Psychosocial Factors Associated with Self-Management in Patients with Diabetes
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measuring Instruments
2.3. Procedures
2.4. Ethical Considerations
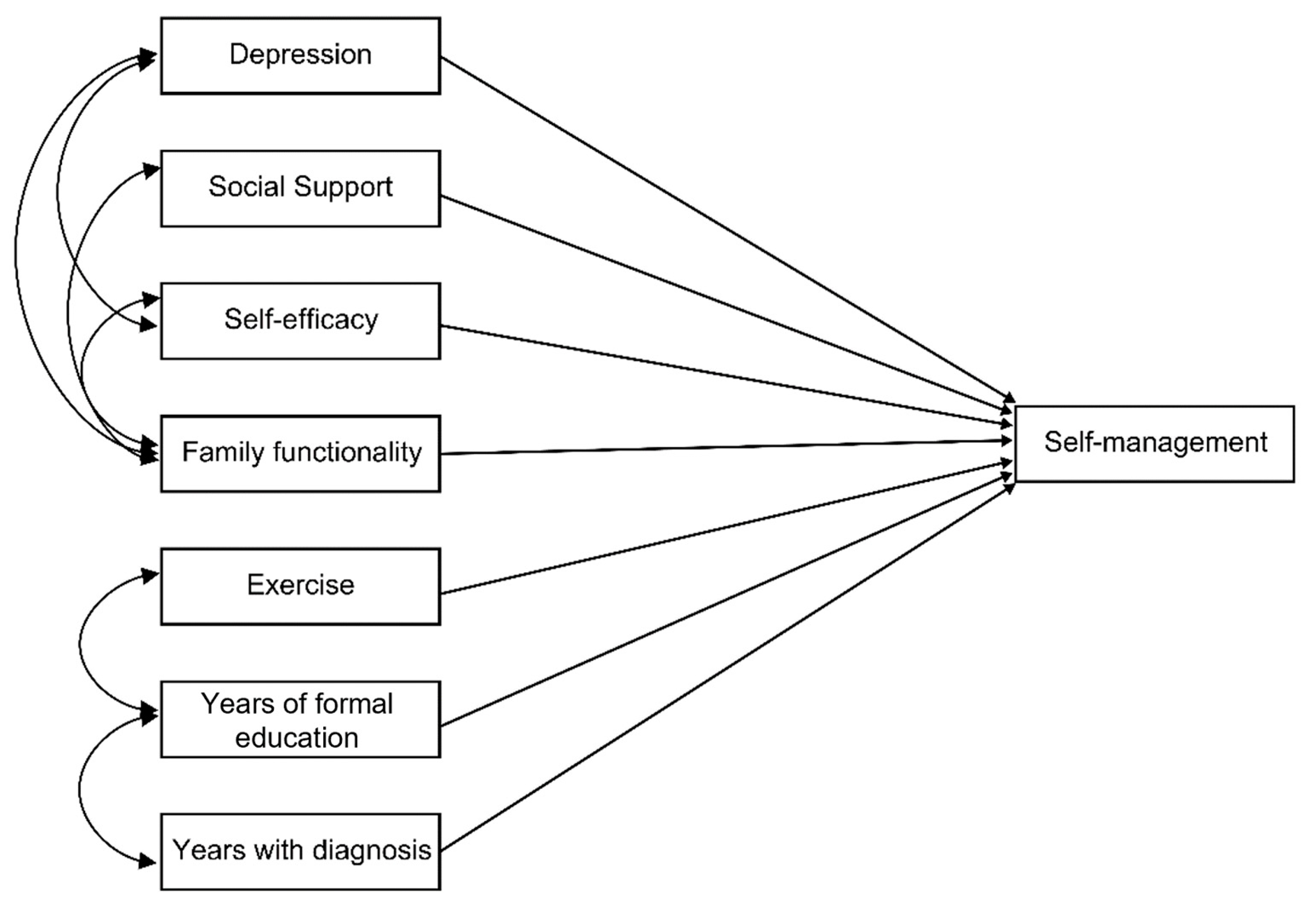
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- International Diabetes Federation. IDF Diabetes Atlas 10th Edición; International Diabetes Federation: Brussels, Belgium, 2021. [Google Scholar]
- Shamah-Levy, T.; Vielma-Orozco, E.; Heredia-Hernández, O.; Romero-Martínez, M.; Mojica-Cuevas, J.; Cuevas-Nasu, L.; Santaella-Castell, J.; Rivera-Dommarco, J. Encuesta Nacional de Salud y Nutrición 2018–19: Resultados Nacionales; Instituto Nacional de Salud Pública: Cuernavaca, México, 2020. [Google Scholar]
- Pan American Health Organization; World Health Organization. Innovative Care for Chronic Condition, Organizing and De-Livering High Quality Care for Chronic Noncommunicable Diseases in the America; PAHO Innovative Care: Washington, DC, USA, 2013. [Google Scholar]
- Baptista, D.R.; Wiens, A.; Pontarolo, R.; Regis, L.; Reis, W.C.T.; Correr, C.J. The chronic care model for type 2 diabetes: A systematic review. Diabetol. Metab. Syndr. 2016, 8, 7. [Google Scholar] [CrossRef] [PubMed]
- Pan American Health Organization. Plan of Action for the Prevention and Control of Noncommunicable Diseases in the Americas 2013–2019; PAHO: Washington, DC, USA, 2015. [Google Scholar]
- Ryan, P.; Sawin, K.J. The individual and family self-management theory: Background and perspectives on context, process, and outcomes. Nurs. Outlook 2009, 57, 217–225.e6. [Google Scholar] [CrossRef] [PubMed]
- Gunggu, A.; Thon, C.C.; Whye, L.C. Predictors of diabetes self-management among type 2 diabetes patients. J. Diabetes Res. 2016, 2016, 9158943. [Google Scholar] [CrossRef] [PubMed]
- Rahimian, B.E.; Besharat, M.A.; Mohajeri, T.M.; Talepasand, S. Predictive role of self-efficacy, belief of treatment effectiveness and social support in diabetes mellitus self-management. Iran. J. Psychiatry Clin. Psychol. 2011, 17, 232–240. [Google Scholar]
- Zhang, X.; Wu, S.; Wang, F.; Mayinuer, Y.; Sun, K.; Hu, K.; Zhang, X.; Sun, X.; Fisher, E.B. Association between social support and self-management behaviors among patients with diabetes in community. J. Peking Univ. 2017, 49, 455–461. [Google Scholar]
- Yang, S.; Kong, W.; Hsue, C.; Fish, A.F.; Chen, Y.; Guo, X.; Lou, Q.; Anderson, R. Knowledge of A1c predicts diabetes self-management and A1c level among chinese patients with type 2 diabetes. PLoS ONE 2016, 11, e0150753. [Google Scholar] [CrossRef] [PubMed]
- Maneze, D.; Everett, B.; Astorga, C.; Yogendran, D.; Salamonson, Y. The influence of health literacy and depression on diabetes self-management: A cross-sectional study. J. Diabetes Res. 2016, 2016, 3458969. [Google Scholar] [CrossRef]
