Home-Based Exergame Program to Improve Physical Function, Fall Efficacy, Depression and Quality of Life in Community-Dwelling Older Adults: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
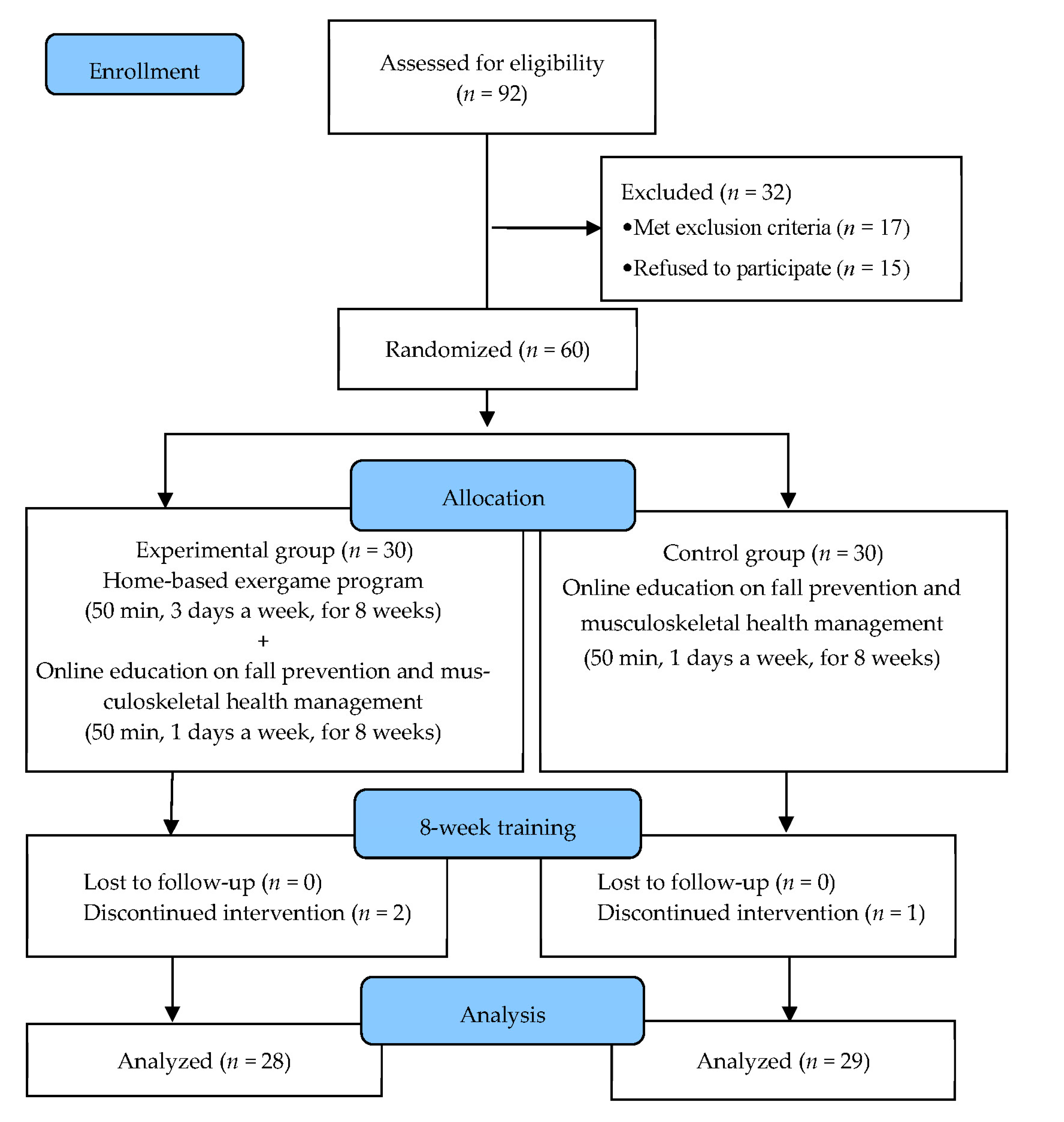
2.1. Study Design
2.2. Participants
2.3. Sample-Size Calculation
2.4. Experimental Procedures
2.5. Intervention
2.6. Outcome Measurements
2.6.1. Physical Function
2.6.2. Falls Efficacy
2.6.3. Depression
2.6.4. Health-Related Quality of Life
2.6.5. Mini-Mental State Examination (MMSE)
2.7. Statistical Analysis
3. Results
3.1. General Characteristics of the Subjects
3.2. Changes in Physical Function
3.3. Changes in Fall Efficacy and Depression
3.4. Changes in Health-Related Quality of Life
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yang, Y.; Zheng, R.; Zhao, L. Population aging, health investment and economic growth: Based on a cross-country panel data analysis. Int. J. Environ. Res. Public Health 2021, 18, 1801. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services. 2021 Profile of Older Americans. Available online: https://acl.gov/aging-and-disability-in-america/data-and-research/profile-older-americans (accessed on 20 January 2023).
