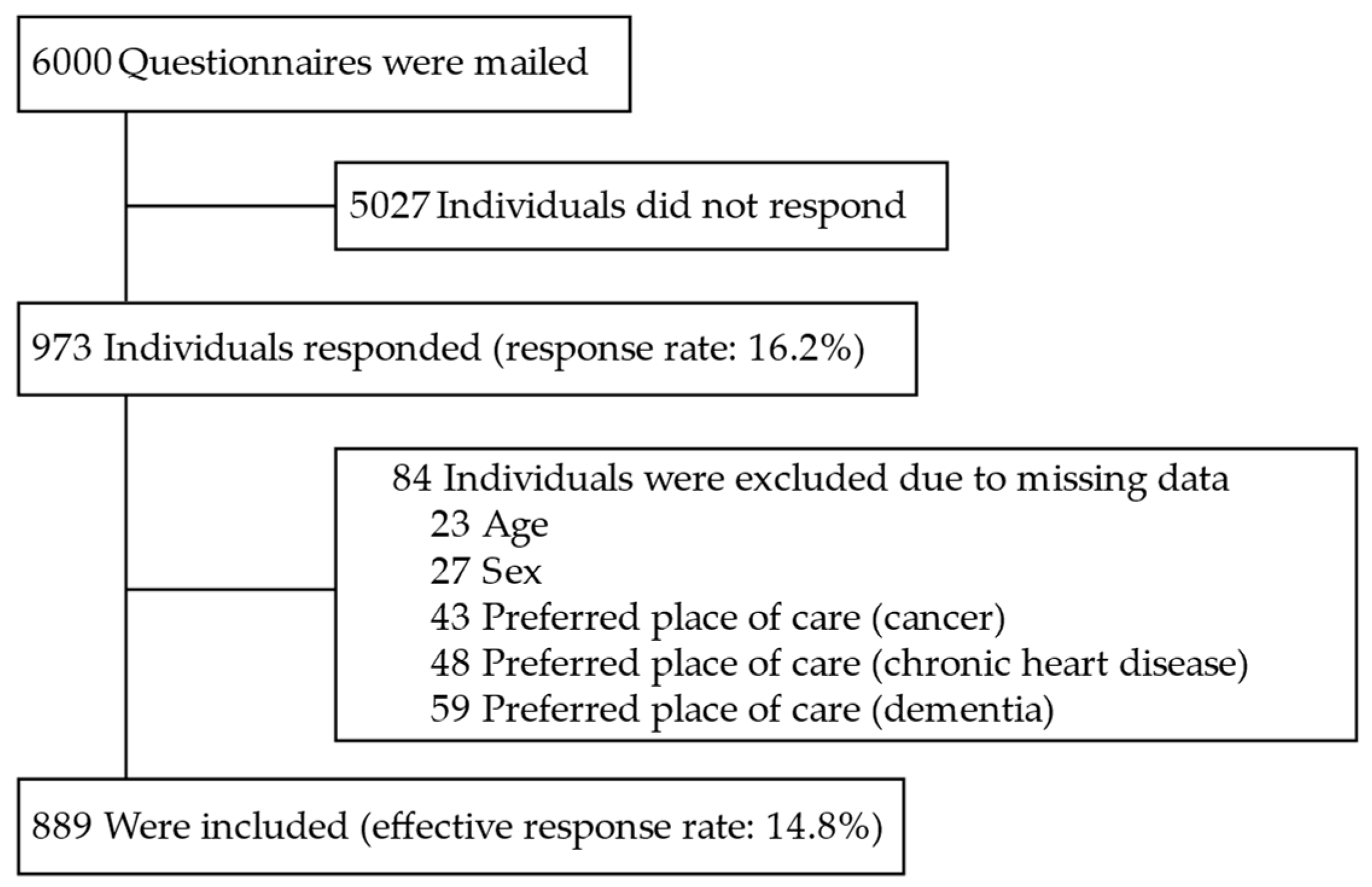
2. Materials and Methods
2.1. Study Design and Participants
2.2. Measures
2.2.1. Dependent Variable
2.2.2. Main Predictors
