Abstract
This study provides a statistical forecast for the development of total elbow arthroplasties (TEAs) in Germany until 2045. The authors used an autoregressive integrated moving average (ARIMA), Error-Trend-Seasonality (ETS), and Poisson model to forecast trends in total elbow arthroplasty based on demographic information and official procedure statistics. They predict a significant increase in total elbow joint replacements, with a higher prevalence among women than men. Comprehensive national data provided by the Federal Statistical Office of Germany (Statistisches Bundesamt) were used to quantify TEA’s total number and incidence rates. Poisson regression, exponential smoothing with Error-Trend-Seasonality, and autoregressive integrated moving average models (ARIMA) were used to predict developments in the total number of surgeries until 2045. Overall, the number of TEAs is projected to increase continuously from 2021 to 2045. This will result in a total number of 982 (TEAs) in 2045 of mostly elderly patients above 80 years. Notably, female patients will receive TEAs 7.5 times more often than men. This is likely influenced by demographic and societal factors such as an ageing population, changes in healthcare access and utilization, and advancements in medical technology. Our projection emphasises the necessity for continuous improvements in surgical training, implant development, and rehabilitation protocols.
1. Introduction
The baby boomer generation will reach retirement age in the upcoming years, which poses challenges to global healthcare systems and likely increases the incidence of degenerative joint diseases [1,2]. The number of arthroscopies of the lower limb is expected to decrease within the next few years, while joint replacements of the upper extremities are expected to grow [3,4,5,6,7]. Additionally, changes in populations with low birth and low immigration rates are also affecting the demographic structure [8,9,10]. An abundance of scientific projections for the development of performed arthroplasties has been published in recent years. Until now, no predictions have been made for the development of total elbow arthroplasty (TEA) in Germany. TEA has undergone significant changes in recent years, with shifts in indications and advancements in surgical techniques and prosthetic designs. For instance, the most common indication for total elbow arthroplasty has transitioned from inflammatory arthritis to traumatic or post-traumatic pathologies [11,12,13]. Advancements in prosthetic designs have also influenced the landscape of TEA. Some prostheses now incorporate features like anterior flanges to enhance implant stability and peri-articular load transfer, aiming to reduce complications such as distal humerus cortical strains. Modular designs broaden adaption to conditions such as distal humeral fractures or radial head complications. [14,15,16] TEA aims to reduce pain, restore elbow function, and thus improve the overall quality of life of the patients. TEA is commonly used to treat severe fractures, failed osteosynthesis, degenerative joint diseases, rheumatoid arthritis (RA), and tumours [17,18,19,20]. In recent years, the numbers for TEA in RA have decreased due to improved medication [21,22]. By that, the main indication for TEA in Germany today is the acute or post-traumatic situation. Today, surgeons can choose from various models and sizes for different indications, emphasising the relevance of TEA in the following years.
The Autoregressive Integrated Moving Average (ARIMA), Error–Trend–Seasonal (ETS), and Poisson Regression (POR) are statistical models used for time series forecasting based on historical data. ARIMA models consider the correlation between an observation and a lagged observation, differences between observations, and moving averages of previous errors to model the data. ETS models are based on decomposing the data into trend, seasonal, and error components, which are then modelled separately. Poisson models are used when the response variable is a count and follows a Poisson distribution, and the number of occurrences is modelled at a fixed interval. These models have been used in medicine for various applications, such as epidemiology, disease forecasting, and healthcare demand prediction [23,24,25]. This study aimed to forecast the incidence and total number of TEA in Germany in the coming years.
2. Materials and Methods
This statistical analysis used comprehensive nationwide data provided by the Federal Statistical Office of Germany (Statistisches Bundesamt, Wiesbaden, Germany). The provided data include inpatient treatment reports from all German hospitals. The data are based on the International Statistical Classification of Diseases and Related Health Problems, Tenth Edition (ICD-10), and the System for Procedures in Medicine (OPS). The data are anonymised, relevant for the billing of the clinics, and subject to official audits by the authorities. To quantify, the total number and incidence rates of TEA depending on the calendar year, age, and sex, the numbers provided were divided into age groups of 10 years. In addition, data regarding the development of the national population in Germany, including age and sex, were retrieved from the official website of the Federal Statistical Office of Germany.
Three different projections were implemented using these data. POR, ETS, and ARIMA were used in the historical procedure rates from 2005 to 2021, which are official population projections from 2020 to 2045. All projections assumed that the observed trend of the past years would continue. Afterwards, the most accurate model was identified by the implementation of the mean absolute percentage error (MAPE), the root mean squared error (RMSE), and the mean absolute error (MAE). The statistical analyses were conducted using R Version 3.4.0 (R Development Core Team, The R Foundation for Statistical Computing, Vienna, Austria).