- Lalnuntluangi, R.; Chelli, K.; Padhy, M. Self-efficacy, outcome expectancy and self-management of type 2 diabetes patients. Indian J. Health Wellbeing 2017, 8, 1040–1043. [Google Scholar]
- Page-Reeves, J.; Regino, L.; Murray-Krezan, C.; Bleecker, M.; Erhardt, E.; Burge, M.; Bearer, E.; Mishra, S. A comparative effectiveness study of two culturally competent models of diabetes self-management programming for Latinos from low-income households. BMC Endocr. Disord. 2017, 17, 46. [Google Scholar] [CrossRef]
- Kueh, Y.C.; Morris, T.; Borkoles, E.; Shee, H. Modelling of diabetes knowledge, attitudes, self-management, and quality of life: A cross-sectional study with an Australian sample. Health Qual. Life Outcomes 2015, 13, 129. [Google Scholar] [CrossRef]
- Lee, E.H.; Lee, Y.W.; Moon, S.H. A structural equation model linking health literacy to self-efficacy, self-care activities, and health-related quality of life in patients with type 2 diabetes. Asian Nurs. Res. 2016, 10, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.Y.; Lee, S.J.; Kim, S.H.; Jung, K.M. A predictive model of health outcomes for young people with type 2 diabetes. Asian Nurs. Res. 2015, 9, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, A.; Reimer, A.; Hermanns, N.; Huber, J.; Ehrmann, D.; Schall, S.; Kulzer, B. Assessing diabetes self-management with the diabetes self-management questionnaire (DSMQ) can help analyse behavioural problems related to reduced glycaemic control. PLoS ONE 2016, 11, e0150774. [Google Scholar] [CrossRef] [PubMed]
- Banda-González, O.L.; Rangel, M.S.; Hiyo, E.P. Modelos predictivos del comportamiento de automanejo de enfermedades crónicas en México y Perú. In El Automanejo en Personas con Enfermedades Crónicas: El Caso de México y Perú; Peñarrieta, M., León, R., Eds.; Colofón: Mexico, México, 2019; pp. 49–72. [Google Scholar]
- León-Hernández, R.; Peñarrieta-de Córdova, M.; Gutiérrez-Gómez, T.; Banda-González, O.; Flores-Barrios, F.; Rivera, M. Predictores del comportamiento de automanejo en personas con enfermedades crónicas de Tamaulipas. Enferm. Univ. 2019, 16, 945–957. [Google Scholar] [CrossRef]
- Lorig, K.R.; Sobel, D.S.; Stewart, A.L.; Brown, B.W., Jr.; Bandura, A.; Ritter, P.; Gonzalez, V.M.; Laurent, D.D.; Holman, H.R. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: A randomized trial. Med. Care 1999, 37, 5–14. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol. Rev. 1977, 84, 191–215. [Google Scholar] [CrossRef]
- Toledano-Toledano, F.; Rodríguez-Rey, R.; Moral de la Rubia, J.; Luna, D. A Sociodemographic variables questionnaire (Q-SV) for research on family caregivers of children with chronic disease. BMC Psychol. 2019, 7, 85. [Google Scholar] [CrossRef]
