Exploring the Impact of Online Medical Team Engagement on Patient Satisfaction: A Semantic Features Perspective
Abstract
1. Introduction
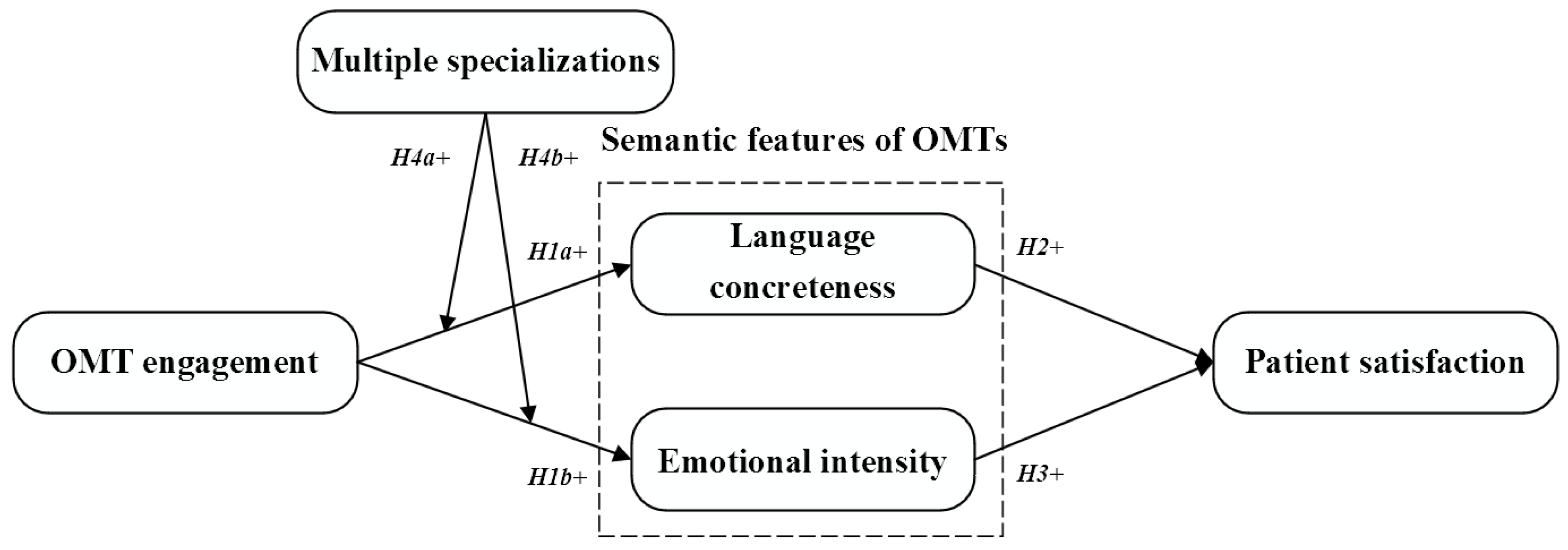
- RQ1: Does OMT engagement improve language concreteness and emotional intensity during OTCs, which subsequently enhances patient satisfaction?
- RQ2: Is the impact of OMT engagement on language concreteness and emotional intensity contingent on multiple specializations?