- Peel, N.M.; McClure, R.J.; Bartlett, H.P. Behavioral determinants of healthy aging. Am. J. Prev. Med. 2005, 28, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.K.; Leng, X.; Hsu, F.C.; Kritchevsky, S.B.; Ding, J.; Earnest, C.P.; Ferrucci, L.; Goodpaster, B.H.; Guralnik, J.M.; Lenchik, L.; et al. The impact of sarcopenia on a physical activity intervention: The lifestyle interventions and independence for elders pilot study (life-p). J. Nutr. Health Aging 2014, 18, 59–64. [Google Scholar] [CrossRef]
- Di Filippo, E.S.; Bondi, D.; Pietrangelo, T.; Fanò-Illic, G.; Fulle, S. Molecular and cellular aspects of sarcopenia, muscle healthy aging and physical conditioning in the elderly. J. Sci. Sport Exerc. 2020, 2, 246–257. [Google Scholar] [CrossRef]
- Marzetti, E.; Leeuwenburgh, C. Skeletal muscle apoptosis, sarcopenia and frailty at old age. Exp. Gerontol. 2006, 41, 1234–1238. [Google Scholar] [CrossRef]
- Walle-Hansen, M.M.; Ranhoff, A.H.; Mellingsaeter, M.; Wang-Hansen, M.S.; Myrstad, M. Health-related quality of life, functional decline, and long-term mortality in older patients following hospitalisation due to COVID-19. BMC Geriatr. 2021, 21, 199. [Google Scholar] [CrossRef]
- Sjodin, H.; Wilder-Smith, A.; Osman, S.; Farooq, Z.; Rocklov, J. Only strict quarantine measures can curb the coronavirus disease (COVID-19) outbreak in italy, 2020. Eurosurveill 2020, 25, 2000280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parmet, W.E.; Sinha, M.S. COVID-19—The law and limits of quarantine. N. Engl. J. Med. 2020, 382, e28. [Google Scholar] [CrossRef]
- Kirwan, R.; McCullough, D.; Butler, T.; Perez de Heredia, F.; Davies, I.G.; Stewart, C. Sarcopenia during covid-19 lockdown restrictions: Long-term health effects of short-term muscle loss. Geroscience 2020, 42, 1547–1578. [Google Scholar] [CrossRef]
- Huang, B.; Huang, Z.; Tan, J.; Xu, H.; Deng, K.; Cheng, J.; Ren, Z.; Gong, X.; Gao, Y. The mediating and interacting role of physical activity and sedentary behavior between diabetes and depression in people with obesity in united states. J. Diabetes Complicat. 2021, 35, 107764. [Google Scholar] [CrossRef]
- Franklin, B.A.; Eijsvogels, T.M.H.; Pandey, A.; Quindry, J.; Toth, P.P. Physical activity, cardiorespiratory fitness, and cardiovascular health: A clinical practice statement of the aspc part i: Bioenergetics, contemporary physical activity recommendations, benefits, risks, extreme exercise regimens, potential maladaptations. Am. J. Prev. Cardiol. 2022, 12, 100424. [Google Scholar] [CrossRef] [PubMed]
- Binda, S.M.; Culham, E.G.; Brouwer, B. Balance, muscle strength, and fear of falling in older adults. Exp. Aging Res. 2003, 29, 205–219. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, M.K.; Nordqvist, A.; Karlsson, C. Physical activity, muscle function, falls and fractures. Food Nutr. Res. 2008, 52, 1920. [Google Scholar] [CrossRef] [Green Version]
- Ensrud, K.E.; Ewing, S.K.; Taylor, B.C.; Fink, H.A.; Cawthon, P.M.; Stone, K.L.; Hillier, T.A.; Cauley, J.A.; Hochberg, M.C.; Rodondi, N.; et al. Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch. Intern. Med. 2008, 168, 382–389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biderman, A.; Cwikel, J.; Fried, A.V.; Galinsky, D. Depression and falls among community dwelling elderly people: A search for common risk factors. J. Epidemiol. Community Health 2002, 56, 631–636. [Google Scholar] [CrossRef] [Green Version]
