Exploring Telemedicine Usage Intention Using Technology Acceptance Model and Social Capital Theory
Abstract
:1. Introduction
2. Materials and Methods
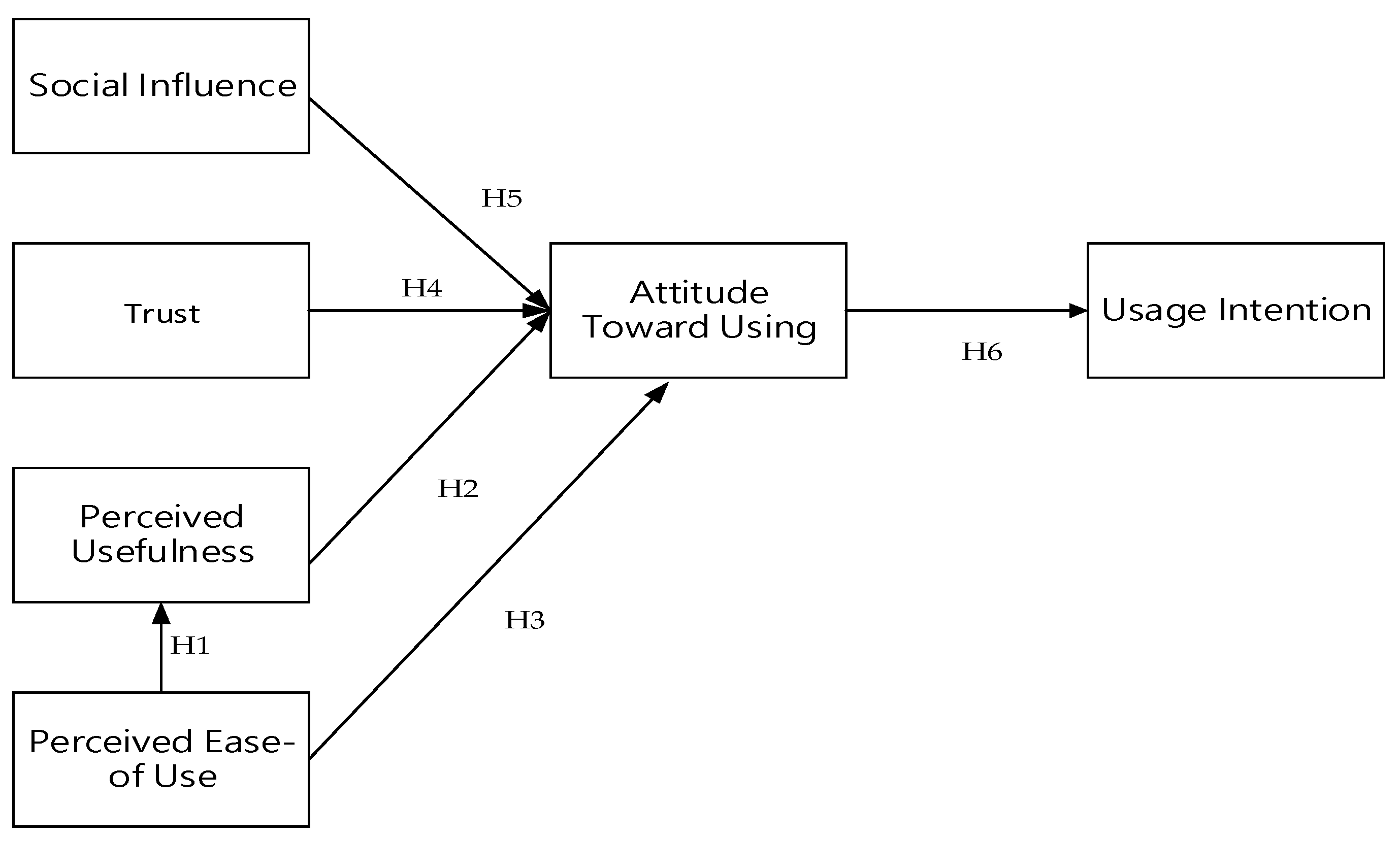
2.1. Theoretical Frameworks and Hypotheses
2.2. Sample Size Determination and Sampling
2.3. Questionnaire Development and Validation
2.4. The Questionnaire Encompassed the following Components
2.5. Handling Missing Data
2.6. Consistency in Telemedicine Platforms
2.7. Ethical Considerations and Data Analysis
2.8. Software Licensing
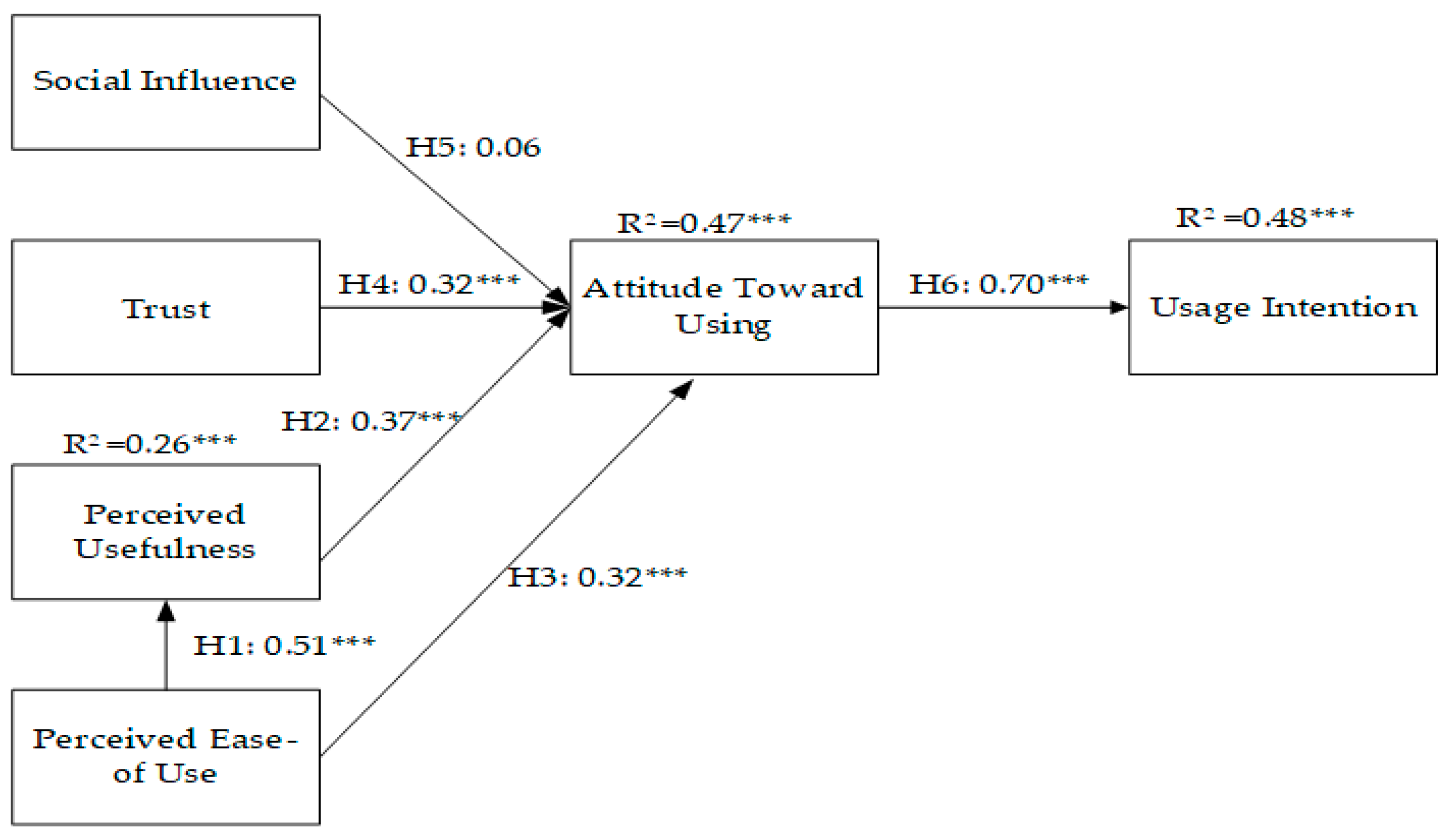
3. Results
4. Discussion and Implication
5. Conclusions
6. Recommendations
7. Limitations and Future Research Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gao, J.; Zheng, P.; Jia, Y.; Chen, H.; Mao, Y.; Chen, S.; Wang, Y.; Fu, H.; Dai, J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 2020, 15, e0231924. [Google Scholar]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed]
- Shachar, C.; Engel, J.; Elwyn, G. Implications for telehealth in a postpandemic future: Regulatory and privacy issues. JAMA 2020, 323, 2375–2376. [Google Scholar] [CrossRef] [PubMed]
- Hollander, J.E.; Carr, B.G. Virtually perfect? Telemedicine for COVID-19. N. Engl. J. Med. 2020, 382, 1679–1681. [Google Scholar] [CrossRef] [PubMed]
- Chuang, M.M.; Lin, C.Y.; Sung, K.T.; Tsai, J.P.; Kuo, J.Y.; Huang, W.H.; Chen, Y.C.; Tsai, C.T.; Su, C.H.; Hou, J.Y.C.; et al. Contemporary Practice in Telemedicine through Telecommunication Technology during COVID-19 Pandemic in Taiwan-A Single Center Experience. Int. J. Gerontol. 2022, 16, 196–201. [Google Scholar]
- Wu, T.C.; Ho, C.T.B. Barriers to telemedicine adoption during the COVID-19 pandemic in Taiwan: Comparison of perceived risks by socioeconomic status correlates. Int. J. Environ. Res. Public Health 2023, 20, 3504. [Google Scholar] [CrossRef] [PubMed]
- Ho, P.H.; Huang, C.C.; Liu, Y.S. Exploring the Key Factors that Affect Patient Willingness to Use Telemedicine. Cheng Ching Med. J. 2021, 17, 27–36. (In Taiwanese) [Google Scholar]
- National Health Insurance Administration. Telemedicine in Response to COVID-19. Available online: https://www.nhi.gov.tw/Content_List.aspx?n=1482911120B73697&topn=787128DAD5F71B1A (accessed on 30 June 2023).