2. Literature Review
2.1. Online Medical Teams and Team Engagement
2.2. Patient Satisfaction
3. Development of Hypotheses
4. Methodology
4.1. Research Context and Data Collection
4.2. Measures
4.3. Analysis and Results
4.4. Robustness Checks
5. Discussion
5.1. Main Findings
5.2. Theoretical Implications
5.3. Practical Implications
5.4. Limitations and Future Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alnashwan, R.; O’Riordan, A.; Sorensen, H. Multiple-Perspective Data-Driven Analysis of Online Health Communities. Healthcare 2023, 11, 2723. [Google Scholar] [CrossRef]
- Chen, Z.; Song, Q.; Wang, A.; Xie, D.; Qi, H. Study on the Relationships between Doctor Characteristics and Online Consultation Volume in the Online Medical Community. Healthcare 2022, 10, 1551. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Wang, Q. Doctors’ Preferences in the Selection of Patients in Online Medical Consultations: An Empirical Study with Doctor–Patient Consultation Data. Healthcare 2022, 10, 1435. [Google Scholar] [CrossRef] [PubMed]
- Meng, F.; Liu, Y.; Zhang, X.; Liu, L. General Knowledge-Sharing and Patient Engagement in Online Health Communities: An Inverted U-Shaped Relationship. J. Knowl. Manag. 2023, 28, 763–788. [Google Scholar] [CrossRef]
- Yang, H.; Yan, Z.; Jia, L.; Liang, H. The Impact of Team Diversity on Physician Teams’ Performance in Online Health Communities. Inf. Process. Manag. 2021, 58, 102421. [Google Scholar] [CrossRef]
- Wu, H.; Deng, Z. Knowledge Collaboration among Physicians in Online Health Communities: A Transactive Memory Perspective. Int. J. Inf. Manag. 2019, 49, 13–33. [Google Scholar] [CrossRef]
- Li, J.; Wu, H.; Deng, Z.; Lu, N.; Evans, R.; Xia, C. How Professional Capital and Team Heterogeneity Affect the Demands of Online Team-Based Medical Service. BMC Med. Inf. Decis. Mak. 2019, 19, 119. [Google Scholar] [CrossRef] [PubMed]
- Guchait, P. The Mediating Effect of Team Engagement between Team Cognitions and Team Outcomes in Service-Management Teams. J. Hosp. Tour. Res. 2016, 40, 139–161. [Google Scholar] [CrossRef]
- Sharma, A.; Bhatnagar, J. Emergence of Team Engagement under Time Pressure: Role of Team Leader and Team Climate. Team Perform. Manag. Int. J. 2017, 23, 171–185. [Google Scholar] [CrossRef]
- Wang, S.; Zhang, X.; Meng, F. What Leads to Effective Online Physician-Patient Communication? The Power of Convergence. In Proceedings of the PACIS 2023, Nanchang, China, 8–12 July 2023; p. 189. [Google Scholar]
- Cao, Q.; Duan, W.; Gan, Q. Exploring Determinants of Voting for the “Helpfulness” of Online User Reviews: A Text Mining Approach. Decis. Support Syst. 2011, 50, 511–521. [Google Scholar] [CrossRef]
- Halder, S.; Tiwari, R.; Sprague, A. Information Extraction from Spam Emails Using Stylistic and Semantic Features to Identify Spammers. In Proceedings of the 2011 IEEE International Conference on Information Reuse & Integration, Las Vegas, NV, USA, 3–5 August 2011; pp. 104–107. [Google Scholar]
- Miller, C.H.; Lane, L.T.; Deatrick, L.M.; Young, A.M.; Potts, K.A. Psychological Reactance and Promotional Health Messages: The Effects of Controlling Language, Lexical Concreteness, and the Restoration of Freedom. Hum. Commun. Res. 2007, 33, 219–240. [Google Scholar] [CrossRef]