2.2.3. Potential Associated Variables
2.3. Statistical Analysis
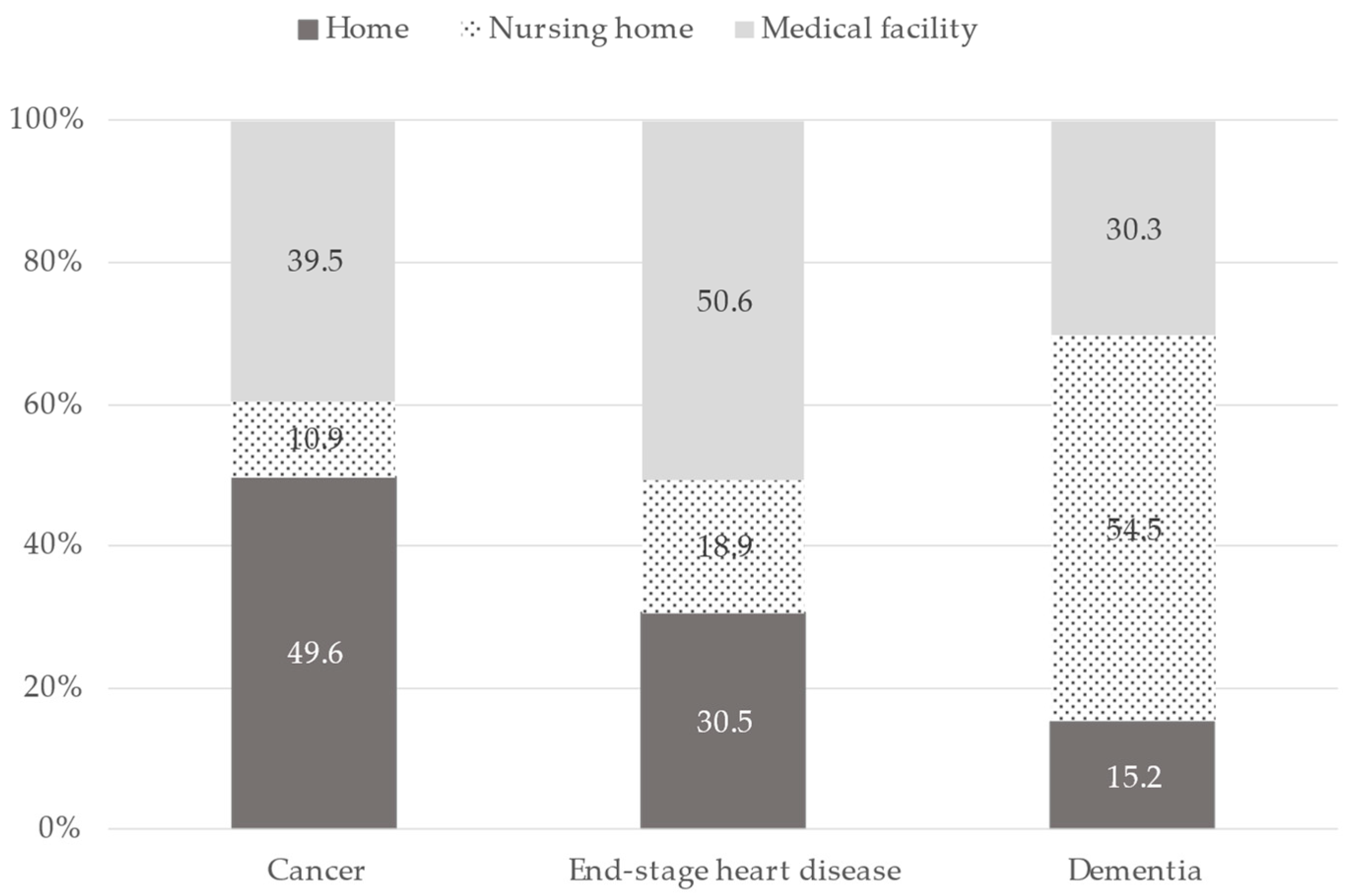
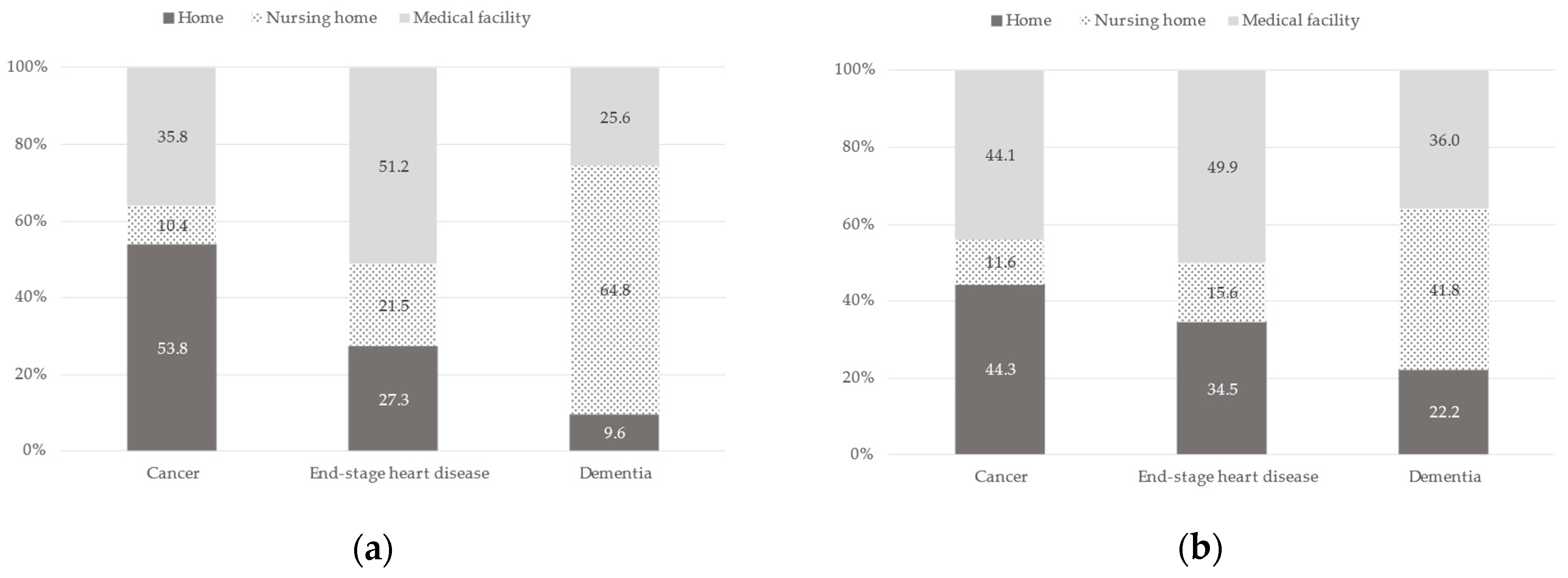
3. Results
4. Discussion
Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Annual Health, Labour and Welfare Report 2021. Available online: https://www.mhlw.go.jp/english/wp/wp-hw14/index.html (accessed on 15 January 2023).
