Development and Validation of a Risk Scoring Tool for Bronchopulmonary Dysplasia in Preterm Infants Based on a Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Research Design and Methods
2.1. Meta-Analysis
2.1.1. Design
2.1.2. Literature Search Strategy
2.1.3. Inclusion and Exclusion Criteria
2.1.4. Data Extraction and Quality Assessment
2.1.5. Statistical Analysis
2.2. Development of the Risk Scoring Tool
2.3. Validation of the Risk Scoring Tool
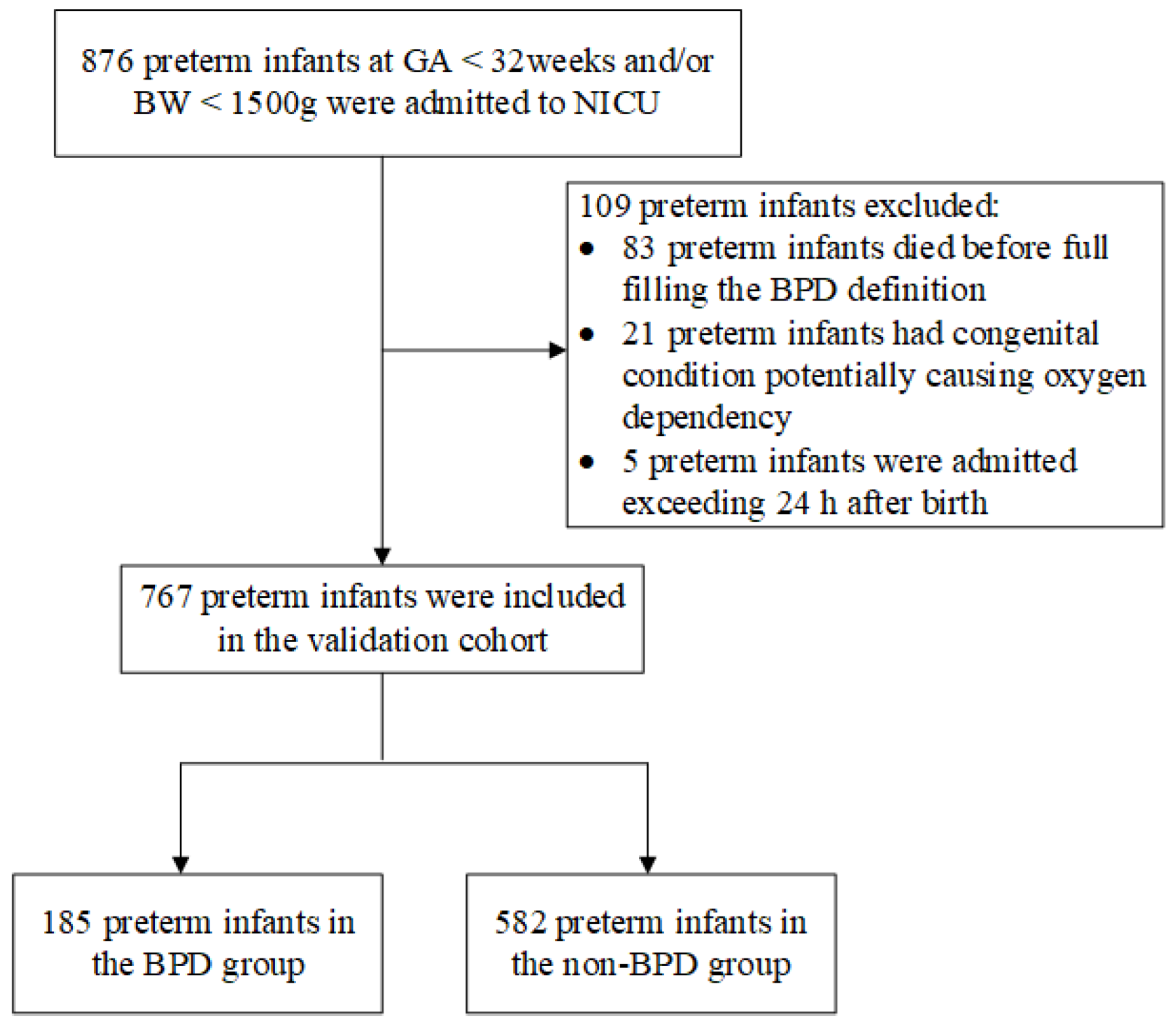
2.3.1. Validation Cohort
2.3.2. Definitions
- (1)
- The diagnosis of BPD was acquired according to the 2018 definition proposed by NICHD [24], preterm infants < 32 weeks’ gestation with radiographically confirmed persistent parenchymal lung disease, and at 36 weeks postmenstrual age (PMA) requiring a certain respiratory support and fraction of inspired oxygen (FiO2) for ≥3 consecutive days to maintain arterial oxygen saturation in the 90–95% range.
- (2)
- Maternal hypertensive disorders (MHD) included chronic hypertension (with blood pressure values ≥ 140/90 mmHg of any cause, hypertension was documented before pregnancy or before 20 weeks’ gestation), gestational hypertension (systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg occurring after 20 weeks’ gestation), preeclampsia (systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg along with proteinuria higher than 300 mg in 24 h, detected after 20 weeks’ gestation in a previously normotensive woman) and eclampsia [25].
- (3)
- Chorioamnionitis (CA) was defined as clinical CA with or without histological proven CA [26].
- (4)
- The administration of antenatal steroids was defined as a single course of 4 doses of 6 mg of dexamethasone given intramuscularly 12 h apart.
- (5)
- Small for gestational age (SGA) was defined as a BW below the 10th percentile or 2 standard deviations below the mean weight for the same GA [27].
- (6)
- Respiratory distress syndrome (RDS) was defined as a clinical symptom (progressive dyspnea several hours after birth) consistent with chest X-ray findings [28].
- (7)
- Surfactant treatment was given as early as possible according to the neonatal respiratory condition after birth combined with evidence of RDS [29].
