Evaluating the Impact of a Virtual Health Coaching Lifestyle Program on Weight Loss after Sleeve Gastrectomy: A Prospective Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Virtual Health Coaching Program
2.3. Data Variables
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rosen, H. Is Obesity A Disease or A Behavior Abnormality? Did the AMA Get It Right? Mo. Med. 2014, 111, 104–108. [Google Scholar]
- Anekwe, C.V.; Jarrell, A.R.; Townsend, M.J.; Gaudier, G.I.; Hiserodt, J.M.; Stanford, F.C. Socioeconomics of Obesity. Curr. Obes. Rep. 2020, 9, 272–279. [Google Scholar] [CrossRef]
- Sarwer, D.B.; Grilo, C.M. Obesity: Psychosocial and behavioral aspects of a modern epidemic: Introduction to the special issue. Am. Psychol. 2020, 75, 135–138. [Google Scholar] [CrossRef]
- Tanamas, S.K.; Shaw, J.E.; Backholer, K.; Magliano, D.J.; Peeters, A. Twelve-year weight change, waist circumference change and incident obesity: The Australian diabetes, obesity and lifestyle study. Obes. Silver Spring Md. 2014, 22, 1538–1545. [Google Scholar] [CrossRef]
- Cassin, S.E.; Sockalingam, S.; Du, C.; Wnuk, S.; Hawa, R.; Parikh, S.V. A pilot randomized controlled trial of telephone-based cognitive behavioural therapy for preoperative bariatric surgery patients. Behav. Res. Ther. 2016, 80, 17–22. [Google Scholar] [CrossRef]
- Popescu, A.L.; Ioniţa-Radu, F.; Jinga, M.; Gavrilă, A.I.; Săvulescu, F.A.; Fierbinţeanu-Braticevici, C. Laparoscopic sleeve gastrectomy and gastroesophageal reflux. Rom. J. Intern. Med. 2018, 56, 227–232. [Google Scholar] [CrossRef]
- Aderinto, N.; Olatunji, G.; Kokori, E.; Olaniyi, P.; Isarinade, T.; Yusuf, I.A. Recent advances in bariatric surgery: A narrative review of weight loss procedures. Ann. Med. Surg. 2023, 85, 6091–6104. [Google Scholar] [CrossRef]
- Kheirvari, M.; Dadkhah Nikroo, N.; Jaafarinejad, H.; Farsimadan, M.; Eshghjoo, S.; Hosseini, S.; Anbara, T. The advantages and disadvantages of sleeve gastrectomy; clinical laboratory to bedside review. Heliyon 2020, 6, e03496. [Google Scholar] [CrossRef]
- Peterli, R.; Wölnerhanssen, B.K.; Peters, T.; Vetter, D.; Kröll, D.; Borbély, Y.; Schultes, B.; Beglinger, C.; Drewe, J.; Schiesser, M.; et al. Effect of Laparoscopic Sleeve Gastrectomy vs Laparoscopic Roux-en-Y Gastric Bypass on Weight Loss in Patients With Morbid Obesity: The SM-BOSS Randomized Clinical Trial. Jama 2018, 319, 255–265. [Google Scholar] [CrossRef]
- Gould, J.C.; Beverstein, G.; Reinhardt, S.; Garren, M.J. Impact of routine and long-term follow-up on weight loss after laparoscopic gastric bypass. Surg. Obes. Relat. Dis. 2007, 3, 627–630. [Google Scholar] [CrossRef]
- Vidal, P.; Ramón, J.M.; Goday, A.; Parri, A.; Crous, X.; Trillo, L.; Pera, M.; Grande, L. Lack of adherence to follow-up visits after bariatric surgery: Reasons and outcome. Obes. Surg. 2014, 24, 179–183. [Google Scholar] [CrossRef]
