COVID-19 Prevention Strategies for Victoria Students within Educational Facilities: An AI-Based Modelling Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Area and Data Collection
2.2. Data Pre-Processing
2.3. Incremental Deep Learning RNN-GRU Model
2.4. RNN-GRU Model Performance Evaluation
2.5. Impact Score Analysis for the Risk Factors
3. Results
3.1. Descriptive Summary
3.2. RNN-GRU Model Performance Evaluation
3.3. Impact Score Analysis for Risk Factors of COVID-19 within Educational Facilities
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Weekly Epidemiological Update on COVID-19—12 October 2022. World Health Organization. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19 (accessed on 11 February 2023).
- Australian Government Department of Health and Aged Care. First Confirmed Case of Novel Coronavirus in Australia. Australian Government Department of Health and Aged Care. Available online: https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/first-confirmed-case-of-novel-coronavirus-in-australia (accessed on 10 December 2022).
- Lee, P.-I.; Hu, Y.-L.; Chen, P.-Y.; Huang, Y.-C.; Hsueh, P.-R. Are children less susceptible to COVID-19? J. Microbiol. Immunol. Infect. 2020, 53, 371–372. [Google Scholar] [CrossRef] [PubMed]
- Yuki, K.; Fujiogi, M.; Koutsogiannaki, S. COVID-19 pathophysiology: A review. Clin. Immunol. 2020, 215, 108427. [Google Scholar] [CrossRef]
- Nikolopoulou, G.B.; Maltezou, H.C. COVID-19 in Children: Where do we Stand? Arch. Med. Res. 2021, 53, 1–8. [Google Scholar] [CrossRef]
- McCafferty, C.; Cai, T.; Borgel, D.; Lasne, D.; Renolleau, S.; Vedrenne-Cloquet, M.; Bonnet, D.; Wu, J.; Zaw, T.; Bhatnagar, A.; et al. Pathophysiological pathway differences in children who present with COVID-19 ARDS compared to COVID -19 induced MIS-C. Nat. Commun. 2022, 13, 2391. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Liang, W.; Rhodes, R.E.; Duan, Y.; Wang, X.; Shang, B.; Yang, Y.; Jiao, J.; Yang, M.; Supriya, R.; et al. A systematic review and meta-analysis on the preventive behaviors in response to the COVID-19 pandemic among children and adolescents. BMC Public Health 2022, 22, e1201. [Google Scholar] [CrossRef]
- Lai, S.; Ruktanonchai, N.W.; Zhou, L.; Prosper, O.; Luo, W.; Floyd, J.R.; Wesolowski, A.; Santillana, M.; Zhang, C.; Du, X.; et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature 2020, 585, 410–413. [Google Scholar] [CrossRef] [PubMed]
- Howard, J.; Huang, A.; Li, Z.; Tufekci, Z.; Zdimal, V.; van der Westhuizen, H.-M.; von Delft, A.; Price, A.; Fridman, L.; Tang, L.-H.; et al. An evidence review of face masks against COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2014564118. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Pan, L.; Tang, S.; Ji, J.S.; Shi, X. Mask use during COVID-19: A risk adjusted strategy. Environ. Pollut. 2020, 266, 115099. [Google Scholar] [CrossRef]
- Güner, H.R.; Hasanoğlu, I.; Aktaş, F. COVID-19: Prevention and control measures in community. Turk. J. Med. Sci. 2020, 50, 571–577. [Google Scholar] [CrossRef]
- Hossain, A.D.; Jarolimova, J.; Elnaiem, A.; Huang, C.X.; Richterman, A.; Ivers, L.C. Effectiveness of contact tracing in the control of infectious diseases: A systematic review. Lancet Public Health 2022, 7, e259–e273. [Google Scholar] [CrossRef]
- Wang, X.; Du, Z.; James, E.; Fox, S.J.; Lachmann, M.; Meyers, L.A.; Bhavnani, D. The effectiveness of COVID-19 testing and contact tracing in a US city. Proc. Natl. Acad. Sci. USA 2022, 119, e2200652119. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Advice for Schools. Available online: https://www.education.vic.gov.au/school/Pages/coronavirus-advice-schools.aspx (accessed on 10 December 2022).
- Research. Monash Education. Available online: https://www.monash.edu/education/research (accessed on 12 December 2022).
- Victorian COVID-19 Data. Coronavirus Victoria. Available online: https://www.coronavirus.vic.gov.au/victorian-coronavirus-covid-19-data (accessed on 8 December 2022).
