Patient Safety Incidents in Primary Care: Comparing APEAS–2007 (Spanish Patient Safety Adverse Events Study in Primary Care) with Data from a Health Area in Catalonia (Spain) in 2019
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Incident Reporting and Data Collection Procedure Project
2.2.1. Step (1): Incident Detection through mAPaSP Study Collaborators
2.2.2. Step (2) Registration of mAPaSP Study Incidents in the Catalan Patient Safety Incident Reporting System Cloud Platform
2.3. Taxonomy and Definition of Variables
2.4. Statistical Analysis
3. Results
3.1. Adverse Events: Prevalence and Nature
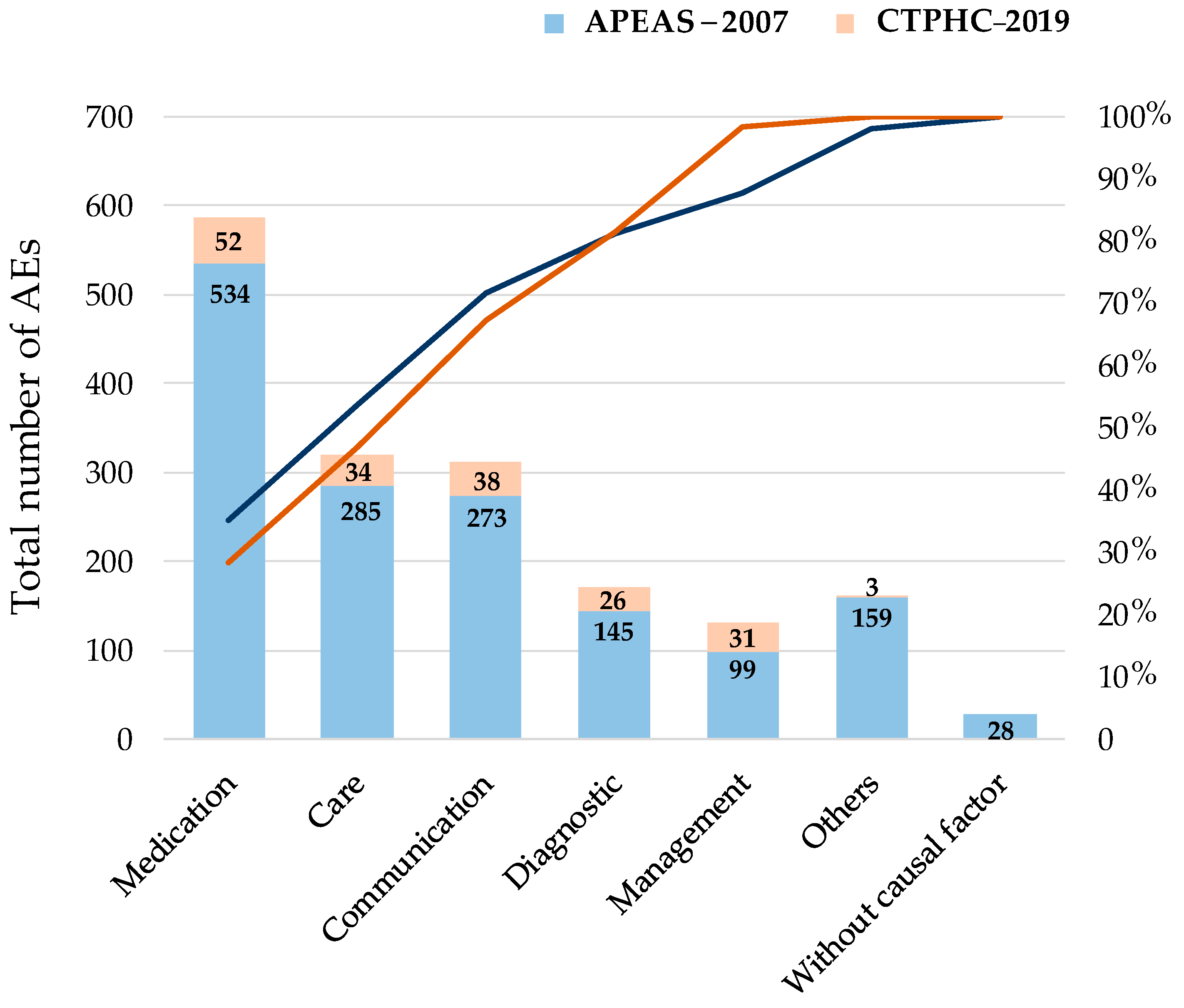
3.2. Adverse Events: Causal Factors
3.3. Severity and Preventability
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AE | Adverse Event |
| APEAS–2007 | Spanish National Adverse Events Study in Primary Health Care in 2007 |
| CTPHC–2019 | Camp de Tarragona Primary Health Care Regional Study in 2019 |
| PHC | Primary Healthcare |
| PS | Patient Safety |
| PSRLS | PS reporting and learning systems |
References
- Vincent, C.; Amalberti, R. Safer Healthcare: Strategies for the Real World; Springer: Oxford, UK, 2016. Available online: https://www.ncbi.nlm.nih.gov/books/NBK481869/ (accessed on 20 December 2023).
- Global Patient Safety Action Plan 2021–2030: Towards Eliminating Avoidable Harm in Health Care. World Health Organization: Geneva, 2021. Available online: https://www.who.int/publications/i/item/9789240032705 (accessed on 20 December 2023).
- Stavropoulou, C.; Doherty, C.; Tosey, P. How Effective Are Incident-Reporting Systems for Improving Patient Safety? A Systematic Literature Review. Milbank Q. 2015, 93, 826–866. [Google Scholar] [CrossRef] [PubMed]
- Auraaen, A.; Slawomirski, L.; Klazinga, N. The economics of patient safety in primary and ambulatory care: Flying blind. OECD Health Work. Pap. 2018, 106. [Google Scholar] [CrossRef]
- Panesar, S.S.; deSilva, D.; Carson-Stevens, A.; Cresswell, K.M.; Salvilla, S.A.; Slight, S.P.; Javad, S.; Netuveli, G.; Larizgoitia, I.; Donaldson, L.J.; et al. How safe is primary care? A systematic review. BMJ Qual. Saf. 2016, 25, 544–553. [Google Scholar] [CrossRef] [PubMed]