- (8)
- Sepsis was defined as an infection that can be proven by the culture of pathogenic bacteria (including bacteria and fungi) in blood, cerebrospinal fluid, or other sterile cavities under the premise of abnormal clinical signs and symptoms [30]. Based on the time of onset, the onset time was split into early-onset sepsis ≤ 3 days, and late-onset sepsis > 3 days.
2.3.3. Statistical Analysis
3. Results
3.1. Meta-Analysis
3.1.1. Literature Search Results
3.1.2. Study Characteristics
3.1.3. Results of the Meta-Analysis
3.1.4. Publication Bias
3.2. Study Populations
3.2.1. Derivation Cohort
3.2.2. Validation Cohort
3.3. Risk Scoring Tool Development
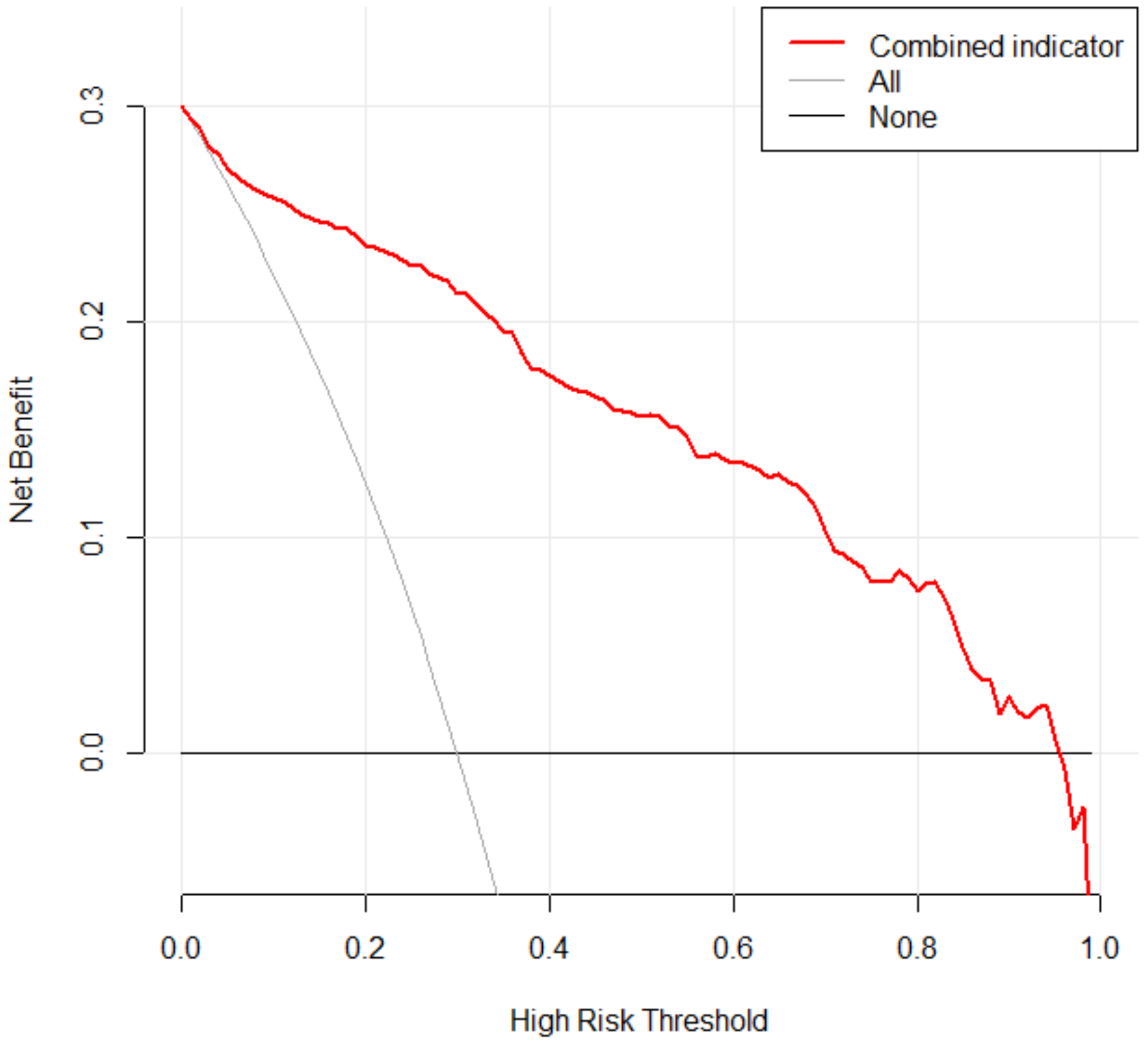
3.4. Risk Scoring Tool Validation
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stoll, B.J.; Hansen, N.I.; Bell, E.F.; Walsh, M.C.; Carlo, W.A.; Shankaran, S.; Laptook, A.R.; Sánchez, P.J.; Van Meurs, K.P.; Wyckoff, M.; et al. Trends in Care Practices, Morbidity, and Mortality of Extremely Preterm Neonates, 1993–2012. JAMA 2015, 314, 1039–1051. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakashima, T.; Inoue, H.; Sakemi, Y.; Ochiai, M.; Yamashita, H.; Ohga, S.; Neonatal Res Network, J. Trends in Bronchopulmonary Dysplasia Among Extremely Preterm Infants in Japan, 2003–2016. J. Pediatr. 2021, 230, 119–125.e117. [Google Scholar] [CrossRef] [PubMed]
- Siffel, C.; Kistler, K.D.; Lewis, J.F.M.; Sarda, S.P. Global incidence of bronchopulmonary dysplasia among extremely preterm infants: A systematic literature review. J. Matern.-Fetal Neonatal Med. 2021, 34, 1721–1731. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, V.C.; Zupancic, J.; Mccormick, M.C.; Croen, L.A.; Greene, J.; Escobar, G.J.; Richardson, D.K. Rehospitalization in the first year of life among infants with bronchopulmonary dysplasia. J. Pediatr. 2004, 144, 799–803. [Google Scholar] [CrossRef]
- Davidson, L.M.; Berkelhamer, S.K. Bronchopulmonary Dysplasia: Chronic Lung Disease of Infancy and Long-Term Pulmonary Outcomes. J. Clin. Med. 2017, 6, 4. [Google Scholar] [CrossRef] [Green Version]
- Cheong, J.; Doyle, L.W. An Update on Pulmonary and Neurodevelopmental Outcomes of Bronchopulmonary Dysplasia. Semin. Perinatol. 2018, 42, 478–484. [Google Scholar] [CrossRef]
- Twilhaar, E.S.; Wade, R.M.; de Kieviet, J.F.; van Goudoever, J.B.; van Elburg, R.M.; Oosterlaan, J. Cognitive Outcomes of Children Born Extremely or Very Preterm Since the 1990s and Associated Risk Factors: A Meta-analysis and Meta-regression. JAMA Pediatr. 2018, 172, 361–367. [Google Scholar] [CrossRef]
- Trembath, A.; Laughon, M.M. Predictors of bronchopulmonary dysplasia. Clin. Perinatol. 2012, 39, 585–601. [Google Scholar] [CrossRef] [Green Version]
- Bonadies, L.; Zaramella, P.; Porzionato, A.; Perilongo, G.; Muraca, M.; Baraldi, E. Present and Future of Bronchopulmonary Dysplasia. J. Clin. Med. 2020, 9, 1539. [Google Scholar] [CrossRef]
- Shahzad, T.; Radajewski, S.; Chao, C.M.; Bellusci, S.; Ehrhardt, H. Pathogenesis of bronchopulmonary dysplasia: When inflammation meets organ development. Mol. Cell. Pediatr. 2016, 3, 23. [Google Scholar] [CrossRef] [Green Version]
- Onland, W.; Debray, T.P.; Laughon, M.M.; Miedema, M.; Cools, F.; Askie, L.M.; Asselin, J.M.; Calvert, S.A.; Courtney, S.E.; Dani, C.; et al. Clinical prediction models for bronchopulmonary dysplasia: A systematic review and external validation study. BMC Pediatr. 2013, 13, 207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gursoy, T.; Hayran, M.; Derin, H.; Ovali, F. A clinical scoring system to predict the development of bronchopulmonary dysplasia. Am. J. Perinatol. 2015, 32, 659–666. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jassem-Bobowicz, J.M.; Klasa-Mazurkiewicz, D.; Zawrocki, A.; Stefanska, K.; Domzalska-Popadiuk, I.; Kwiatkowski, S.; Preis, K. Prediction Model for Bronchopulmonary Dysplasia in Preterm Newborns. Children 2021, 8, 886. [Google Scholar] [CrossRef] [PubMed]
- Ding, L.; Wang, H.; Geng, H.; Cui, N.; Huang, F.; Zhu, X.; Zhu, X. Prediction of Bronchopulmonary Dysplasia in Preterm Infants Using Postnatal Risk Factors. Front. Pediatr. 2020, 8, 349. [Google Scholar] [CrossRef] [PubMed]
