Predicting Depression in Older Adults after the COVID-19 Pandemic Using ICF Model
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Model and Data Source
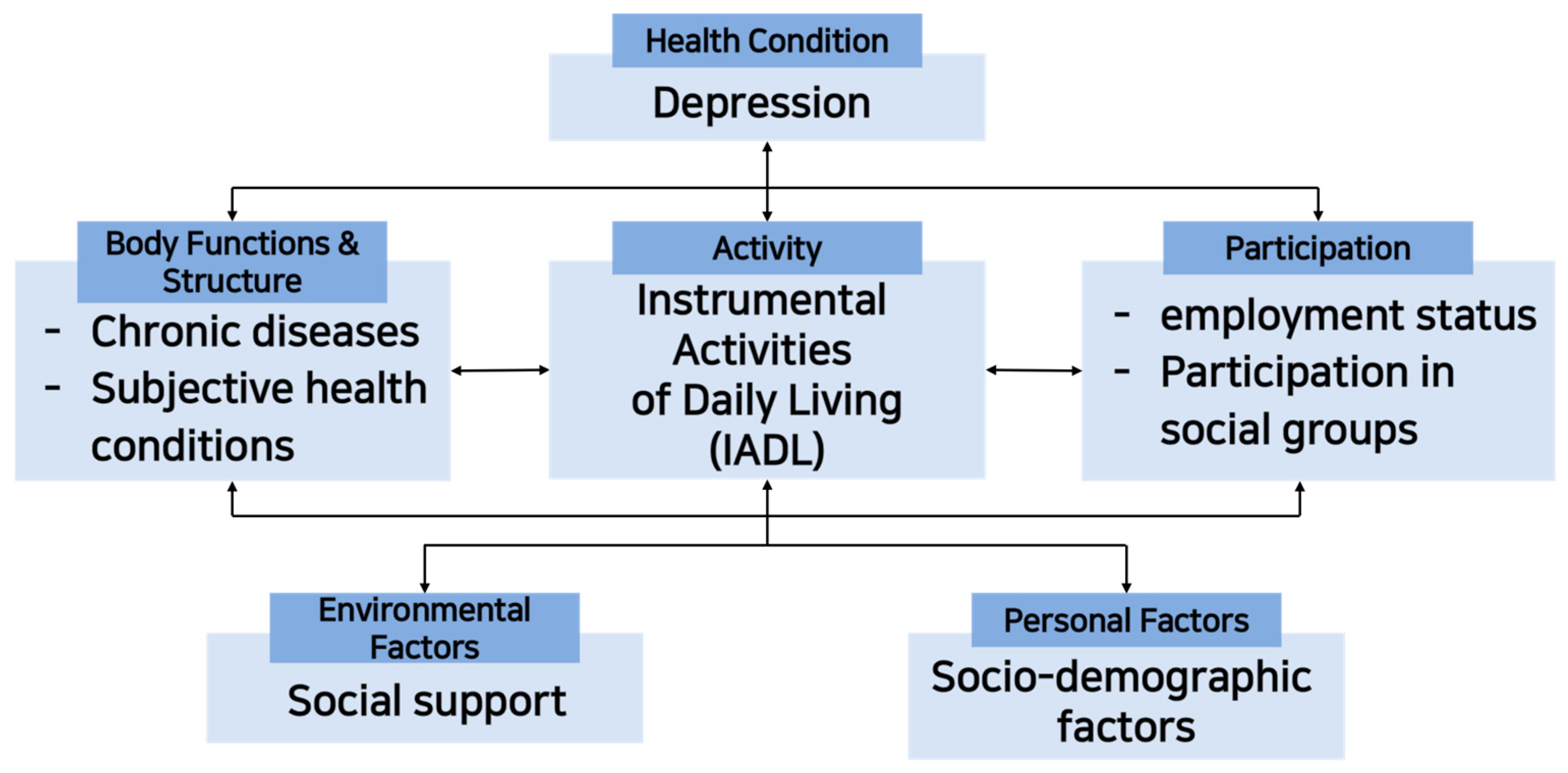
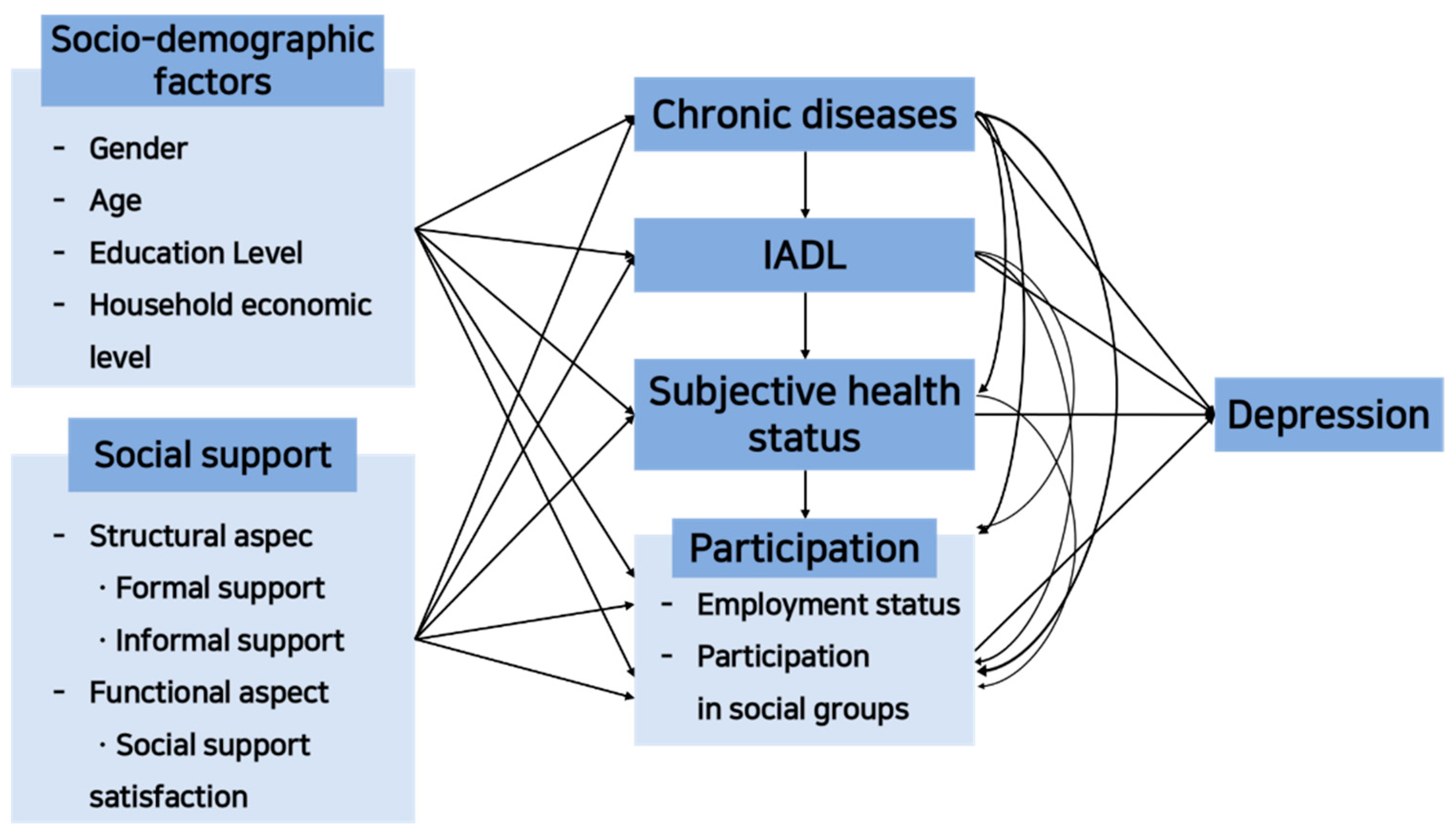
2.1.1. Model Framework
2.1.2. Data Source
2.2. Measurement and Definition of Variables
2.2.1. Depression
2.2.2. Personal Factors: Socio-Demographic Factors
2.2.3. Environmental Factors: Social Support
2.2.4. Body Functions and Structures: Chronic Diseases and Subjective Health Conditions
2.2.5. Activities: Instrumental Activities of Daily Living (IADL)
2.2.6. Social Participation: Employment Status and Participation in Social Groups
2.3. Analysis Methods
3. Results
3.1. General Characteristics
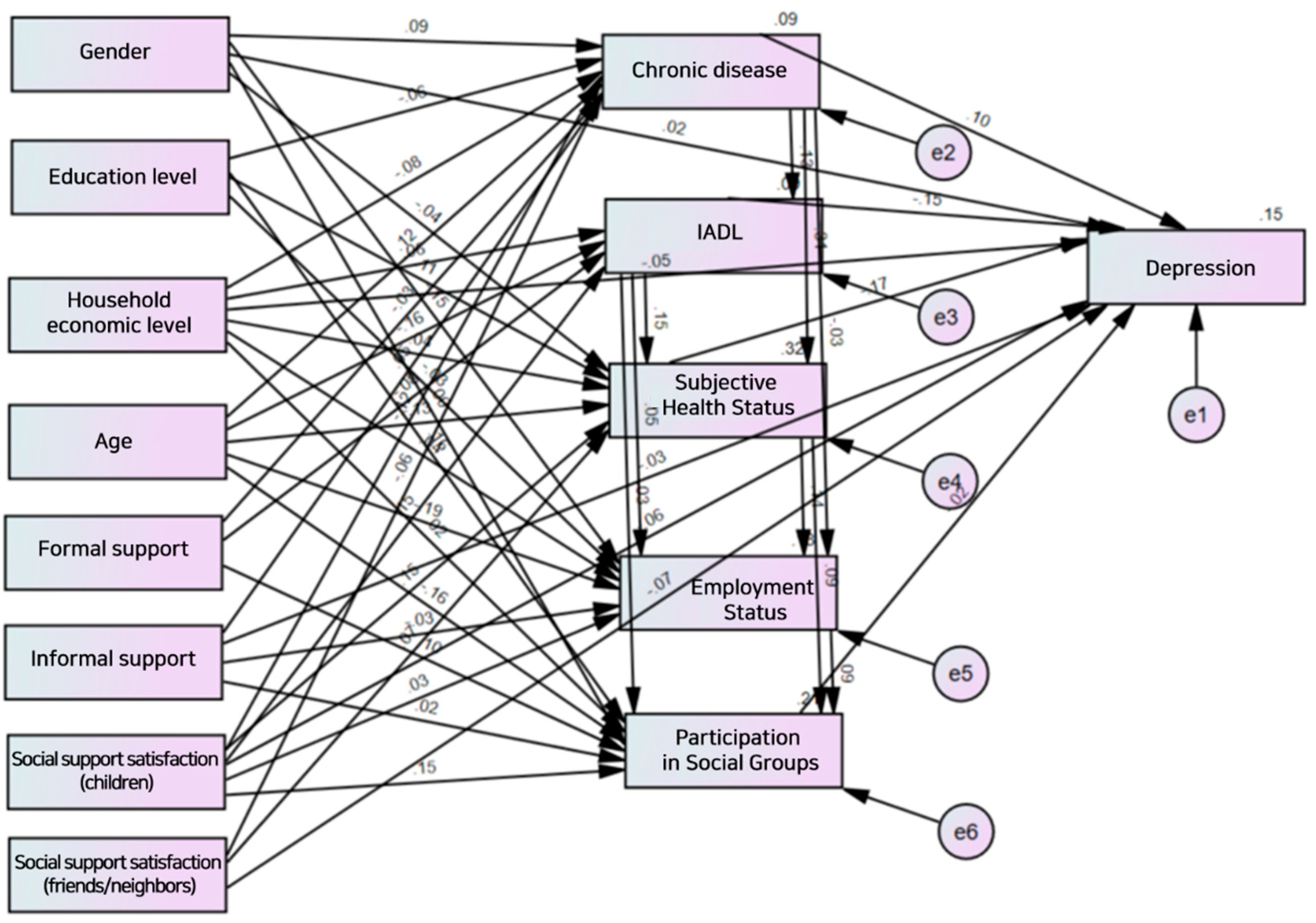
3.2. Predictive Model Verification