- Iwagami, M.; Tamiya, N. The long-term care insurance system in Japan: Past, present, and future. JMA J. 2019, 2, 67–69. [Google Scholar] [CrossRef] [PubMed]
- Lepping, P.; Stanly, T.; Turner, J. Systematic review on the prevalence of lack of capacity in medical and psychiatric settings. Clin. Med. 2015, 15, 337–343. [Google Scholar] [CrossRef]
- Miyashita, J.; Shimizu, S.; Shiraishi, R.; Mori, M.; Okawa, K.; Aita, K.; Mitsuoka, S.; Nishikawa, M.; Kizawa, Y.; Morita, T.; et al. Culturally adapted consensus definition and action guideline: Japan’s advance care planning. J. Pain Symptom Manag. 2022, 64, 602–613. [Google Scholar] [CrossRef] [PubMed]
- Sudore, R.L.; Lum, H.D.; You, J.J.; Hanson, L.C.; Meier, D.E.; Pantilat, S.Z.; Matlock, D.D.; Rietjens, J.A.C.; Korfage, I.J.; Ritchie, C.S.; et al. Defining advance care planning for adults: A consensus definition from a multidisciplinary Delphi panel. J. Pain Symptom Manag. 2017, 53, 821–832.e1. [Google Scholar] [CrossRef] [PubMed]
- Jimenez, G.; Tan, W.S.; Virk, A.K.; Low, C.K.; Car, J.; Ho, A.H.Y. Overview of systematic reviews of advance care planning: Summary of evidence and global lessons. J. Pain Symptom Manag. 2018, 56, 436–459.e25. [Google Scholar] [CrossRef] [PubMed]
- Ikari, T.; Hiratsuka, Y.; Cheng, S.Y.; Miyashita, M.; Morita, T.; Mori, M.; Uneno, Y.; Amano, K.; Uehara, Y.; Yamaguchi, T.; et al. Factors associated with good death of patients with advanced cancer: A prospective study in Japan. Support. Care Cancer 2022, 30, 9577–9586. [Google Scholar] [CrossRef]
- Peck, V.; Valiani, S.; Tanuseputro, P.; Mulpuru, S.; Kyeremanteng, K.; Fitzgibbon, E.; Forster, A.; Kobewka, D. Advance care planning after hospital discharge: Qualitative analysis of facilitators and barriers from patient interviews. BMC Palliat. Care 2018, 17, 127. [Google Scholar] [CrossRef]
- Piers, R.D.; van Eechoud, I.J.; Van Camp, S.; Grypdonck, M.; Deveugele, M.; Verbeke, N.C.; Van Den Noortgate, N.J. Advance Care Planning in terminally ill and frail older persons. Patient Educ. Couns. 2013, 90, 323–329. [Google Scholar] [CrossRef]
- Rosa, W.E.; Izumi, S.; Sullivan, D.R.; Lakin, J.; Rosenberg, A.R.; Creutzfeldt, C.J.; Lafond, D.; Tjia, J.; Cotter, V.; Wallace, C.; et al. Advance care planning in serious illness: A narrative review. J. Pain Symptom Manag. 2023, 65, e63–e78. [Google Scholar] [CrossRef]
- Fukui, S.; Yoshiuchi, K.; Fujita, J.; Sawai, M.; Watanabe, M. Japanese people’s preference for place of end-of-life care and death: A population-based nationwide survey. J. Pain Symptom Manag. 2011, 42, 882–892. [Google Scholar] [CrossRef]
- Nishie, H.; Mizobuchi, S.; Suzuki, E.; Sato, K.; Toda, Y.; Matsuoka, J.; Morimatsu, H. Living will interest and preferred end-of-life care and death locations among Japanese adults 50 and over: A population-based survey. Acta Med. Okayama 2014, 68, 339–348. [Google Scholar] [CrossRef] [PubMed]
- Wilson, D.M.; Cohen, J.; Deliens, L.; Hewitt, J.A.; Houttekier, D. The preferred place of last days: Results of a representative population-based public survey. J. Palliat. Med. 2013, 16, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Gomes, B.; Calanzani, N.; Gysels, M.; Hall, S.; Higginson, I.J. Heterogeneity and changes in preferences for dying at home: A systematic review. BMC Palliat. Care 2013, 12, 7. [Google Scholar] [CrossRef] [PubMed]
- Chung, R.Y.; Wong, E.L.; Kiang, N.; Chau, P.Y.; Lau, J.Y.C.; Wong, S.Y.; Yeoh, E.K.; Woo, J.W. Knowledge, attitudes, and preferences of advance decisions, end-of-life care, and place of care and death in Hong Kong. A population-based telephone survey of 1067 adults. J. Am. Med. Dir. Assoc. 2017, 18, 367.e19–367.e27. [Google Scholar] [CrossRef]
- Jiraphan, A.; Pitanupong, J. General population-based study on preferences towards end-of-life care in Southern Thailand: A cross-sectional survey. BMC Palliat. Care 2022, 21, 36. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare Number of Deaths, the Proportion of Place of Death. Available online: https://view.officeapps.live.com/op/view.aspx?src=https%3A%2F%2Fwww.mhlw.go.jp%2Ftoukei%2Fyouran%2Fdatar03k%2F1-25.xlsx&wdOrigin=BROWSELINK (accessed on 15 January 2023).