- Cai, H.; Jiang, L.; Liu, Y.; Shen, T.; Yang, Z.; Wang, S.; Ma, Y. Development and verification of a risk prediction model for bronchopulmonary dysplasia in very low birth weight infants. Transl. Pediatr. 2021, 10, 2533–2543. [Google Scholar] [CrossRef]
- Wang, X.; Ma, Y.; Wang, S.; Dong, W.; Lei, X. Platelet is the early predictor of bronchopulmonary dysplasia in very premature infants: An observational cohort study. BMC Pulm. Med. 2022, 22, 109. [Google Scholar] [CrossRef]
- El Faleh, I.; Faouzi, M.; Adams, M.; Gerull, R.; Chnayna, J.; Giannoni, E.; Roth-Kleiner, M. Bronchopulmonary dysplasia: A predictive scoring system for very low birth weight infants. A diagnostic accuracy study with prospective data collection. Eur. J. Pediatr. 2021, 180, 2453–2461. [Google Scholar] [CrossRef] [PubMed]
- Kwok, T.C.; Batey, N.; Luu, K.L.; Prayle, A.; Sharkey, D. Bronchopulmonary dysplasia prediction models: A systematic review and meta-analysis with validation. Pediatr. Res. 2023, 1–12. [Google Scholar] [CrossRef]
- Laughon, M.M.; Langer, J.C.; Bose, C.L.; Smith, P.B.; Ambalavanan, N.; Kennedy, K.A.; Stoll, B.J.; Buchter, S.; Laptook, A.R.; Ehrenkranz, R.A.; et al. Prediction of bronchopulmonary dysplasia by postnatal age in extremely premature infants. Am. J. Respir. Crit. Care Med. 2011, 183, 1715–1722. [Google Scholar] [CrossRef] [Green Version]
- Shim, S.-Y.; Yun, J.Y.; Cho, S.J.; Kim, M.H.; Park, E.A. The Prediction of Bronchopulmonary Dysplasia in Very Low Birth Weight Infants through Clinical Indicators within 1 Hour of Delivery. J. Korean Med. Sci. 2021, 36, e81. [Google Scholar] [CrossRef]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000, 283, 2008–2012. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ (Clin. Res. Ed.) 2021, 372, n160. [Google Scholar] [CrossRef] [PubMed]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, R.D.; Jobe, A.H.; Koso-Thomas, M.; Bancalari, E.; Viscardi, R.M.; Hartert, T.V.; Ryan, R.M.; Kallapur, S.G.; Steinhorn, R.H.; Konduri, G.G.; et al. Bronchopulmonary Dysplasia: Executive Summary of a Workshop. J. Pediatr. 2018, 197, 300–308. [Google Scholar] [CrossRef] [PubMed]
- Rocha, G.M.; de Lima, F.F.; Machado, A.P.; Guimarães, H.A. Hypertensive Disorders during Pregnancy and Risk of Bronchopulmonary Dysplasia in Very Preterm Infants. Am. J. Perinatol. 2019, 36, 176–183. [Google Scholar] [CrossRef] [Green Version]
- Du Plessis, A.H.; van Rooyen, D.R.M.; Jardien-Baboo, S.; Ten Ham-Baloyi, W. Screening and diagnosis of women for chorioamnionitis: An integrative literature review. Midwifery 2022, 113, 103417. [Google Scholar] [CrossRef]
- Sharma, D.; Farahbakhsh, N.; Shastri, S.; Sharma, P. Intrauterine growth restriction—Part 2. J. Matern.-Fetal Neonatal. Med. 2016, 29, 4037–4048. [Google Scholar] [CrossRef]
- Duan, X.; Li, J.; Chen, L.; Shi, Y.; Chen, X.; Xue, T.; Liu, C.; Wang, X.; Qiu, Q.; Yu, Z.; et al. Surfactant Therapy for Respiratory Distress Syndrome in High- and Ultra-High-Altitude Settings. Front. Pediatr. 2022, 10, 777360. [Google Scholar] [CrossRef]
- Sweet, D.G.; Carnielli, V.; Greisen, G.; Hallman, M.; Ozek, E.; Te Pas, A.; Plavka, R.; Roehr, C.C.; Saugstad, O.D.; Simeoni, U.; et al. European Consensus Guidelines on the Management of Respiratory Distress Syndrome—2019 Update. Neonatology 2019, 115, 432–450. [Google Scholar] [CrossRef] [Green Version]
- Gao, Y.; Hou, L.; Lu, C.; Wang, Q.; Pan, B.; Wang, Q.; Tian, J.; Ge, L. Enteral Lactoferrin Supplementation for Preventing Sepsis and Necrotizing Enterocolitis in Preterm Infants: A Meta-Analysis With Trial Sequential Analysis of Randomized Controlled Trials. Front. Pharmacol. 2020, 11, 1186. [Google Scholar] [CrossRef]
- Abele-Horn, M.; Genzel-Boroviczeny, O.; Uhlig, T.; Zimmermann, A.; Peters, J.; Scholz, M. Ureaplasma urealyticum colonization and bronchopulmonary dysplasia: A comparative prospective multicentre study. Eur. J. Pediatr. 1998, 157, 1004–1011. [Google Scholar] [CrossRef] [PubMed]
- Hannaford, K.; Todd, D.A.; Jeffery, H.; John, E.; Blyth, K.; Gilbert, G.L. Role of ureaplasma urealyticum in lung disease of prematurity. Arch. Dis. Childhood. Fetal Neonatal. Ed. 1999, 81, F162–F167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Korhonen, P.; Tammela, O.; Koivisto, A.M.; Laippala, P.; Ikonen, S. Frequency and risk factors in bronchopulmonary dysplasia in a cohort of very low birth weight infants. Early Hum. Dev. 1999, 54, 245–258. [Google Scholar] [CrossRef] [PubMed]