- Avery, A.J.; Sheehan, C.; Bell, B.; Armstrong, S.; Ashcroft, D.M.; Boyd, M.J.; Chuter, A.; Cooper, A.; Donnelly, A.; Edwards, A.; et al. Incidence, nature and causes of avoidable significant harm in primary care in England: Retrospective case note review. BMJ Qual. Saf. 2021, 30, 961–976. [Google Scholar] [CrossRef] [PubMed]
- Panagioti, M.; Khan, K.; Keers, R.N.; Abuzour, A.; Phipps, D.; Kontopantelis, E.; Bower, P.; Campbell, S.; Haneef, R.; Avery, A.J.; et al. Prevalence, severity, and nature of preventable patient harm across medical care settings: Systematic review and meta-analysis. BMJ 2019, 366, 14185. [Google Scholar] [CrossRef] [PubMed]
- Guerra-García, M.M.; Campos-Rivas, B.; Sanmarful-Schwarz, A.; Vírseda-Sacristán, A.; Dorrego-López, M.A.; Charle-Crespo, Á. Descripción de factores contribuyentes en sucesos adversos relacionados con la seguridad del paciente y su evitabilidad. Aten Primaria 2018, 50, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Oliva, G.; Alava, F.; Navarro, L.; Esquerra, M.; Lushchenkova, O.; Davins, J.; Vallès, R. Notificación de incidentes relacionados con la seguridad del paciente en los hospitales de Cataluña durante el período 2010–2013. Med. Clin. 2014, 143 (Suppl. S1), 55–61. [Google Scholar] [CrossRef] [PubMed]
- APEAS Study. Patient Safety in Primary Healthcare; Ministry of Health and Consumer Affairs: Madrid, Spain, 2008. [Google Scholar]
- Aranaz-Andrés, J.M.; Aibar, C.; Limón, R.; Mira, J.J.; Vitaller, J.; Agra, Y.; Terol, E. A study of the prevalence of adverse events in primary healthcare in Spain. Eur. J. Public Health 2012, 22, 921–925. [Google Scholar] [CrossRef] [PubMed]
- Sistema de Notificación y Aprendizaje para la Seguridad del Paciente (SiNASP). Primer Informe de Incidentes de Seguridad Notificados al Sistema Año 2013. Ministerio de Sanidad, Servicios Sociales e Igualdad Centro de Publicaciones: Spain, 2015. Available online: https://seguridaddelpaciente.sanidad.gob.es/proyectos/financiacionEstudios/sistemasInformacionNotificacion/incidentesEASNS/sinasp2013.htm (accessed on 20 December 2023).
