Effect of Devised Simultaneous Physical Function Improvement Training and Posture Learning Exercises on Posture
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
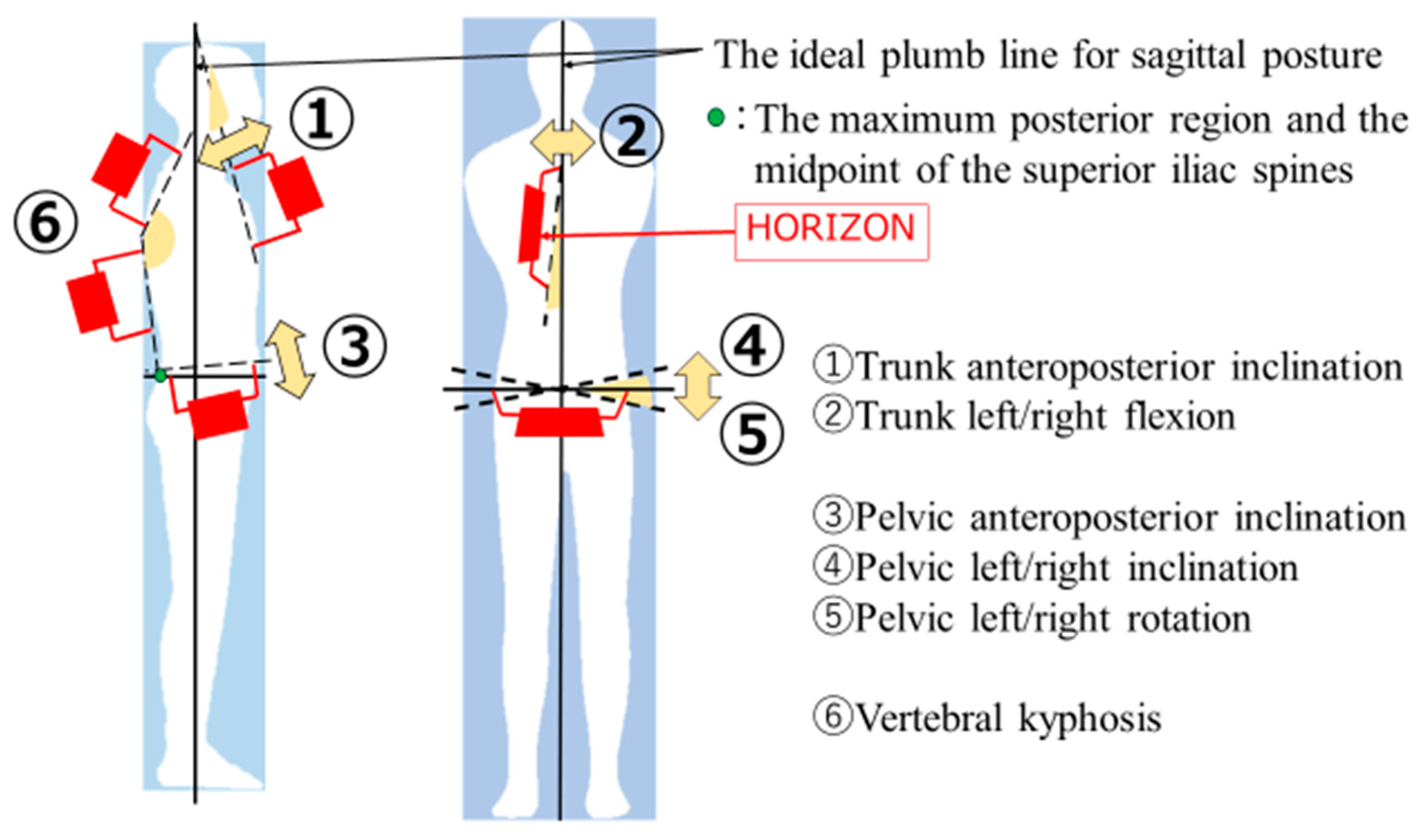
2.2. Measurements
2.2.1. Basic Information
2.2.2. Posture Evaluation
2.3. Grouping
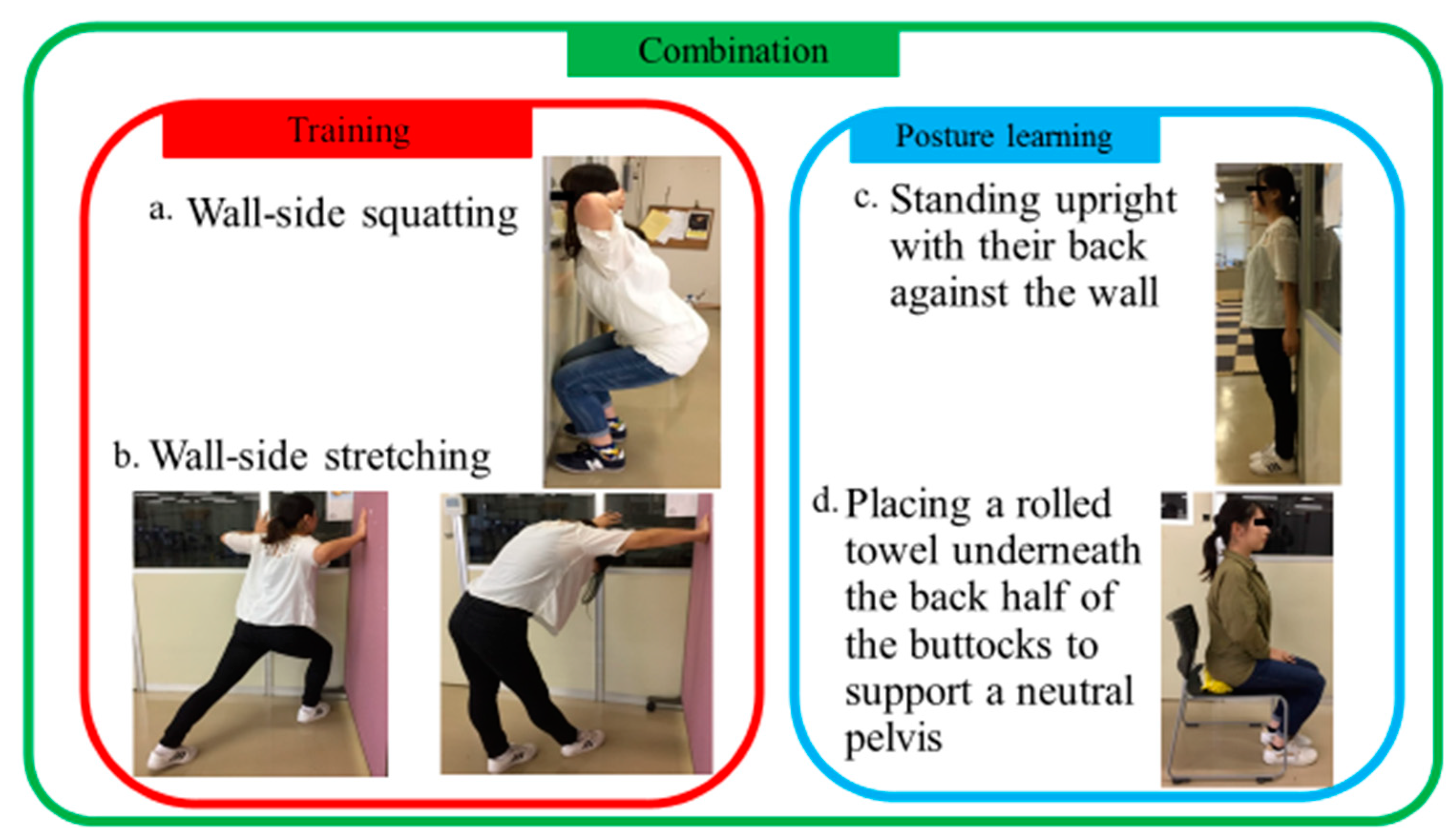
2.4. Details of the 4-Week Program
2.4.1. Wall-Side Squatting
2.4.2. Wall-Side Stretching
2.4.3. Standing Upright with Their Back against the Wall
2.4.4. Rolled Towel under the Sacrum
2.5. Measurement Protocol
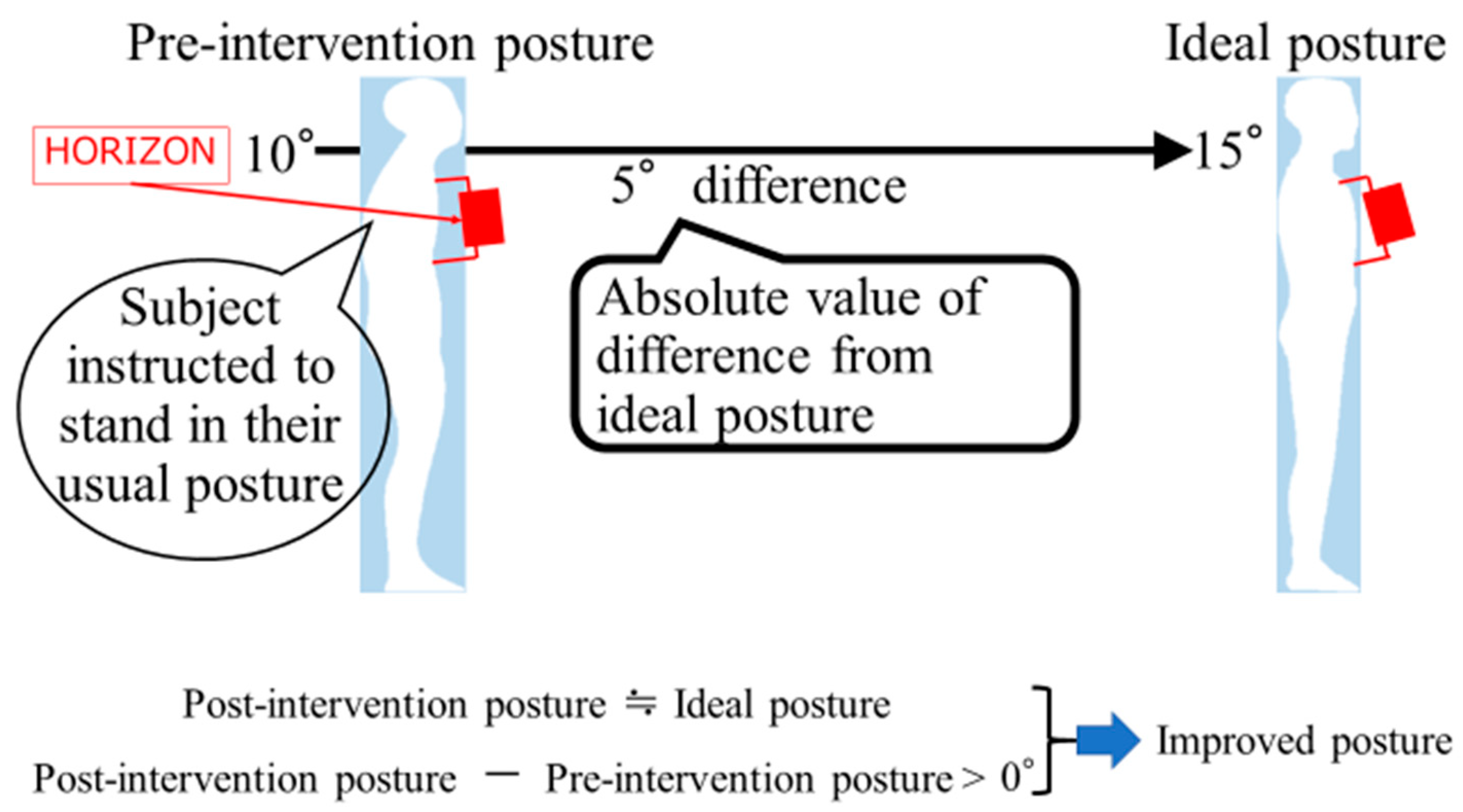
2.6. Definition of Improved Posture
2.7. Statistical Analysis
3. Results
3.1. Basic Characteristics of Each Group
3.2. Comparison of Improvement in Posture Evaluation Items between Groups
3.3. Percentage of People with Improved Posture
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mujawar, J.C.; Sagar, J.H. Prevalence of Upper Cross Syndrome in Laundry Workers. Indian J. Occup. Environ. Med. 2019, 23, 54–56. [Google Scholar] [CrossRef] [PubMed]
- Sasun, A.R.; Jawade, S.; Chitale, N. Measuring the Efficacy of Myofascial Rollers and Post-isometric Relaxation Technique in Relieving Pain Intensity and Postural Deviation Using Plumb Line Assessment for the Treatment of Upper Cross Syndrome in Dental Undergraduate (UG) Students. Cureus 2022, 14, e29831. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, W.S.; Hamza, H.H.; ElSais, W.M. Assessment of neck pain and cervical mobility among female computer workers at Hail University. Int. J. Occup. Saf. Erg. 2015, 21, 105–110. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K.; Ogata, T. Locomotive Syndrome: Definition and Management. Clin. Rev. Bone Min. Metab. 2016, 14, 56–67. [Google Scholar] [CrossRef]