- Assakran, B.S.; Widyan, A.M.; Alhumaidan, N.A.; Alharbi, F.A.; Alhnaya, M.A.; Aljabali, A.A.; Aleid, M.A. Dietary assessment and patient-perspective reasons for poor adherence to diet and exercise post bariatric surgery. BMC Res. Notes 2020, 13, 526. [Google Scholar] [CrossRef]
- Park, S.; Kim, S.; Kim, S.; Shin, A.R.; Park, Y. Nutritional Intervention for a Patient With Sleeve Gastrectomy. Clin. Nutr. Res. 2023, 12, 177–183. [Google Scholar] [CrossRef]
- Freire, R.H.; Borges, M.C.; Alvarez-Leite, J.I.; Toulson Davisson Correia, M.I. Food quality, physical activity, and nutritional follow-up as determinant of weight regain after Roux-en-Y gastric bypass. Nutrition 2012, 28, 53–58. [Google Scholar] [CrossRef]
- Kushner, R.F.; Sorensen, K.W. Prevention of Weight Regain Following Bariatric Surgery. Curr. Obes. Rep. 2015, 4, 198–206. [Google Scholar] [CrossRef]
- Sherf Dagan, S.; Goldenshluger, A.; Globus, I.; Schweiger, C.; Kessler, Y.; Kowen Sandbank, G.; Ben-Porat, T.; Sinai, T. Nutritional Recommendations for Adult Bariatric Surgery Patients: Clinical Practice. Adv. Nutr. 2017, 8, 382–394. [Google Scholar] [CrossRef]
- Johnson, K.E.; Alencar, M.K.; Coakley, K.E.; Swift, D.L.; Cole, N.H.; Mermier, C.M.; Kravitz, L.; Amorim, F.T.; Gibson, A.L. Telemedicine-Based Health Coaching Is Effective for Inducing Weight Loss and Improving Metabolic Markers. Telemed. J. e-Health 2019, 25, 85–92. [Google Scholar] [CrossRef]
- Pottle, J. Virtual reality and the transformation of medical education. Future Healthc. J. 2019, 6, 181–185. [Google Scholar] [CrossRef]
- Ju, H.; Kang, E.; Kim, Y.; Ko, H.; Cho, B. The Effectiveness of a Mobile Health Care App and Human Coaching Program in Primary Care Clinics: Pilot Multicenter Real-World Study. JMIR mhealth uhealth 2022, 10, e34531. [Google Scholar] [CrossRef]
- Khanijahani, A.; Akinci, N.; Quitiquit, E. A Systematic Review of the Role of Telemedicine in Blood Pressure Control: Focus on Patient Engagement. Curr. Hypertens. Rep. 2022, 24, 247–258. [Google Scholar] [CrossRef]
- Li, Z.; Pan, Y.; Zhang, Y.; Qin, J.; Lei, X. Dietary experiences after bariatric surgery in patients with obesity: A qualitative systematic review. Obes. Surg. 2022, 32, 2023–2034. [Google Scholar] [CrossRef]
- Bradley, L.E.; Forman, E.M.; Kerrigan, S.G.; Goldstein, S.P.; Butryn, M.L.; Thomas, J.G.; Herbert, J.D.; Sarwer, D.B. Project HELP: A Remotely Delivered Behavioral Intervention for Weight Regain after Bariatric Surgery. Obes. Surg. 2017, 27, 586–598. [Google Scholar] [CrossRef]
- Alencar, M.K.; Johnson, K.; Mullur, R.; Gray, V.; Gutierrez, E.; Korosteleva, O. The efficacy of a telemedicine-based weight loss program with video conference health coaching support. J. Telemed. Telecare 2019, 25, 151–157. [Google Scholar] [CrossRef]