- Archer, S.; Hull, L.; Soukup, T.; Mayer, E.; Athanasiou, T.; Sevdalis, N.; Darzi, A. Development of a theoretical framework of factors affecting patient safety incident reporting: A theoretical review of the literature. BMJ Open 2017, 7, e017155. [Google Scholar] [CrossRef]
- Sheikh, A.; Panesar, S.S.; Larizgoitia, I.; Bates, D.W.; Donaldson, L.J. Safer primary care for all: A global imperative. Lancet Glob. Health 2013, 1, e182–e183. [Google Scholar] [CrossRef]
- Astier-Peña, M.P.; Torijano-Casalengua, M.L.; Olivera-Cañadas, G.; Silvestre-Busto, C.; Agra-Varela, Y.; Maderuelo-Fernández, J.Á. Are Spanish primary care professionals aware of patient safety? Eur. J. Public Health 2015, 25, 781–787. [Google Scholar] [CrossRef] [PubMed]
- Sistema de Notificación y Aprendizaje para la Seguridad del Paciente (SiNASP). Incidentes de Seguridad Notificados en 2018. Ministerio de Sanidad, Servicios Sociales e Igualdad Centro de Publicaciones: Spain, 2020. Available online: https://sinasp.es/storage/Documentos/Publicacion/informes_de_notificaciones_si_n_a_s_p/hQb_InformeSiNASP2018.pdf (accessed on 20 December 2023).
- Astier-Peña, M.P.; Torijano-Casalengua, M.L.; Añel-Rodríguez, R.; Palacio-Lapuente, J.; Aibar-Remón, C. Pasado, presente y futuro de la seguridad del paciente en Atención Primaria. Aten Primaria 2021, 53 (Suppl. S1), 102221. [Google Scholar] [CrossRef] [PubMed]
- Gens-Barberà, M.; Hernández-Vidal, N.; Vidal-Esteve, E.; Mengíbar-García, Y.; Hospital-Guardiola, I.; Oya-Girona, E.M.; Bejarano-Romero, F.; Castro-Muniain, C.; Satué-Gracia, E.M.; Rey-Reñones, C.; et al. Analysis of Patient Safety Incidents in Primary Care Reported in an Electronic Registry Application. Int. J. Environ. Res. Public Health 2021, 18, 8941. [Google Scholar] [CrossRef] [PubMed]
- Massanés, M.; Álava, F.; Oliva, G.; Navarro, L.; Jiménez, M.; Esquerra, M.; Davins, J.; Rams, N. Notificació i gestió d’incidents relacionats amb la seguretat dels pacients com a eina per a la millora contínua. Ann. Med. 2017, 100, 18–22. [Google Scholar]
- Gens-Barberà, M.; Hernández-Vidal, N.; Castro-Muniain, C.; Hospital-Guardiola, I.; Oya-Girona, E.M.; Bejarano-Romero, F.; Rey-Reñones, C.; Martín-Luján, F.; en Nombre del Grupo de Estudio de Calidad y Seguridad del Paciente de Tarragona (QiSP-TAR). Incidentes de seguridad del paciente notificados antes y después del inicio de la pandemia de COVID-19 en atención primaria en Tarragona. Aten. Primaria 2021, 53, 102217. [Google Scholar] [CrossRef] [PubMed]
- World Alliance for Patient Safety. Conceptual Framework for the International Classification for Patient Safety Version 1.1: Final Technical Report January 2009; WHO: Geneva, Switzerland, 2009; Available online: https://apps.who.int/iris/handle/10665/70882 (accessed on 2 May 2023).