- Hirano, K.; Imagama, S.; Hasegawa, Y.; Wakao, N.; Muramoto, A.; Ishiguro, N. Impact of back muscle strength and aging on locomotive syndrome in community living Japanese women. Nagoya J. Med. Sci. 2013, 75, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Kasukawa, Y.; Miyakoshi, N.; Hongo, M.; Ishikawa, Y.; Noguchi, H.; Kamo, K.; Sasaki, H.; Murata, K.; Shimada, Y. Relationships between falls, spinal curvature, spinal mobility and back extensor strength in elderly people. J. Bone Min. Metab. 2010, 28, 82–87. [Google Scholar] [CrossRef]
- Page, P. Muscle imbalances in older adults: Improving posture and decreasing pain. J. Act. Aging. 2005, 3, 30. [Google Scholar]
- Fukuda, T. Statokinetic Reflexes in Equilibrium and Movement; University Tokyo Press: Tokyo, Japan, 1984; pp. 110–123. [Google Scholar]
- Janda, V. Janda Compendium Vol II; Orthopaedic Physical Therapy Practice: Minneapolis, MN, USA, 1997; pp. 7–13. [Google Scholar]
- Goldberg, L.; Elliot, D.L.; Kuehl, K.S. A comparison of the cardiovascular effects of running and weight training. J. Strength Cond. Res. 1994, 8, 219–224. [Google Scholar]
- Stuart, M.J.; Meglan, D.A.; Lutz, G.E.; Growney, E.S.; An, K.N. Comparison of intersegmental tibiofemoral joint forces and muscle activity during various closed kinetic chain exercises. Am. J. Sport. Med. 1996, 24, 792–799. [Google Scholar] [CrossRef]
- Fry, A.C. Coaching considerations for the barbell squat-Part 1. J. Strength Cond. Res. 1993, 15, 556–569. [Google Scholar]
- Cho, M. The effects of modified wall squat exercises on average adults’ deep abdominal muscle thickness and lumbar stability. J. Phys. Sci. 2013, 25, 689–692. [Google Scholar] [CrossRef] [PubMed]
- Willson, J.D.; Dougherty, C.P.; Ireland, M.L.; Davis, I.M. Core stability and its relationship to lower extremity function and injury. J. Am. Acad. Orthop. Surg. 2005, 13, 316–325. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y. The influence of unstable modified wall squat exercises on the posture of female university students. J. Phys. Sci. 2015, 27, 2477–2480. [Google Scholar] [CrossRef] [PubMed]