- Peng, C.-H.; Yin, D.; Zhang, H. More than Words in Medical Question-and-Answer Sites: A Content–Context Congruence Perspective. Inf. Syst. Res. 2020, 31, 913–928. [Google Scholar] [CrossRef]
- Huang, Q.; Liu, H.; Zhong, X. The Impact of Transactive Memory Systems on Team Performance. Inf. Technol. People 2013, 26, 191–212. [Google Scholar] [CrossRef]
- Deng, Z.; Fan, G.; Deng, Z.; Wang, B. Why Doctors Participate in Teams of Online Health Communities? A Social Identity and Brand Resource Perspective. Inf. Syst. Front. 2023. [Google Scholar] [CrossRef]
- Liu, H.; Perera, S.C.; Wang, J.-J.; Leonhardt, J.M. Physician Engagement in Online Medical Teams: A Multilevel Investigation. J. Bus. Res. 2023, 157, 113588. [Google Scholar] [CrossRef]
- Du, W.; Liu, W.; Guo, X.; Vogel, D. How Team Diversity Influences Online Medical Team Service Performance Through Shared Leadership: An Input–Process–Output Perspective. Group. Decis. Negot. 2023, 33, 27–54. [Google Scholar] [CrossRef]
- Liu, X.; Chen, M.; Li, J.; Ma, L. How to Manage Diversity and Enhance Team Performance: Evidence from Online Doctor Teams in China. Int. J. Environ. Res. Public Health 2019, 17, 48. [Google Scholar] [CrossRef] [PubMed]
- Costa, P.L.; Passos, A.M.; Bakker, A.B. Direct and Contextual Influence of Team Conflict on Team Resources, Team Work Engagement, and Team Performance. Negot. Confl. Man. Res. 2015, 8, 211–227. [Google Scholar] [CrossRef]
- Tims, M.; Bakker, A.B.; Derks, D.; van Rhenen, W. Job Crafting at the Team and Individual Level: Implications for Work Engagement and Performance. Group Organ. Manag. 2013, 38, 427–454. [Google Scholar] [CrossRef]
- Navajas-Romero, V.; Ceular-Villamandos, N.; Pérez-Priego, M.A.; Caridad-López Del Río, L. Sustainable Human Resource Management the Mediating Role between Work Engagement and Teamwork Performance. PLoS ONE 2022, 17, e0271134. [Google Scholar] [CrossRef]
- Rosell, L.; Alexandersson, N.; Hagberg, O.; Nilbert, M. Benefits, Barriers and Opinions on Multidisciplinary Team Meetings: A Survey in Swedish Cancer Care. BMC Health Serv. Res. 2018, 18, 249. [Google Scholar] [CrossRef] [PubMed]
- Clarke, D.; Forster, A. Improving Post-Stroke Recovery: The Role of the Multidisciplinary Health Care Team. J. Multidiscip. Healthc. 2015, 8, 433–442. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhang, X.; Liu, L.; Lai, K. Does Voice Matter? Investigating Patient Satisfaction on Mobile Health Consultation. Inf. Process. Manag. 2023, 60, 103362. [Google Scholar] [CrossRef]
- Jiang, S. How Does Online Patient–Provider Communication Heal? Examining the Role of Patient Satisfaction and Communication Experience in China. Health Commun. 2019, 34, 1637–1644. [Google Scholar] [CrossRef] [PubMed]
- Kostagiolas, P.; Milkas, A.; Kourouthanassis, P.; Dimitriadis, K.; Tsioufis, K.; Tousoulis, D.; Niakas, D. The Impact of Health Information Needs’ Satisfaction of Hypertensive Patients on Their Clinical Outcomes. Aslib J. Inf. Manag. 2020, 73, 43–62. [Google Scholar] [CrossRef]
- Shirley, E.D.; Sanders, J.O. Patient Satisfaction: Implications and Predictors of Success. J. Bone Jt. Surg.-Am. Vol. 2013, 95, e69. [Google Scholar] [CrossRef] [PubMed]
- Bre’dart, A.; Bouleuc, C.; Dolbeault, S. Doctor-Patient Communication and Satisfaction with Care in Oncology. Curr. Opin. Oncol. 2005, 17, 351–354. [Google Scholar] [CrossRef] [PubMed]