- Tseng, H.M.; Chung, P.J.; Wang, H.H.; Chuang, Y.J. Examining Factors Related to Acceptance of Telemedicine among Taiwan’s Expatriate Workers Living in Shang Hai of China. J. Taiwan Assoc. Med. Inform. 2020, 18, 13–28. (In Taiwanese) [Google Scholar]
- Harst, L.; Lantzsch, H.; Scheibe, M. Theories predicting end-user acceptance of telemedicine use: Systematic review. J. Med. Internet Res. 2019, 21, e13117. [Google Scholar] [CrossRef] [PubMed]
- Holtz, B.; Mitchell, K.; Hirko, K.; Ford, S. Using the Technology Acceptance Model to Characterize Barriers and Opportunities of Telemedicine in Rural Populations: Survey and Interview Study. JMIR. Form. Res. 2022, 6, e35130. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, K.M.; Campbell, R.S.; Fiester, A.; Simpson, R.L.; Hertel, C. Bringing care home: How telemonitoring can expand population health management beyond the hospital. Nurs. Adm. Q. 2014, 38, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Esser, P.E.; Goossens, R.H. A framework for the design of user-centred teleconsulting systems. J. Telemed. Telecare 2009, 15, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Riley, W.T.; Rivera, D.E.; Atienza, A.A.; Nilsen, W.; Allison, S.M.; Mermelstein, R. Health behavior models in the age of mobile interventions: Are our theories up to the task? Transl. Behav. Med. 2011, 1, 53–71. [Google Scholar] [CrossRef] [PubMed]
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Bourdieu, P. The forms of capttal. In Handbook of Theory and Research for the Sociology of Education; Richardson, J., Ed.; Greenwood: New York, NY, USA, 1986; pp. 241–258. [Google Scholar]
- Coleman, J.S. Social capital in the creation of human capital. Am. J. Sociol. 1988, 94, S95–S120. [Google Scholar] [CrossRef]
- Dika, S.L.; Singh, K. Applications of social capital in educational literature: A critical synthesis. Rev. Educ. Res. 2002, 72, 31–60. [Google Scholar] [CrossRef]
- Lin, K.Y.; Lu, H.P. Intention to continue using Facebook fan pages from the perspective of social capital theory. Cyberpsychol. Behav. Soc. Netw. 2011, 14, 565–570. [Google Scholar] [CrossRef] [PubMed]