- Christensen, K. Manual muscle testing and postural imbalance. Dyn. Chiropr. 2000, 18, 199–202. [Google Scholar]
- Noro, K.; Naruse, T.; Lueder, R.; Naoi, N.; Kozawa, M. Application of Zen sitting principles to microscopic surgery seating. Appl. Ergon. 2012, 43, 308–319. [Google Scholar] [CrossRef] [PubMed]
- Takahira, N. Low Back Pain Improves with a Rolled Towel; Kawade Shobo Shinsha: Tokyo, Japan, 2013; pp. 51–76. (In Japanese) [Google Scholar]
- Suzuki, Y.; Kamide, N.; Mizuno, K.; Takahashi-Narita, K.; Hiraga, Y.; Fukuda, M. Validity and reliability of evaluation of posture using a digital inclination meter. J. Phys. Ther. 2011, 23, 431–435. [Google Scholar] [CrossRef]
- Suzuki, Y.; Kawai, H.; Kojima, M.; Shiba, Y.; Yoshida, H.; Hirano, H.; Fujiwara, Y.; Ihara, K.; Obuchi, S. Construct validity of posture as a measure of physical function in elderly individuals: Use of a digitalized inclinometer to assess trunk inclination. Geriatr. Gerontol. Int. 2016, 16, 1068–1073. [Google Scholar] [CrossRef] [PubMed]
- Ueda, T.; Shiba, Y.; Watanabe, S.; Sato, H.; Mizuno, K. A New Device for Measuring Spinal Kyphosis: Validity and Reproducibility of Measurements Obtained Using a Small Gyro-embedded Device. Phys. Ther. Jpn. 2014, 41, 331–337. (In Japanese) [Google Scholar] [CrossRef]
- Rancour, J.; Holmes, C.F.; Cipriani, D.J. The effects of intermittent stretching following a 4-week static stretching protocol: A randomized trial. J. Strength Cond. Res. 2009, 23, 2217–2222. [Google Scholar] [CrossRef]
- Johnson, J. Postural Correction (Hands-on Guides for Therapists); Human Kinetics: Champaign, IL, USA, 2016. [Google Scholar]
