The Association of Smoking with Contact Dermatitis: A Cross-Sectional Study
Abstract
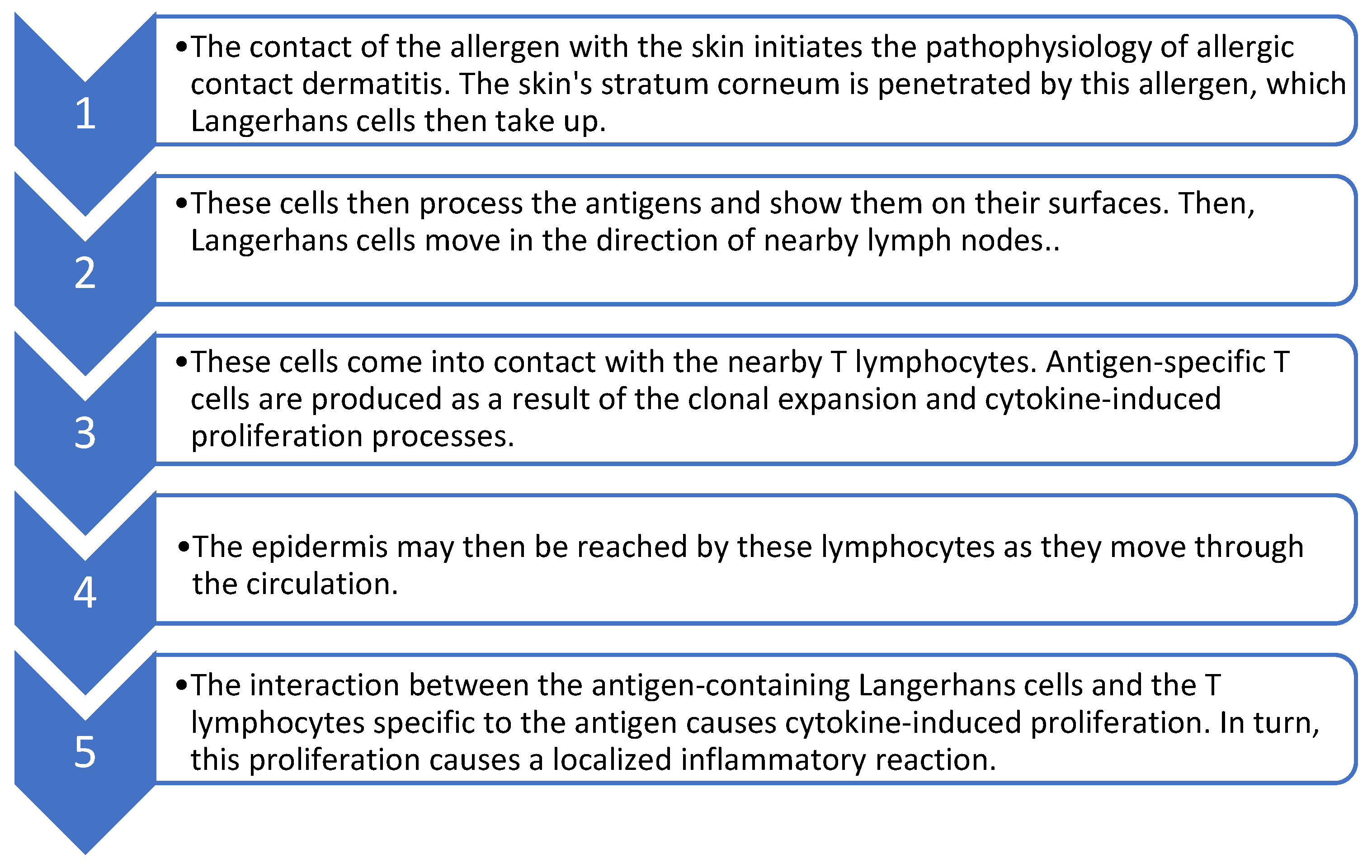
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dastagiri, P.; Shaji, N.M. Irritant Contact Dermatitis with Secondary Infection Treated with Individualised Homoeopathic Medicine-A Case Report. Int. J. Ayush. Care 2021, 5, 187–196. [Google Scholar]
- Ribeiro, W.R.; Queiroz, A.G.; Mendes, E.; Casaro, M.B.; Nascimento, C.M.; Coelho, L.S.S.F.; Martins, F.S.; Leite-Silva, V.R.; Ferreira, C.M. Preventive oral supplementation with Bifidobacterium longum 51A alleviates oxazolone-induced allergic contact dermatitis-like skin inflammation in mice. Benef. Microbes 2021, 12, 199–209. [Google Scholar] [CrossRef]
- Allergic Contact Dermatitis. Available online: https://www.ncbi.nlm.nih.gov/books/NBK568684 (accessed on 3 December 2022).