- Acreditació d’equips d’atenció Primària a Catalunya: Manual d’estàndards. Departament de Salut: Barcelona 2015. Available online: https://scientiasalut.gencat.cat/handle/11351/1679 (accessed on 20 December 2023).
- Cooper, J.; Williams, H.; Hibbert, P.; Edwards, A.; Butt, A.; Wood, F.; Parry, G.; Smith, P.; Sheikh, A.; Donaldson, L.; et al. Classification of patient-safety incidents in primary care. Bull. World Health Organ 2018, 96, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Davins, J.; Gens, M.; Pareja, C.; Guzmán, R.; Marquet, R.; Vallès, R. El modelo de acreditación de atención primaria de Catalunya: Un modelo válido. Med. Clin. 2014, 143, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Integrated Health Services. Administrative Errors: Technical Series on Safer Primary Care; World Health Organization: Geneva, Switzerland, 2016; Available online: https://iris.who.int/handle/10665/252270 (accessed on 20 December 2023).
- de la Torre-Pérez, L.; Granés, L.; Prat Marín, A.; Bertran, M.J. A hospital incident reporting system (2016–2019): Learning from notifier’s perception on incidents’ risk, severity and frequency of adverse events. J. Healthc Qual. Res. 2023, 38, 93–104. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Molero, S.; Laserna-Jiménez, C.; Baiget-Ortega, A.; Flayeh-Beneyto, S.; Ríos-Jiménez, A.; Fabrellas-Padrés, N. Treatment of minor health problems by primary care nurses: A cross-sectional study. J. Clin. Nurs. 2023, 32, 2913–2921. [Google Scholar] [CrossRef]
- Granel, N.; Manresa-Domínguez, J.M.; Watson, C.E.; Gómez-Ibáñez, R.; Bernabeu-Tamayo, M.D. Nurses’ perceptions of patient safety culture: A mixed-methods study. BMC Health Serv Res 2020, 20, 584. [Google Scholar] [CrossRef]
- Leape, L.L. Reporting of adverse events. N. Engl. J. Med. 2002, 347, 1633–1638. [Google Scholar] [CrossRef]
- Howell, A.M.; Burns, E.M.; Bouras, G.; Donaldson, L.J.; Athanasiou, T.; Darzi, A. Can Patient Safety Incident Reports Be Used to Compare Hospital Safety? Results from a Quantitative Analysis of the English National Reporting and Learning System Data. PLoS ONE 2015, 10, e0144107. [Google Scholar] [CrossRef]
- Davins-Miralles, J.; Gens, M.; García, A.; Álava-Cano, F.; Oliva-Oliva, G.; Lushchenkova, O.; Navarro, L.; Esquerra, M.; Fabré, P.; Constante, C. Desenvolupament de les unitats funcionals de seguretat dels pacients en l’atenció primària de Catalunya. Ann Med. 2012, 96, 111–114. [Google Scholar]
- Gens-Barberà, M.; Hernández-Vidal, N.; Mengíbar-García, Y.; Ayala-Villuendas, D.; Hernández-Villén, O.; Martín-Luján, F.; Pareja-Rossell, C.; Gràcia-Escoriza, R. “Coneixement, innovació i tecnología”, treballem junts per millorar la seguretat del pacient: Aplicació proactiva en seguretat dels pacients proSP. Ann Med. 2021, 104, 6–10. [Google Scholar]