- Marshall, D.D.; Kotelchuck, M.; Young, T.E.; Bose, C.L.; Kruyer, L.; O’Shea, T.M. Risk factors for chronic lung disease in the surfactant era: A North Carolina population-based study of very low birth weight infants. North Carolina Neonatologists Association. Pediatrics 1999, 104, 1345–1350. [Google Scholar] [CrossRef]
- Grupo Colaborativo Neocosur. Very-low-birth-weight infant outcomes in 11 South American NICUs. J. Perinatol. Off. J. Calif. Perinat. Assoc. 2002, 22, 2–7. [Google Scholar] [CrossRef] [Green Version]
- Redline, R.W.; Wilson-Costello, D.; Hack, M. Placental and other perinatal risk factors for chronic lung disease in very low birth weight infants. Pediatr. Res. 2002, 52, 713–719. [Google Scholar] [CrossRef]
- Reiss, I.; Landmann, E.; Heckmann, M.; Misselwitz, B.; Gortner, L. Increased risk of bronchopulmonary dysplasia and increased mortality in very preterm infants being small for gestational age. Arch. Gynecol. Obstet. 2003, 269, 40–44. [Google Scholar] [CrossRef]
- Antonucci, R.; Contu, P.; Porcella, A.; Atzeni, C.; Chiappe, S. Intrauterine smoke exposure: A new risk factor for bronchopulmonary dysplasia? J. Perinat. Med. 2004, 32, 272–277. [Google Scholar] [CrossRef]
- Choi, C.W.; Kim, B.I.; Park, J.D.; Koh, Y.Y.; Choi, J.H.; Choi, J.Y. Risk factors for the different types of chronic lung diseases of prematurity according to the preceding respiratory distress syndrome. Pediatr. Int. Off. J. Jpn. Pediatr. Soc. 2005, 47, 417–423. [Google Scholar] [CrossRef]
- Hentschel, J.; Berger, T.; Tschopp, A.; Muller, M.; Adams, M.; Bucher, H.U.; Swiss Neonatal, N. Population-based study of bronchopulmonary dysplasia in very low birth weight infants in Switzerland. Eur. J. Pediatr. 2005, 164, 292–297. [Google Scholar] [CrossRef]
- Tai, P.-Y.; Hsu, C.-H.; Kao, H.-H.; Hung, H.-Y.; Chang, J.-H.; Jim, W.-T. Risk Factors for Chronic Lung Disease in Very Low Birth Weight Infants: A Five-Year Multicenter Study in Taiwan. Clin. Neonatol. 2005, 12, 13–18. [Google Scholar] [CrossRef]
- Henderson-Smart, D.J.; Hutchinson, J.L.; Donoghue, D.A.; Evans, N.J.; Simpson, J.M.; Wright, I.; Australian New Zealand Neonatal Network. Prenatal predictors of chronic lung disease in very preterm infants. Arch. Dis. Child. -Fetal Neonatal Ed. 2006, 91, F40–F45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tapia, J.L.; Agost, D.; Alegria, A.; Standen, J.; Escobar, M.; Grandi, C.; Musante, G.; Zegarra, J.; Estay, A.; Ramirez, R.; et al. Bronchopulmonary dysplasia: Incidence, risk factors and resource utilization in a population of South American very low birth weight infants. J. Pediatr. 2006, 82, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Ameenudeen, S.A.K.M.; Boo, N.Y.; Chan, L.G. Risk factors associated with chronic lung disease in Malaysian very low birthweight infants. Med. J. Malays. 2007, 62, 40–45. [Google Scholar]
- Bhering, C.A.; Mochdece, C.C.; Moreira, M.E.; Rocco, J.R.; Sant’Anna, G.M. Bronchopulmonary dysplasia prediction model for 7-day-old infants. J. Pediatr. 2007, 83, 163–170. [Google Scholar] [CrossRef] [PubMed]
- Honma, Y.; Yada, Y.; Takahashi, N.; Momoi, M.Y.; Nakamura, Y. Certain type of chronic lung disease of newborns is associated with Ureaplasma urealyticum infection in utero. Pediatr. Int. Off. J. Jpn. Pediatr. Soc. 2007, 49, 479–484. [Google Scholar] [CrossRef]
- Demirel, N.; Bas, A.Y.; Zenciroglu, A. Bronchopulmonary dysplasia in very low birth weight infants. Indian J. Pediatr. 2009, 76, 695–698. [Google Scholar] [CrossRef]
- Guimaraes, H.; Rocha, G.; Vasconcellos, G.; Proenca, E.; Carreira, M.L.; Sossai, M.d.R.; Morais, B.; Martins, I.; Rodrigues, T.; Severo, M. Risk factors for bronchopulmonary dysplasia in five Portuguese neonatal intensive care units. Rev. Port. Pneumol. 2010, 16, 419–430. [Google Scholar] [CrossRef] [Green Version]
- Gantar, I.S.; Babnik, J.; Cerar, L.K.; Sinkovec, J.; Wraber, B. Prenatal and postnatal risk factors for developing bronchopulmonary dysplasia. Signa Vitae 2011, 6, 46–51. [Google Scholar] [CrossRef] [Green Version]