- Bolognia, J.; Jorizzo, J.; Schaffer, J. Dermatology, Pekín; Elsevier: Amesterdam, The Netherlands, 2018. [Google Scholar]
- Carol, L.; Taylor, J.S. Contact dermatitis and related disorders. In ACP Medicine Hamilton (CA); BC Decker Inc.: Hamilton, ON, Canada, 2008. [Google Scholar]
- Bordel-Gómez, M.T.; Miranda-Romero, A.; Castrodeza-Sanz, J. Epidemiology of contact dermatitis: Prevalence of sensitization to different allergens and associated factors. Actas Dermosifiliogr. 2010, 101, 59–75. [Google Scholar] [CrossRef]
- Shakoor, Z.; Al-Mutairi, A.S.; Al-Shenaifi, A.M.; Al-Abdulsalam, A.M.; Al-Shirah, B.Z.; Al-Harbi, S.A. Screening for skin-sensitizing allergens among patients with clinically suspected allergic contact dermatitis. Saudi Med. J. 2017, 38, 922–927. [Google Scholar] [CrossRef]
- Li, Y.; Li, L. Contact dermatitis: Classifications and management. Clin. Rev. Allergy Immunol. 2021, 61, 245–281. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, G.; Rasmussen, K.; Bregnhøj, A.; Isaksson, M.; Diepgen, T.L.; Carstensen, O. Causes of irritant contact dermatitis after occupational skin exposure: A systematic review. Int. Arch. Occup. Environ. Health 2021, 95, 35–65. [Google Scholar] [CrossRef] [PubMed]
- Moradi-Lakeh, M.; El Bcheraoui, C.; Tuffaha, M.; Daoud, F.; Al Saeedi, M.; Basulaiman, M.; Memish, Z.A.; AlMazroa, M.A.; Al Rabeeah, A.A.; Mokdad, A.H. Tobacco consumption in the Kingdom of Saudi Arabia, 2013: Findings from a national survey. BMC Public Health 2015, 15, 611. [Google Scholar] [CrossRef] [PubMed]
- Bonamonte, D.; Vestita, M.; Filoni, A.; Mastrolonardo, M.; Angelini, G.; Foti, C. Tobacco-induced contact dermatitis. Eur. J. Dermatol. 2016, 26, 223–231. [Google Scholar] [CrossRef]
- Armstrong, A.; Armstrong, E.; Fuller, E.; Sockolov, M.; Voyles, S. Smoking and pathogenesis of psoriasis: A review of oxidative, inflammatory and genetic mechanisms. Br. J. Dermatol. 2011, 165, 1162–1168. [Google Scholar] [CrossRef] [PubMed]
- Arnson, Y.; Shoenfeld, Y.; Amital, H. Effects of tobacco smoke on immunity, inflammation and autoimmunity. J. Autoimmun. 2010, 34, J258–J265. [Google Scholar] [CrossRef]
- Ertle, C.M.; Rommel, F.R.; Tumala, S.; Moriwaki, Y.; Klein, J.; Kruse, J.; Gieler, U.; Peters, E.M.J. New Pathways for the Skin’s Stress Response: The Cholinergic Neuropeptide SLURP-1 Can Activate Mast Cells and Alter Cytokine Production in Mice. Front. Immunol. 2021, 12, 631881. [Google Scholar] [CrossRef]
- Strzelak, A.; Ratajczak, A.; Adamiec, A.; Feleszko, W. Tobacco smoke induces and alters immune responses in the lung triggering inflammation, allergy, asthma and other lung diseases: A mechanistic review. Int. J. Environ. Res. Public Health 2018, 15, 1033. [Google Scholar] [CrossRef] [PubMed]
- Linneberg, A.; Nielsen, N.H.; Menné, T.; Madsen, F.; Jørgensen, T. Smoking might be a risk factor for contact allergy. J. Allergy Clin. Immunol. 2003, 111, 980–984. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, K.A.; Armbrecht, E.S.; Burkemper, N.M. The association of smoking with contact dermatitis and hand eczema—A review. Int. J. Dermatol. 2018, 57, 375–387. [Google Scholar] [CrossRef]