- Carlfjord, S.; Öhrn, A.; Gunnarsson, A. Experiences from ten years of incident reporting in health care: A qualitative study among department managers and coordinators. BMC Health Serv. Res. 2018, 18, 113. [Google Scholar] [CrossRef]
- de Kam, D.; Kok, J.; Grit, K.; Leistikow, I.; Vlemminx, M.; Bal, R. How incident reporting systems can stimulate social and participative learning: A mixed-methods study. Health Policy 2020, 124, 834–841. [Google Scholar] [CrossRef]
- Verbeek-van Noord, I.; Smits, M.; Zwijnenberg, N.C.; Spreeuwenberg, P.; Wagner, C. A nation-wide transition in patient safety culture: A multilevel analysis on two cross-sectional surveys. Int. J. Qual. Health Care 2019, 31, 627–632. [Google Scholar] [CrossRef] [PubMed]
- Lawati, M.H.A.; Dennis, S.; Short, S.D.; Abdulhadi, N.N. Patient safety and safety culture in primary health care: A systematic review. BMC Fam. Pract. 2018, 19, 104. [Google Scholar] [CrossRef]
- Morris, R.L.; Stocks, S.J.; Alam, R.; Taylor, S.; Rolfe, C.; Glover, S.W.; Whitcombe, J.; Campbell, S.M. Identifying primary care patient safety research priorities in the UK: A James Lind Alliance Priority Setting Partnership. BMJ Open 2018, 8, e020870. [Google Scholar] [CrossRef]
- Chaneliere, M.; Koehler, D.; Morlan, T.; Berra, J.; Colin, C.; Dupie, I.; Michel, P. Factors contributing to patient safety incidents in primary care: A descriptive analysis of patient safety incidents in a French study using CADYA (categorization of errors in primary care). BMC Fam. Pract. 2018, 19, 121. [Google Scholar] [CrossRef]
- Michel, P.; Brami, J.; Chanelière, M.; Kret, M.; Mosnier, A.; Dupie, I.; Haeringer-Cholet, A.; Keriel-Gascou, M.; Maradan, C.; Villebrun, F.; et al. Patient safety incidents are common in primary care: A national prospective active incident reporting survey. PLoS ONE 2017, 12, e0165455. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.; Jürgens, J.; Redaèlli, M.; Klingberg, K.; Hautz, W.E.; Stock, S. Impact of the communication and patient hand-off tool SBAR on patient safety: A systematic review. BMJ Open 2018, 8, e022202. [Google Scholar] [CrossRef] [PubMed]
- Gleeson, L.L.; Clyne, B.; Barlow, J.W.; Ryan, B.; Murphy, P.; Wallace, E.; De Brún, A.; Mellon, L.; Hanratty, M.; Ennis, M.; et al. Medication safety incidents associated with the remote delivery of primary care: A rapid review. Int. J. Pharm. Pract. 2022, 30, 495–506. [Google Scholar] [CrossRef] [PubMed]
- Bates, D.W.; Levine, D.; Syrowatka, A.; Kuznetsova, M.; Craig, K.J.T.; Rui, A.; Jackson, G.P.; Rhee, K. The potential of artificial intelligence to improve patient safety: A scoping review. NPJ Digit. Med. 2021, 4, 54. [Google Scholar] [CrossRef] [PubMed]
- Portela-Romero, M.; Bugarín-González, R.; Rodríguez-Calvo, M.S. La cultura de seguridad del paciente en los médicos internos residentes de Medicina Familiar y Comunitaria de Galicia. Aten. Primaria 2017, 49, 343–350. [Google Scholar] [CrossRef] [PubMed]