- Gortner, L.; Misselwitz, B.; Milligan, D.; Zeitlin, J.; Kollee, L.; Boerch, K.; Agostino, R.; Van Reempts, P.; Chabernaud, J.-L.; Breart, G.; et al. Rates of Bronchopulmonary Dysplasia in Very Preterm Neonates in Europe: Results from the MOSAIC Cohort. Neonatology 2011, 99, 112–117. [Google Scholar] [CrossRef]
- Gagliardi, L.; Bellu, R.; Lista, G.; Zanini, R. Do differences in delivery room intubation explain different rates of bronchopulmonary dysplasia between hospitals? Arch. Dis. Child. Fetal Neonatal Ed. 2011, 96, F30–F35. [Google Scholar] [CrossRef]
- Zhang, H.; Fang, J.; Su, H.; Chen, M. Risk factors for bronchopulmonary dysplasia in neonates born at ≤ 1500 g (1999–2009). Pediatr. Int. 2011, 53, 915–920. [Google Scholar] [CrossRef] [PubMed]
- Löfqvist, C.; Hellgren, G.; Niklasson, A.; Engström, E.; Ley, D.; Hansen-Pupp, I. Low postnatal serum IGF-I levels are associated with bronchopulmonary dysplasia (BPD). Acta Paediatr. 2012, 101, 1211–1216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Shea, J.E.; Davis, P.G.; Doyle, L.W. Maternal preeclampsia and risk of bronchopulmonary dysplasia in preterm infants. Pediatr. Res. 2012, 71, 210–214. [Google Scholar] [CrossRef] [PubMed]
- Rojas, M.X.; Rojas, M.A.; Lozano, J.M.; Rondon, M.A.; Charry, L.P. Regional variation on rates of bronchopulmonary dysplasia and associated risk factors. ISRN Pediatr. 2012, 2012, 685151. [Google Scholar] [CrossRef] [Green Version]
- Klinger, G.; Sokolover, N.; Boyko, V.; Sirota, L.; Lerner-Geva, L.; Reichman, B.; Israel Neonatal, N. Perinatal risk factors for bronchopulmonary dysplasia in a national cohort of very-low-birthweight infants. Am. J. Obstet. Gynecol. 2013, 208, 115.e1–115.e9. [Google Scholar] [CrossRef]
- Shima, Y.; Kumasaka, S.; Migita, M. Perinatal risk factors for adverse long-term pulmonary outcome in premature infants: Comparison of different definitions of bronchopulmonary dysplasia/chronic lung disease. Pediatr. Int. Off. J. Jpn. Pediatr. Soc. 2013, 55, 578–581. [Google Scholar] [CrossRef]
- Yen, T.-A.; Yang, H.-I.; Hsieh, W.-S.; Chou, H.-C.; Chen, C.-Y.; Tsou, K.-I.; Tsao, P.-N.; Taiwan Premature Infant Dev, C. Preeclampsia and the Risk of Bronchopulmonary Dysplasia in VLBW Infants: A Population Based Study. PLoS ONE 2013, 8, e75168. [Google Scholar] [CrossRef] [Green Version]
- Alshehri, M.A. Are preterm infants at high altitude at greater risk for the development of bronchopulmonary dysplasia? J. Trop. Pediatr. 2014, 60, 68–73. [Google Scholar] [CrossRef] [Green Version]
- Novitsky, A.; Tuttle, D.; Locke, R.G.; Saiman, L.; Mackley, A.; Paul, D.A. Prolonged Early Antibiotic Use and Bronchopulmonary Dysplasia in Very Low Birth Weight Infants. Am. J. Perinatol. 2015, 32, 43–48. [Google Scholar] [CrossRef]
- Sasi, A.; Abraham, V.; Davies-Tuck, M.; Polglase, G.R.; Jenkin, G.; Miller, S.L.; Malhotra, A. Impact of intrauterine growth restriction on preterm lung disease. Acta Paediatr. 2015, 104, e552–e556. [Google Scholar] [CrossRef] [PubMed]
- Duan, J.; Kong, X.; Li, Q.; Hua, S.; Zhang, S.; Zhang, X.; Feng, Z. Association between anemia and bronchopulmonary dysplasia in preterm infants. Sci. Rep. 2016, 6, 22717. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fonseca, L.T.; Senna, D.C.; Silveira, R.C.; Procianoy, R.S. Association between Breast Milk and Bronchopulmonary Dysplasia: A Single Center Observational Study. Am. J. Perinatol. 2017, 34, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Lio, A.; Rosati, P.; Pastorino, R.; Cota, F.; Tana, M.; Tirone, C.; Aurilia, C.; Ricci, C.; Gambacorta, A.; Paladini, A.; et al. Fetal Doppler velocimetry and bronchopulmonary dysplasia risk among growth-restricted preterm infants: An observational study. BMJ Open 2017, 7, e015232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soliman, N.; Chaput, K.; Alshaikh, B.; Yusuf, K. Preeclampsia and the Risk of Bronchopulmonary Dysplasia in Preterm Infants Less Than 32 Weeks’ Gestation. Am. J. Perinatol. 2017, 34, 585–592. [Google Scholar] [CrossRef]
- Jung, E.; Lee, B.S. Late-Onset Sepsis as a Risk Factor for Bronchopulmonary Dysplasia in Extremely Low Birth Weight Infants: A Nationwide Cohort Study. Sci. Rep. 2019, 9, 15448. [Google Scholar] [CrossRef] [Green Version]