- Janda, V. Muscle and cervicogenic pain syndromes. In Physical Therapy for the Cervical and Thoracic Spine; Grant, R.E., Ed.; Churchill Livingstone: Melbourne, Australia, 1988; pp. 153–166. [Google Scholar]
- Claeys, K.; Brumagne, S.; Deklerck, J.; Vanderhaeghen, J.; Dankaerts, W. Sagittal evaluation of usual standing and sitting spinal posture. J. Bodyw. Mov. Ther. 2016, 20, 326–333. [Google Scholar] [CrossRef]
- Kuo, Y.L.; Tully, E.A.; Galea, M.P. Kinematics of sagittal spine and lower limb movement in healthy older adults during sit-to-stand from two seat heights. Spine 2010, 35, E1–E7. [Google Scholar] [CrossRef] [PubMed]
- Roussouly, P.; Pinheiro-Franco, J.L. Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur. Spine J. 2011, 20, 609–618. [Google Scholar] [CrossRef] [PubMed]
- Vialle, R.; Levassor, N.; Rillardon, L.; Templier, A.; Skalli, W.; Guigui, P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J. Bone Jt. Surg. Am. 2005, 87, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Staffel, F. Die menschlichen Haltungstypen und ihre Beziehungen; J.F. Bergmann: Wiesbaden, Germany, 1889. [Google Scholar]
- Kendall, F.P.; McCreary, E.K.; Provance, P.G.; Rodgers, M.M.; Romani, W.A. Muscles: Testing and Function with Posture and Pain, 5th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2005. [Google Scholar]
| Control (n = 10) | Training (n = 10) | Posture (n = 10) | Combination (n = 10) | F-Value | p-Value | ||
|---|---|---|---|---|---|---|---|
| Age (years) | 20.3 ± 0.6 | 21.1 ± 0.9 | 21.1 ± 0.9 | 21.2 ± 0.7 | 2.30 | 0.09 | |
| Height (cm) | 158.2 ± 5.5 | 159.8 ± 6.2 | 159.6 ± 4.9 | 159.8 ± 3.2 | 0.20 | 0.89 | |
| Weight (kg) | 52.5 ± 7.1 | 54.8 ± 6.6 | 53.4 ± 6.2 | 55.4 ± 6.4 | 0.37 | 0.77 | |
| BMI (kg/m2) | 21.0 ± 1.7 | 21.4 ± 1.7 | 20.9 ± 1.7 | 21.7 ± 2.0 | 0.41 | 0.74 | |
