Potentially Avoidable Hospitalizations by Asthma and COPD in Switzerland from 1998 to 2018: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Length
2.2. Variables, Data Sources, and Measurements
2.3. Potentially Avoidable Hospitalizations
2.4. Consequences of Potentially Avoidable Hospitalizations
2.5. Inclusion and Exclusion Criteria
2.6. Statistical Analysis
2.7. Ethics Statement
3. Results
3.1. Characteristics of Potentially Avoidable Hospitalizations
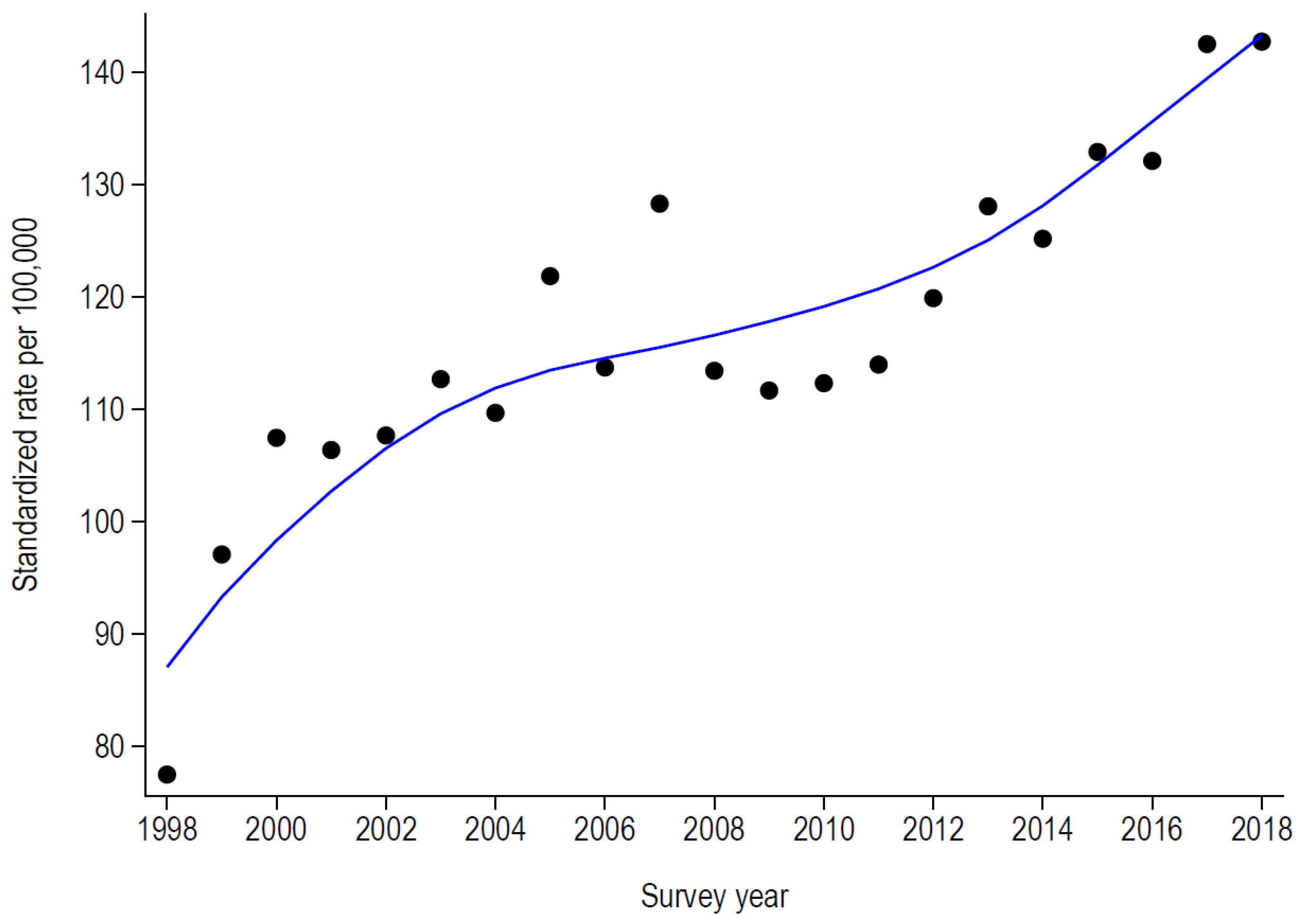
3.2. Trends of Potentially Avoidable Hospitalizations
3.3. Consequences of Potentially Avoidable Hospitalizations
4. Discussion
4.1. Characteristics of Potentially Avoidable Hospitalizations
4.2. Trends in Potentially Avoidable Hospitalizations
4.3. Implications of Potentially Avoidable Hospitalizations for Public Health
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Global Initiative for Asthma (GINA). Global Strategy for Asthma Management and Prevention. 2022. Available online: https://ginasthma.org/ (accessed on 18 January 2023).