- Shubert, T.E.; McCulloch, K.; Hartman, M.; Giuliani, C.A. The effect of an exercise-based balance intervention on physical and cognitive performance for older adults: A pilot study. J. Geriatr. Phys. Ther. 2010, 33, 157–164. [Google Scholar] [CrossRef]
- Chase, J.A. Interventions to increase physical activity among older adults: A meta-analysis. Gerontologist 2015, 55, 706–718. [Google Scholar] [CrossRef] [Green Version]
- Park, S.H.; Han, K.S.; Kang, C.B. Effects of exercise programs on depressive symptoms, quality of life, and self-esteem in older people: A systematic review of randomized controlled trials. Appl. Nurs. Res. 2014, 27, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Suleiman-Martos, N.; Garcia-Lara, R.; Albendin-Garcia, L.; Romero-Bejar, J.L.; Canadas-De La Fuente, G.A.; Monsalve-Reyes, C.; Gomez-Urquiza, J.L. Effects of active video games on physical function in independent community-dwelling older adults: A systematic review and meta-analysis. J. Adv. Nurs. 2022, 78, 1228–1244. [Google Scholar] [CrossRef]
- Wang, R.Y.; Huang, Y.C.; Zhou, J.H.; Cheng, S.J.; Yang, Y.R. Effects of exergame-based dual-task training on executive function and dual-task performance in community-dwelling older people: A randomized-controlled trial. Games Health J. 2021, 10, 347–354. [Google Scholar] [CrossRef]
- Ambrosino, P.; Fuschillo, S.; Papa, A.; Di Minno, M.N.D.; Maniscalco, M. Exergaming as a supportive tool for home-based rehabilitation in the COVID-19 pandemic era. Games Health J. 2020, 9, 311–313. [Google Scholar] [CrossRef] [PubMed]
- Chao, Y.Y.; Scherer, Y.K.; Montgomery, C.A. Effects of using nintendo wii exergames in older adults: A review of the literature. J. Aging Health 2015, 27, 379–402. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.M.; Chen Hsieh, J.S.; Chen, Y.C.; Yang, S.Y.; Lin, H.K. Effects of kinect exergames on balance training among community older adults: A randomized controlled trial. Medicine 2020, 99, e21228. [Google Scholar] [CrossRef]
- Campo-Prieto, P.; Cancela, J.M.; Rodríguez-Fuentes, G. Immersive virtual reality as physical therapy in older adults: Present or future (systematic review). Virtual Real. 2021, 25, 801–817. [Google Scholar] [CrossRef]
- Capodaglio, E.M.; Cavalagli, A.; Panigazzi, M. Exergame for the functional rehabilitation of adults over 55 with neurological diseases. G. Ital. Med. Lav. Ergon. 2022, 44, 59–76. [Google Scholar]
- Alfieri, F.M.; da Silva Dias, C.; de Oliveira, N.C.; Battistella, L.R. Gamification in musculoskeletal rehabilitation. Curr. Rev. Musculoskelet. Med. 2022, 15, 629–636. [Google Scholar] [CrossRef] [PubMed]
- Saghaei, M. Random allocation software for parallel group randomized trials. BMC Med. Res. Methodol. 2004, 4, 26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haines, T.P.; Russell, T.; Brauer, S.G.; Erwin, S.; Lane, P.; Urry, S.; Jasiewicz, J.; Condie, P. Effectiveness of a video-based exercise programme to reduce falls and improve health-related quality of life among older adults discharged from hospital: A pilot randomized controlled trial. Clin. Rehabil. 2009, 23, 973–985. [Google Scholar] [CrossRef]
- Khanal, P.; He, L.; Stebbings, G.K.; Onambele-Pearson, G.L.; Degens, H.; Williams, A.G.; Thomis, M.; Morse, C.I. Static one-leg standing balance test as a screening tool for low muscle mass in healthy elderly women. Aging Clin. Exp. Res. 2021, 33, 1831–1839. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the probability for falls in community-dwelling older adults using the timed up & go test. Phys. Ther. 2000, 80, 896–903. [Google Scholar]