| TAPI (°) | Ideal | 19.2 ± 3.5 | 17.9 ± 2.7 | 17.0 ± 3.8 | 16.8 ± 3.3 | 1.08 | 0.37 |
| Pre | 15.7 ± 3.3 | 12.5 ± 3.6 | 15.9 ± 2.5 | 12.5 ± 3.3 | 3.59 | 0.02 | |
| PAPI (°) | Ideal | 10.9 ± 1.8 | 15.2 ± 2.3 | 12.0 ± 2.1 | 16.4 ± 1.6 | 17.50 | 0.00 |
| Pre | 6.6 ± 0.9 | 9.5 ± 3.4 | 6.8 ± 1.7 | 9.2 ± 2.8 | 4.08 | 0.01 | |
| VKA (°) | Ideal | 170.8 ± 3.4 | 170.4 ± 3.7 | 169.5 ± 5.6 | 170.8 ± 3.2 | 0.21 | 0.89 |
| Pre | 166.4 ± 2.9 | 163.3 ± 4.3 | 164.1 ± 7.0 | 165.9 ± 4.7 | 0.86 | 0.47 | |
| Pairs Compared | No Adjustment | Adjustment a | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Average b | 95% CI | p-Value | Average b | 95% CI | p-Value | ||||||||
| TAPI | Post day 1 | Control | Training | −3.40 | −6.18 | to | −0.62 | 0.009 | −2.29 | −4.82 | to | 0.25 | 0.097 |
| Posture | −0.17 | −2.94 | to | 2.61 | 1.000 | −1.18 | −3.88 | to | 1.51 | 1.000 | |||
| Combination | −2.53 | −5.31 | to | 0.24 | 0.091 | −2.18 | −4.75 | to | 0.39 | 0.139 | |||
| Combination | Training | −0.87 | −3.64 | to | 1.91 | 1.000 | −0.11 | −2.67 | to | 2.45 | 1.000 | ||
| Posture | 2.37 | −0.41 | to | 5.14 | 0.136 | 1.00 | −1.73 | to | 3.72 | 1.000 | |||
| Posture | Training | −3.23 | −6.01 | to | −0.46 | 0.015 | −1.11 | −3.80 | to | 1.58 | 1.000 | ||
| Day 27 | Control | Training | −3.80 | −6.46 | to | −1.14 | 0.002 | −2.55 | −4.62 | to | −0.49 | 0.009 | |
| Posture | 0.27 | −2.39 | to | 2.92 | 1.000 | −0.64 | −2.84 | to | 1.56 | 1.000 | |||
| Combination | −2.90 | −5.56 | to | −0.24 | 0.026 | −2.34 | −4.43 | to | −0.25 | 0.022 | |||
| Combination | Training | −0.90 | −3.56 | to | 1.76 | 1.000 | −0.21 | −2.30 | to | 1.88 | 1.000 | ||
| Posture | 3.17 | 0.51 | to | 5.82 | 0.012 | 1.70 | −0.52 | to | 3.92 | 0.232 | |||
| Posture | Training | −4.07 | −6.72 | to | −1.41 | 0.001 | −1.91 | −4.11 | to | 0.28 | 0.118 | ||