- Hernan, A.L.; Giles, S.J.; Carson-Stevens, A.; Morgan, M.; Lewis, P.; Hind, J.; Versace, V. Nature and type of patient-reported safety incidents in primary care: Cross-sectional survey of patients from Australia and England. BMJ Open 2021, 11, e042551. [Google Scholar] [CrossRef]
- Fiol-deRoque, M.A.; Serrano-Ripol, M.J.; Gens-Barberà, M.; Sánchez, E.; Mayer, M.A.; Martín-Luján, F.; Valderas, J.M.; Ricci-Cabello, I. Impacto de la pandemia de COVID-19 en la seguridad del paciente percibida por los pacientes en Atención Primaria. Aten. Primaria 2021, 53, 102222. [Google Scholar] [CrossRef]

| Nature of AEs | APEAS–2007 | CTPHC–2019 | p-Value | ||
|---|---|---|---|---|---|
| N = 1108 | % (IC 95%) | N = 165 | % (IC 95%) | ||
| Related to medication | 530 | 47.83 (44.91–50.78) | 46 | 27.88 (21.04–34.72) | <0.001 |
| Worsened clinical course of the underlying disease | 221 | 19.95 (17.70–22.40) | 65 | 39.39 (31.94–46.85) | |
| Related to procedures | 118 | 10.65 (8.97–12.60) | 23 | 13.94 (8.65–19.22) | |
| Associated with healthcare-related infections | 93 | 8.39 (6.90–10.17) | 2 | 1.21 (0.03–2.88) | |
| Related to care | 72 | 6.50 (5.19–8.11) | 9 | 5.45 (1.99–8.92) | |
| Others | 74 | 6.68 (5.35–8.30) | 20 | 12.12 (7.14–17.10) | |
| Grade of Severity | APEAS–2007 | CTPHC–2019 | p-Value | ||
|---|---|---|---|---|---|
| N = 1108 | % (IC 95%) | N = 105 | % (IC 95%) | ||
| Mild | 606 | 54.69 (51.76–57.62) | - | - | p < 0.001 |
| Moderate | 421 | 38.00 (35.14–40.85) | 103 | 98.1 (95.48–99.48) | |
| Severe | 81 | 7.31 (5.78–8.84) | 2 | 1.90 (0.52–4.52) | |
| APEAS–2007 | CTPHC–2019 | p-Value | |||
|---|---|---|---|---|---|
| N | % Avoidable Events | N | % Avoidable Events | ||
| Total PCP | |||||
| Related to procedure | 94 | 79.7 | 20 | 86.96 | 0.567 |
| Associated with healthcare-related infections | 74 | 79.6 | 2 | 100.0 | 1.0 |
| Related to care | 52 | 72.2 | 8 | 88.89 | 0.434 |
| Related to medication | 313 | 59.1 | 17 | 43.59 | 0.085 |
| Worsened clinical course of the underlying disease | 183 | 82.8 | 49 | 90.74 | 0.219 |
| Other factors | 79 | 83.8 | 17 | 85.0 | 1.0 |
| Total | 778 | 70.2 | 113 | 76.87 | 0.116 |
| Family doctors | |||||
| Procedure | 33 | 75.0 | 14 | 87.5 | 0.481 |
| Infection | 26 | 74.3 | 2 | 100.0 | 1.0 |
| Healthcare | 12 | 70.6 | 3 | 100.0 | 0.540 |
| Medication | 229 | 58.0 | 13 | 40.63 | 0.003 |
| Worsened evolutionary course of the disease | 131 | 81.4 | 31 | 88.57 | 0.439 |
| Other factors | 31 | 83.8 | 11 | 84.62 | 1.0 |
| Total | 462 | 67.1 | 74 | 73.27 | 0.308 |
| Nurse | |||||
| Procedure | 60 | 82.2 | 4 | 80.0 | 1.0 |
| Infection | 47 | 82.5 | - | - | |
| Healthcare | 39 | 73.6 | 4 | 80.0 | 1.0 |
| Medication | 70 | 64.2 | 4 | 66.67 | 1.0 |