- Yamagishi, A.; Morita, T.; Miyashita, M.; Yoshida, S.; Akizuki, N.; Shirahige, Y.; Akiyama, M.; Eguchi, K. Preferred place of care and place of death of the general public and cancer patients in Japan. Support. Care Cancer 2012, 20, 2575–2582. [Google Scholar] [CrossRef]
- Sanford, A.M.; Orrell, M.; Tolson, D.; Abbatecola, A.M.; Arai, H.; Bauer, J.M.; Cruz-Jentoft, A.J.; Dong, B.; Ga, H.; Goel, A.; et al. An international definition for “nursing home”. J. Am. Med. Dir. Assoc. 2015, 16, 181–184. [Google Scholar] [CrossRef]
- Miyashita, M.; Sanjo, M.; Morita, T.; Hirai, K.; Uchitomi, Y. Good death in cancer care: A nationwide quantitative study. Ann. Oncol. 2007, 18, 1090–1097. [Google Scholar] [CrossRef]
- Martin, R.S.; Hayes, B.; Gregorevic, K.; Lim, W.K. The effects of advance care planning interventions on nursing home residents: A systematic review. J. Am. Med. Dir. Assoc. 2016, 17, 284–293. [Google Scholar] [CrossRef]
- Ouchi, Y.; Rakugi, H.; Arai, H.; Akishita, M.; Ito, H.; Toba, K.; Kai, I. Joint Committee of Japan Gerontological Society (JGLS) and Japan Geriatrics Society (JGS) on the definition and classification of the elderly Redefining the elderly as aged 75 years and older: Proposal from the Joint Committee of Japan Gerontological Society and the Japan Geriatrics Society. Geriatr. Gerontol. Int. 2017, 17, 1045–1047. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare Health Care Insurance System. Available online: https://www.mhlw.go.jp/english/wp/wp-hw5/dl/23010201e.pdf (accessed on 10 December 2022).
- Sanjo, M.; Miyashita, M.; Morita, T.; Hirai, K.; Kawa, M.; Akechi, T.; Uchitomi, Y. Preferences regarding end-of-life cancer care and associations with good-death concepts: A population-based survey in Japan. Ann. Oncol. 2007, 18, 1539–1547. [Google Scholar] [CrossRef] [PubMed]
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; Butler, J.; Casey, D.E., Jr.; Colvin, M.M.; Drazner, M.H.; Filippatos, G.S.; Fonarow, G.C.; Givertz, M.M.; et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines and the Heart Failure Society of America. Circulation 2017, 136, e137–e161. [Google Scholar] [CrossRef] [PubMed]
- Okumura, T.; Sawamura, A.; Murohara, T. Palliative and end-of-life care for heart failure patients in an aging society. Korean J. Intern. Med. 2018, 33, 1039–1049. [Google Scholar] [CrossRef] [PubMed]
- McIlvennan, C.K.; Allen, L.A. Palliative care in patients with heart failure. BMJ 2016, 353, i1010. [Google Scholar] [CrossRef] [PubMed]
- Sachs, G.A.; Shega, J.W.; Cox-Hayley, D. Barriers to excellent end-of-life care for patients with dementia. J. Gen. Intern. Med. 2004, 19, 1057–1063. [Google Scholar] [CrossRef]
- Regier, N.G.; Hodgson, N.A.; Gitlin, L.N. Characteristics of activities for persons with dementia at the mild, moderate, and severe stages. Gerontologist 2017, 57, 987–997. [Google Scholar] [CrossRef]
- Arai, Y.; Arai, A.; Zarit, S.H. What do we know about dementia?: A survey on knowledge about dementia in the general public of Japan. Int. J. Geriatr. Psychiatry 2008, 23, 433–438. [Google Scholar] [CrossRef]
- Natsume, M.; Watanabe, K.; Matsumoto, S.; Naruge, D.; Hayashi, K.; Furuse, J.; Kawamura, M.; Jinno, H.; Sano, K.; Fukushima, R.; et al. Factors influencing cancer patients’ choice of end-of-life care place. J. Palliat. Med. 2018, 21, 751–765. [Google Scholar] [CrossRef]