- Muehlbauer, T.; Roth, R.; Mueller, S.; Granacher, U. Intra and intersession reliability of balance measures during one-leg standing in young adults. J. Strength Cond. Res. 2011, 25, 2228–2234. [Google Scholar] [CrossRef] [PubMed]
- Downs, S.; Marquez, J.; Chiarelli, P. The berg balance scale has high intra- and inter-rater reliability but absolute reliability varies across the scale: A systematic review. J. Physiother. 2013, 59, 93–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duncan, P.W.; Weiner, D.K.; Chandler, J.; Studenski, S. Functional reach: A new clinical measure of balance. J. Gerontol. 1990, 45, M192–M197. [Google Scholar] [CrossRef]
- Ng, S.S.; Hui-Chan, C.W. The timed up & go test: Its reliability and association with lower-limb impairments and locomotor capacities in people with chronic stroke. Arch. Phys. Med. Rehabil. 2005, 86, 1641–1647. [Google Scholar] [PubMed]
- Duncan, P.W.; Propst, M.; Nelson, S.G. Reliability of the fugl-meyer assessment of sensorimotor recovery following cerebrovascular accident. Phys. Ther. 1983, 63, 1606–1610. [Google Scholar] [CrossRef]
- Hill, K.D.; Schwarz, J.A.; Kalogeropoulos, A.J.; Gibson, S.J. Fear of falling revisited. Arch. Phys. Med. Rehabil. 1996, 77, 1025–1029. [Google Scholar] [CrossRef]
- Resnick, B.; Orwig, D.; Yu-Yahiro, J.; Hawkes, W.; Shardell, M.; Hebel, J.R.; Zimmerman, S.; Golden, J.; Werner, M.; Magaziner, J. Testing the effectiveness of the exercise plus program in older women post-hip fracture. Ann. Behav. Med. 2007, 34, 67–76. [Google Scholar] [CrossRef]
- Kempen, G.I.; Yardley, L.; Van Haastregt, J.C.; Zijlstra, G.R.; Beyer, N.; Hauer, K.; Todd, C. The short fes-i: A shortened version of the falls efficacy scale-international to assess fear of falling. Age Ageing 2008, 37, 45–50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shin, C.; Park, M.H.; Lee, S.H.; Ko, Y.H.; Kim, Y.K.; Han, K.M.; Jeong, H.G.; Han, C. Usefulness of the 15-item geriatric depression scale (gds-15) for classifying minor and major depressive disorders among community-dwelling elders. J. Affect. Disord. 2019, 259, 370–375. [Google Scholar] [CrossRef]
- Ertan, T.; Eker, E. Reliability, validity, and factor structure of the geriatric depression scale in turkish elderly: Are there different factor structures for different cultures? Int. Psychogeriatr. 2000, 12, 163–172. [Google Scholar] [CrossRef]
- Lins, L.; Carvalho, F.M. Sf-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med. 2016, 4, 2050312116671725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McHorney, C.A.; Ware Johne, J.; Anastasiae, R. The mos 36-item short-form health survey (sf-36): Ii. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med. Care 1993, 31, 247–263. [Google Scholar] [CrossRef] [Green Version]
- Ware, J.E., Jr.; Sherbourne, C.D. The mos 36-item short-form health survey (sf-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Tombaugh, T.N.; McIntyre, N.J. The mini-mental state examination: A comprehensive review. J. Am. Geriatr. Soc. 1992, 40, 922–935. [Google Scholar] [CrossRef]
- Talkowski, J.B.; Brach, J.S.; Studenski, S.; Newman, A.B. Impact of health perception, balance perception, fall history, balance performance, and gait speed on walking activity in older adults. Phys. Ther. 2008, 88, 1474–1481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maki, B.E.; Holliday, P.J.; Topper, A.K. A prospective study of postural balance and risk of falling in an ambulatory and independent elderly population. J. Gerontol. 1994, 49, M72–M84. [Google Scholar] [CrossRef]