3.2.1. Verification of Predictive Model’s Goodness of Fit
3.2.2. Estimation of Predictive Model’s Path Coefficients
3.2.3. Effect Analysis of the Predictive Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Meier, J.V.; Noel, J.A.; Kaspar, K. Alone together: Computer-mediated communication in leisure time during and after the COVID-19 pandemic. Front. Psychol. 2021, 12, 666655. [Google Scholar] [CrossRef] [PubMed]
- Altena, E.; Baglioni, C.; Espie, C.A.; Ellis, J.; Gavriloff, D.; Holzinger, B.; Schlarb, A.; Frase, L.; Jernelöv, S.; Riemann, D.; et al. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: Practical recommendations from a task force of the European CBT-I Academy. J. Sleep Res. 2020, 29, e13052. [Google Scholar] [CrossRef] [PubMed]
- Rocha, D.D.M.; Abreu, I.M.D.; Mendes, P.M.; Leite, H.D.C.S.; Ferreira, M.D.C.S. Psychosocial effects of social distancing during coronavirus infections: Integrative review. Acta Paul. Enferm. 2021, 34, eAPE01141. [Google Scholar] [CrossRef]
- Hwang, T.J.; Rabheru, K.; Peisah, C.; Reichman, W.; Ikeda, M. Loneliness and social isolation during the COVID-19 pandemic. Int. Psychogeriatr. 2020, 32, 1217–1220. [Google Scholar] [CrossRef]
- Van Orden, K.A.; Bower, E.; Lutz, J.; Silva, C.; Gallegos, A.M.; Podgorski, C.A.; Santos, E.J.; Conwell, Y. Strategies to promote social connections among older adults during “social distancing” restrictions. Am. J. Geriatr. Psychiatry 2021, 29, 816–827. [Google Scholar] [CrossRef]
- “Corona Blue” Is “Corona Depression”. Available online: https://www.korean.go.kr/front/board/boardStandardView.do?board_id=6&mn_id=19&b_seq=773&pageIndex=5 (accessed on 15 February 2023).