- Tan, W. School closures were over-weighted against the mitigation of COVID-19 transmission. Medicine 2021, 100, e26709. [Google Scholar] [CrossRef]
- Lyu, S.; Lee, V.C.S.; Liu, G. An Intelligent Hybrid Cloud-Based ANP and AI Model for Development Site Selection. In Intelligent Systems and Applications; IntelliSys 2022; Lecture Notes in Networks and Systems; Springer: Cham, Switzerland, 2022; pp. 84–102. [Google Scholar] [CrossRef]
- Song, Y.; Li, L.; Peng, Y.; Liu, D. Lithium-ion battery remaining useful life prediction based on GRU-RNN. In Proceedings of the 2018 12th International Conference on Reliability, Maintainability, and Safety (ICRMS), Shanghai, China, 17–19 October 2018; pp. 317–322. [Google Scholar]
- Zainuddin, Z.; EA, P.A.; Hasan, M.H. Predicting machine failure using recurrent neural network-gated recurrent unit (RNN-GRU) through time series data. Bull. Electr. Eng. Inform. 2021, 10, 870–878. [Google Scholar]
- Enrolment: School Age Requirements and Age Exemptions. education.vic.gov.au. Available online: https://www2.education.vic.gov.au/pal/enrolment/guidance/school-age-requirements (accessed on 8 December 2022).
- Coronavirus (COVID-19) Information. Victorian Government. Available online: https://www.vic.gov.au/coronavirus-covid-19-information (accessed on 10 December 2022).
- COVID-19 Government Response Tracker. Homepage. Available online: https://www.bsg.ox.ac.uk/research/covid-19-government-response-tracker (accessed on 1 December 2022).
- Promoting COVID-19 Vaccine Access for Students Aged 12+. Available online: https://www.education.vic.gov.au/Documents/about/department/covid-19/vaccinations/student-vaccine-pack/Students-Vaccine-Stakeholder-Pack.pdf (accessed on 11 February 2023).
- Coronavirus (COVID-19) Victoria. Coronavirus Victoria. Available online: https://www.coronavirus.vic.gov.au/ (accessed on 12 February 2023).
- Liu, Y.; Rocklöv, J. The effective reproductive number of the Omicron variant of SARS-CoV-2 is several times relative to Delta. J. Travel Med. 2022, 29, taac037. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Health Topics. World Health Organization. Available online: https://www.who.int/health-topics/ (accessed on 1 December 2022).
- Australian Government Department of Health and Aged Care. COVID-19 Disease and Symptoms. Australian Government Department of Health and Aged Care. Available online: https://www.health.gov.au/health-alerts/covid-19/symptoms (accessed on 1 December 2022).
- Yan, L.; Talic, S.; Wild, H.; Gasevic, D.; Gasević, D.; Ilic, D.; Deppeler, J.; Corrigan, D.; Martinez-Maldonado, R.; Trauer, J. Transmission of SARS-CoV-2 in a primary school setting with and without public health measures using real-world contact data: A modelling study. J. Glob. Health 2022, 12, 05034. [Google Scholar] [CrossRef]
- Chung, J.; Kastner, K.; Dinh, L.; Goel, K.; Courville, A.C.; Bengio, Y. A recurrent latent variable model for sequential data. Adv. Neural Inf. Process. Syst. 2015, 28. [Google Scholar]