- Thyssen, J.P.; Johansen, J.D.; Menné, T.; Nielsen, N.H.; Linneberg, A. Effect of tobacco smoking and alcohol consumption on the prevalence of nickel sensitization and contact sensitization. Acta Derm. Venereol. 2010, 90, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Karrow, N.A. Activation of the hypothalamic—Pituitary—Adrenal axis and autonomic nervous system during inflammation and altered programming of the neuroendocrine—immune axis during fetal and neonatal development: Lessons learned from the model inflammagen, lipopolysaccharide. Brain Behav. Immun. 2006, 20, 144–158. [Google Scholar]
- Le Coz, C.J.; Foti, C.; Bonamonte, D.; Angelini, G.; Romita, P. Cigarette and cigar makers and tobacco workers. Kanerva’s Occup. Dermatol. 2020, 2020, 1855–1860. [Google Scholar]
- Tobacco Questions for Surveys: A Subset of Key Questions from the Global Adult Tobacco Survey (GATS). Available online: https://apps.who.int/iris/handle/10665/87331 (accessed on 3 December 2022).
- Murphy, P.B.; Atwater, A.R.; Mueller, M. Available online: https://www.ncbi.nlm.nih.gov/books/NBK532866 (accessed on 3 December 2022).
- Lukács, J.; Schliemann, S.; Elsner, P. Association between smoking and hand dermatitis—a systematic review and meta-analysis. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 1280–1284. [Google Scholar] [CrossRef]
- Saulyte, J.; Regueira, C.; Montes-Martínez, A.; Khudyakov, P.; Takkouche, B. Active or passive exposure to tobacco smoking and allergic rhinitis, allergic dermatitis, and food allergy in adults and children: A systematic review and meta-analysis. PLoS Med. 2014, 11, e1001611. [Google Scholar] [CrossRef]
- Sawada, Y.; Saito-Sasaki, N.; Mashima, E.; Nakamura, M. Daily Lifestyle and Inflammatory Skin Diseases. Int. J. Mol. Sci. 2021, 22, 5204. [Google Scholar] [CrossRef]
- Molin, S.; Ruzicka, T.; Herzinger, T. Smoking is associated with combined allergic and irritant hand eczema, contact allergies and hyperhidrosis. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 2483–2486. [Google Scholar] [CrossRef]
- Kantor, R.; Kim, A.; Thyssen, J.P.; Silverberg, J.I. Association of atopic dermatitis with smoking: A systematic review and meta-analysis. J. Am. Acad. Dermatol. 2016, 75, 1119–1125.e1. [Google Scholar] [CrossRef] [PubMed]
- Jing, D.; Li, J.; Tao, J.; Wang, X.; Shan, S.; Kang, X.; Wu, B.; Zhang, Y.; Xiao, Y.; Chen, X.; et al. Associations of second-hand smoke exposure with hand eczema and atopic dermatitis among college students in China. Sci. Rep. 2020, 10, 17400. [Google Scholar] [CrossRef] [PubMed]
- Wollenberg, A.; Barbarot, S.; Bieber, T.; Christen-Zaech, S.; Deleuran, M.; Fink-Wagner, A.; Gieler, U.; Girolomoni, G.; Lau, S.; Muraro, A.; et al. Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: Part I. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 657–682. [Google Scholar] [CrossRef] [PubMed]
- Torkashvand, J.; Farzadkia, M.; Sobhi, H.R.; Esrafili, A. Littered cigarette butt as a well-known hazardous waste: A comprehensive systematic review. J. Hazard. Mater. 2020, 383, 121242. [Google Scholar] [CrossRef] [PubMed]