- Namkung, E.H. Social and economic experiences and health changes for older persons during the COVID-19 pandemic. Health Welf. Policy Forum 2021, 300, 72–85. [Google Scholar] [CrossRef]
- Kasar, K.S.; Karaman, E. Life in lockdown: Social isolation, loneliness and quality of life in the elderly during the COVID-19 pandemic: A scoping review. Geriatr. Nurs. 2021, 42, 1222–1229. [Google Scholar] [CrossRef]
- Sepúlveda-Loyola, W.; Rodríguez-Sánchez, I.; Pérez-Rodríguez, P.; Ganz, F.; Torralba, R.; Oliveira, D.V.; Rodríguez-Mañas, L. Impact of social isolation due to COVID-19 on health in older people: Mental and physical effects and recommendations. J. Nutr. Health Aging 2020, 24, 938–947. [Google Scholar] [CrossRef]
- Chan, A.; Malhotra, C.; Malhotra, R.; Østbye, T. Living arrangements, social networks and depressive symptoms among older men and women in Singapore. Int. J. Geriatr. Psychiatry 2011, 26, 630–639. [Google Scholar] [CrossRef]
- Oh, D.J.; Yang, H.W.; Suh, S.W.; Byun, S.; Kim, T.H.; Kwak, K.P.; Kim, B.J.; Kim, S.G.; Kim, J.L.; Moon, S.W.; et al. The impact of the COVID-19 pandemic on depression in community-dwelling older adults: A prospective cohort study. Psychol. Med. 2021, 1–8. [Google Scholar] [CrossRef]
- Chung, S.D. A path analysis on depression among the elderly of institutional settings. J. Korean Gerontol. Soc. 2005, 25, 75–90. [Google Scholar]
- Akhtar-Danesh, N.; Landeen, J. Relation between depression and sociodemographic factors. Int. J. Ment. Health Syst. 2007, 1, 4. [Google Scholar] [CrossRef] [PubMed]
- Stegenga, B.T.; Nazareth, I.; Torres-González, F.; Xavier, M.; Švab, I.; Geerlings, M.I.; Bottomley, C.; Marston, L.; King, M. Depression, anxiety and physical function: Exploring the strength of causality. J. Epidemiol. Community Health 2012, 66, e25. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Functioning, Disability and Health: ICF; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Djernes, J.K. Prevalence and predictors of depression in populations of elderly: A review. Acta Psychiatr. Scand. 2006, 113, 372–387. [Google Scholar] [CrossRef] [PubMed]
- Vink, D.; Aartsen, M.J.; Schoevers, R.A. Risk factors for anxiety and depression in the elderly: A review. J. Affect. Disord. 2008, 106, 29–44. [Google Scholar] [CrossRef] [PubMed]
- Wu, Q.; Feng, J.; Pan, C.W. Risk factors for depression in the elderly: An umbrella review of published meta-analyses and systematic reviews. J. Affect. Disord. 2022, 307, 37–45. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. A Survey of the Elderly in 2020; Ministry of Health and Welfare, Korea Institute for Health and Social Affairs: Sejong, Republic of Korea, 2021.