- Lord, S.R.; Clark, R.D.; Webster, I.W. Physiological factors associated with falls in an elderly population. J. Am. Geriatr. Soc. 1991, 39, 1194–1200. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Speechley, M.; Ginter, S.F. Risk factors for falls among elderly persons living in the community. N. Engl. J. Med. 1988, 319, 1701–1707. [Google Scholar] [CrossRef]
- Reelick, M.F.; van Iersel, M.B.; Kessels, R.P.; Rikkert, M.G. The influence of fear of falling on gait and balance in older people. Age Ageing 2009, 38, 435–440. [Google Scholar] [CrossRef] [Green Version]
- El-Bagalaty, A.E.; Mohamed, M.E.; Abdelraouf, O.R.; Abdel Ghafar, M.A.; Abdelaal, A.K.; Abdelgalil, A.A.; Mousa, G.S. Balance and fall risk assessment in community-dwelling older adults after recovery from COVID-19: A cross-sectional study. Sports 2023, 11, 28. [Google Scholar] [CrossRef]
- Pua, Y.H.; Ong, P.H.; Clark, R.A.; Matcher, D.B.; Lim, E.C. Falls efficacy, postural balance, and risk for falls in older adults with falls-related emergency department visits: Prospective cohort study. BMC Geriatr. 2017, 17, 291. [Google Scholar] [CrossRef] [Green Version]
- Lai, C.H.; Peng, C.W.; Chen, Y.L.; Huang, C.P.; Hsiao, Y.L.; Chen, S.C. Effects of interactive video-game based system exercise on the balance of the elderly. Gait Posture 2013, 37, 511–515. [Google Scholar] [CrossRef] [PubMed]
- Cicek, A.; Ozdincler, A.R.; Tarakci, E. Interactive video game-based approaches improve mobility and mood in older adults: A nonrandomized, controlled trïal. J. Bodyw. Mov. Ther. 2020, 24, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Kayama, H.; Okamoto, K.; Nishiguchi, S.; Yukutake, T.; Tanigawa, T.; Nagai, K.; Yamada, M.; Aoyama, T. Efficacy of an exercise game based on kinect in improving physical performances of fall risk factors in community-dwelling older adults. Games Health J. 2013, 2, 247–252. [Google Scholar] [CrossRef] [PubMed]
- van Diest, M.; Stegenga, J.; Wortche, H.J.; Postema, K.; Verkerke, G.J.; Lamoth, C.J. Suitability of kinect for measuring whole body movement patterns during exergaming. J. Biomech. 2014, 47, 2925–2932. [Google Scholar] [CrossRef]
- Decaestecker, T.N.; Coopman, E.M.; Van Peteghem, C.H.; Van Bocxlaer, J.F. Suitability testing of commercial solid-phase extraction sorbents for sample clean-up in systematic toxicological analysis using liquid chromatography-(tandem) mass spectrometry. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2003, 789, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Chow, D.H.; Mann, S.K. Effect of cyber-golfing on balance amongst the elderly in hong kong: A pilot randomised trial. Hong Kong J. Occup. Ther. 2015, 26, 9–13. [Google Scholar] [CrossRef] [Green Version]
- Milanovic, Z.; Pantelic, S.; Trajkovic, N.; Sporis, G.; Kostic, R.; James, N. Age-related decrease in physical activity and functional fitness among elderly men and women. Clin. Interv. Aging 2013, 8, 549–556. [Google Scholar] [CrossRef] [Green Version]
- Quail, G.G. An approach to the assessment of falls in the elderly. Aust. Fam. Physician 1994, 23, 873, 876–882. [Google Scholar]