- Putnam, R. The prosperous community: Social capital and public life. Am. Prospect 1993, 13, 35–42. [Google Scholar]
- Schneider, G.E.; Griffith, W.H.; Knoedler, J.T. The Great Disruption: Human Nature and the Reconstitution of Social Order; The Free Press: New York, NY, USA, 2000. [Google Scholar]
- Baptista, G.; Oliveira, T. Understanding mobile banking: The unified theory of acceptance and use of technology combined with cultural moderators. Comput. Hum. Behav. 2015, 50, 418–430. [Google Scholar] [CrossRef]
- Kissi, J.; Dai, B.; Dogbe, C.S.; Banahene, J.; Ernest, O. Predictive factors of physicians’ satisfaction with telemedicine services acceptance. Health Inform. J. 2020, 26, 1866–1880. [Google Scholar] [CrossRef] [PubMed]
- Naqvi, M.H.A.; Jiang, Y.; Miao, M.; Naqvi, M.H. The effect of social influence, trust, and entertainment value on social media use: Evidence from Pakistan. Cogent. Bus. Manag. 2020, 7, 1723825. [Google Scholar] [CrossRef]
- Mensah, I.K.; Mi, J. Computer self-efficacy and e-government service adoption: The moderating role of age as a demographic factor. Int. J. Public Adm. 2019, 42, 158–167. [Google Scholar] [CrossRef]
- Granić, A.; Marangunić, N. Technology acceptance model in educational context: A systematic literature review. Br. J. Educ. Technol. 2019, 50, 2572–2593. [Google Scholar] [CrossRef]
- Kamal, S.A.; Shafiq, M.; Kakria, P. Investigating acceptance of telemedicine services through an extended technology acceptance model (TAM). Technol. Soc. 2020, 60, 101212. [Google Scholar] [CrossRef]
- Venkatesh, V.; Morris, M.G.; Davis, G.B.; Davis, F.D. User acceptance of information technology: Toward a unified view. MIS Q. 2003, 27, 425–478. [Google Scholar] [CrossRef]
- Lu, J.; Yao, J.E.; Yu, C.S. Personal innovativeness, social influences and adoption of wireless Internet services via mobile technology. J. Strate Inform. Syst. 2005, 14, 245–268. [Google Scholar] [CrossRef]
- Zhou, L.; Bao, J.; Watzlaf, V.; Parmanto, B. Barriers to and facilitators of the use of mobile health apps from a security perspective: Mixed-methods study. JMIR mHealth uHealth 2019, 7, e11223. [Google Scholar] [CrossRef] [PubMed]