- King, A.; Hoppe, R.B. “Best Practice” for Patient-Centered Communication: A Narrative Review. J. Grad. Med. Educ. 2013, 5, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Wrench, J.S.; Booth-Butterfield, M. Increasing Patient Satisfaction and Compliance: An Examination of Physician Humor Orientation, Compliance-gaining Strategies, and Perceived Credibility. Commun. Q. 2003, 51, 482–503. [Google Scholar] [CrossRef]
- Wu, H.; Lu, N. Service Provision, Pricing, and Patient Satisfaction in Online Health Communities. Int. J. Med. Inform. 2018, 110, 77–89. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Guo, X.; Wu, T. Exploring the Influence of the Online Physician Service Delivery Process on Patient Satisfaction. Decis. Support Syst. 2015, 78, 113–121. [Google Scholar] [CrossRef]
- Liu, Y.; Ren, C.; Shi, D.; Li, K.; Zhang, X. Evaluating the Social Value of Online Health Information for Third-Party Patients: Is Uncertainty Always Bad? Inf. Process. Manag. 2020, 57, 102259. [Google Scholar] [CrossRef]
- Costa, P.L.; Passos, A.M.; Bakker, A.B. Team Work Engagement: A Model of Emergence. J. Occupat. Organ. Psychol. 2014, 87, 414–436. [Google Scholar] [CrossRef]
- Spurgeon, P.; Clark, J.; Wathes, R. Medical Engagement and Improving Quality of Care. Future Hosp. J. 2015, 2, 199–202. [Google Scholar] [CrossRef] [PubMed]
- Rahmadani, V.G.; Schaufeli, W.B.; Stouten, J.; Zhang, Z.; Zulkarnain, Z. Engaging Leadership and Its Implication for Work Engagement and Job Outcomes at the Individual and Team Level: A Multi-Level Longitudinal Study. Int. J. Environ. Res. Public Health 2020, 17, 776. [Google Scholar] [CrossRef]
- Shin, Y.; Hur, W.-M.; Choi, W.-H. Coworker Support as a Double-Edged Sword: A Moderated Mediation Model of Job Crafting, Work Engagement, and Job Performance. Int. J. Hum. Resour. Manag. 2020, 31, 1417–1438. [Google Scholar] [CrossRef]
- Hansen, J.; Wänke, M. Truth from Language and Truth from Fit: The Impact of Linguistic Concreteness and Level of Construal on Subjective Truth. Pers. Soc. Psychol. Bull. 2010, 36, 1576–1588. [Google Scholar] [CrossRef] [PubMed]
- Larrimore, L.; Jiang, L.; Larrimore, J.; Markowitz, D.; Gorski, S. Peer to Peer Lending: The Relationship between Language Features, Trustworthiness, and Persuasion Success. J. Appl. Commun. Res. 2011, 39, 19–37. [Google Scholar] [CrossRef]
- Williams, A.; Giles, H.; Coupland, N.; Dalby, M.; Manasse, H. The Communicative Contexts of Elderly Social Support and Health: A Theoretical Model. Health Commun. 1990, 2, 123–143. [Google Scholar] [CrossRef]
- Farzadnia, S.; Giles, H. Patient-Provider Health Interactions: A Communication Accommodation Theory Perspective. Int. J. Soc. Cult. Lang. 2015, 3, 17–34. [Google Scholar]
- Hojat, M.; Louis, D.Z.; Markham, F.W.; Wender, R.; Rabinowitz, C.; Gonnella, J.S. Physicians’ Empathy and Clinical Outcomes for Diabetic Patients. Acad. Med. 2011, 86, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.S.; Kaplowitz, S.; Johnston, M.V. The Effects of Physician Empathy on Patient Satisfaction and Compliance. Eval. Health Prof. 2004, 27, 237–251. [Google Scholar] [CrossRef]
- Horwitz, S.K.; Horwitz, I.B. The Effects of Team Diversity on Team Outcomes: A Meta-Analytic Review of Team Demography. J. Manag. 2007, 33, 987–1015. [Google Scholar] [CrossRef]