- Battersby, M.W.; Ask, A.; Reece, M.M.; Markwick, M.J.; Collins, J.P. The partners in health scale: The development and psychometric properties of a generic assessment scale for chronic condition self-management. Aust. J. Prim. Health 2003, 9, 41–52. [Google Scholar] [CrossRef]
- Peñarrieta-de Córdova, I.; Barrios, F.F.; Gutierrez-Gomes, T.; Piñonez-Martinez, M.S.; Quintero-Valle, L.M.; Castañeda-Hidalgo, H. Self-management in chronic conditions: Partners in health scale instrument validation. Nurs. Manag. 2014, 20, 32–37. [Google Scholar] [CrossRef]
- León, H.; Peñarrieta, C.; Gutiérrez, G.; Gutiérrez, T. Validación de instrumentos de indicadores de salud y psicosociales. Red de automanejo de enfermedades crónicas. In Estrategias de Aprendizaje en Cronicidad; Gutiérrez, T., Ed.; Colofón: Mexico, México, 2019; pp. 65–84. [Google Scholar]
- Broadhead, W.E.; Gehlbach, S.H.; de Gruy, F.V.; Kaplan, B.H. The Duke-UNC functional social support questionnaire. measurement of social support in family medicine patients. Med. Care 1988, 26, 709–723. [Google Scholar] [CrossRef]
- Piña, J.; Icedo, B. Validación del cuestionario de apoyo social funcional en personas seropositivas al vih del noroeste de Mexico. Cienc. Enferm. 2007, 13, 53–63. [Google Scholar] [CrossRef]
- Smilkstein, G. The family APGAR: A proposal for a family function test and its use by physicians. J. Fam. Pract. 1978, 6, 1231–1239. [Google Scholar] [PubMed]
- Cuba, M.A.S.; Espinoza, M.A. APGAR familiar: Una herramienta para detectar disfunción familiar. Revista Médica la Paz 2014, 20, 53–57. [Google Scholar]
- Lorig, K.; Stewart, A.; Ritter, P.; Gonzalez, V.; Lynch, J.; Laurent, D. Outcome Measures for Health Education and Other Health Care Interventions; Sage: Thousand Oaks, CA, USA, 1996. [Google Scholar]
- Ory, M.G.; Ahn, S.; Jiang, L.; Smith, M.L.; Ritter, P.L.; Whitelaw, N.; Lorig, K. Successes of a national study of the chronic disease self-management program: Meeting the triple aim of health care reform. Med. Care 2013, 51, 992–998. [Google Scholar] [CrossRef] [PubMed]
- Sociedad Mexicana de Psicología. Código Ético Del Psicólogo; Trillas: Mexico, México, 2010. [Google Scholar]
- World Medical Association. World medical association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Ruiz, M.A.; Pardo, A.; San Martín, R. Modelos de ecuaciones estructurales. Papeles del Psicólogo 2010, 31, 34–45. [Google Scholar]
- Portillo, M.T.E.; Gómez, J.A.H.; Ortega, V.E.; Moreno, G.M. Modelos de ecuaciones estructurales: Características, fases, construcción, aplicación y resultados. Cienc. Trab. 2016, 18, 16–22. [Google Scholar] [CrossRef]
- Vesely, S.; Klöckner, C.A. Social desirability in environmental psychology research: Three meta-analyses. Front. Psychol. 2020, 11, 1395. [Google Scholar] [CrossRef]

| n = 183 | N | % | M | SD |
|---|---|---|---|---|