- Mahallei, M.; Hosseini, M.B.; Esmaili, H.; Assadi, G.R. Relationship between Ureaplasma urealyticum Colonization and Bronchopulmonary Dysplasia in Very Low Birth Weight Premature Infants: A prospective cohort study. Iran. J. Neonatol. 2019, 10, 12–18. [Google Scholar] [CrossRef]
- Malikiwi, A.I.; Lee, Y.-M.; Davies-Tuck, M.; Wong, F.Y. Postnatal nutritional deficit is an independent predictor of bronchopulmonary dysplasia among extremely premature infants born at or less than 28 weeks gestation. Early Human Dev. 2019, 131, 29–35. [Google Scholar] [CrossRef]
- Patel, R.M.; Knezevic, A.; Yang, J.; Shenvi, N.; Hinkes, M.; Roback, J.D.; Easley, K.A.; Josephson, C.D. Enteral iron supplementation, red blood cell transfusion, and risk of bronchopulmonary dysplasia in very-low-birth-weight infants. Transfusion 2019, 59, 1675–1682. [Google Scholar] [CrossRef]
- Ryan, R.M.; Feng, R.; Bazacliu, C.; Ferkol, T.W.; Ren, C.L.; Mariani, T.J.; Poindexter, B.B.; Wang, F.; Moore, P.E.; Chougnet, C.; et al. Black Race Is Associated with a Lower Risk of Bronchopulmonary Dysplasia. J. Pediatr. 2019, 207, 130–135.e132. [Google Scholar] [CrossRef]
- Tagliaferro, T.; Jain, D.; Vanbuskirk, S.; Bancalari, E.; Claure, N. Maternal preeclampsia and respiratory outcomes in extremely premature infants. Pediatr. Res. 2019, 85, 693–696. [Google Scholar] [CrossRef] [PubMed]
- Zhou, D.; Shi, F.; Xiong, Y.; Zhou, M.; Wan, H.; Liu, H. Increased serum Th2 chemokine levels are associated with bronchopulmonary dysplasia in premature infants. Eur. J. Pediatr. 2019, 178, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Qiu, X.; Sun, P.; Lin, Y.; Huang, Z.; Yang, C.; Walther, F.J. Neonatal ibuprofen exposure and bronchopulmonary dysplasia in extremely premature infants. J. Perinatol. 2020, 40, 124–129. [Google Scholar] [CrossRef]
- Cokyaman, T.; Kavuncuoglu, S. Bronchopulmonary dysplasia frequency and risk factors in very low birth weight infants: A 3-year retrospective study. North. Clin. Istanb. 2020, 7, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.H.; Shin, S.H.; Kim, S.H.; Kim, Y.J.; Kim, H.S.J.S.R. The Association of Pregnancy-induced Hypertension with Bronchopulmonary Dysplasia—A Retrospective Study Based on the Korean Neonatal Network database. Sci. Rep. 2020, 10, 5600. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ebrahimi, M.E.; Romijn, M.; Vliegenthart, R.J.S.; Visser, D.H.; van Kaam, A.H.; Onland, W. The association between clinical and biochemical characteristics of late-onset sepsis and bronchopulmonary dysplasia in preterm infants. Eur. J. Pediatr. 2021, 180, 2147–2154. [Google Scholar] [CrossRef] [PubMed]
- Li, S.-J.; Feng, Q.; Tian, X.-Y.; Zhou, Y.; Ji, Y.; Li, Y.-M.; Zhai, S.-F.; Guo, W.; Zhang, F.; Zheng, R.-X.; et al. Delivery room resuscitation and short-term outcomes of extremely preterm and extremely low birth weight infants: A multicenter survey in North China. Chin. Med. J. 2021, 134, 1561–1568. [Google Scholar] [CrossRef]
- Lu, T.; Liang, B.; Jia, Y.; Cai, J.; Wang, D.; Liu, M.; He, B.; Wang, Q. Relationship between bronchopulmonary dysplasia, long-term lung function, and vitamin D level at birth in preterm infants. Transl. Pediatr. 2021, 10, 3075–3081. [Google Scholar] [CrossRef]
- Ming, S.; Zhang, D.; Chen, L.; Shi, Y. Effects of anemia and red blood cell transfusion in preterm infants on the development of bronchopulmonary dysplasia: A propensity score analysis. All Life 2021, 14, 830–839. [Google Scholar] [CrossRef]
- Sucasas Alonso, A.; Pertega Diaz, S.; Saez Soto, R.; Avila-Alvarez, A. Epidemiology and risk factors for bronchopulmonary dysplasia in preterm infants born at or less than 32 weeks of gestation. An. Pediatr. 2022, 96, 242–251. [Google Scholar] [CrossRef]
- Hartling, L.; Liang, Y.; Lacaze-Masmonteil, T. Chorioamnionitis as a risk factor for bronchopulmonary dysplasia: A systematic review and meta-analysis. Arch. Dis. Childhood. Fetal Neonatal Ed. 2012, 97, F8–F17. [Google Scholar] [CrossRef] [PubMed]
- Torchin, H.; Lorthe, E.; Goffinet, F.; Kayem, G.; Subtil, D.; Truffert, P.; Devisme, L.; Benhammou, V.; Jarreau, P.H.; Ancel, P.Y. Histologic Chorioamnionitis and Bronchopulmonary Dysplasia in Preterm Infants: The Epidemiologic Study on Low Gestational Ages 2 Cohort. J. Pediatr. 2017, 187, 98–104.e103. [Google Scholar] [CrossRef] [PubMed]