3. Results
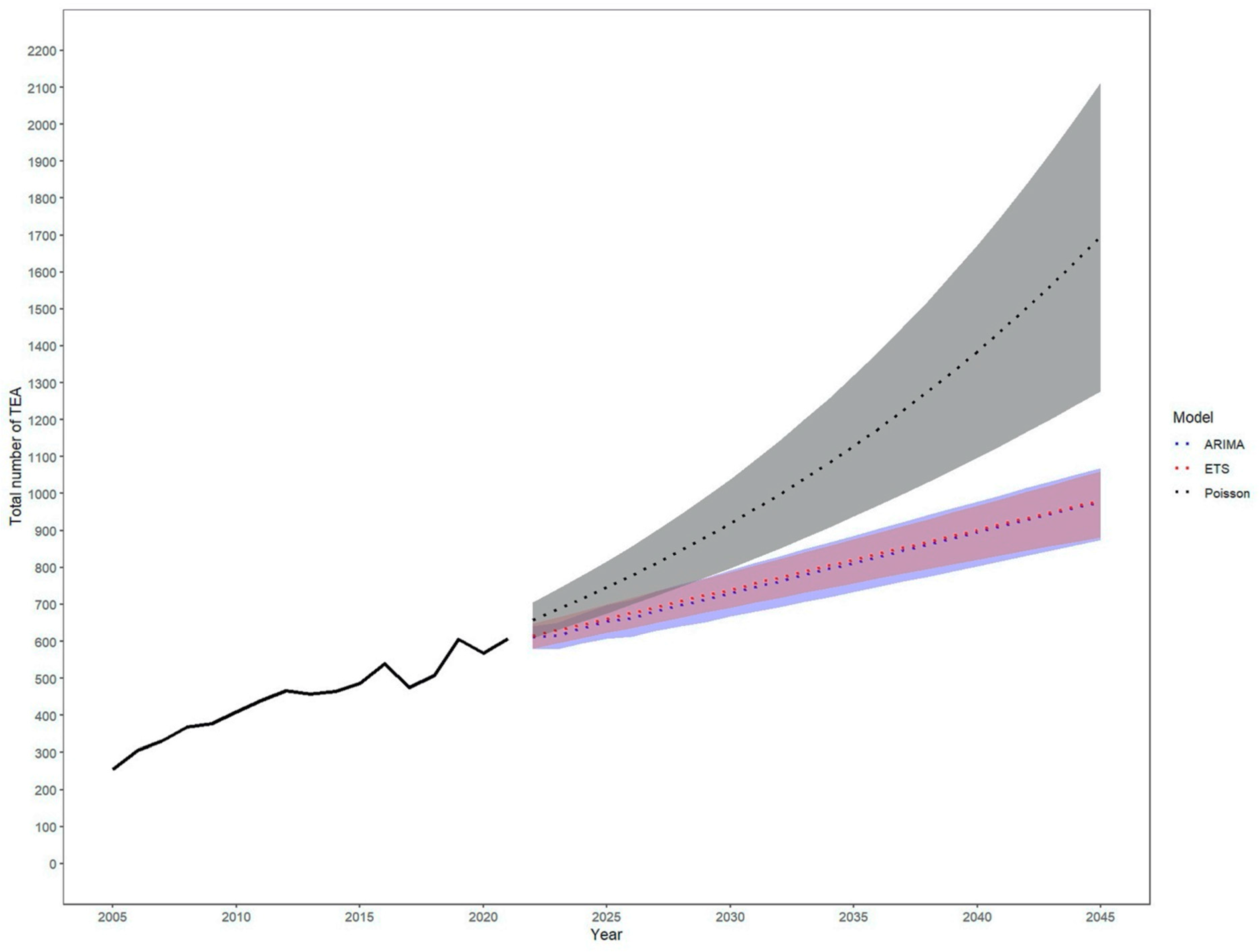
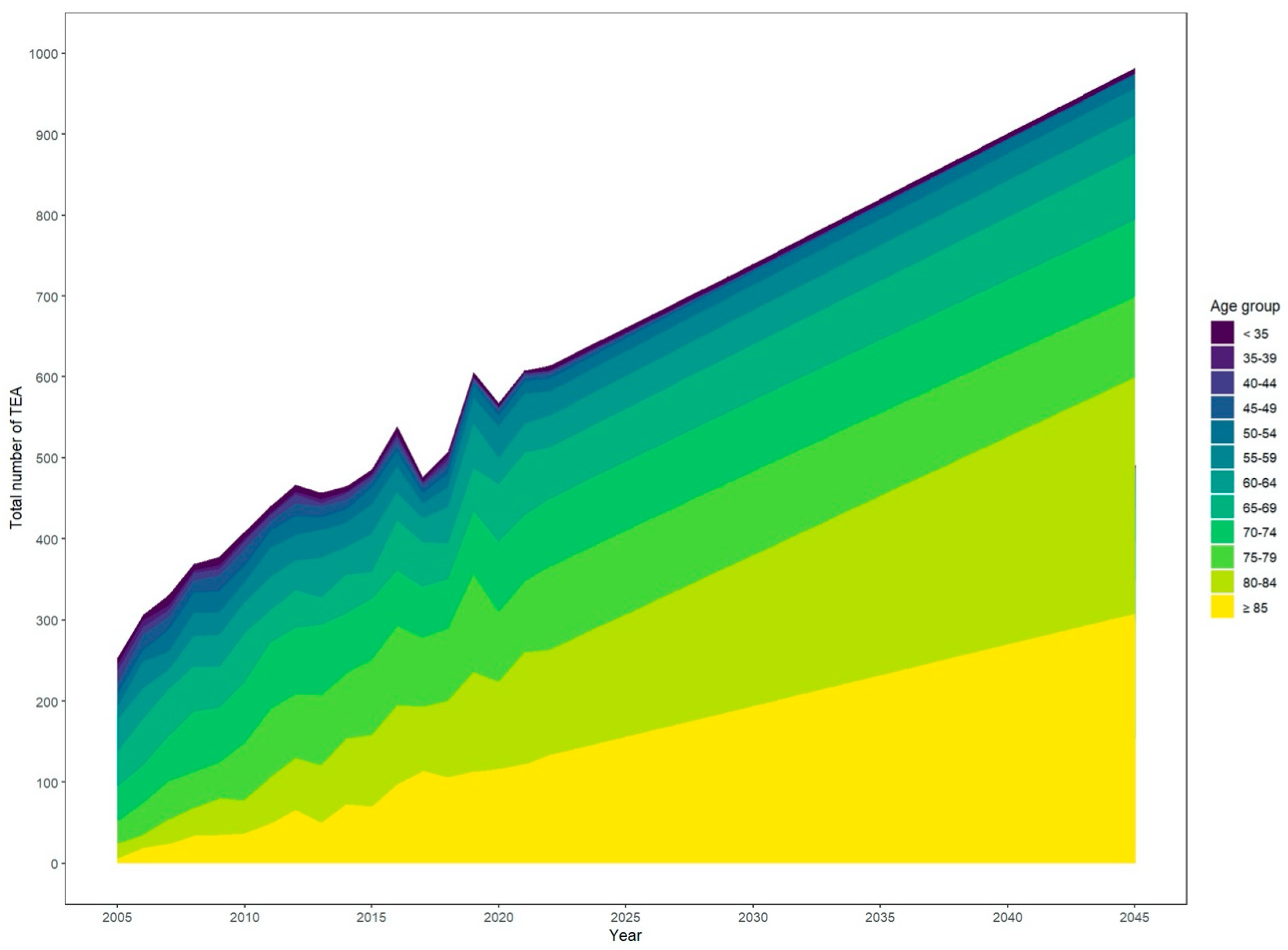
Over the past few years, the total number of TEAs has steadily increased. At the same time, the population has become older. Based on exponential smoothing modelling, the number of TEAs is projected to increase from 2021 to 2045 continuously (Figure 1 and Figure 2). Specifically, the incidence rate of TEA is expected to grow by around 63% to 1.2 per 100,000 inhabitants [95% CI 