- Chen, P.Y.; Wei, S.H.; Hsieh, W.L.; Cheen, J.R.; Chen, L.K.; Kao, C.L. Lower limb power rehabilitation (llpr) using interactive video game for improvement of balance function in older people. Arch. Gerontol. Geriatr. 2012, 55, 677–682. [Google Scholar] [CrossRef]
- Maillot, P.; Perrot, A.; Hartley, A. Effects of interactive physical-activity video-game training on physical and cognitive function in older adults. Psychol. Aging 2012, 27, 589–600. [Google Scholar] [CrossRef] [Green Version]
- Orsega-Smith, E.; Davis, J.; Slavish, K.; Gimbutas, L. Wii fit balance intervention in community-dwelling older adults. Games Health J. 2012, 1, 431–435. [Google Scholar] [CrossRef]
- Gomez, F.; Wu, Y.Y.; Auais, M.; Vafaei, A.; Zunzunegui, M.V. A simple algorithm to predict falls in primary care patients aged 65 to 74 years: The international mobility in aging study. J. Am. Med. Dir. Assoc. 2017, 18, 774–779. [Google Scholar] [CrossRef]
- Yuan, R.Y.; Chen, S.C.; Peng, C.W.; Lin, Y.N.; Chang, Y.T.; Lai, C.H. Effects of interactive video-game-based exercise on balance in older adults with mild-to-moderate parkinson’s disease. J. Neuroeng. Rehabil. 2020, 17, 91. [Google Scholar] [CrossRef] [PubMed]
- Aung, T.N.N.; Moolphate, S.; Koyanagi, Y.; Angkurawaranon, C.; Supakankunti, S.; Yuasa, M.; Aung, M.N. Depression and associated factors among community-dwelling thai older adults in northern thailand: The relationship between history of fall and geriatric depression. Int. J. Environ. Res. Public Health 2022, 19, 10574. [Google Scholar] [CrossRef]
- Rodrigues, E.V.; Gallo, L.H.; Guimaraes, A.T.B.; Melo Filho, J.; Luna, B.C.; Gomes, A.R.S. Effects of dance exergaming on depressive symptoms, fear of falling, and musculoskeletal function in fallers and nonfallers community-dwelling older women. Rejuvenation Res. 2018, 21, 518–526. [Google Scholar] [CrossRef]
- Drazich, B.F.; LaFave, S.; Crane, B.M.; Szanton, S.L.; Carlson, M.C.; Budhathoki, C.; Taylor, J.L. Exergames and depressive symptoms in older adults: A systematic review. Games Health J. 2020, 9, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Sato, D.; Kaneda, K.; Wakabayashi, H.; Nomura, T. Comparison of 2-year effects of once and twice weekly water exercise on activities of daily living ability of community dwelling frail elderly. Arch. Gerontol. Geriatr. 2009, 49, 123–128. [Google Scholar] [CrossRef]
- Cacciata, M.; Stromberg, A.; Lee, J.A.; Sorkin, D.; Lombardo, D.; Clancy, S.; Nyamathi, A.; Evangelista, L.S. Effect of exergaming on health-related quality of life in older adults: A systematic review. Int. J. Nurs. Stud. 2019, 93, 30–40. [Google Scholar] [CrossRef]
- Karahan, A.Y.; Tok, F.; Taskin, H.; Kucuksarac, S.; Basaran, A.; Yildirim, P. Effects of exergames on balance, functional mobility, and quality of life of geriatrics versus home exercise programme: Randomized controlled study. Cent. Eur. J. Public Health 2015, 23, S14–S18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, J.; Huang, H.C.; Cheng, T.C.E.; Wong, M.K.; Teng, C.I. Effects of playing exergames on quality of life among young adults: A 12-week randomized controlled trial. Int. J. Environ. Res. Public Health 2023, 20, 1359. [Google Scholar] [CrossRef] [PubMed]
| Experimental Group (n = 28) | Control Group (n = 29) | χ2/t | p | |
|---|---|---|---|---|
| Age (year) | 80.39 ± 2.57 | 79.10 ± 3.90 | 1.467 | 0.148 |
| Height (cm) | 164.36 ± 7.21 | 161.55 ± 9.97 | 1.213 | 0.230 |
| Weight (kg) | 61.40 ± 7.51 | 60.33 ± 8.86 | 0.493 | 0.624 |
| BMI (point) | 22.71 ± 2.26 | 23.04 ± 1.99 | 0.580 | 0.564 |