- Gao, J.; Lanchantin, J.; Soffa, M.L.; Qi, Y. Black-box generation of adversarial text sequences to evade deep learning classifiers. In Proceedings of the 2018 IEEE Security and Privacy Workshops (SPW), San Francisco, CA, USA, 24 May 2018; pp. 50–56. [Google Scholar]
- Stephen, R.I.; Olumoh, J.; Tyndall, J.; Adegboye, O. Risk Factors for COVID-19 Infection among Healthcare Workers in North-East Nigeria. Healthcare 2022, 10, 1919. [Google Scholar] [CrossRef]
- Esposito, S.; Principi, N. School closure during the coronavirus disease 2019 (COVID-19) pandemic: An effective intervention at the global level? JAMA Pediatr. 2020, 174, 921–922. [Google Scholar] [CrossRef]
- BBhuiyan, M.U.; Stiboy, E.; Hassan, M.Z.; Chan, M.; Islam, M.S.; Haider, N.; Jaffe, A.; Homaira, N. Epidemiology of COVID-19 infection in young children under five years: A systematic review and meta-analysis. Vaccine 2021, 39, 667–677. [Google Scholar] [CrossRef] [PubMed]
- Vitiello, A.; Ferrara, F.; Troiano, V.; La Porta, R. COVID-19 vaccines and decreased transmission of SARS-CoV-2. Inflammopharmacology 2021, 29, 1357–1360. [Google Scholar] [CrossRef]
- Schoch-Spana, M.; Brunson, E.K.; Long, R.; Ruth, A.; Ravi, S.J.; Trotochaud, M.; Borio, L.; Brewer, J.; Buccina, J.; Connell, N.; et al. The public’s role in COVID-19 vaccination: Human-centered recommendations to enhance pandemic vaccine awareness, access, and acceptance in the United States. Vaccine 2020, 39, 6004–6012. [Google Scholar] [CrossRef] [PubMed]
- Al-Hazmi, A.; Gosadi, I.; Somily, A.; Alsubaie, S.; Bin Saeed, A. Knowledge, attitude and practice of secondary schools and university students toward Middle East Respiratory Syndrome epidemic in Saudi Arabia: A cross-sectional study. Saudi J. Biol. Sci. 2018, 25, 572–577. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tran, T.H.; Sasikumar, S.N.; Hennessy, A.; O’Loughlin, A.; Morgan, L. Associations between restrictions on public mobility and slowing of new COVID -19 case rates in three countries. Med. J. Aust. 2020, 213, 471–473. [Google Scholar] [CrossRef] [PubMed]
- Tamang, S.T.; Lhendup, K.; Dorji, T. Control of travel-related COVID-19 in Bhutan. J. Travel Med. 2021, 28, taab137. [Google Scholar] [CrossRef]
- Kharroubi, S.; Saleh, F. Are Lockdown Measures Effective Against COVID-19? Front. Public Health 2020, 8, 549692. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Roy, D.; Sinha, K.; Parveen, S.; Sharma, G.; Joshi, G. Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res. 2020, 293, 113429. [Google Scholar] [CrossRef] [PubMed]
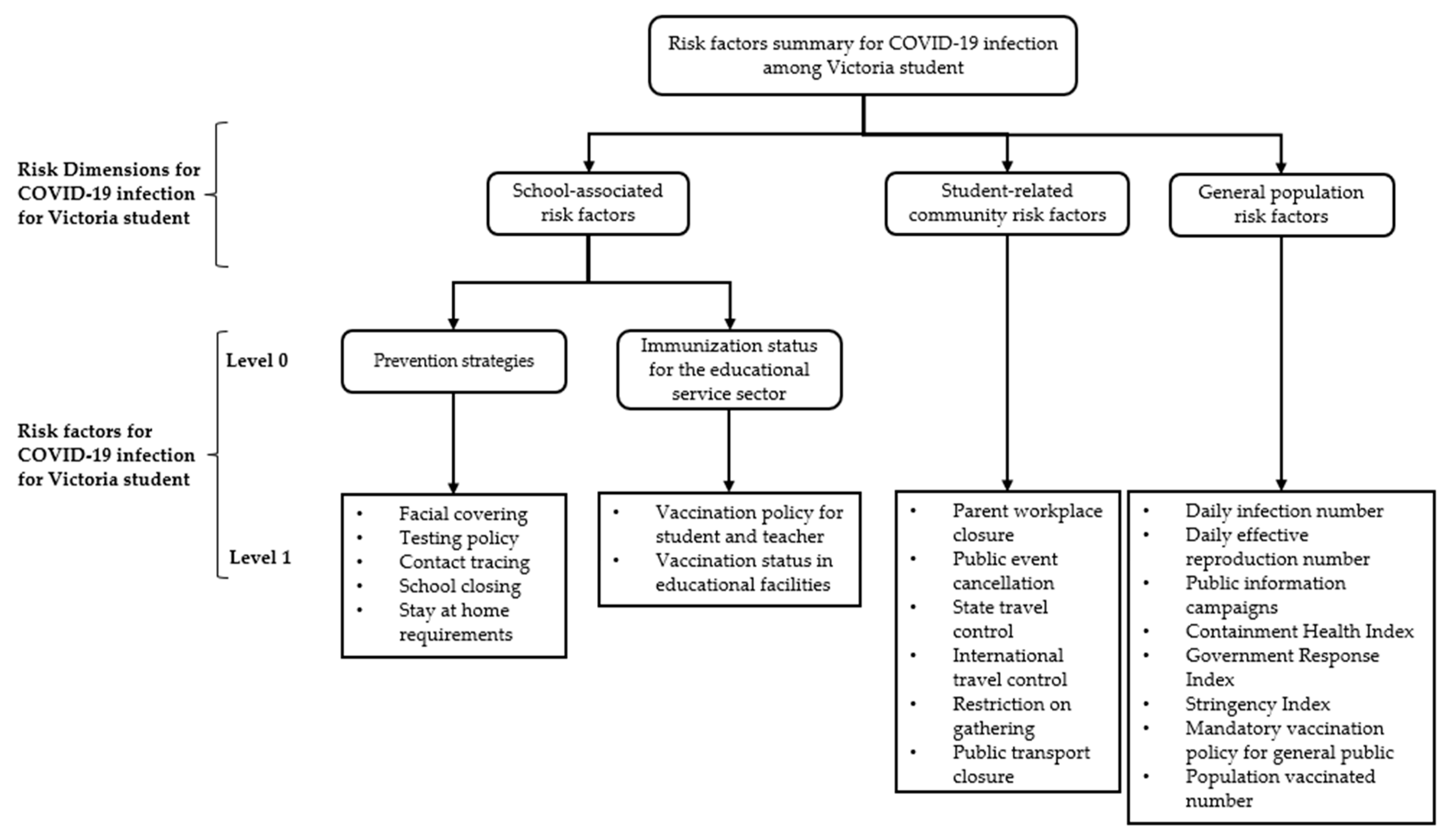







| Dimensions | Risk Factors | Description |
|---|---|---|
| School-associated risk factors (Prevention strategies) | Facial covering | Facial covering requirement |
| Testing policy | Testing policy of a symptomatic person | |
| Contact tracing | School-initiated contact tracing following a positive diagnosis | |
| School closing | School operation status: open or closed | |