- Parra, C.; Jódar-Sánchez, F.; Jiménez-Hernández, M.D.; Vigil, E.; Palomino-García, A.; Moniche-Álvarez, F.; De la Torre Laviana, F.J.; Bonachela, P.; Fernández, F.J.; Cayuela-Domínguez, A.; et al. Development, implementation, and evaluation of a telemedicine service for the treatment of acute stroke patients: Tele Stroke. Interact. J. Med. Res. 2012, 1, e2163. [Google Scholar] [CrossRef] [PubMed]
- Kao, M.Y.; Wu, C.I. Self-rated health and social capital: Cross-national analysis of international social survey data. Taiwan J. Public Health 2020, 39, 509–521. (In Taiwanese) [Google Scholar]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User acceptance of computer technology: A comparison of two theoretical models. Manag. Sci. 1989, 35, 982–1003. [Google Scholar] [CrossRef]
- Chakraborty, R.; Lee, J.; Bagchi-Sen, S.; Upadhyaya, S.; Rao, H.R. Online shopping intention in the context of data breach in online retail stores: An examination of older and younger adults. Decis. Support Syst. 2016, 83, 47–56. [Google Scholar] [CrossRef]
- Kim, H.W.; Chan, H.C.; Gupta, S. Value-based adoption of mobile internet: An empirical investigation. Decis. Support Syst. 2007, 43, 111–126. [Google Scholar] [CrossRef]
- Martins, C.; Oliveira, T.; Popovi, A. Understanding the Internet banking adoption: A unified theory of acceptance and use of technology and perceived risk application. Int. J. Inf. Manag. 2014, 34, 1–13. [Google Scholar] [CrossRef]
- Smith, R.; Deitz, G.; Royne, M.B.; Hansen, J.D.; Grünhagen, M.; Witte, C. Cross-cultural examination of online shopping behavior: A comparison of Norway, Germany, and the United States. J. Bus. Res. 2013, 66, 328–335. [Google Scholar] [CrossRef]
- Scherer, R.; Siddiq, F.; Tondeur, J. The technology acceptance model (TAM): A meta-analytic structural equation modeling approach to explaining teachers’ adoption of digital technology in education. Comput. Edu. 2019, 128, 13–35. [Google Scholar] [CrossRef]
- Harman, H.H. Modern Factor Analysis, 3rd ed.; The University of Chicago Press: Chicago, IL, USA, 1976. [Google Scholar]
- Podsakoff, P.M.; MacKenzie, S.B.; Lee, J.Y.; Podsakoff, N.P. Common method biases in behavioral research: A critical review of the literature and recommended remedies. J. Appl. Psychol. 2003, 88, 879–903. [Google Scholar] [CrossRef] [PubMed]