| MMSE | 25.93 ± 1.25 | 25.52 ± 1.02 | 1.365 | 0.178 |
| Gender (male/female) | 17/11 | 14/15 | 0.346 | 0.888 |
| Experimental Group (n = 28) | Control Group (n = 29) | t | p | CI for Difference | Effect Size | MDC | |||
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | MDC% | |||||||
| OLST (sec) | Pre | 28.09 ± 4.33 | 27.13 ± 6.54 | 0.652 | 0.517 | - | - | - | - |
| Post | 36.43 ± 5.50 | 27.75 ± 7.35 | - | - | - | - | - | - | |
| Pre–Post | 8.34 ± 1.91 | 0.61 ± 4.92 | 7.765 | 0.000 | 5.73 | 9.72 | 2.06 | 1.00 | |
| t | 23.149 | 0.672 | - | - | - | - | - | 11.97 | |
| p | 0.000 | 0.507 | - | - | - | - | - | - | |
| BBS (point) | Pre | 46.36 ± 4.29 | 44.62 ± 4.81 | 1.438 | 0.156 | - | - | - | - |
| Post | 48.18 ± 3.71 | 44.86 ± 4.70 | - | - | - | - | - | - | |
| Pre–Post | 1.82 ± 1.52 | 0.24 ± 0.79 | 4.963 | 0.000 | 0.94 | 2.22 | 1.31 | 0.79 | |
| t | 6.355 | 1.655 | - | - | - | - | - | 43.62 | |
| p | 0.000 | 0.109 | - | - | - | - | - | - | |
| FRT (cm) | Pre | 23.29 ± 4.48 | 24.66 ± 2.75 | 1.399 | 0.168 | - | - | - | - |
| Post | 26.57 ± 3.79 | 24.52 ± 2.76 | - | - | - | - | - | - | |
| Pre–Post | 3.28 ± 4.18 | −0.14 ± 3.60 | 3.317 | 0.002 | 1.36 | 5.49 | 0.88 | 2.19 | |
| t | 4.148 | 0.215 | - | - | - | - | - | 66.82 | |
| p | 0.000 | 0.831 | - | - | - | - | - | - | |
| TUGT (sec) | Pre | 12.35 ± 3.79 | 12.18 ± 4.06 | 0.158 | 0.875 | - | - | - | - |
| Post | 10.80 ± 3.87 | 11.97 ± 4.56 | - | - | - | - | - | - | |
| Pre–Post | −1.55 ± 1.17 | −0.21 ± 0.90 | 4.856 | 0.000 | −1.89 | −0.79 | −1.29 | 0.00 | |
| t | 7.014 | 1.267 | - | - | - | - | - | 0.00 | |
| p | 0.000 | 0.216 | - | - | - | - | - | - | |
| FTSTS (sec) | Pre | 15.87 ± 4.33 | 15.73 ± 4.36 | 0.117 | 0.908 | - | - | - | - |
| Post | 13.09 ± 3.83 | 15.94 ± 4.39 | - | - | - | - | - | - | |
| Pre–Post | −2.78 ± 1.76 | 0.20 ± 2.12 | 5.770 | 0.000 | −4.02 | −1.95 | −1.53 | 0.92 | |
| t | 8.365 | 0.519 | - | - | - | - | - | 33.14 | |
| p | 0.000 | 0.608 | - | - | - | - | - | - | |
| Experimental Group (n = 28) | Control Group (n = 29) | t | p | CI for Difference | Effect Size | MDC | |||
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | MDC% | |||||||
| MFES (point) | Pre | 6.63 ± 1.59 | 6.07 ±1.70 | 1.299 | 0.199 | - | - | - | - |
| Post | 7.05 ± 1.46 | 5.97 ± 1.50 | - | - | - | - | - | - | |
| Pre–Post | 0.42 ± 0.41 | −0.10 ± 0.88 | 2.840 | 0.006 | 0.15 | 0.89 | 0.75 | 0.21 | |
| t | 5.488 | 0.609 | - | - | - | - | - | 50.51 | |
| p | 0.000 | 0.548 | - | - | - | - | - | - | |
| GDS (point) | Pre | 13.21 ± 4.52 | 13.34 ± 4.75 | 0.106 | 0.916 | - | - | - | - |
| Post | 10.54 ± 3.84 | 13.55 ± 4.62 | - | - | - | - | - | - | |
| Pre–Post | −2.68 ± 1.93 | 0.21 ± 0.94 | 7.228 | 0.000 | −3.69 | −2.09 | −1.92 | 1.01 | |
| t | 7.361 | 1.186 | - | - | - | - | - | 37.66 | |
| p | 0.000 | 0.246 | - | - | - | - | - | - | |
| Experimental Group (n = 28) | Control Group (n = 29) | t | p | CI for Difference | Effect Size | MDC | |||
|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | MDC% | |||||||
| Physical Function (%) | Pre | 62.74 ± 14.91 | 61.38 ± 14.38 | 0.350 | 0.727 | - | - | - | - |
| Post | 65.89 ± 13.31 | 60.94 ± 15.25 | - | - | - | - | - | - | |
| Pre–Post | 3.15 ± 3.35 | −0.44 ± 1.94 | 4.975 | 0.000 | 0.02 | 0.05 | 1.32 | 0.02 | |
| t | 4.985 | 1.212 | - | - | - | - | - | 55.60 | |
| p | 0.000 | 0.236 | - | - | - | - | - | - | |
| Role limitations due to physical health (%) | Pre | 58.5% ± 20.27 | 61.62 ± 16.61 | 0.536 | 3.069 | - | - | - | - |