- Kee, B.S. A preliminary study for the standardization of geriatric depression scale short form-Korea version. J. Korean Neuropsychiatr. Assoc. 1996, 35, 298–307. [Google Scholar]
- Lee, S.C.; Kim, W.H.; Chang, S.M.; Kim, B.S.; Lee, D.W.; Bae, J.N.; Cho, M.J. The use of the Korean version of Short Form Geriatric Depression Scale (SGDS-K) in the community dwelling elderly in Korea. J. Korean Geriatr. Psychiatry 2013, 17, 37–43. [Google Scholar]
- Won, C.W.; Rho, Y.G.; SunWoo, D.; Lee, Y.S. The validity and reliability of Korean Instrumental Activities of Daily Living (K-IADL) scale. J. Korean Geriatr. Soc. 2002, 6, 273–280. [Google Scholar]
- Park, Y.K.; Suh, S.R. A predictive model of instrumental activities of daily living in community-dwelling elderly based on ICF model. J. Korea Contents Assoc. 2018, 18, 113–123. [Google Scholar] [CrossRef]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Park, J.I.; Park, T.W.; Yang, J.C.; Chung, S.K. Factors associated with depression among elderly K oreans: The role of chronic illness, subjective health status, and cognitive impairment. Psychogeriatrics 2016, 16, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Niti, M.; Ng, T.P.; Kua, E.H.; Ho, R.C.M.; Tan, C.H. Depression and chronic medical illnesses in Asian older adults: The role of subjective health and functional status. Int. J. Geriatr. Psychiatry 2007, 22, 1087–1094. [Google Scholar] [CrossRef] [PubMed]
- Han, S.-H.; Kang, J.K.; Hong, J.-S. A Study of Factors Related to the Subjective Health Status of Elderly Population in Korea. Health Policy Manag. 2021, 31, 56–64. [Google Scholar] [CrossRef]
- Hwang, S.H.; Hwang, J.W. Subjective Health Status by degrees Conducting Activities of Daily Living. J. Converg. Inf. Technol. 2019, 9, 268–273. [Google Scholar] [CrossRef]
- Wang, D.X.; Yao, J.; Zirek, Y.; Reijnierse, E.M.; Maier, A.B. Muscle mass, strength, and physical performance predicting activities of daily living: A meta-analysis. J. Cachexia Sarcopenia Muscle 2020, 11, 3–25. [Google Scholar] [CrossRef]
- Girgus, J.S.; Yang, K.; Ferri, C.V. The gender difference in depression: Are elderly women at greater risk for depression than elderly men? Geriatrics 2017, 2, 35. [Google Scholar] [CrossRef]
- Demura, S.; Sato, S. Relationships between depression, lifestyle and quality of life in the community dwelling elderly: A comparison between gender and age groups. J. Physiol. Anthropol. Appl. Hum. Sci. 2003, 22, 159–166. [Google Scholar] [CrossRef]
- Heun, R.; Hein, S. Risk factors of major depression in the elderly. Eur. Psychiatry 2005, 20, 199–204. [Google Scholar] [CrossRef]
- Saikia, A.M.; Mahanta, N.; Saikia, A.M.; Deka, H.; Boruah, B.; Mehanta, R. Depression in elderly: A community–based study from Assam. Indian J. Basic Appl. Med. Res. 2016, 5, 42–48. [Google Scholar]
| Subgroups | Classification | Variables | N (%) | |
|---|---|---|---|---|
| No Depression | Personal Factors | Gender | Male | 3549 (41.1) |
| Female | 5078 (58.9) | |||
| Age | 65–74 years old | 5367 (62.2) | ||
| 75–84 years old | 2782 (32.2) | |||
| ≥85 years old | 478 (5.5) | |||
| Education Level | Elementary school graduation or below | 3665 (42.5) | ||
| Middle school graduation | 2028 (23.5) | |||
| High school graduation | 2468 (28.6) | |||
| College graduation or above | 466 (5.4) | |||
| Household economic level | National basic livelihood security recipient | 519 (6.0) | ||
| national basic livelihood security non-recipient | 8108 (94.0) | |||
| Environmental Factors | Formal support (used a senior citizen center or senior welfare service center in the community in the past year) | Used | 2557 (29.6) | |
| Never used | 6070 (70.4) | |||