- Ufholz, K.; Bhargava, D. A Review of Telemedicine Interventions for Weight Loss. Curr. Cardiovasc. Risk Rep. 2021, 15, 17. [Google Scholar] [CrossRef]
- Calcaterra, V.; Verduci, E.; Vandoni, M.; Rossi, V.; Di Profio, E.; Carnevale Pellino, V.; Tranfaglia, V.; Pascuzzi, M.C.; Borsani, B.; Bosetti, A.; et al. Telehealth: A Useful Tool for the Management of Nutrition and Exercise Programs in Pediatric Obesity in the COVID-19 Era. Nutrients 2021, 13, 3689. [Google Scholar] [CrossRef]
- Watson, A.; Bickmore, T.; Cange, A.; Kulshreshtha, A.; Kvedar, J. An internet-based virtual coach to promote physical activity adherence in overweight adults: Randomized controlled trial. J. Med. Internet Res. 2012, 14, e1. [Google Scholar] [CrossRef]
- Johnson, K.; Gutierrez, E.; Dionicio, P.; McConnell, J.; Sauls, R.; Alencar, M. Telehealth-Based Health Coaching Produces Significant Weight Loss over 12 Months in a Usual Care Setting. Int. Med. Educ. 2022, 1, 79–84. [Google Scholar] [CrossRef]
- Lim, W.X.; Fook-Chong, S.; Lim, J.W.; Gan, W.H. The Outcomes of App-Based Health Coaching to Improve Dietary Behavior Among Nurses in a Tertiary Hospital: Pilot Intervention Study. JMIR Nurs. 2022, 5, e36811. [Google Scholar] [CrossRef]
- Burton, L.; Rush, K.L.; Smith, M.A.; Davis, S.; Rodriguez Echeverria, P.; Suazo Hidalgo, L.; Görges, M. Empowering Patients Through Virtual Care Delivery: Qualitative Study with Micropractice Clinic Patients and Health Care Providers. JMIR Form. Res. 2022, 6, e32528. [Google Scholar] [CrossRef]
- Markert, C.; Sasangohar, F.; Mortazavi, B.J.; Fields, S. The Use of Telehealth Technology to Support Health Coaching for Older Adults: Literature Review. JMIR Hum. Factors 2021, 8, e23796. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef]
- Williams, A.M.; Bhatti, U.F.; Alam, H.B.; Nikolian, V.C. The role of telemedicine in postoperative care. mHealth 2018, 4, 11. [Google Scholar] [CrossRef]
- Martin, L.R.; Williams, S.L.; Haskard, K.B.; Dimatteo, M.R. The challenge of patient adherence. Ther. Clin. Risk Manag. 2005, 1, 189–199. [Google Scholar]
- Gajarawala, S.N.; Pelkowski, J.N. Telehealth Benefits and Barriers. J. Nurse Pract. JNP 2021, 17, 218–221. [Google Scholar] [CrossRef]
- Sauls, R.; Crowder, S.L.; James, C.; Khimani, F.; Stern, M. Quality of life in the digital age: Young adult hematopoietic stem cell transplantation patients and healthcare providers’ views of telehealth. Support. Care Cancer 2024, 32, 270. [Google Scholar] [CrossRef]
- Gendia, A.; Zyada, A.; Nasir, M.T.; Elfar, M.; Sakr, M.; Rehman, M.U.; Cota, A.; Clark, J. Virtual Reality as a Surgical Care Package for Patients Undergoing Weight Loss Surgery: A Narrative Review of the Impact of an Emerging Technology. Cureus 2022, 14, e29608. [Google Scholar] [CrossRef]