| Stay at home requirements | The policy that instructs people to remain at home and not leave for non-essential purposes | |
| School-associated risk factors (Immunisation status for the educational service sector) | Vaccination policy for student and teacher | Policies for vaccine delivery of the educators in primary and secondary schools, tertiary education students, and staff |
| Vaccination status in educational facilities | Vaccination status for the educators in primary and secondary school, tertiary education students and staff | |
| Student-related community risk factors | Parent workplace closure | Parent or relative’s workplace operation status: open or closed |
| Public event cancellation | Public events cancelling status. This factor could lead to a higher secondary infection within the educational facilities | |
| State travel control | Restrictions on internal movement within the state | |
| International travel control | Restrictions on international travel | |
| Restrictions on gatherings | Social gathering restriction level: limit the number of people who can gather in one public place at a given time | |
| Public transport closing | Operation status: open or closed. Student commute to school by public transport, which may infect them with COVID-19 and lead a secondary transmission within the educational facilities | |
| General population risk factors | Daily infection number | Daily infection number within the Victoria area |
| Daily effective reproduction number | Spreadability of COVID-19 | |
| Public information campaigns | COVID-19 public information campaign | |
| Containment Health Index | Government containment health policy index | |
| Government Response Index | Government COVID-19 Response Index | |
| Stringency Index | Social restriction level | |
| Mandatory vaccination policy | Mandatory vaccination policy for the general public | |
| Population vaccinated number | The number of vaccinated people in Victoria |
| GRU Component | Formula | Function |
|---|---|---|
| Reset gate | Sigmoid function will transfer value into range of 0 to 1 to decide proportion of data for forget purpose | |
| Update gate | Sigmoid function will transfer value into range of 0 to 1 to decide proportion of data for update purpose | |
| Output | Update output-based results from reset and update gate |
| Model | 0–9 Years | 10–19 Years | ||||
|---|---|---|---|---|---|---|
| R2 | RMSE | MAE | R2 | RMSE | MAE | |
| RNN-GRU | 0.9796 | 0.2777 | 0.0601 | 0.9796 | 0.2809 | 0.0634 |
| Kernel Ridge | 0.8649 | 0.3795 | 0.0965 | 0.9461 | 0.3256 | 0.0853 |
| Ridge regression | 0.7879 | 0.4249 | 0.1446 | 0.9244 | 0.3543 | 0.1130 |
| Bayesian Ridge | 0.7818 | 0.4279 | 0.1380 | 0.9223 | 0.3568 | 0.1202 |
| Gradient Boosting Regressor | 0.7538 | 0.4410 | 0.1622 | 0.9161 | 0.3637 | 0.1181 |
| Lasso regression | 0.7478 | 0.4437 | 0.1508 | 0.9156 | 0.3643 | 0.1241 |
| ElasticNet | 0.7415 | 0.4464 | 0.1524 | 0.8781 | 0.3992 | 0.1498 |