| Informal support (frequency of meeting an acquaintance in the past year) | ≥2 times a year | 1381 (16.0) | ||
| 1–2 times every 3 months | 2464 (28.6) | |||
| 1–2 times a month | 3371 (39.1) | |||
| Once a week | 908 (10.5) | |||
| Everyday | 503 (5.8) | |||
| Social support satisfaction (relationship with children) | Dissatisfied | 236 (2.7) | ||
| Not satisfied or dissatisfied | 1729 (20.2) | |||
| Satisfied | 6662 (77.2) | |||
| Social support satisfaction (relationship with friends/neighbors) | Dissatisfied | 359 (4.2) | ||
| Not satisfied or dissatisfied | 2867 (33.2) | |||
| Satisfied | 5401 (62.6) | |||
| Physical Functions and Structures | Chronic disease | ≤1 | 4286 (49.7) | |
| 2–4 | 4082 (47.3) | |||
| ≥5 | 259 (3.0) | |||
| Subjective health status | Poor | 1216 (14.1) | ||
| Average | 2740 (31.8) | |||
| Good | 4671 (54.1) | |||
| Activities | Instrumental Activities of Daily Living (IADL) | ≤25 points | 190 (2.2) | |
| ≥26 points | 8437 (97.8) | |||
| Social Participation | Employment status | No | 5304 (61.5) | |
| Yes | 3323 (38.5) | |||
| Participation in social groups | No | 4806 (55.7) | ||
| Yes | 3821 (44.3) | |||
| Depression | Personal Factors | Gender | Male | 422 (32.6) |
| Female | 871 (67.4) | |||
| Age | 65–74 years old | 610 (47.2) | ||
| 75–84 years old | 551 (42.6) | |||
| ≥85 years old | 132 (10.2) | |||
| Education Level | Elementary school graduation or below | 766 (59.2) | ||
| Middle school graduation | 302 (23.4) | |||
| High school graduation | 186 (14.4) | |||
| College graduation or above | 39 (3.0) | |||
| Household economic level | National basic livelihood security recipient | 206 (15.9) | ||
| national basic livelihood security non-recipient | 1087 (84.1) | |||
| Environmental Factors | Formal support (used a senior citizen center or senior welfare service center in the community in the past year) | Used | 401 (31.0) | |
| Never used | 892 (69.0) | |||
| Informal support (frequency of meeting an acquaintance in the past year) | ≥2 times a year | 305 (23.6) | ||
| 1–2 times every 3 months | 334 (25.8) | |||
| 1–2 times a month | 458 (35.4) | |||
| Once a week | 126 (9.7) | |||
| Everyday | 70 (5.4) | |||
| Social support satisfaction (relationship with children) | Dissatisfied | 145 (11.2) | ||
| Not satisfied or dissatisfied | 387 (29.9) | |||
| Satisfied | 761 (58.9) | |||
| Social support satisfaction (relationship with friends/neighbors) | Dissatisfied | 253 (19.6) | ||
| Not satisfied or dissatisfied | 513 (39.7) | |||
| Satisfied | 527 (40.8) | |||
| Physical Functions and Structures | Chronic disease | ≤1 | 314 (24.3) | |
| 2–4 | 754 (58.3) | |||
| ≥5 | 225 (17.4) | |||
| Subjective health status | Poor | 644 (49.8) | ||
| Average | 380 (29.4) | |||
| Good | 269 (20.8) | |||
| Activities | Instrumental Activities of Daily Living (IADL) | ≤25 points | 214 (16.6) | |
| ≥26 points | 1079 (83.4) | |||
| Social Participation | Employment status | No | 1002 (77.5) | |
| Yes | 291 (22.5) | |||
| Participation in social groups | No | 973 (75.3) | ||
| Yes | 320 (24.7) | |||
| CMIN/DF | GFI | AGFI | SRMR | TLI | CFI | RMSEA |
|---|---|---|---|---|---|---|
| 1.653 | 1.000 | 0.998 | 0.0037 | 0.997 | 0.999 | 0.008 |
| Path | β | S.E. | C.R. | SMC | |
|---|---|---|---|---|---|
| Chronic Disease | ← Gender | 0.092 | 0.012 | 9.114 *** | 0.088 |
| ← Education level | −0.063 | 0.007 | −5.623 *** | ||
| ← Household economic level | −0.081 | 0.022 | −8.245 *** | ||
| ← Age | 0.118 | 0.010 | 11.034 *** | ||
| ← Informal support | 0.049 | 0.005 | 5.11 *** | ||
| ← Formal support | −0.029 | 0.013 | −2.799 ** | ||
| ← Social support satisfaction (friends/neighbors) | −0.117 | 0.010 | −11.078 *** | ||