1.1–1.3], leading to a projected total number of 982 TEA [95% CI 882–1060] in 2045 up from 608 in 2021.
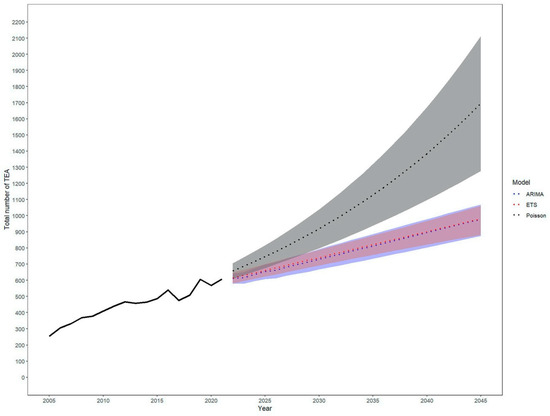
Figure 1.
Increase depending on the model chosen (Autoregressive Integrated Moving Average (ARIMA), Error–Trend–Seasonality (ETS), and Poisson). The historical data is displayed by the solid line. The statistical models differ and are shown in the colour-coded section.
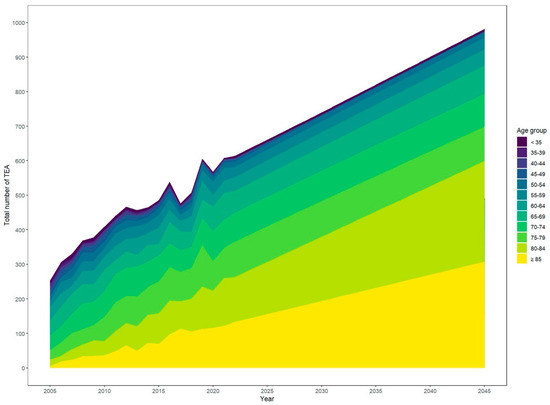
Figure 2.