- Mangone, L.; Marinelli, F.; Bisceglia, I.; Braghiroli, M.B.; Mastrofilippo, V.; Pezzarossi, A.; Morabito, F.; Aguzzoli, L.; Mandato, V.D. Optimizing Outcomes through a Multidisciplinary Team Approach in Endometrial Cancer. Healthcare 2024, 12, 64. [Google Scholar] [CrossRef] [PubMed]
- Peters, L.; Karren, R.J. An Examination of the Roles of Trust and Functional Diversity on Virtual Team Performance Ratings. Group Organ. Manag. 2009, 34, 479–504. [Google Scholar] [CrossRef]
- Ali, A.; Wang, H.; Khan, A.N. Mechanism to Enhance Team Creative Performance through Social Media: A Transactive Memory System Approach. Comput. Hum. Behav. 2019, 91, 115–126. [Google Scholar] [CrossRef]
- Bhandar, M.; Pan, S.; Tan, B.C.Y. Towards Understanding the Roles of Social Capital in Knowledge Integration: A Case Study of a Collaborative Information Systems Project. J. Am. Soc. Inf. Sci. 2007, 58, 263–274. [Google Scholar] [CrossRef]
- Brysbaert, M.; Warriner, A.B.; Kuperman, V. Concreteness Ratings for 40 Thousand Generally Known English Word Lemmas. Behav. Res. 2014, 46, 904–911. [Google Scholar] [CrossRef] [PubMed]
- Cousins, K.A.Q.; Ash, S.; Olm, C.A.; Grossman, M. Longitudinal Changes in Semantic Concreteness in Semantic Variant Primary Progressive Aphasia (svPPA). eNeuro 2018, 5, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Boyd, R.; Ashokkumar, A.; Seraj, S.; Pennebaker, J. The Development and Psychometric Properties of LIWC-22; University of Texas at Austin: Austin, TX, USA, 2022. [Google Scholar]
- Dekker, J.; Karchoud, J.; Braamse, A.M.J.; Buiting, H.; Konings, I.R.H.M.; van Linde, M.E.; Schuurhuizen, C.S.E.W.; Sprangers, M.A.G.; Beekman, A.T.F.; Verheul, H.M.W. Clinical Management of Emotions in Patients with Cancer: Introducing the Approach “Emotional Support and Case Finding”. Transl. Behav. Med. 2020, 10, 1399–1405. [Google Scholar] [CrossRef]
- Qiao, W.; Yan, Z.; Wang, X. Join or Not: The Impact of Physicians’ Group Joining Behavior on Their Online Demand and Reputation in Online Health Communities. Inf. Process. Manag. 2021, 58, 102634. [Google Scholar] [CrossRef]
| Variable | N | Mean | Std. Dev. | Min | Median | Max |
|---|---|---|---|---|---|---|
| Patient satisfaction | 92,946 | 0.971 | 1.907 | 0.000 | 0.000 | 54.90 |
| OMT engagement | 92,946 | 0.349 | 0.201 | 0.043 | 0.333 | 1.000 |
| Language concreteness | 92,946 | 1.445 | 0.449 | 0.114 | 1.388 | 4.969 |
| Emotional intensity | 92,946 | 0.087 | 0.054 | 0.000 | 0.081 | 0.615 |
| Multiple specializations | 92,946 | 0.104 | 0.305 | 0.000 | 0.000 | 1.000 |
| Sex | 92,946 | 0.448 | 0.497 | 0.000 | 0.000 | 1.000 |
| Age | 92,946 | 35.44 | 20.86 | 0.500 | 34.00 | 100.0 |
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| Variables | Language Concreteness | Language Concreteness | Language Concreteness | Emotional Intensity | Emotional Intensity | Emotional Intensity |
| OMT engagement | 0.025 * | 0.022 * | −0.005 *** | −0.004 ** | ||
| (0.013) | (0.013) | (0.002) | (0.002) | |||
| Multiple specializations | −0.005 | −0.448 *** | −0.005 *** | −0.082 *** | ||
| (0.006) | (0.008) | (0.001) | (0.001) | |||
| Multiple specializations * Language concreteness | 1.412 *** | |||||
| (0.016) | ||||||
| Multiple specialization * Emotional intensity | 0.915 *** | |||||
| (0.012) | ||||||
| Sex | −0.005 | −0.004 | −0.004 | −0.000 | −0.000 | 0.000 |