- Tello, J.; Satylganova, A.; Barbazza, E. Assessing Health Services Delivery Performance with Hospitalizations for Ambulatory Care Sensitive Conditions; WHO: Rome, Italy, 2016. [Google Scholar]
- WHO. Chronic Obstructive Pulmonary Disease (COPD). 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd) (accessed on 25 December 2022).
- Celli, B.R.; Wedzicha, J.A. Update on Clinical Aspects of Chronic Obstructive Pulmonary Disease. N. Engl. J. Med. 2019, 381, 1257–1266. [Google Scholar] [CrossRef] [PubMed]
- Criner, R.N.; Han, M.K. COPD Care in the 21st Century: A Public Health Priority. Respir. Care 2018, 63, 591–600. [Google Scholar] [CrossRef] [PubMed]
- Singh, D.; Agusti, A.; Anzueto, A.; Barnes, P.J.; Bourbeau, J.; Celli, B.R.; Criner, G.J.; Frith, P.; Halpin, D.M.G.; Han, M.; et al. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease: The GOLD science committee report 2019. Eur. Respir. J. 2019, 53, 1900164. [Google Scholar] [CrossRef] [PubMed]
- De Pietro, C.; Camenzind, P.; Sturny, I.; Crivelli, L.; Edwards-Garavoglia, S.; Spranger, A.; Wittenbecher, F.; Quentin, W. Switzerland: Health System Review. Health Syst. Transit. 2015, 17, 1–288. [Google Scholar]
- Federal Office of Public Health. Key Figures for Swiss Hospitals. Available online: https://www.bag.admin.ch/bag/en/home/zahlen-und-statistiken/zahlen-fakten-zu-spitaelern/kennzahlen-der-schweizer-spitaeler.html (accessed on 11 April 2023).
- Cohidon, C.; Cornuz, J.; Senn, N. Primary care in Switzerland: Evolution of physicians’ profile and activities in twenty years (1993–2012). BMC Fam. Pr. 2015, 16, 107. [Google Scholar] [CrossRef]
- Rosano, A.; Loha, C.A.; Falvo, R.; Van Der Zee, J.; Ricciardi, W.; Guasticchi, G.; De Belvis, A.G. The relationship between avoidable hospitalization and accessibility to primary care: A systematic review. Eur. J. Public Health 2012, 23, 356–360. [Google Scholar] [CrossRef]
- Cartier, T.; Naiditch, M.; Lombrail, P. Avoidable Hospitalizations: The Sole Responsibility of Primary Care? Rev. Epidemiol. Sante Publ. 2014, 62, 225–236. [Google Scholar] [CrossRef]
- OECD. Stat. Health Care Quality Indicators. Available online: https://stats.oecd.org/Index.aspx?DataSetCode=HEALTH_HCQI (accessed on 8 January 2023).
- OECD. Health Care Quality and Outcomes Indicators. Available online: https://www.oecd.org/health/health-care-quality-outcomes-indicators.htm (accessed on 15 April 2023).
- OECD. Health Care Quality and Outcomes (HCQO) 2020–2021 Indicator Definitions. Available online: http://www.oecd.org/els/health-systems/Definitions-of-Health-Care-Quality-Outcomes.pdf (accessed on 8 January 2023).