Projected overall increase in total elbow arthroplasty.
The three prediction models used in this study to estimate the future incidence of TEA are ARIMA, ETS, and Poisson. The accuracy of these models was evaluated using three metrics: Mean Absolute Percentage Error (MAPE), Root Mean Squared Error (RMSE), and Mean Absolute Error (MAE). The ETS model showed the highest accuracy among the three models, with a MAPE of 5.8%, RMSE of 37.4, and MAE of 31.6. The ARIMA model had a MAPE of 7.3%, RMSE of 47.9, and MAE of 39.3, while the Poisson model had a MAPE of 8.2%, RMSE of 58.8, and MAE of 51.4 (Table 1). These results suggest that the ETS model is the most accurate for predicting the incidence of TEA in the future. However, the accuracy of these models can vary depending on the specific dataset and context in which they are used. Therefore, it is recommended that the performance of different models be evaluated on a case-by-case basis before selecting a model for future predictions.

Table 1.
Accuracy of predictions.
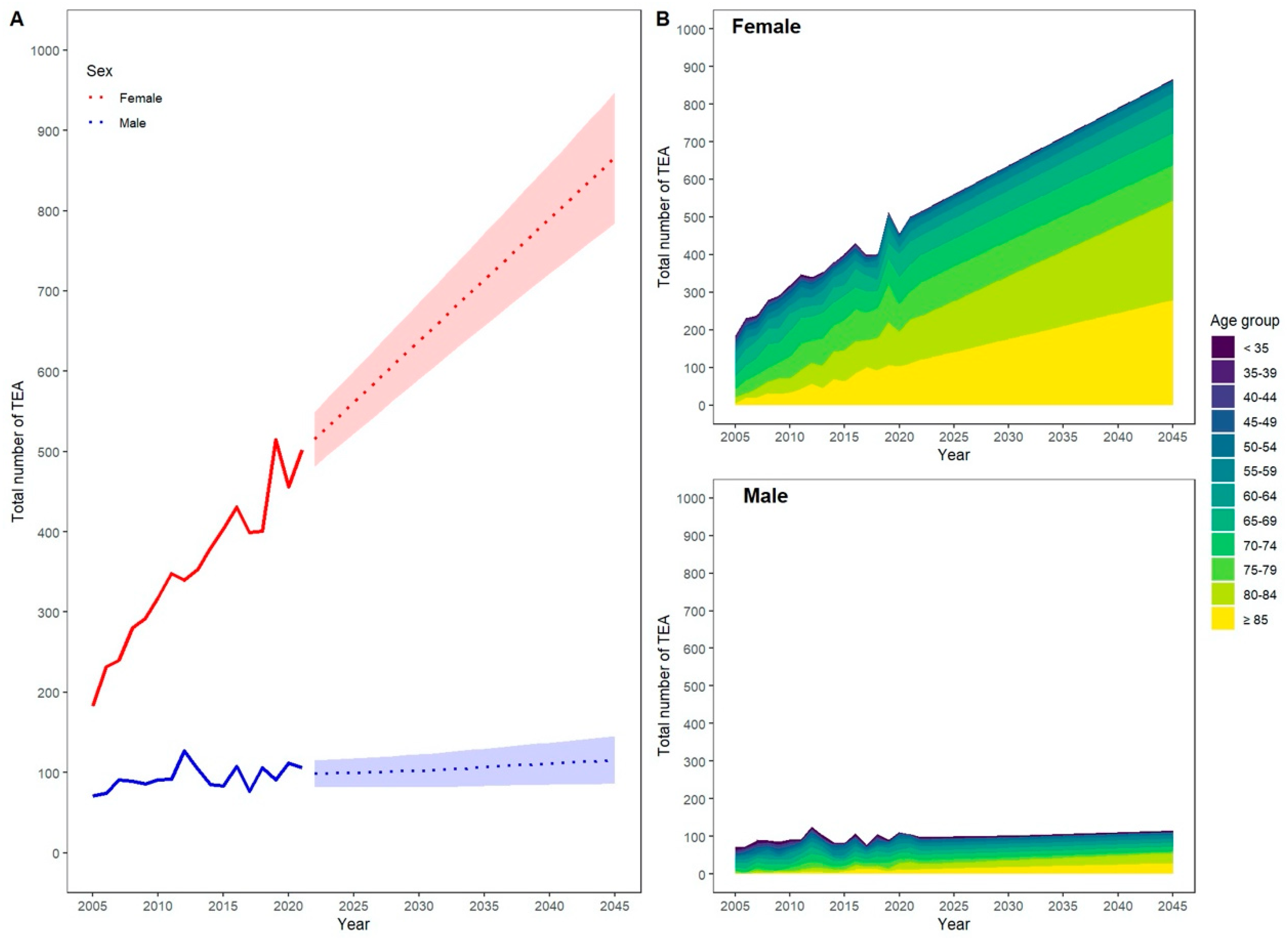
Based on our projection, this increase is mainly driven by a rising number of predominantly female patients aged 80 years and older. This is expected to lead to a 2.3-fold increase in performed procedures for all patients aged 80 years and older in 2045 compared with 2021. In total, TEA will be performed seven times more often in women than in men in 2045, corresponding to a projected total number of 866 TEA [95% CI 785–948] for women and 116 [95% CI 86–146] for men in 2045.