| Day 34 | Control | Training | −1.70 | −4.30 | to | 0.90 | 0.458 | −0.49 | −2.38 | to | 1.40 | 1.000 | |
| Posture | 1.10 | −1.50 | to | 3.70 | 1.000 | 0.52 | −1.49 | to | 2.53 | 1.000 | |||
| Combination | −1.00 | −3.60 | to | 1.60 | 1.000 | 0.03 | −1.88 | to | 1.95 | 1.000 | |||
| Combination | Training | −0.70 | −3.30 | to | 1.90 | 1.000 | −0.52 | −2.43 | to | 1.39 | 1.000 | ||
| Posture | 2.10 | −0.50 | to | 4.70 | 0.182 | 0.49 | −1.54 | to | 2.52 | 1.000 | |||
| Posture | Training | −2.80 | −5.40 | to | −0.20 | 0.029 | −1.01 | −3.02 | to | 1.00 | 1.000 | ||
| PAPI | Post day 1 | Control | Training | −2.43 | −4.91 | to | 0.04 | 0.056 | −2.49 | −6.02 | to | 1.05 | 0.338 |
| Posture | −3.20 | −5.68 | to | −0.72 | 0.006 | −2.47 | −6.11 | to | 1.17 | 0.389 | |||
| Combination | −4.77 | −7.24 | to | −2.29 | <0.001 | −5.35 | −8.87 | to | −1.83 | <0.001 | |||
| Combination | Training | 2.33 | −0.14 | to | 4.81 | 0.075 | 2.86 | 0.47 | to | 5.26 | 0.012 | ||
| Posture | 1.57 | −0.91 | to | 4.04 | 0.514 | 2.87 | 0.32 | to | 5.42 | 0.020 | |||
| Posture | Training | 0.77 | −1.71 | to | 3.24 | 1.000 | −0.01 | −2.58 | to | 2.56 | 1.000 | ||
| Day 27 | Control | Training | −2.43 | −5.05 | to | 0.18 | 0.081 | −2.93 | −6.44 | to | 0.58 | 0.151 | |
| Posture | −4.03 | −6.65 | to | −1.42 | <0.001 | −3.36 | −6.98 | to | 0.25 | 0.081 | |||
| Combination | −5.30 | −7.91 | to | −2.69 | <0.001 | −6.19 | −9.68 | to | −2.69 | <0.001 | |||
| Combination | Training | 2.87 | 0.25 | to | 5.48 | 0.025 | 3.26 | 0.88 | to | 5.64 | 0.003 | ||
| Posture | 1.27 | −1.35 | to | 3.88 | 1.000 | 2.82 | 0.29 | to | 5.36 | 0.022 | |||
| Posture | Training | 1.60 | −1.01 | to | 4.21 | 0.577 | 0.43 | −2.12 | to | 2.99 | 1.000 | ||
| Day 34 | Control | Training | −1.10 | −2.72 | to | 0.52 | 0.393 | −1.49 | −3.20 | to | 0.22 | 0.121 | |
| Posture | −0.30 | −1.92 | to | 1.32 | 1.000 | 0.36 | −1.40 | to | 2.13 | 1.000 | |||