| Post | 61.32 ± 18.00 | 61.55 ± 17.33 | - | - | - | - | - | - | |
| Pre–Post | 2.75 ± 4.46 | −0.07 ± 2.10 | 3.069 | 0.003 | 0.01 | 0.05 | 0.81 | 0.02 | |
| t | 3.262 | 0.177 | - | - | - | - | - | 84.97 | |
| p | 0.003 | 0.861 | - | - | - | - | - | - | |
| Bodily Pain (%) | Pre | 61.20 ± 16.62 | 57.61 ± 16.22 | 0.824 | 0.413 | - | - | - | - |
| Post | 61.43 ± 16.37 | 56.81 ± 17.21 | - | - | - | - | - | - | |
| Pre–Post | 0.23 ± 3.57 | −0.80 ± 2.61 | 1.247 | 0.218 | −0.01 | 0.03 | 0.33 | 0.02 | |
| t | 0.341 | 1.653 | - | - | - | - | - | 811.99 | |
| p | 0.735 | 0.110 | - | - | - | - | - | - | |
| General Health (%) | Pre | 54.57 ± 12.71 | 56.83 ± 12.93 | 0.664 | 0.509 | - | - | - | - |
| Post | 56.34 ± 12.48 | 56.75 ± 12.78 | - | - | - | - | - | - | |
| Pre–Post | 1.77 ± 3.58 | −0.08 ± 1.02 | 2.668 | 0.010 | 0.00 | 0.03 | 0.71 | 0.02 | |
| t | 2.615 | 0.406 | - | - | - | - | - | 105.99 | |
| p | 0.014 | 0.688 | - | - | - | - | - | - | |
| Vitality (%) | Pre | 61.96 ± 12.27 | 60.86 ± 12.18 | 0.340 | 0.735 | - | - | - | - |
| Post | 62.79 ± 11.92 | 60.52 ± 12.44 | - | - | - | - | - | - | |
| Pre–Post | 0.82 ± 1.72 | −0.34 ± 0.94 | 3.191 | 0.002 | 0.00 | 0.02 | 0.85 | 0.00 | |
| t | 2.523 | 1.986 | - | - | - | - | - | 0.00 | |
| p | 0.018 | 0.057 | - | - | - | - | - | - | |
| Social Functioning (%) | Pre | 79.29 ± 17.83 | 76.90 ± 20.20 | 0.473 | 0.638 | - | - | - | - |
| Post | 79.68 ± 17.34 | 76.90 ± 20.10 | - | - | - | - | - | - | |
| Pre–Post | 0.39 ± 2.38 | 0.00 ± 0.60 | 0.862 | 0.392 | −0.01 | 0.01 | 0.23 | 0.01 | |
| t | 0.874 | 0.000 | - | - | - | - | - | 317.08 | |
| p | 0.390 | 1.000 | - | - | - | - | - | - | |
| Role limitations due to emotional problems (%) | Pre | 63.57 ± 22.84 | 62.07 ± 22.26 | 0.251 | 0.802 | - | - | - | - |
| Post | 64.18 ± 22.06 | 62.32 ± 21.89 | - | - | - | - | - | - | |
| Pre–Post | 0.61 ± 2.21 | 0.25 ± 1.46 | 0.718 | 0.476 | −0.01 | 0.01 | 0.19 | 0.01 | |
| t | 1.457 | 0.935 | - | - | - | - | - | 190.29 | |
| p | 0.157 | 0.358 | - | - | - | - | - | - | |
| Mental Health (%) | Pre | 65.14 ± 12.64 | 67.17 ± 12.16 | 0.618 | 0.539 | - | - | - | - |
| Post | 65.39 ± 12.69 | 67.52 ± 11.88 | - | - | - | - | - | - | |
| Pre–Post | 0.25 ± 0.70 | 0.34 ± 2.39 | 0.201 | 0.841 | −0.01 | 0.01 | −0.05 | 0.00 | |
| t | 1.888 | 0.776 | - | - | - | - | - | 0.00 | |
| p | 0.070 | 0.445 | - | - | - | - | - | - | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, K. Home-Based Exergame Program to Improve Physical Function, Fall Efficacy, Depression and Quality of Life in Community-Dwelling Older Adults: A Randomized Controlled Trial. Healthcare 2023, 11, 1109. https://doi.org/10.3390/healthcare11081109
Lee K. Home-Based Exergame Program to Improve Physical Function, Fall Efficacy, Depression and Quality of Life in Community-Dwelling Older Adults: A Randomized Controlled Trial. Healthcare. 2023; 11(8):1109. https://doi.org/10.3390/healthcare11081109
Chicago/Turabian StyleLee, Kyeongjin. 2023. "Home-Based Exergame Program to Improve Physical Function, Fall Efficacy, Depression and Quality of Life in Community-Dwelling Older Adults: A Randomized Controlled Trial" Healthcare 11, no. 8: 1109. https://doi.org/10.3390/healthcare11081109
APA StyleLee, K. (2023). Home-Based Exergame Program to Improve Physical Function, Fall Efficacy, Depression and Quality of Life in Community-Dwelling Older Adults: A Randomized Controlled Trial. Healthcare, 11(8), 1109. https://doi.org/10.3390/healthcare11081109