- Perniciaro, S.; Casarin, J.; Nosetti, L.; Binda, C.; Salvatore, S.; Ghezzi, F.; Agosti, M. Early- and Late-Respiratory Outcome in Very Low Birth Weight with or without Intrauterine Inflammation. Am. J. Perinatol. 2020, 37, S76–S83. [Google Scholar] [CrossRef] [PubMed]
- Villamor-Martinez, E.; Álvarez-Fuente, M.; Ghazi, A.M.T.; Degraeuwe, P.; Zimmermann, L.J.I.; Kramer, B.W.; Villamor, E. Association of Chorioamnionitis With Bronchopulmonary Dysplasia Among Preterm Infants: A Systematic Review, Meta-analysis, and Metaregression. JAMA Netw. Open 2019, 2, e1914611. [Google Scholar] [CrossRef] [PubMed]
- Ackermann, B.W.; Klotz, D.; Hentschel, R.; Thome, U.H.; van Kaam, A.H. High-frequency ventilation in preterm infants and neonates. Pediatr. Res. 2022, 1–9. [Google Scholar] [CrossRef]
- Isayama, T.; Lee, S.K.; Mori, R.; Kusuda, S.; Fujimura, M.; Ye, X.Y.; Shah, P.S. Comparison of mortality and morbidity of very low birth weight infants between Canada and Japan. Pediatrics 2012, 130, e957–e965. [Google Scholar] [CrossRef] [Green Version]
- Thébaud, B.; Goss, K.N.; Laughon, M.; Whitsett, J.A.; Abman, S.H.; Steinhorn, R.H.; Aschner, J.L.; Davis, P.G.; McGrath-Morrow, S.A.; Soll, R.F.; et al. Bronchopulmonary dysplasia. Nat. Reviews. Dis. Prim. 2019, 5, 78. [Google Scholar] [CrossRef]
- Rocha, G.; de Lima, F.F.; Machado, A.P.; Guimarães, H.; Proença, E.; Carvalho, C.; Martins, L.G.; Martins, T.; Freitas, A.; Dias, C.P.; et al. Small for gestational age very preterm infants present a higher risk of developing bronchopulmonary dysplasia. J. Neonatal-Perinat. Med. 2019, 12, 419–427. [Google Scholar] [CrossRef]
- Rozance, P.J.; Seedorf, G.J.; Brown, A.; Roe, G.; O’Meara, M.C.; Gien, J.; Tang, J.R.; Abman, S.H. Intrauterine growth restriction decreases pulmonary alveolar and vessel growth and causes pulmonary artery endothelial cell dysfunction in vitro in fetal sheep. Am. J. Physiology. Lung Cell. Mol. Physiol. 2011, 301, L860–L871. [Google Scholar] [CrossRef]
- Silveyra, P.; Fuentes, N.; Rodriguez Bauza, D.E. Sex and Gender Differences in Lung Disease. Adv. Exp. Med. Biol. 2021, 1304, 227–258. [Google Scholar] [CrossRef]
- Binet, M.E.; Bujold, E.; Lefebvre, F.; Tremblay, Y.; Piedboeuf, B. Role of gender in morbidity and mortality of extremely premature neonates. Am. J. Perinatol. 2012, 29, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Leary, S.; Das, P.; Ponnalagu, D.; Singh, H.; Bhandari, V. Genetic Strain and Sex Differences in a Hyperoxia-Induced Mouse Model of Varying Severity of Bronchopulmonary Dysplasia. Am. J. Pathol. 2019, 189, 999–1014. [Google Scholar] [CrossRef] [PubMed]
- Dalili, H.; Nili, F.; Sheikh, M.; Hardani, A.K.; Shariat, M.; Nayeri, F. Comparison of the Four Proposed Apgar Scoring Systems in the Assessment of Birth Asphyxia and Adverse Early Neurologic Outcomes. PLoS ONE 2015, 10, e0122116. [Google Scholar] [CrossRef]
- Cnattingius, S.; Norman, M.; Granath, F.; Petersson, G.; Stephansson, O.; Frisell, T. Apgar Score Components at 5 Minutes: Risks and Prediction of Neonatal Mortality. Paediatr. Perinat. Epidemiol. 2017, 31, 328–337. [Google Scholar] [CrossRef] [PubMed]
- Aly, H.; Massaro, A.N.; Patel, K.; El-Mohandes, A.A. Is it safer to intubate premature infants in the delivery room? Pediatrics 2005, 115, 1660–1665. [Google Scholar] [CrossRef]
- Qian, M.; Yu, Z.B.; Chen, X.H.; Xu, Y.; Ma, Y.L.; Jiang, S.Y.; Wang, H.Y.; Wang, Z.Q.; Han, L.R.; Li, S.S.; et al. Clinical features of preterm infants with a birth weight less than 1 500 g undergoing different intensities of resuscitation: A multicenter retrospective analysis. Chin. J. Contemp. Pediatr. 2021, 23, 593–598. [Google Scholar] [CrossRef]
- Kakkilaya, V.; Jubran, I.; Mashruwala, V.; Ramon, E.; Simcik, V.N.; Marshall, M.; Brown, L.S.; Jaleel, M.A.; Kapadia, V.S. Quality Improvement Project to Decrease Delivery Room Intubations in Preterm Infants. Pediatrics 2019, 143, e20180201. [Google Scholar] [CrossRef] [Green Version]
- Whitsett, J.A.; Wert, S.E.; Weaver, T.E. Diseases of pulmonary surfactant homeostasis. Annu. Rev. Pathol. 2015, 10, 371–393. [Google Scholar] [CrossRef] [Green Version]
- Behnke, J.; Lemyre, B.; Czernik, C.; Zimmer, K.P.; Ehrhardt, H.; Waitz, M. Non-Invasive Ventilation in Neonatology. Dtsch. Arztebl. Int. 2019, 116, 177–183. [Google Scholar] [CrossRef]