| (0.003) | (0.003) | (0.003) | (0.000) | (0.000386) | (0.000) | |
| Age | 0.001 *** | 0.001 *** | 0.001 *** | −7.46 × 10−5 *** | −7.60 × 10−5 *** | −7.27 × 10−5 *** |
| (0.000) | (0.000) | (9.77 × 10−5) | (1.28 × 10−5) | (1.28 × 10−5) | (1.24 × 10−5) | |
| Constant | 1.427 *** | 1.419 *** | 1.417 *** | 0.090 *** | 0.092 *** | 0.092 *** |
| (0.004) | (0.006) | (0.006) | (0.001) | (0.001) | (0.001) | |
| Team fixed effects | YES | YES | YES | YES | YES | YES |
| No. of teams | 2122 | 2122 | 2122 | 2122 | 2122 | 2122 |
| Observations | 92,946 | 92,946 | 92,946 | 92,946 | 92,946 | 92,946 |
| R-squared | 0.199 | 0.199 | 0.262 | 0.122 | 0.123 | 0.179 |
| (1) | (2) | |
|---|---|---|
| Variables | Patient Satisfaction | Patient Satisfaction |
| Language concreteness | 0.097 *** | |
| (0.014) | ||
| Emotional intensity | 2.624 *** | |
| (0.111) | ||
| Sex | 0.010 | 0.012 |
| (0.013) | (0.013) | |
| Age | −0.000 | −5.28 × 10−5 |
| (0.000) | (0.000) | |
| Constant | 0.973 *** | 0.598 *** |
| (0.017) | (0.027) | |
| Team fixed effects | YES | YES |
| No. of teams | 2122 | 2122 |
| Observations | 92,946 | 92,946 |
| R-squared | 0.225 | 0.230 |
| Paths | Direct Effect | 95%CI | Indirect Effect | 95%CI |
|---|---|---|---|---|
| OMT engagement—Language concreteness—Patient satisfaction | 1.360 | (1.271, 1.453) | 0.013 | (0.009, 0.017) |
| OMT engagement—Emotional intensity—Patient satisfaction | 1.394 | (1.304, 1.489) | −0.023 | (−0.028, −0.017) |
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| Variables | Language Concreteness | Language Concreteness | Language Concreteness | Emotional Intensity | Emotional Intensity | Emotional Intensity |
| OMT engagement | 0.049 *** | 0.028 *** | −0.012 *** | −0.011 *** | ||
| (0.008) | (0.007) | (0.001) | (0.001) | |||
| Multiple specializations | −0.010 * | −0.537 *** | −0.001 ** | −0.085 *** | ||
| (0.005) | (0.007) | (0.001) | (0.001) | |||
| Multiple specializations * Language concreteness | 1.617 *** | |||||
| (0.016) | ||||||
| Multiple specializations * Emotional intensity | 0.999 *** | |||||
| (0.012) | ||||||
| Sex | 0.010 *** | 0.010 *** | 0.005 * | −0.001 ** | −0.001 ** | −0.000 |
| (0.003) | (0.003) | (0.003) | (0.000) | (0.000) | (0.000) | |
| Age | 0.001 *** | 0.001 *** | 0.001 *** | 0.000 *** | 0.000 *** | 9.85 × 10−5 *** |
| (7.06 × 10−5) | (7.06 × 10−5) | (6.71× 10−5) | (8.52 × 10−6) | (8.51× 10−6) | (8.19 × 10−6) | |
| Constant | 1.393 *** | 1.376 *** | 1.390 *** | 0.084 *** | 0.088 *** | 0.088 *** |
| (0.003) | (0.004) | (0.004) | (0.000) | (0.001) | (0.000) | |
| Observations | 92,946 | 92,946 | 92,946 | 92,946 | 92,946 | 92,946 |
| R-squared | 0.004 | 0.005 | 0.102 | 0.002 | 0.004 | 0.078 |
| (1) | (2) | |
|---|---|---|
| Variables | Patient Satisfaction | Patient Satisfaction |
| Language concreteness | 0.125 *** | |
| (0.014) | ||
| Emotional intensity | 2.275 *** | |
| (0.117) | ||
| Sex | 0.067 *** | 0.068 *** |
| (0.013) | (0.013) | |
| Age | −0.002 *** | −0.002 *** |
| (0.000) | (0.000) | |
| Constant | 1.005 *** | 0.640 *** |
| (0.014) | (0.025) | |
| Observations | 92,946 | 92,946 |
| R-squared | 0.001 | 0.006 |
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| Variables | Language Concreteness | Language Concreteness | Language Concreteness | Emotional Intensity | Emotional Intensity | Emotional Intensity |