| ← Social support satisfaction (children) | −0.061 | 0.011 | −5.814 *** | ||
| IADL | ← Household economic level | 0.061 | 0.007 | 6.228 *** | 0.095 |
| ← Age | −0.162 | 0.003 | −15.796 *** | ||
| ← Formal support | −0.079 | 0.004 | −7.902 *** | ||
| ← Social support satisfaction (friends/neighbors) | 0.148 | 0.003 | 14.992 *** | ||
| ← Chronic disease | −0.130 | 0.003 | −13.116 *** | ||
| Subjective Health Status | ← Gender | −0.039 | 0.014 | −4.465 *** | 0.323 |
| ← Education level | 0.112 | 0.008 | 11.741 *** | ||
| ← Household economic level | 0.040 | 0.025 | 4.696 *** | ||
| ← Age | −0.134 | 0.012 | −14.644 *** | ||
| ← Social support satisfaction (friends/neighbors) | 0.151 | 0.012 | 16.422 *** | ||
| ← Social support satisfaction (children) | 0.067 | 0.013 | 7.542 *** | ||
| ← Chronic disease | −0.313 | 0.011 | −35.892 *** | ||
| ← IADL | 0.153 | 0.034 | 17.707 *** | ||
| Employment Status | ← Gender | −0.152 | 0.010 | −15.319 *** | 0.128 |
| ← Education level | −0.025 | 0.006 | −2.296 * | ||
| ← Household economic level | 0.038 | 0.018 | 3.944 *** | ||
| ← Age | −0.189 | 0.008 | −17.927 *** | ||
| ← Informal support | −0.032 | 0.004 | −3.408 *** | ||
| ← Social support satisfaction (friends/neighbors) | 0.032 | 0.008 | 3.229 ** | ||
| ← Chronic disease | −0.030 | 0.009 | −2.816 ** | ||
| ← IADL | 0.046 | 0.024 | 4.613 *** | ||
| ← Subjective health status | 0.141 | 0.007 | 12.436 *** | ||
| Participation in Social Groups | ← Education level | 0.163 | 0.005 | 15.469 *** | 0.214 |
| ← Household economic level | 0.016 | 0.017 | 1.765 | ||
| ← Age | −0.162 | 0.008 | −15.648 *** | ||
| ← Formal support | 0.096 | 0.010 | 10.06 *** | ||
| ← Informal support | 0.022 | 0.004 | 2.456 * | ||
| ← Social support satisfaction (friends/neighbors) | 0.152 | 0.008 | 15.791 *** | ||
| ← Gender | 0.001 | 0.010 | 0.099 | ||
| ← IADL | 0.027 | 0.024 | 2.797 ** | ||
| ← Subjective health status | 0.091 | 0.007 | 8.878 *** | ||
| ← Employment status | 0.092 | 0.010 | 9.658 *** | ||
| Depression | ← Gender | 0.015 | 0.006 | 1.631 | 0.147 |
| ← Household economic level | −0.052 | 0.012 | −5.433 *** | ||
| ← Informal support | −0.031 | 0.003 | −3.298 *** | ||
| ← Social support satisfaction (friends/neighbors) | −0.065 | 0.006 | −6.156 *** | ||
| ← Social support satisfaction (children) | −0.075 | 0.006 | −7.427 *** | ||
| ← Chronic disease | 0.100 | 0.006 | 9.591 *** | ||
| ← IADL | −0.149 | 0.017 | −15.12 *** | ||
| ← Subjective health status | −0.166 | 0.005 | −14.893 *** | ||
| ← Participation in social groups | −0.021 | 0.007 | −2.138 * | ||
| Path | Total Effect | Direct Effect | Indirect Effect | |
|---|---|---|---|---|
| Chronic Disease | ← Social support satisfaction (children) | −0.061 *** | −0.061 *** | - |
| ← Social support satisfaction (friends/neighbors) | −0.117 *** | −0.117 *** | - | |
| ← Formal support | −0.029 *** | −0.029 ** | - | |
| ← Informal support | 0.049 *** | 0.049 *** | - | |
| ← Age | 0.118 *** | 0.118 *** | - | |
| ← Household economic level | −0.081 *** | −0.081 *** | - | |
| ← Education level | −0.063 *** | −0.063 *** | - | |
| ← Gender | 0.092 *** | 0.092 *** | - | |
| IADL | ← Social support satisfaction (children) | 0.008 ** | 0 | 0.008 *** |
| ← Social support satisfaction (friends/neighbors) | 0.164 *** | 0.148 *** | 0.015 *** | |
| ← Formal support | −0.076 *** | −0.079 *** | 0.004 ** | |
| ← Informal support | −0.006 *** | 0 | −0.006 *** | |
| ← Age | −0.177 *** | −0.162 *** | −0.015 *** | |
| ← Household economic level | 0.071 *** | 0.061 *** | 0.010 *** | |
| ← Education level | 0.008 | 0 | 0.008 *** | |
| ← Gender | −0.012 *** | 0 | −0.012 *** | |
| ← Chronic disease | −0.130 *** | −0.130 *** | - | |