- Wiggins, N.; Droney, J.; Mohammed, K.; Riley, J.; Sleeman, K.E. Understanding the factors associated with patients with dementia achieving their preferred place of death: A retrospective cohort study. Age Ageing 2019, 48, 433–439. [Google Scholar] [CrossRef]
- Skorstengaard, M.H.; Neergaard, M.A.; Andreassen, P.; Brogaard, T.; Bendstrup, E.; Løkke, A.; Aagaard, S.; Wiggers, H.; Bech, P.; Jensen, A.B. Preferred place of care and death in terminally ill patients with lung and heart disease compared to cancer patients. J. Palliat. Med. 2017, 20, 1217–1224. [Google Scholar] [CrossRef]
- Hoare, S.; Morris, Z.S.; Kelly, M.P.; Kuhn, I.; Barclay, S. Do patients want to die at home? A systematic review of the UK literature, focused on missing preferences for place of death. PLoS ONE 2015, 10, e0142723. [Google Scholar] [CrossRef] [PubMed]
- Neergaard, M.A.; Brogaard, T.; Vedsted, P.; Jensen, A.B. Asking terminally ill patients about their preferences concerning place of care and death. Int. J. Palliat. Nurs. 2018, 24, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Evans, R.; Finucane, A.; Vanhegan, L.; Arnold, E.; Oxenham, D. Do place-of-death preferences for patients receiving specialist palliative care change over time? Int. J. Palliat. Nurs. 2014, 20, 579–583. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | N (%) |
|---|---|
| Age, years | |
| <65 | 492 (55.3) |
| ≥65 | 397 (44.7) |
| By decade | |
| 20–29 | 39 (4.4) |
| 30–39 | 107 (12.1) |
| 40–49 | 137 (15.4) |
| 50–59 | 133 (15.0) |
| 60–69 | 188 (21.1) |
| 70–79 | 188 (21.1) |
| ≥80 | 97 (10.9) |
| Sex | |
| Men | 498 (56.0) |
| Women | 391 (44.0) |
| Education | |
| Elementary school | 92 (10.4) |
| High school | 306 (34.4) |
| Junior college | 171 (19.2) |
| Bachelor’s degree or graduate school | 317 (35.7) |
| No answer | 3 (0.3) |
| Living arrangements | |
| Alone | 142 (16.0) |
| With ≥1 family member | 727 (81.8) |
| No answer | 20 (2.2) |
| Has a family doctor | |
| Yes | 364 (40.9) |
| No | 518 (58.3) |
| No answer | 7 (0.8) |
| Experience caring for a loved one | |
| Yes | 332 (37.4) |
| No | 549 (61.7) |
| No answer | 8 (0.9) |
| Experienced death of a loved one | |
| Yes | 371 (41.7) |
| No | 484 (54.4) |
| No answer | 34 (3.8) |
| Discussed future treatment | |
| Yes | 351 (39.5) |
| No | 505 (56.8) |
| No answer | 33 (3.7) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hanari, K.; Moody, S.Y.; Sugiyama, T.; Tamiya, N. Preferred Place of End-of-Life Care Based on Clinical Scenario: A Cross-Sectional Study of a General Japanese Population. Healthcare 2023, 11, 406. https://doi.org/10.3390/healthcare11030406
Hanari K, Moody SY, Sugiyama T, Tamiya N. Preferred Place of End-of-Life Care Based on Clinical Scenario: A Cross-Sectional Study of a General Japanese Population. Healthcare. 2023; 11(3):406. https://doi.org/10.3390/healthcare11030406
Chicago/Turabian StyleHanari, Kyoko, Sandra Y. Moody, Takehiro Sugiyama, and Nanako Tamiya. 2023. "Preferred Place of End-of-Life Care Based on Clinical Scenario: A Cross-Sectional Study of a General Japanese Population" Healthcare 11, no. 3: 406. https://doi.org/10.3390/healthcare11030406
APA StyleHanari, K., Moody, S. Y., Sugiyama, T., & Tamiya, N. (2023). Preferred Place of End-of-Life Care Based on Clinical Scenario: A Cross-Sectional Study of a General Japanese Population. Healthcare, 11(3), 406. https://doi.org/10.3390/healthcare11030406