| XG Boost Regressor | 0.7409 | 0.4467 | 0.1512 | 0.8735 | 0.4029 | 0.1221 |
| Random forest | 0.3751 | 0.5567 | 0.2781 | 0.7233 | 0.4901 | 0.1963 |
| Support vector regression | 0.2311 | 0.5863 | 0.2956 | 0.7089 | 0.4963 | 0.2047 |
| Dimensions | Risk Factors | Age Group | Total | ||
|---|---|---|---|---|---|
| Group 0–9 | Group 10–19 | Sum of Risk Factors | Sum of Dimensions | ||
| School-associated risk factors (Prevention strategies) | Contact tracing | 0.2771 | 0.3340 | 0.6110 1 | 3.0372 (23.77%) 2 |
| Testing policy | 0.2734 | 0.3375 | 0.6109 | ||
| Facial Coverings | 0.2721 | 0.3350 | 0.6071 | ||
| School closing | 0.2738 | 0.3323 | 0.6061 | ||
| Stay at home requirements | 0.2716 | 0.3305 | 0.6022 | ||
| School-associated risk factors (Immunisation status for the educational service sector) | Vaccination policy for student and teacher | 0.2758 | 0.3341 | 0.6100 | 1.2159 (9.52%) 2 |
| Vaccination statue in educational facilities | 0.2727 | 0.3332 | 0.6059 | ||
| Student-related community risk factors | State travel control | 0.2743 | 0.3390 | 0.6133 | 3.6534 (28.59%) |
| International travel controls | 0.2757 | 0.3357 | 0.6114 | ||
| Public event cancellation | 0.2764 | 0.3337 | 0.6101 | ||
| Restrictions on gatherings | 0.2772 | 0.3308 | 0.6080 | ||
| Public transport Closing | 0.2748 | 0.3314 | 0.6063 | ||
| Parent workplace closure | 0.2720 | 0.3324 | 0.6043 | ||
| General population risk factors | Daily infection number | 0.2755 | 0.3365 | 0.6121 | 4.8714 (38.12%) |
| Mandatory vaccination policy | 0.2782 | 0.3319 | 0.6101 | ||
| Stringency Index | 0.2740 | 0.3359 | 0.6100 | ||
| Public information campaigns | 0.2720 | 0.3366 | 0.6086 | ||
| Population Vaccinated | 0.2766 | 0.3316 | 0.6082 | ||
| Total Effective reproduction number | 0.2728 | 0.3349 | 0.6077 | ||
| Containment Health Index | 0.2756 | 0.3319 | 0.6075 | ||
| Government Response Index | 0.2745 | 0.3327 | 0.6072 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lyu, S.; Adegboye, O.; Adhinugraha, K.; Emeto, T.I.; Taniar, D. COVID-19 Prevention Strategies for Victoria Students within Educational Facilities: An AI-Based Modelling Study. Healthcare 2023, 11, 860. https://doi.org/10.3390/healthcare11060860
Lyu S, Adegboye O, Adhinugraha K, Emeto TI, Taniar D. COVID-19 Prevention Strategies for Victoria Students within Educational Facilities: An AI-Based Modelling Study. Healthcare. 2023; 11(6):860. https://doi.org/10.3390/healthcare11060860
Chicago/Turabian StyleLyu, Shiyang, Oyelola Adegboye, Kiki Adhinugraha, Theophilus I. Emeto, and David Taniar. 2023. "COVID-19 Prevention Strategies for Victoria Students within Educational Facilities: An AI-Based Modelling Study" Healthcare 11, no. 6: 860. https://doi.org/10.3390/healthcare11060860
APA StyleLyu, S., Adegboye, O., Adhinugraha, K., Emeto, T. I., & Taniar, D. (2023). COVID-19 Prevention Strategies for Victoria Students within Educational Facilities: An AI-Based Modelling Study. Healthcare, 11(6), 860. https://doi.org/10.3390/healthcare11060860