The data in the table show the projected total numbers and incidence rates of total elbow arthroplasty (TEA) in Germany from 2021 to 2045 (Table 2). The data are based on comprehensive nationwide data provided by the Federal Statistical Office of Germany and include information on TEA’s total number and incidence rates as a function of calendar year, age, and gender. The population is expected to increase from 82.7 million in 2021 to 83.76 million in 2024 and will then slightly decline annually until it reaches 82.1 million in 2045. This increase in population, in combination with increasing cases and an overall ageing population, is reflected in the projected total number of TEA procedures, which is expected to rise from 608 in 2021 to 982 in 2045.

Table 2.
Predictions of numbers for the upcoming years.
The data also show differences in the incidence rates of TEA between males and females. In 2021, the incidence rate of TEA was 0.74 per 100,000 individuals, with a projected relative increase of 0.94% in males and 0.73% in females in 2022. This trend is anticipated to persist, with the incidence rate of TEA projected to rise faster in males than in females until 2031. After 2031, the incidence rate is expected to increase more quickly in females than in males (Figure 3).
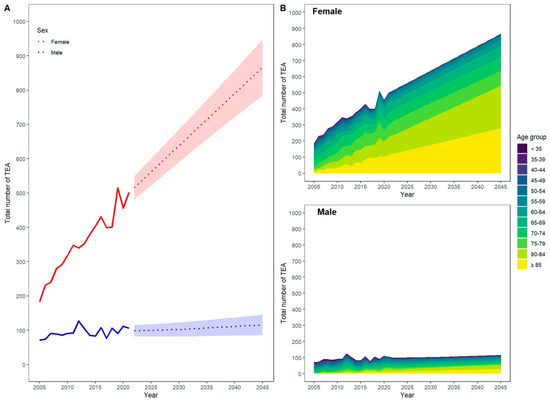
Figure 3.
Increase in total elbow arthroplasty (TEA) by age, (A) total increase with CI, (B) total increase by sex and age group.
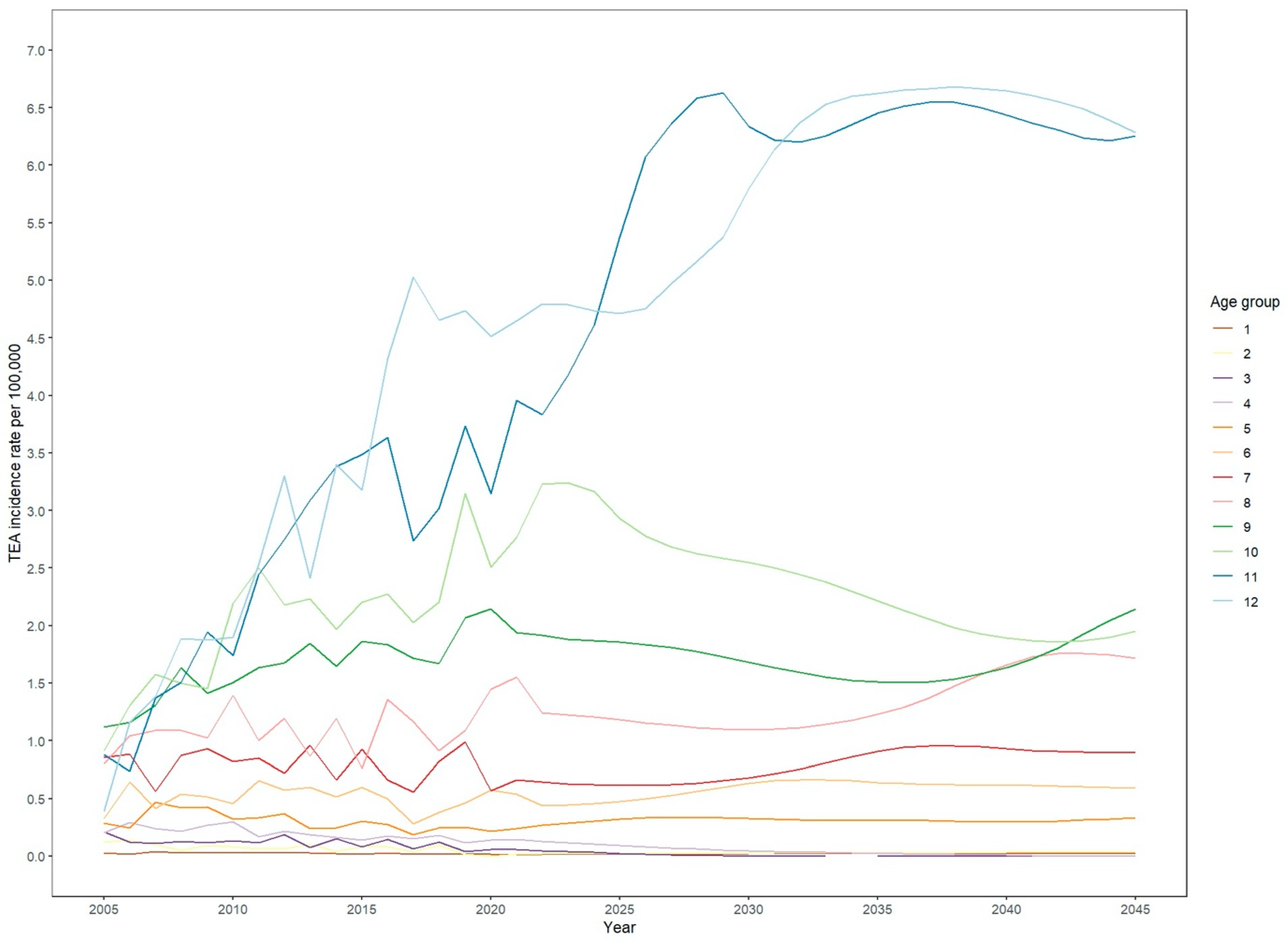
Furthermore, the data provide information on the projected total number and incidence rates of TEA as a function of age. The data show that TEA is performed most often in individuals aged 70 years and older, with the incidence rate increasing steadily (Figure 4). The highest incidence rate is projected for individuals aged 80 years and older.
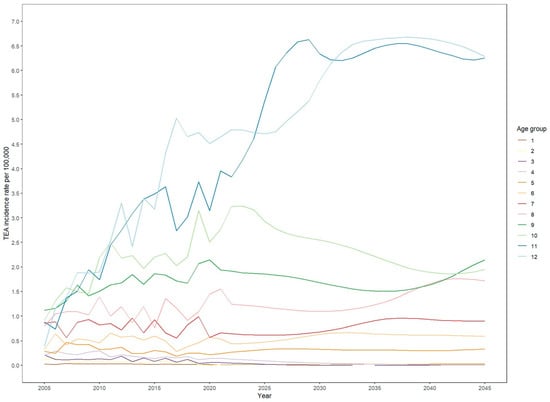
Figure 4.
Development of implanted TEA incidence by age group.
4. Discussion
Statistical models such as ARIMA, ETS, and Poisson are used to make predictions for future counts of surgeries based on historical trends. The provided data show the incidence rates of TEA for men and women from 2005 to 2045. Throughout the years, there have been notable sex differences in the incidence rates according to the official numbers provided by the government. In 2005, the incidence rate for TEA in men was 0.18, while for women, it was higher at 0.43. Over the years, both incidence rates generally increased, but women consistently have higher rates than men. In 2020, the incidence rate for men was 0.27, while for