- Bagozzi, R.P.; Yi, Y. Specification, evaluation, and interpretation of structural equation models. J. Acad. Mark. Sci. 2012, 40, 8–34. [Google Scholar] [CrossRef]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis: A Global Perspective, 7th ed.; MacMillan: New York, NY, USA, 2010. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Bagozzi, R.P.; Yi, Y.; Phillips, L.W. Assessing construct validity in organizational research. Adm. Sci. Q. 1991, 36, 421–458. [Google Scholar] [CrossRef]
- van Velsen, L.; van der Geest, T.; van de Wijngaert, L.; van den Berg, S.; Steehouder, M. Personalization has a Price, Controllability is the Currency: Predictors for the Intention to use Personalized eGovernment Websites. J. Organ. Comput. Electron. Commer. 2015, 25, 76–97. [Google Scholar] [CrossRef]
- Park, H.; Chon, Y.; Lee, J.; Choi, I.J.; Yoon, K.H. Service design attributes affecting diabetic patient preferences of telemedicine in South Korea. Telemed. J. eHealth 2011, 17, 442–451. [Google Scholar] [CrossRef] [PubMed]
- Morton, M.E.; Wiedenbeck, S. EHR acceptance factors in ambulatory care: A survey of physician perceptions. Perspect. Health Inf. Manag. 2010, 7, 1c. [Google Scholar] [PubMed]
- Melas, C.D.; Zampetakis, L.A.; Dimopoulou, A.; Moustakis, V. Modeling the acceptance of clinical information systems among hospital medical staff: An extended TAM model. J. Biomed. Inform. 2011, 44, 553–564. [Google Scholar] [CrossRef] [PubMed]
- Aggelidis, V.P.; Chatzoglou, P.D. Using a modified technology acceptance model in hospitals. Int. J. Med. Inform. 2009, 78, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Almojaibel, A.A.; Munk, N.; Goodfellow, L.T.; Fisher, T.F.; Miller, K.K.; Comer, A.R.; Bakas, T.; Justiss, M.D. Development and validation of the tele-pulmonary rehabilitation acceptance scale. Respir. Care. 2019, 64, 1057–1064. [Google Scholar] [CrossRef] [PubMed]
- Doma, S.S.; Elaref, N.A.; Abo Elnaga, M.A. Factors affecting electronic word-of-mouth on social networking websites in Egypt: An application of the technology acceptance model. Int. J. Netw. Virtual. Organ. 2015, 2015, 1–31. [Google Scholar] [CrossRef]