- Eggli, Y.; Desquins, B.; Seker, E.; Halfon, P. Comparing potentially avoidable hospitalization rates related to ambulatory care sensitive conditions in Switzerland: The need to refine the definition of health conditions and to adjust for population health status. BMC Health Serv. Res. 2014, 14, 25. [Google Scholar] [CrossRef]
- Berlin, C.; Busato, A.; Rosemann, T.; Djalali, S.; Maessen, M. Avoidable hospitalizations in Switzerland: A small area analysis on regional variation, density of physicians, hospital supply and rurality. BMC Health Serv. Res. 2014, 14, 289. [Google Scholar] [CrossRef]
- Gygli, N.; Zúñiga, F.; Simon, M. Regional variation of potentially avoidable hospitalisations in Switzerland: An observational study. BMC Health Serv. Res. 2021, 21, 849. [Google Scholar] [CrossRef]
- WHO. International Statistical Classification of Diseases and Related Health Problems (ICD). Available online: https://www.who.int/standards/classifications/classification-of-diseases (accessed on 8 January 2023).
- OFS. Classification Suisse des Interventions Chirurgicales (CHOP). Available online: https://www.bfs.admin.ch/bfs/fr/home/statistiques/sante/nomenclatures/medkk/instruments-codage-medical.assetdetail.5808564.html (accessed on 8 January 2023).
- OECD. Length of Hospital Stay (Indication). Available online: https://data.oecd.org/healthcare/length-of-hospital-stay.htm (accessed on 15 April 2023).
- Halfon, P.; Eggli, Y.; van Melle, G.; Chevalier, J.; Wasserfallen, J.-B.; Burnand, B. Measuring potentially avoidable hospital readmissions. J. Clin. Epidemiol. 2002, 55, 573–587. [Google Scholar] [CrossRef] [PubMed]
- Deyo, R.A.; Cherkin, D.C.; Ciol, M.A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J. Clin. Epidemiol. 1992, 45, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Federal Act on Research Involving Human Beings (HRA) of 30 September 2011 (Status as of 1 December 2022), Article 2 Paragraph 2c). Available online: https://www.fedlex.admin.ch/eli/cc/2013/617/en (accessed on 8 January 2023).
- OECD. Health at a Glance 2021: OECD Indicators. Available online: https://www.oecd-ilibrary.org/sites/eeeae3eb-en/index.html?itemId=/content/component/eeeae3eb-en (accessed on 8 January 2023).
- Chowdhury, N.U.; Guntur, V.P.; Newcomb, D.C.; Wechsler, M.E. Sex and gender in asthma. Eur. Respir. Rev. 2021, 30, 210067. [Google Scholar] [CrossRef]
- Federal Statistical Office. Portraits of the Cantons. Available online: https://www.bfs.admin.ch/bfs/en/home/statistics/regional-statistics/regional-portraits-key-figures/cantons.html (accessed on 16 March 2023).
- Ntritsos, G.; Franek, J.; Belbasis, L.; Christou, M.A.; Markozannes, G.; Altman, P.; Fogel, R.; Sayre, T.; Ntzani, E.E.; Evangelou, E. Gender-specific estimates of COPD prevalence: A systematic review and meta-analysis. Int. J. Chronic Obstr. Pulm. Dis. 2018, 13, 1507–1514. [Google Scholar] [CrossRef] [PubMed]
- Spycher, J.; Morisod, K.; Eggli, Y.; Moschetti, K.; Le Pogam, M.-A.; Peytremann-Bridevaux, I.; Bodenmann, P.; Marti, J.; Indicators on Healthcare Equity in Switzerland. New Evidence and Challenges. Report Commissioned by the Federal Office of Public Health. Bern: FOPH. 2021. Available online: https://www.bag.admin.ch/dam/bag/de/dokumente/nat-gesundheitsstrategien/nat-programm-migration-und-gesundheit/chancengleich-heit-in-der-gesundheitsversorgung/report-indicators-on-healthcare-equity.pdf.download.pdf/Bericht%20Indicators%20on%20Healthcare%20Equity.pdf (accessed on 16 March 2023).