| Sex | ||||
| Male | 10 | 5.5 | ||
| Female | 173 | 94.5 | ||
| Marital status | ||||
| Married | 147 | 80.3 | ||
| Widower | 14 | 7.7 | ||
| Divorced | 12 | 6.6 | ||
| Single | 10 | 5.5 | ||
| Age | 55.4 | 11.5 |
| n = 183 | n | % | M | SD |
|---|---|---|---|---|
| Levels of self-management | ||||
| Low self-management | 81 | 44.3 | ||
| Medium self-management | 67 | 36.6 | ||
| High self-management | 35 | 19.1 | ||
| Levels of depression | ||||
| No symptoms | 107 | 58.5 | ||
| Mild symptoms | 52 | 28.4 | ||
| Moderate symptoms | 18 | 9.8 | ||
| Severe symptoms | 3 | 1.6 | ||
| Serious symptoms | 3 | 1.6 | ||
| Levels of family functionality | ||||
| Functional | 118 | 64.5 | ||
| Mild dysfunction | 29 | 15.8 | ||
| Moderate dysfunction | 16 | 8.7 | ||
| Severe dysfunction | 20 | 10.9 | ||
| Social support | ||||
| With social support | 42 | 23.0 | ||
| No social support | 141 | 77.0 | ||
| Self-efficacy | 7.09 | 2.19 | ||
| Exercise, in min. | 66.97 | 85.55 | ||
| Years of formal education | 6.45 | 3.61 | ||
| Years with a diagnosis | 10.35 | 7.98 | ||
| Total | 183 | 100.0 |
| Model | Absolute Fit or Goodness of Fit | Comparative Fit | Parsimonious Fit | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| χ2 | gl | χ2/gl | RMSEA | RMSR | GFI | CFI | NFI | PNFI | PGFI | |
| 1 | 16.364 | 15 | 1.09 | 0.022 | 28.359 | 0.977 | 0.992 | 0.917 | 0.491 | 0.407 |
| 2 | 8.054 | 9 | 0.89 | 0.000 | 4.251 | 0.987 | 1.00 | 0.954 | 0.409 | 0.317 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
León-Hernández, R.; Rodríguez-Pérez, A.C.; Pérez-González, Y.M.; de Córdova, M.I.P.; de León-Escobedo, R.; Gómez-Gutiérrez, T.; Toledano-Toledano, F. Psychosocial Factors Associated with Self-Management in Patients with Diabetes. Healthcare 2023, 11, 1284. https://doi.org/10.3390/healthcare11091284
León-Hernández R, Rodríguez-Pérez AC, Pérez-González YM, de Córdova MIP, de León-Escobedo R, Gómez-Gutiérrez T, Toledano-Toledano F. Psychosocial Factors Associated with Self-Management in Patients with Diabetes. Healthcare. 2023; 11(9):1284. https://doi.org/10.3390/healthcare11091284
Chicago/Turabian StyleLeón-Hernández, Rodrigo, Andrea C. Rodríguez-Pérez, Yessica M. Pérez-González, María I. P. de Córdova, Raúl de León-Escobedo, Tranquilina Gómez-Gutiérrez, and Filiberto Toledano-Toledano. 2023. "Psychosocial Factors Associated with Self-Management in Patients with Diabetes" Healthcare 11, no. 9: 1284. https://doi.org/10.3390/healthcare11091284
APA StyleLeón-Hernández, R., Rodríguez-Pérez, A. C., Pérez-González, Y. M., de Córdova, M. I. P., de León-Escobedo, R., Gómez-Gutiérrez, T., & Toledano-Toledano, F. (2023). Psychosocial Factors Associated with Self-Management in Patients with Diabetes. Healthcare, 11(9), 1284. https://doi.org/10.3390/healthcare11091284