women, it was 1.08. This trend continues until 2045, with women consistently having higher incidence rates than men. The abovementioned differences in incidence rates suggest variations in susceptibility, risk factors, or exposure to the condition between men and women. Investigating potential underlying factors contributing to these discrepancies is essential to understand the condition better and develop targeted prevention and treatment strategies for both sexes. Our projection data indicate that the observed sex differences in the increase in TEA cases until 2045 are primarily driven by a rising number of patients who are 80 years and older. This is further compounded by the fact that women generally have a more significant life expectancy than men, which partially explains the sex differences in projected cases for TEA. This is highlighted by the overall increase in such procedures for patients 80 and older, which will be 2.3-fold when 2045 data are compared with 2021 as the base year. However, other factors such as different prevalence and severity of elbow joint disorders between men and women or sex-dependent healthcare-seeking behaviour can cause this discrepancy between sexes [26,27]. Furthermore, different bone conditions caused by osteoporosis impact the prevalence of complex fractures of the forearm [28].
Orthopaedic surgeons in Germany face unique challenges due to demographic changes. Factors contributing to these demographic shifts include low birth rates and limited immigration, resulting in a declining population [29]. With an ageing population and increasing life expectancy, the prevalence of orthopaedic pathologies such as femoral neck fractures and the need for hip, shoulder, and knee replacements are expected to improve continuously [24,30].
Traumatic conditions substantially influenced the development of TEA within the last decade. While inflammatory diseases remain the main indication for TEA, acute trauma represents the second most prevalent indication, with increasing numbers. This is highlighted by an increase in severe injuries like AO Type C fractures over the past two decades [31]. This is likely associated with ageing, as mentioned above in (Western) societies [32]. Recent studies have shown the superiority of treatments with TEA for complex fractures such as Dubberly Type B or multifragmentary fractures of the trochlea without the possibility of osteosynthesis [33,34,35]. Given the continuous development of implants, it is to be expected that complex fractures in elderly patients will be treated with TEA in the future.