- Shadangi, P.Y.; Kar, S.; Mohanty, A.K.; Dash, M. Physician’s attitude towards acceptance of telemedicine technology for delivering health care services. Int. J. Mech. Eng. Technol. 2018, 9, 715–722. [Google Scholar]
| Measure | Item | Frequency N = 646 | Percentage (%) |
|---|---|---|---|
| Gender | Male | 234 | 36.2 |
| Female | 412 | 63.8 | |
| Age group | <30 | 157 | 24.3 |
| 31–40 | 131 | 20.3 | |
| 41–50 | 192 | 29.7 | |
| 51–60 | 127 | 19.7 | |
| >61 | 39 | 6.0 | |
| Education level | Elementary school | 5 | 0.8 |
| Junior high school | 14 | 2.2 | |
| Senior high school | 133 | 20.6 | |
| Bachelor’s degree | 400 | 61.9 | |
| Postgraduate (Master’s/Doctoral) | 94 | 14.6 | |
| Marital status | Married | 323 | 42.6 |
| Single | 275 | 50.0 | |
| Widowed (divorced) | 48 | 7.4 |
| Measure | PU | PEOU | ATU | SI | Trust | UI |
|---|---|---|---|---|---|---|
| Perceived Usefulness (PU) | ||||||
| Perceived Ease of Use (PEOU) | 0.507 | |||||
| Attitude Toward Using (ATU) | 0.658 | 0.640 | ||||
| Social Influence (SI) | 0.568 | 0.508 | 0.556 | |||
| Trust | 0.597 | 0.616 | 0.675 | 0.642 | ||
| Usage Intention (UI) | 0.710 | 0.590 | 0.747 | 0.706 | 0.750 | |
| Cronbach’s α | 0.766 | 0.867 | 0.780 | 0.918 | 0.879 | 0.927 |
| CR | 0.705 | 0.847 | 0.634 | 0.869 | 0.716 | 0.850 |
| AVE | 0.445 | 0.582 | 0.369 | 0.624 | 0.457 | 0.416 |
| Mean | 3.647 | 3.837 | 4.018 | 3.356 | 4.005 | 3.741 |
| Standard Deviation | 0.649 | 0.682 | 0.624 | 0.725 | 0.639 | 0.639 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kung, L.-H.; Yan, Y.-H.; Kung, C.-M. Exploring Telemedicine Usage Intention Using Technology Acceptance Model and Social Capital Theory. Healthcare 2024, 12, 1267. https://doi.org/10.3390/healthcare12131267
Kung L-H, Yan Y-H, Kung C-M. Exploring Telemedicine Usage Intention Using Technology Acceptance Model and Social Capital Theory. Healthcare. 2024; 12(13):1267. https://doi.org/10.3390/healthcare12131267
Chicago/Turabian StyleKung, Liang-Hsi, Yu-Hua Yan, and Chih-Ming Kung. 2024. "Exploring Telemedicine Usage Intention Using Technology Acceptance Model and Social Capital Theory" Healthcare 12, no. 13: 1267. https://doi.org/10.3390/healthcare12131267