| Smoker N (%) | Non-Smoker N (%) | p-Value | |
|---|---|---|---|
| Male | 26 (83.9) | 65 (23.5) | <0.001 |
| Female | 5 (16.1) | 212 (76.5) | |
| Age (Mean ± SD) | 38 ± 5.6 | 40 ± 6.7 | >0.05 |
| Educational Level | 19 (61.3) | 159 (57.4) | >0.05 |
| Dry Skin | 20 (64.5) | 221 (79.8) | >0.05 |
| Allergic Rhinitis | 11(35.5) | 137(49) | >0.05 |
| Asthma | 9 (29) | 129 (46) | >0.05 |
| Smokers N (%) | Non-Smokers N (%) | Relative Risk | p-Value | |
|---|---|---|---|---|
| ACD | 8 (25.8) | 142 (51.3) | 0.5 | 0.007 |
| ICD | 23 (74.2) | 135 (48.7) | 1.5 |
| Prevalence of ACD (%) | Odds Ratio * (95% CI) | p-Value | |
|---|---|---|---|
| Smoking Status: | |||
| Never | 51.3% | 1.00 | |
| Daily | 30.0% | 1.39 (0.44–4.46) | 0.577 |
| Less than daily | 18.2% | 0.60 (0.11–3.33) | 0.563 |
| Previously | 20.6% | 1.01 (0.35–2.98) | 0.973 |
| ACD | ICD | Total | p-Value | |||
|---|---|---|---|---|---|---|
| N | % | N | % | N | ||
| Cigarettes | 4 | 33.33 | 8 | 66.67 | 12 | 0.077 |
| Cigars | 0 | 0.00 | 7 | 100.00 | 7 | 0.003 |
| Shisha | 3 | 33.33 | 6 | 66.67 | 9 | 0.127 |
| ACD | ICD | p-Value | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Duration of Smoking | 12.83 | 9.55 | 20.25 | 16.92 | 11.26 | 6.99 | 0.369 |
| Smokers N (%) | Non-Smokers N (%) | p-Value | |
|---|---|---|---|
| Hand | 9 (29) | 54 (19.5) | >0.05 |
| Face | 1 (3.2) | 17 (6.1) | >0.05 |
| Foot | 0 | 15 (5.4) | >0.05 |
| Trunk or Other | 6 (19.4) | 35 (16.2) | >0.05 |
| More Than One of the Above | 15 (48.4) | 132 (47.7) | >0.05 |
| Smokers N (%) | Non-Smokers N (%) | p-Value | |
|---|---|---|---|
| Right hand | 3 (18.7) | 14 (17.3) | >0.05 |
| Left hand | 3 (18.7) | 4 (4.9) | 0.03 |
| Both | 10 (62.5) | 63 (77) | >0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alotaibi, G.F.; Alsalman, H.H.; Alhallaf, R.A.; Ahmad, R.A.; Alshareef, H.A.; Muammar, J.M.; Alsaif, F.M.; Alotaibi, F.F.; Balaha, M.F.; Ahmed, N.J.; et al. The Association of Smoking with Contact Dermatitis: A Cross-Sectional Study. Healthcare 2023, 11, 427. https://doi.org/10.3390/healthcare11030427
Alotaibi GF, Alsalman HH, Alhallaf RA, Ahmad RA, Alshareef HA, Muammar JM, Alsaif FM, Alotaibi FF, Balaha MF, Ahmed NJ, et al. The Association of Smoking with Contact Dermatitis: A Cross-Sectional Study. Healthcare. 2023; 11(3):427. https://doi.org/10.3390/healthcare11030427
Chicago/Turabian StyleAlotaibi, Ghadah F., Hanan H. Alsalman, Rama A. Alhallaf, Rayan A. Ahmad, Hashem A. Alshareef, Jumanah Meshari Muammar, Fahad M. Alsaif, Felwah F. Alotaibi, Mohamed F. Balaha, Nehad J. Ahmed, and et al. 2023. "The Association of Smoking with Contact Dermatitis: A Cross-Sectional Study" Healthcare 11, no. 3: 427. https://doi.org/10.3390/healthcare11030427
APA StyleAlotaibi, G. F., Alsalman, H. H., Alhallaf, R. A., Ahmad, R. A., Alshareef, H. A., Muammar, J. M., Alsaif, F. M., Alotaibi, F. F., Balaha, M. F., Ahmed, N. J., Khafagy, E.-S., Alotaibi, H. F., Alshammari, R., & Fatani, S. (2023). The Association of Smoking with Contact Dermatitis: A Cross-Sectional Study. Healthcare, 11(3), 427. https://doi.org/10.3390/healthcare11030427