Simultaneously, the percentage of TEA indications based on inflammatory joint diseases is decreasing, most likely due to innovations in anti-inflammatory medications such as disease-modifying drugs (DMARD) and antibodies in industrialised countries [36,37]. Nevertheless, a relevant number of patients suffering from RA require TEA, as evidenced by virtually unchanging incidences in this population [38,39]. However, our projection suggests a trend towards trauma as the main indication for TEA. Still, it might be influenced by the increasing number of rheumatic joint diseases in the overall population [36].
Additionally, the increase in primary TEA will inevitably trigger an increase in complications, such as infections, periprosthetic fractures, and mechanical failure. Consequentially, revision TEA will pose an additional challenge for the surgical team. This emphasises the necessity for more research and innovations to improve diagnostics for infections and treatments for periprosthetic fractures or loosening, as well as overall longevity.
5. Conclusions
Predicting future technological breakthroughs is challenging [40]. However, ongoing research and development in elbow prostheses suggest potential advances. For example, advancements in biomaterials may lead to new implant materials with improved mechanical properties and biocompatibility [41,42,43]. Those might result in longer-lasting, more durable, and personalised prostheses [44,45]. Similarly, developing new surgical techniques and technologies, such as robotics and virtual reality, may enhance the accuracy and precision of implant placement and reduce the risk of complications [46,47].
Fractures in elderly patients are common. The demographic changes will likely significantly increase the total number of fractures, leading to an increased need for total arthroplasties in the upper limb, including the elbow [7,48]. A high activity level for TEA might aggravate the problem, causing more fracture-related indications [49]. On the other hand, the increasing demand for joint replacement surgery may strain healthcare resources and lead to longer wait times for surgery. Elbow arthroplasty is a technically challenging procedure that requires a high level of skill and experience, which can limit its availability in certain regions or healthcare systems. More surgeons need to be trained in surgical techniques for TEA. Therefore, ongoing TEA research, training, and development are essential to ensure patients receive the best possible care.
While short-term outcomes of TEA surgery are favourable, there is a lack of data regarding elbow prostheses’ long-term effectiveness and durability [50,51]. This is particularly important because contemporary joint replacement surgery is frequently performed in younger patients who may require revision surgery later in life [52,53].
The authors acknowledge the limitations of the presented manuscript. Most importantly, this work is based on official numbers provided by the German government. The forecasted numbers refer to an industrialised country with an overall high level of medical care. The developments described above for Germany are certainly transferable to other countries. Still, they cannot reflect the trends for regions with different medical systems or demographics and thus lack generalisability. The statistical analysis in this paper provides trend values that can predict trends that can be affected by unpredictable events such as international crises, wars or pandemics. Overall, this work can be used to better plan and manage future challenges in TEA.
Author Contributions
F.K., V.J.H. and K.K. were involved in the Conceptualization and Design of this study. F.K. and V.J.H. worked on the data acquisition and curation. K.K. was responsible for methodology, software and data analysis. F.K. was the main author of this study and was responsible for the visualisation. J.L., J.K., A.K. and M.H. were conducted by reviewing and editing. L.P.M. and T.L. contributed as supervisors. All authors have read and agreed to the published version of the manuscript.
Funding
No financial or other forms of support were provided to the authors of this study, their relatives, or their family members. The authors independently conducted all aspects of the research, including the design, data collection, analysis and interpretation. This declaration ensures the integrity and impartiality of the findings presented in this paper. The authors affirm no conflicts of interest related to this work. This study was conducted without any external funding. The authors did not receive financial support from any organisation or institution to conduct this research. All resources and expenses associated with the study were covered by the authors themselves.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data used in this study are available upon request. Interested researchers can obtain access to the dataset by contacting the corresponding author. This ensures transparency and allows for the reproducibility and verification of the study’s findings.
Acknowledgments
We thank Rob J. Hyndman, Department of Econometrics and Business Statistics, Monash University, Australia, for advising and supporting the authors with the statistical analysis.
Conflicts of Interest
The authors declare no conflicts of interest. The data utilised in this study are publicly available and entirely anonymous, ensuring that no personal or identifiable information is used. Consequently, the study did not require approval from the local ethics board, as it complies with ethical standards for research involving publicly accessible and anonymised datasets.