| OMT engagement | 0.061 *** | 0.028 *** | −0.006 *** | −0.006 *** | ||
| (0.011) | (0.011) | (0.001) | (0.001) | |||
| Multiple specializations | −0.012 ** | −0.535 *** | −0.003 *** | −0.087 *** | ||
| (0.006) | (0.007) | (0.001) | (0.001) | |||
| Multiple specializations * | 1.611 *** | |||||
| Language concreteness | (0.016) | |||||
| Multiple specializations * | 0.994 *** | |||||
| Emotional intensity | (0.012) | |||||
| Sex | 0.002 | 0.002 | −0.001 | −0.001 *** | −0.001 *** | −0.001 ** |
| (0.003) | (0.003) | (0.003) | (0.000) | (0.000) | (0.000) | |
| Age | 0.001 *** | 0.001 *** | 0.001 *** | 0.000 *** | 9.88 × 10−5 *** | 9.62 × 10−5 *** |
| (7.04 × 10−5) | (7.04 × 10−5) | (6.69 × 10−5) | (8.52 × 10−6) | (8.52 × 10−6) | (8.20 × 10−6) | |
| Price | −0.000 *** | −0.000 *** | −0.000 *** | −6.90 × 10−5 *** | −5.92 × 10−6 *** | −4.02 × 10−6 ** |
| (1.70 × 10−5) | (1.71 × 10−5) | (1.62 × 10−5) | (2.06 × 10−6) | (2.07 × 10−6) | (1.99 × 10−6) | |
| Team size | 0.002 *** | 0.005 *** | 0.004 *** | 0.001 *** | 0.001 *** | 0.001 *** |
| (0.001) | (0.001) | (0.001) | (7.29 × 10−5) | (0.000) | (9.89 × 10−5) | |
| Leader response | 0.038 *** | 0.035 *** | 0.041 *** | 0.000 | 0.001 ** | 0.001 ** |
| (0.003) | (0.003) | (0.003) | (0.000) | (0.000) | (0.000) | |
| Tenure | −0.022 *** | −0.022 *** | −0.022 *** | 0.002 *** | 0.002 *** | 0.002 *** |
| (0.001) | (0.001) | (0.001) | (0.000) | (0.000) | (0.000) | |
| Constant | 1.475 *** | 1.443 *** | 1.455 *** | 0.072 *** | 0.075 *** | 0.076 *** |
| (0.007) | (0.009) | (0.009) | (0.001) | (0.001) | (0.001) | |
| Observations | 92,946 | 92,946 | 92,946 | 92,946 | 92,946 | 92,946 |
| R-squared | 0.013 | 0.014 | 0.110 | 0.006 | 0.007 | 0.080 |
| (1) | (2) | |
|---|---|---|
| Variables | Patient Satisfaction | Patient Satisfaction |
| Language concreteness | 0.124 *** | |
| (0.014) | ||
| Emotional intensity | 2.400 *** | |
| (0.116) | ||
| Sex | 0.094 *** | 0.097 *** |
| (0.013) | (0.013) | |
| Age | −0.002 *** | −0.003 *** |
| (0.000) | (0.000) | |
| Price | 0.002 *** | 0.002 *** |
| (7.19 × 10−5) | (7.18 × 10−5) | |
| Team size | −0.044 *** | −0.047 *** |
| (0.003) | (0.003) | |
| Leader response | 0.383 *** | 0.377 *** |
| (0.015) | (0.014) | |
| Tenure | 0.008 | 0.006 |
| (0.005) | (0.005) | |
| Constant | 0.751 *** | 0.396 *** |
| (0.031) | (0.038) | |
| Observations | 92,946 | 92,946 |
| R-squared | 0.017 | 0.023 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, S.; Zhang, X. Exploring the Impact of Online Medical Team Engagement on Patient Satisfaction: A Semantic Features Perspective. Healthcare 2024, 12, 1113. https://doi.org/10.3390/healthcare12111113
Wang S, Zhang X. Exploring the Impact of Online Medical Team Engagement on Patient Satisfaction: A Semantic Features Perspective. Healthcare. 2024; 12(11):1113. https://doi.org/10.3390/healthcare12111113
Chicago/Turabian StyleWang, Siqi, and Xiaofei Zhang. 2024. "Exploring the Impact of Online Medical Team Engagement on Patient Satisfaction: A Semantic Features Perspective" Healthcare 12, no. 11: 1113. https://doi.org/10.3390/healthcare12111113
APA StyleWang, S., & Zhang, X. (2024). Exploring the Impact of Online Medical Team Engagement on Patient Satisfaction: A Semantic Features Perspective. Healthcare, 12(11), 1113. https://doi.org/10.3390/healthcare12111113