| Worsened evolutionary course of the disease | 37 | 86.0 | 15 | 93.75 | 0.661 |
| Other factors | 27 | 87.1 | 5 | 83.33 | 1.0 |
| Total | 280 | 76.5 | 22 | 84.21 | 0.382 |
| Nature of AE | APEAS–2007 | CTPHC–2019 | p-Value | ||
|---|---|---|---|---|---|
| N = 1108 | % (IC 95%) | N = 165 | % (IC 95%) | ||
| Related to medication | 530 | 47.83 (44.91–50.78) | 46 | 27.88 (21.04–34.72) | <0.001 |
| Worsened clinical course of the underlying disease | 221 | 19.95 (17.70–22.40) | 65 | 39.39 (31.94–46.85) | |
| Related to procedures | 118 | 10.65 (8.97–12.60) | 23 | 13.94 (8.65–19.22) | |
| Associated with healthcare-related infections | 93 | 8.39 (6.90–10.17) | 2 | 1.21 (0.03–2.88) | |
| Related to care | 72 | 6.50 (5.19–8.11) | 9 | 5.45 (1.99–8.92) | |
| Others | 74 | 6.68 (5.35–8.30) | 20 | 12.12 (7.14–17.10) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gens-Barberà, M.; Astier-Peña, M.-P.; Hernández-Vidal, N.; Hospital-Guardiola, I.; Bejarano-Romero, F.; Oya-Girona, E.M.; Mengíbar-Garcia, Y.; Mansergas-Collado, N.; Vila-Rovira, A.; Martínez-Torres, S.; et al. Patient Safety Incidents in Primary Care: Comparing APEAS–2007 (Spanish Patient Safety Adverse Events Study in Primary Care) with Data from a Health Area in Catalonia (Spain) in 2019. Healthcare 2024, 12, 1086. https://doi.org/10.3390/healthcare12111086
Gens-Barberà M, Astier-Peña M-P, Hernández-Vidal N, Hospital-Guardiola I, Bejarano-Romero F, Oya-Girona EM, Mengíbar-Garcia Y, Mansergas-Collado N, Vila-Rovira A, Martínez-Torres S, et al. Patient Safety Incidents in Primary Care: Comparing APEAS–2007 (Spanish Patient Safety Adverse Events Study in Primary Care) with Data from a Health Area in Catalonia (Spain) in 2019. Healthcare. 2024; 12(11):1086. https://doi.org/10.3390/healthcare12111086
Chicago/Turabian StyleGens-Barberà, Montserrat, Maria-Pilar Astier-Peña, Núria Hernández-Vidal, Immaculada Hospital-Guardiola, Ferran Bejarano-Romero, Eva Mª Oya-Girona, Yolanda Mengíbar-Garcia, Nuria Mansergas-Collado, Angel Vila-Rovira, Sara Martínez-Torres, and et al. 2024. "Patient Safety Incidents in Primary Care: Comparing APEAS–2007 (Spanish Patient Safety Adverse Events Study in Primary Care) with Data from a Health Area in Catalonia (Spain) in 2019" Healthcare 12, no. 11: 1086. https://doi.org/10.3390/healthcare12111086
APA StyleGens-Barberà, M., Astier-Peña, M.-P., Hernández-Vidal, N., Hospital-Guardiola, I., Bejarano-Romero, F., Oya-Girona, E. M., Mengíbar-Garcia, Y., Mansergas-Collado, N., Vila-Rovira, A., Martínez-Torres, S., Rey-Reñones, C., Martín-Luján, F., & QiSP-Tar Research Group. (2024). Patient Safety Incidents in Primary Care: Comparing APEAS–2007 (Spanish Patient Safety Adverse Events Study in Primary Care) with Data from a Health Area in Catalonia (Spain) in 2019. Healthcare, 12(11), 1086. https://doi.org/10.3390/healthcare12111086