| Combination | −1.47 | −3.08 | to | 0.15 | 0.095 | −1.76 | −3.47 | to | −0.05 | 0.040 | |||
| Combination | Training | 0.37 | −1.25 | to | 1.98 | 1.000 | 0.27 | −0.89 | to | 1.43 | 1.000 | ||
| Posture | 1.17 | −0.45 | to | 2.78 | 0.309 | 2.12 | 0.89 | to | 3.36 | <0.001 | |||
| Posture | Training | −0.80 | −2.42 | to | 0.82 | 1.000 | −1.85 | −3.10 | to | −0.61 | 0.001 | ||
| VKA | Post day 1 | Control | Training | −3.77 | −7.19 | to | −0.34 | 0.024 | −2.23 | −4.92 | to | 0.46 | 0.156 |
| Posture | −3.93 | −7.36 | to | −0.51 | 0.017 | −3.12 | −5.72 | to | −0.51 | 0.012 | |||
| Combination | −2.10 | −5.52 | to | 1.32 | 0.572 | −1.77 | −4.40 | to | 0.85 | 0.398 | |||
| Combination | Training | −1.67 | −5.09 | to | 1.76 | 1.000 | −0.46 | −3.02 | to | 2.10 | 1.000 | ||
| Posture | −1.83 | −5.26 | to | 1.59 | 0.862 | −1.35 | −3.82 | to | 1.13 | 0.815 | |||
| Posture | Training | 0.17 | −3.26 | to | 3.59 | 1.000 | 0.89 | −1.66 | to | 3.43 | 1.000 | ||
| Day 27 | Control | Training | −4.87 | −8.03 | to | −1.70 | <0.001 | −3.50 | −5.66 | to | −1.33 | <0.001 | |
| Posture | −4.40 | −7.57 | to | −1.23 | 0.003 | −3.64 | −5.73 | to | −1.54 | <0.001 | |||
| Combination | −2.73 | −5.90 | to | 0.43 | 0.127 | −2.57 | −4.68 | to | −0.46 | 0.010 | |||
| Combination | Training | −2.13 | −5.30 | to | 1.03 | 0.409 | −0.92 | −2.98 | to | 1.14 | 1.000 | ||
| Posture | −1.67 | −4.83 | to | 1.50 | 0.903 | −1.06 | −3.05 | to | 0.93 | 0.856 | |||
| Posture | Training | −0.47 | −3.63 | to | 2.70 | 1.000 | 0.14 | −1.91 | to | 2.18 | 1.000 | ||
| Day 34 | Control | Training | −1.97 | −5.16 | to | 1.23 | 0.567 | −0.67 | −3.28 | to | 1.95 | 1.000 | |
| Posture | −1.90 | −5.10 | to | 1.30 | 0.635 | −1.62 | −4.15 | to | 0.91 | 0.486 | |||
| Combination | −1.37 | −4.56 | to | 1.83 | 1.000 | −1.49 | −4.04 | to | 1.06 | 0.665 | |||