- Dantas, I.; Santana, R.; Sarmento, J.; Aguiar, P. The impact of multiple chronic diseases on hospitalizations for ambulatory care sensitive conditions. BMC Health Serv. Res. 2016, 16, 348. [Google Scholar] [CrossRef] [PubMed]
- O’Malley, A.S.; Pharm, H.H.; Schrag, D.; Wu, B.; Bach, P.B. Potentially avoidable hospitalizations for COPD and pneumonia: The role of physician and practice characteristics. Med. Care 2007, 45, 562–570. [Google Scholar] [CrossRef]
- van Loenen, T.; van den Berg, M.; Westert, G.P.; Faber, M.J. Organizational aspects of primary care related to avoidable hospitalization: A systematic review. Fam. Pract. 2014, 31, 502–516. [Google Scholar] [CrossRef]
- OFSP. Influenza—Résultats de Laboratoire à Déclaration Obligatoire. Available online: https://www.bag.admin.ch/bag/fr/home/zahlen-und-statistiken/zahlen-zu-infektionskrankheiten/meldepflichtige-infektionskrankheiten—Woechentliche-fallzahlen.html (accessed on 7 March 2023).
- Paul, M.C.; Dik, J.-W.H.; Hoekstra, T.; Van Dijk, C.E. Admissions for ambulatory care sensitive conditions: A national observational study in the general and COPD population. Eur. J. Public Health 2019, 29, 213–219. [Google Scholar] [CrossRef]
- Sharma, N.; Schwendimann, R.; Endrich, O.; Ausserhofer, D.; Simon, M. Variation of Daily Care Demand in Swiss General Hospitals: Longitudinal Study on Capacity Utilization, Patient Turnover and Clinical Complexity Levels. J. Med. Internet Res. 2021, 23, e27163. [Google Scholar] [CrossRef]
- Swiss Health Observatory (Obsan). Available online: https://ind.obsan.admin.ch/en/indicator/monam/expenditure-on-prevention-and-health-promotion-by-service (accessed on 16 March 2023).
- Gusmano, M.K.; Rodwin, V.G.; Weisz, D. A new way to compare health systems: Avoidable hospital conditions in manhattan And Paris. Health Aff. 2006, 25, 510–520. [Google Scholar] [CrossRef] [PubMed]
- Eggli, Y.; Halfon, P.; Piaget-Rossel, R.; Bischoff, T. Measuring medically unjustified hospitalizations in Switzerland. BMC Health Serv. Res. 2022, 22, 158. [Google Scholar] [CrossRef] [PubMed]



| Characteristics | Asthma | COPD |
|---|---|---|
| N | 25,260 | 135,069 |
| Women (%) | 16,694 (66.1) | 57,341 (42.5) |
| Age groups (%) | ||
| [20, 30] | 2720 (10.8) | 454 (0.3) |
| [30, 40] | 3146 (12.5) | 1115 (0.8) |
| [40, 50] | 3894 (15.4) | 4254 (3.2) |
| [50, 60] | 3912 (15.5) | 15,527 (11.5) |
| [60, 70] | 3671 (14.5) | 33,956 (25.1) |
| [70, 80] | 4247 (16.8) | 47,337 (35.1) |
| [80, 90] | 3140 (12.4) | 29,011 (21.5) |
| [90, ∞] | 530 (2.1) | 3415 (2.5) |
| Swiss nationality (%) | 19,076 (75.5) | 116,881 (86.5) |
| Region (%) | ||
| Leman | 6015 (23.8) | 24,824 (18.4) |
| Mittelland | 4915 (19.5) | 26,185 (19.4) |
| Northwest | 4440 (17.6) | 25,285 (18.7) |
| Zurich | 3435 (13.6) | 22,192 (16.4) |
| Eastern | 3110 (12.3) | 17,170 (12.7) |
| Central | 1702 (6.7) | 9795 (7.3) |
| Ticino | 1643 (6.5) | 9618 (7.1) |