| Subjective Health Status | ← Social support satisfaction (children) | 0.087 *** | 0.067 *** | 0.020 *** |
| ← Social support satisfaction (friends/neighbors) | 0.212 *** | 0.151 *** | 0.062 *** | |
| ← Formal support | −0.003 | 0 | −0.003 | |
| ← Informal support | −0.016 *** | 0 | −0.016 *** | |
| ← Age | −0.199 *** | −0.134 *** | −0.064 *** | |
| ← Household economic level | 0.076 *** | 0.040 *** | 0.036 *** | |
| ← Education level | 0.133 *** | 0.112 *** | 0.021 *** | |
| ← Gender | −0.070 *** | −0.039 *** | −0.031 *** | |
| ← Chronic disease | −0.332 *** | −0.313 *** | −0.020 *** | |
| ← IADL | 0.153 *** | 0.153 *** | - | |
| Employment Status | ← Social support satisfaction (children) | 0.015 *** | 0 | 0.015 *** |
| ← Social support satisfaction (friends/neighbors) | 0.073 *** | 0.032 *** | 0.041 *** | |
| ← Formal support | −0.003 ** | 0 | −0.003 * | |
| ← Informal support | −0.036 *** | −0.032 ** | −0.004 *** | |
| ← Age | −0.228 *** | −0.189 *** | −0.040 *** | |
| ← Household economic level | 0.054 *** | 0.038 *** | 0.016 *** | |
| ← Education level | −0.004 *** | −0.025 ** | 0.021 *** | |
| ← Gender | −0.165 *** | −0.152 *** | −0.013 *** | |
| ← Chronic disease | −0.083 *** | −0.030 ** | −0.053 *** | |
| ← IADL | 0.068 *** | 0.046 *** | 0.022 *** | |
| ← Subjective health status | 0.141 *** | 0.141 *** | - | |
| Participation in Social Groups | ← Social support satisfaction (children) | 0.009 *** | 0 | 0.009 *** |
| ← Social support satisfaction (friends/neighbors) | 0.182 *** | 0.152 *** | 0.030 *** | |
| ← Formal support | 0.094 *** | 0.096 *** | −0.003 ** | |
| ← Informal support | 0.017 * | 0.022 ** | −0.005 *** | |
| ← Age | −0.206 *** | −0.162 *** | −0.044 *** | |
| ← Household economic level | 0.030 *** | 0.016 | 0.014 *** | |
| ← Education level | 0.175 | 0.163 *** | 0.012 *** | |
| ← Gender | −0.021 * | 0.001 | −0.022 *** | |
| ← Chronic disease | −0.041 *** | 0 | −0.041 *** | |
| ← IADL | 0.047 *** | 0.027 *** | 0.020 *** | |
| ← Subjective health status | 0.104 *** | 0.091 *** | 0.013 *** | |
| ← Employment status | 0.092 *** | 0.092 *** | - | |
| Depression | ← Social support satisfaction (children) | −0.097 *** | −0.075 *** | −0.022 *** |
| ← Social support satisfaction (friends/neighbors) | −0.140 *** | −0.065 *** | −0.075 *** | |
| ← Formal support | 0.007 * | 0 | 0.007 * | |
| ← Informal support | −0.023 * | −0.031 *** | 0.008 *** | |
| ← Age | 0.075 *** | 0 | 0.075 *** | |
| ← Household economic level | −0.083 *** | −0.052 *** | −0.032 *** | |
| ← Education level | −0.033 *** | 0 | −0.033 *** | |
| ← Gender | 0.038 *** | 0.015 | 0.023 *** | |
| ← Chronic disease | 0.175 *** | 0.100 *** | 0.075 *** | |
| ← IADL | −0.175 *** | −0.149 *** | −0.026 *** | |
| ← Subjective health status | −0.168 *** | −0.166 *** | −0.002 * | |
| ← Employment status | −0.002 * | 0 | −0.002 * | |
| ← Participation in social groups | −0.021 * | −0.021 * | - | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Been, S.; Byeon, H. Predicting Depression in Older Adults after the COVID-19 Pandemic Using ICF Model. Healthcare 2023, 11, 1181. https://doi.org/10.3390/healthcare11081181
Been S, Byeon H. Predicting Depression in Older Adults after the COVID-19 Pandemic Using ICF Model. Healthcare. 2023; 11(8):1181. https://doi.org/10.3390/healthcare11081181
Chicago/Turabian StyleBeen, Seonjae, and Haewon Byeon. 2023. "Predicting Depression in Older Adults after the COVID-19 Pandemic Using ICF Model" Healthcare 11, no. 8: 1181. https://doi.org/10.3390/healthcare11081181
APA StyleBeen, S., & Byeon, H. (2023). Predicting Depression in Older Adults after the COVID-19 Pandemic Using ICF Model. Healthcare, 11(8), 1181. https://doi.org/10.3390/healthcare11081181