| Combination | Training | −0.60 | −3.80 | to | 2.60 | 1.000 | 0.82 | −1.67 | to | 3.31 | 1.000 | ||
| Posture | −0.53 | −3.73 | to | 2.66 | 1.000 | −0.14 | −2.54 | to | 2.27 | 1.000 | |||
| Posture | Training | −0.07 | −3.26 | to | 3.13 | 1.000 | 0.96 | −1.51 | to | 3.43 | 1.000 | ||
| Control (n = 10) | Training (n = 10) | Posture (n = 10) | Combination (n = 10) | |
|---|---|---|---|---|
| Post day 1 | 20/40/50/10 | 90/90/90/70 | 70/90/90/60 | 90/100/80/70 |
| Day 27 | 40/10/40/0 | 100/90/100/90 | 60/100/90/50 | 100/100/100/100 |
| Day 34 | 30/10/50/0 | 70/70/70/40 | 50/30/80/20 | 50/60/60/20 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takahira, N.; Kudo, S.; Ofusa, M.; Sakai, K.; Tsuda, K.; Tozaki, K.; Takahashi, Y.; Kaneda, H. Effect of Devised Simultaneous Physical Function Improvement Training and Posture Learning Exercises on Posture. Healthcare 2023, 11, 1287. https://doi.org/10.3390/healthcare11091287
Takahira N, Kudo S, Ofusa M, Sakai K, Tsuda K, Tozaki K, Takahashi Y, Kaneda H. Effect of Devised Simultaneous Physical Function Improvement Training and Posture Learning Exercises on Posture. Healthcare. 2023; 11(9):1287. https://doi.org/10.3390/healthcare11091287
Chicago/Turabian StyleTakahira, Naonobu, Sho Kudo, Mako Ofusa, Kenta Sakai, Kouji Tsuda, Kiyoshi Tozaki, Yoshiki Takahashi, and Hiroaki Kaneda. 2023. "Effect of Devised Simultaneous Physical Function Improvement Training and Posture Learning Exercises on Posture" Healthcare 11, no. 9: 1287. https://doi.org/10.3390/healthcare11091287
APA StyleTakahira, N., Kudo, S., Ofusa, M., Sakai, K., Tsuda, K., Tozaki, K., Takahashi, Y., & Kaneda, H. (2023). Effect of Devised Simultaneous Physical Function Improvement Training and Posture Learning Exercises on Posture. Healthcare, 11(9), 1287. https://doi.org/10.3390/healthcare11091287