| Compulsory insurance (%) | 24,148 (95.6) | 132,284 (97.9) |
| Emergency admission (%) | 19,775 (78.3) | 99,586 (73.7) |
| Patient’s decision to access healthcare (%) | 9537 (37.8) | 31,682 (23.5) |
| Charlson’s index categories (%) | ||
| 0–1 | 18,487 (73.2) | 5750 (4.3) |
| 2–3 | 5729 (22.7) | 95,240 (70.5) |
| ≥4 | 1044 (4.1) | 34,079 (25.2) |
| Asthma | COPD | |||
|---|---|---|---|---|
| Year | Number | Rate | Number | Rate |
| 1998 | 864 | 17.17 | 3501 | 77.4 |
| 1999 | 1144 | 22.26 | 4453 | 97.0 |
| 2000 | 1285 | 24.95 | 4986 | 107.4 |
| 2001 | 1282 | 24.21 | 5048 | 106.3 |
| 2002 | 1206 | 22.84 | 5185 | 107.6 |
| 2003 | 1183 | 21.63 | 5514 | 112.6 |
| 2004 | 1309 | 23.65 | 5469 | 109.6 |
| 2005 | 1186 | 21.34 | 6188 | 121.8 |
| 2006 | 1037 | 18.32 | 5880 | 113.7 |
| 2007 | 1206 | 20.84 | 6758 | 128.3 |
| 2008 | 1148 | 19.61 | 6114 | 113.4 |
| 2009 | 1216 | 20.58 | 6135 | 111.6 |
| 2010 | 1126 | 18.76 | 6284 | 112.3 |
| 2011 | 1145 | 18.59 | 6483 | 113.9 |
| 2012 | 1141 | 18.23 | 6963 | 119.9 |
| 2013 | 1291 | 20.53 | 7599 | 128.0 |
| 2014 | 1244 | 19.42 | 7579 | 125.1 |
| 2015 | 1240 | 19.03 | 8197 | 132.9 |
| 2016 | 1340 | 20.24 | 8306 | 132.1 |
| 2017 | 1292 | 19.36 | 9114 | 142.5 |
| 2018 | 1375 | 20.36 | 9313 | 142.7 |
| Asthma | COPD | |||
|---|---|---|---|---|
| Year | Days | Occupied Beds | Days | Occupied Beds |
| 1998 | 10,590 | 29 | 52,529 | 144 |
| 1999 | 13,064 | 36 | 67,929 | 186 |
| 2000 | 14,173 | 39 | 71,776 | 197 |
| 2001 | 12,783 | 35 | 73,314 | 201 |
| 2002 | 11,637 | 32 | 72,122 | 198 |
| 2003 | 10,710 | 29 | 72,815 | 199 |
| 2004 | 11,679 | 32 | 70,976 | 194 |
| 2005 | 9843 | 27 | 74,855 | 205 |
| 2006 | 7576 | 21 | 71,035 | 195 |
| 2007 | 8385 | 23 | 79,741 | 218 |
| 2008 | 8182 | 22 | 69,223 | 190 |
| 2009 | 9387 | 26 | 68,297 | 187 |
| 2010 | 8343 | 23 | 68,116 | 187 |
| 2011 | 8154 | 22 | 69,871 | 191 |
| 2012 | 7749 | 21 | 73,942 | 203 |
| 2013 | 9156 | 25 | 78,940 | 216 |
| 2014 | 8717 | 24 | 79,872 | 219 |
| 2015 | 7689 | 21 | 74,155 | 203 |
| 2016 | 8271 | 23 | 75,425 | 207 |
| 2017 | 7710 | 21 | 83,794 | 230 |
| 2018 | 8200 | 22 | 84,863 | 233 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gouveia, A.; Mauron, C.; Marques-Vidal, P. Potentially Avoidable Hospitalizations by Asthma and COPD in Switzerland from 1998 to 2018: A Cross-Sectional Study. Healthcare 2023, 11, 1229. https://doi.org/10.3390/healthcare11091229
Gouveia A, Mauron C, Marques-Vidal P. Potentially Avoidable Hospitalizations by Asthma and COPD in Switzerland from 1998 to 2018: A Cross-Sectional Study. Healthcare. 2023; 11(9):1229. https://doi.org/10.3390/healthcare11091229
Chicago/Turabian StyleGouveia, Alexandre, Charlène Mauron, and Pedro Marques-Vidal. 2023. "Potentially Avoidable Hospitalizations by Asthma and COPD in Switzerland from 1998 to 2018: A Cross-Sectional Study" Healthcare 11, no. 9: 1229. https://doi.org/10.3390/healthcare11091229