- Beitler, J.R.; Malhotra, A.; Thompson, B.T. Ventilator-induced Lung Injury. Clin. Chest Med. 2016, 37, 633–646. [Google Scholar] [CrossRef]
- Kalikkot Thekkeveedu, R.; El-Saie, A.; Prakash, V.; Katakam, L.; Shivanna, B. Ventilation-Induced Lung Injury (VILI) in Neonates: Evidence-Based Concepts and Lung-Protective Strategies. J. Clin. Med. 2022, 11, 557. [Google Scholar] [CrossRef] [PubMed]



| Risk Factors | Risk Stratification | OR | 95% CI | β-Coefficient | Scores |
|---|---|---|---|---|---|
| CA | yes/no | 3.56 | [2.49, 5.11] | 1.270 | 5 |
| GA | per 1 week increase | 0.64 | [0.62, 0.67] | −0.446 | −2 |
| BW | per 100 g increase | 0.78 | [0.76, 0.80] | −0.248 | −1 |
| Sex | male/female | 1.46 | [1.39, 1.54] | 0.378 | 2 |
| SGA | yes/no | 4.78 | [3.88, 5.88] | 1.564 | 6 |
| 5 min Apgar score | per 1 point increase | 0.71 | [0.64, 0.78] | −0.342 | −1 |
| DRI | yes/no | 2.77 | [2.27, 3.39] | 1.019 | 4 |
| Surfactant | yes/no | 3.59 | [2.90, 4.45] | 1.278 | 5 |
| RDS | yes/no | 5.08 | [4.06, 6.35] | 1.625 | 7 |
| Measurement Indicators | Sensitivity | Specificity | Youden Index | AUC | 95% CI | p |
|---|---|---|---|---|---|---|
| Combined indicator | 0.897 | 0.873 | 0.770 | 0.907 | [0.883, 0.931] | 0.000 |
| CA | 0.373 | 0.914 | 0.287 | 0.644 | [0.594, 0.693] | 0.000 |
| GA | 0.773 | 0.706 | 0.479 | 0.800 | [0.764, 0.837] | 0.000 |
| BW | 0.741 | 0.761 | 0.502 | 0.807 | [0.770, 0.844] | 0.000 |
| Sex | 0.616 | 0.510 | 0.126 | 0.563 | [0.516, 0.610] | 0.009 |
| SGA | 0.449 | 0.744 | 0.193 | 0.596 | [0.548, 0.645] | 0.000 |
| 5 min Apgar Score | 0.692 | 0.936 | 0.628 | 0.809 | [0.767, 0.851] | 0.000 |
| DRI | 0.514 | 0.837 | 0.351 | 0.675 | [0.627, 0.723] | 0.000 |
| Surfactant | 0.681 | 0.643 | 0.324 | 0.662 | [0.617, 0.707] | 0.000 |
| RDS | 0.957 | 0.302 | 0.259 | 0.630 | [0.588, 0.671] | 0.000 |
| Risk Stratification | Total (n = 767) | BPD (n = 185) | Prevalence Rate (%) | χ2 | p | OR (95% CI) |
|---|---|---|---|---|---|---|
| Low | 200 | 1 | 0.5 | |||
| Low-intermediate | 327 | 18 | 5.5 | 8.944 | 0.000 | 11.592 [1.535, 87.520] |
| High-intermediate | 221 | 148 | 67.0 | 202.852 | 0.000 | 403.452 [55.439, 2936.093] |
| High | 19 | 18 | 94.7 | 194.485 | 0.000 | 3582.000 [214.906,59703.777] |
| Bronchopulmonary Dysplasia Risk-Scoring Tool for Preterm Infants | |
|---|---|
| Variable Category and Risk Factors | Points |
| Chorioamnionitis | 5 |
| Gestational age (GA) (select one) | |
| ≥32 weeks | 0 |
| 24–31+6 weeks | 2 × [32 − GA] |
| <24 weeks | 18 |
| Birth weight (BW) (select one) | |
| ≥1500 g | 0 |
| 500–1499 g | 1 × [15 − BW/100] |
| <500 g | 11 |
| Male | 2 |
| Small for gestational age | 6 |
| 5 min Apgar score (select one) | |
| ≥8 | 0 |
| 3–7 | 1 × (8 − 5 min Apgar score) |
| ≤2 | 6 |
| Delivery room intubation | 4 |
| Surfactant | 5 |
| Respiratory distress syndrome | 7 |
| “[ ]” means ceiling function; | |
| Scoring risk ranges: 0–12, low; 13–25, low-intermediate; 26–44, high-intermediate; ≥45, high. | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, Z.; Wang, L.; Wang, Y.; Zhang, M.; Xu, Y.; Liu, A. Development and Validation of a Risk Scoring Tool for Bronchopulmonary Dysplasia in Preterm Infants Based on a Systematic Review and Meta-Analysis. Healthcare 2023, 11, 778. https://doi.org/10.3390/healthcare11050778
Yu Z, Wang L, Wang Y, Zhang M, Xu Y, Liu A. Development and Validation of a Risk Scoring Tool for Bronchopulmonary Dysplasia in Preterm Infants Based on a Systematic Review and Meta-Analysis. Healthcare. 2023; 11(5):778. https://doi.org/10.3390/healthcare11050778
Chicago/Turabian StyleYu, Zhumei, Lili Wang, Yang Wang, Min Zhang, Yanqin Xu, and Annuo Liu. 2023. "Development and Validation of a Risk Scoring Tool for Bronchopulmonary Dysplasia in Preterm Infants Based on a Systematic Review and Meta-Analysis" Healthcare 11, no. 5: 778. https://doi.org/10.3390/healthcare11050778
APA StyleYu, Z., Wang, L., Wang, Y., Zhang, M., Xu, Y., & Liu, A. (2023). Development and Validation of a Risk Scoring Tool for Bronchopulmonary Dysplasia in Preterm Infants Based on a Systematic Review and Meta-Analysis. Healthcare, 11(5), 778. https://doi.org/10.3390/healthcare11050778