- Alencar, M.; Johnson, K.; Gray, V.; Mullur, R.; Gutierrez, E.; Dionico, P. Telehealth-Based Health Coaching Increases m-Health Device Adherence and Rate of Weight Loss in Obese Participants. Telemed. J. e-Health 2020, 26, 365–368. [Google Scholar] [CrossRef]
- Thom, D.H.; Wolf, J.; Gardner, H.; DeVore, D.; Lin, M.; Ma, A.; Ibarra-Castro, A.; Saba, G. A Qualitative Study of How Health Coaches Support Patients in Making Health-Related Decisions and Behavioral Changes. Ann. Fam. Med. 2016, 14, 509–516. [Google Scholar] [CrossRef]
| Weekly sessions (months 1–3) | Build and maintain rapport Create progress toward 12-month wellness vision Motivational interviewing to support generative moments Discuss nutritional and physical activity goals and progress |
| Biweekly sessions (months 4–6) | Continue maintaining rapport Explore strengths and values to health behavior and change Troubleshoot barriers and highlight strengths Bi-directional feedback with MD |
| Monthly sessions (months 6–12) | Continue maintaining rapport Schedule subsequent health coaching visits Goal setting—monthly Continue reviewing strengths and weaknesses |
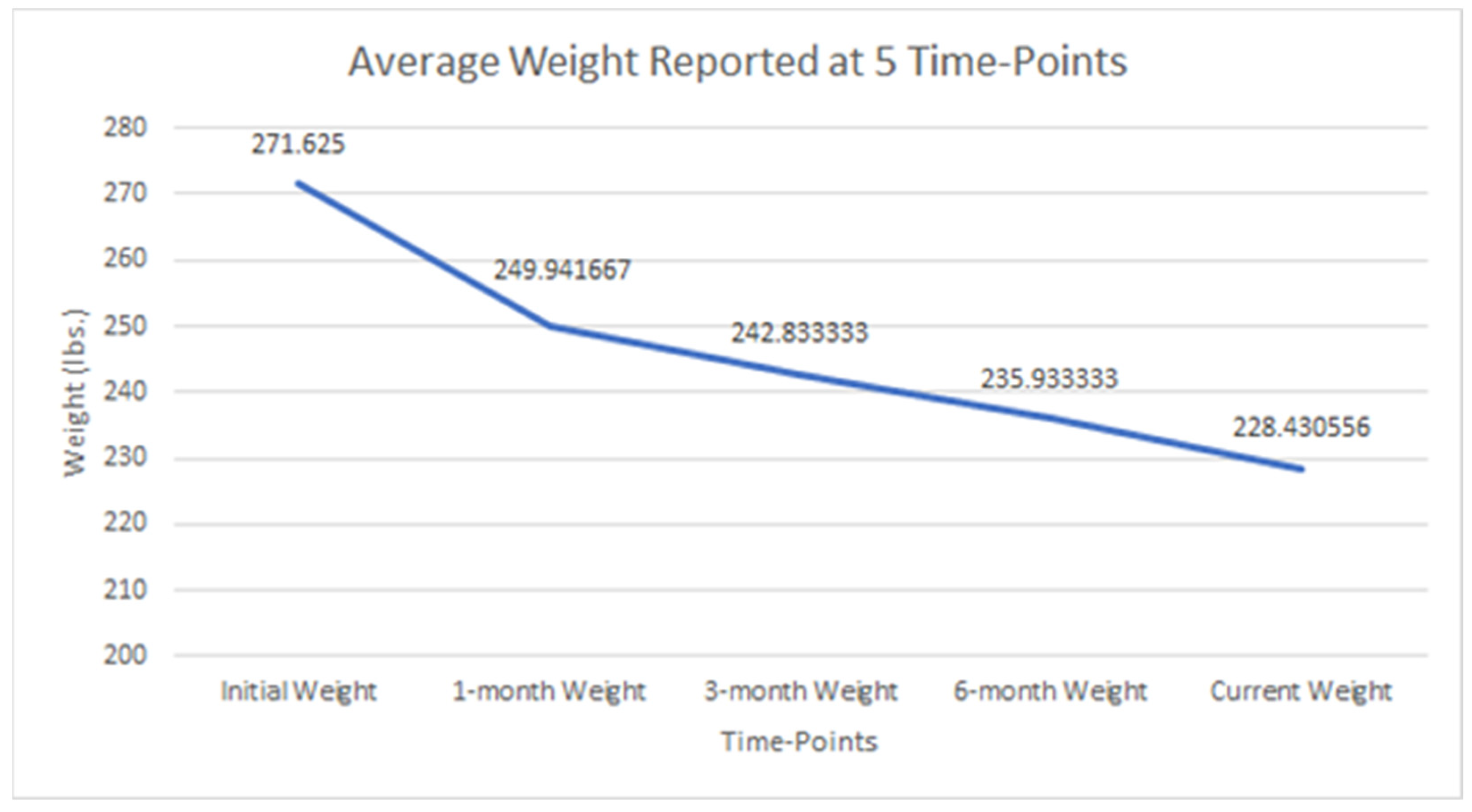
| N = 38 | p Value | |
|---|---|---|
| Age: Mean ± SD [range], years | 52.3 ± 12.9 [24.8–75.1] | |
| Initial BMI: Mean ± SD [range] | 44.5 ± 8.6 [27.9–70.6] | <0.001 * |
| Current BMI: Mean ± SD [range] | 37.1 ± 6.6 [25.7–51.1] | |
| Gender: n (%) Female | 35 (97.0) | |
| Height: Mean ± SD [range], inches | 65.6 ± 2.6 [59–71.2] | |
| Initial Weight: Mean ± SD [range], kg. | 123.3 ± 24.1 [77.1–191.9] | <0.001 * |
| 1-month Weight: Mean ± SD [range], kg. | 113.5 ± 20.6 [75.8.0–163.3] | <0.001 * |
| 3-month Weight: Mean ± SD [range], kg. | 110.1 ± 19.5 [73.5–155.6] | <0.001 * |
| 6-month Weight: Mean ± SD [range], kg. | 106.8 ± 18.8 [72.2–149.2] | <0.001 * |
| Current Weight: Mean ± SD [range], kg. | 102.8± 18.3 [71.2–149.2] | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strauss, K.; Sauls, R.; Alencar, M.K.; Johnson, K.E. Evaluating the Impact of a Virtual Health Coaching Lifestyle Program on Weight Loss after Sleeve Gastrectomy: A Prospective Study. Healthcare 2024, 12, 1256. https://doi.org/10.3390/healthcare12131256
Strauss K, Sauls R, Alencar MK, Johnson KE. Evaluating the Impact of a Virtual Health Coaching Lifestyle Program on Weight Loss after Sleeve Gastrectomy: A Prospective Study. Healthcare. 2024; 12(13):1256. https://doi.org/10.3390/healthcare12131256
Chicago/Turabian StyleStrauss, Kristina, Rachel Sauls, Michelle K. Alencar, and Kelly E. Johnson. 2024. "Evaluating the Impact of a Virtual Health Coaching Lifestyle Program on Weight Loss after Sleeve Gastrectomy: A Prospective Study" Healthcare 12, no. 13: 1256. https://doi.org/10.3390/healthcare12131256