References
- Jacob, L.; Breuer, J.; Kostev, K. Prevalence of chronic diseases among older patients in German general practices. GMS Ger. Med. Sci. 2016, 14, Doc03. [Google Scholar]
- Nowossadeck, E. Population aging and hospitalization for chronic disease in Germany. Dtsch. Ärzteblatt Int. 2012, 109, 151–157. [Google Scholar] [CrossRef]
- Pilz, V.; Hanstein, T.; Skripitz, R. Projections of primary hip arthroplasty in Germany until 2040. Acta Orthop. 2018, 89, 308–313. [Google Scholar] [CrossRef]
- Inacio, M.C.S.; Graves, S.E.; Pratt, N.L.; Roughead, E.E.; Nemes, S. Increase in Total Joint Arthroplasty Projected from 2014 to 2046 in Australia: A Conservative Local Model With International Implications. Clin. Orthop. Relat. Res. 2017, 475, 2130–2137. [Google Scholar] [CrossRef]
- Kurtz, S.; Ong, K.; Lau, E.; Mowat, F.; Halpern, M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Jt. Surg. 2007, 89, 780–785. [Google Scholar] [CrossRef]
- Day, J.S.; Lau, E.; Ong, K.L.; Williams, G.R.; Ramsey, M.L.; Kurtz, S.M. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J. Shoulder Elb. Surg. 2010, 19, 1115–1120. [Google Scholar] [CrossRef]
- Rupp, M.; Lau, E.; Kurtz, S.M.; Alt, V. Projections of primary TKA and THA in Germany from 2016 through 2040. Clin. Orthop. Relat. Res. 2020, 478, 1622–1633. [Google Scholar] [CrossRef]
- Coleman, D.; Rowthorn, R. Who’s afraid of population decline? A critical examination of its consequences. Popul. Dev. Rev. 2011, 37, 217–248. [Google Scholar] [CrossRef]
- Weber, H. Could Immigration Prevent Population Decline? The Demographic Prospects of Germany Revisited. Comp. Popul. Stud. 2015, 40, 166–189. [Google Scholar] [CrossRef]
- Schollgen, I.; Huxhold, O.; Tesch-Romer, C. Socioeconomic status and health in the second half of life: Findings from the German Ageing Survey. Eur. J. Ageing 2010, 7, 17–28. [Google Scholar] [CrossRef]
- Gay, D.M.; Lyman, S.; Do, H.; Hotchkiss, R.N.; Marx, R.G.; Daluiski, A. Indications and reoperation rates for total elbow arthroplasty: An analysis of trends in New York State. J. Bone Jt. Surg. Am. 2012, 94, 110–117. [Google Scholar] [CrossRef]
- Burkhart, K.J.; Watts, A.C.; Athwal, G.S.; Hollinger, B.; Wegmann, K.; Müller, L.P. Complication Management in Distal Humerus Hemiarthroplasty. In Elbow Arthroplasty: Current Techniques and Complications; Springer: Berlin/Heidelberg, Germany, 2020; pp. 233–241. [Google Scholar]
- Kolusu, D.N.; Mekala, D.K.R. A study on clinical outcome of total elbow arthroplasty. Int. J. Orthop. Sci. 2018, 4, 522–526. [Google Scholar] [CrossRef]
- Craik, J.D.; Laffer, C.H.; Richards, S.W.; Walsh, S.P.; Evans, S.L. Distal humerus cortical strains following total elbow arthroplasty. Proc. Inst. Mech. Eng. H 2013, 227, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Rotini, R.; Ricciarelli, M.; Guerra, E.; Marinelli, A.; Celli, A. Elbow hemiarthroplasty in distal humeral fractures: Indication, surgical technique and results. Injury 2023, 54 (Suppl. S1), S36–S45. [Google Scholar] [CrossRef] [PubMed]
- Wagener, M.L.; De Vos, M.J.; Hendriks, J.C.; Eygendaal, D.; Verdonschot, N. Stability of the unlinked Latitude total elbow prosthesis: A biomechanical in vitro analysis. Clin. Biomech. 2013, 28, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Müller, L.P.; Hollinger, B.; Burkhart, K. Ellenbogen: Expertise Orthopädie und Unfallchirurgie; Georg Thieme Verlag: New York, NY, USA, 2016. [Google Scholar]
- Bachman, D.; Cil, A. Current concepts in elbow arthroplasty. EFORT Open Rev. 2017, 2, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Samdanis, V.; Manoharan, G.; Jordan, R.W.; Watts, A.C.; Jenkins, P.; Kulkarni, R.; Thomas, M.; Rangan, A.; Hay, S.M. Indications and outcome in total elbow arthroplasty: A systematic review. Shoulder Elb. 2020, 12, 353–361. [Google Scholar] [CrossRef]
- Petscavage, J.M.; Ha, A.S.; Chew, F.S. Radiologic review of total elbow, radial head, and capitellar resurfacing arthroplasty. Radiographics 2012, 32, 129–149. [Google Scholar] [CrossRef]
- Keely Boyle, K.; Rachala, S.; Nodzo, S.R. Centers for Disease Control and Prevention 2017 Guidelines for Prevention of Surgical Site Infections: Review and Relevant Recommendations. Curr. Rev. Musculoskelet. Med. 2018, 11, 357–369. [Google Scholar] [CrossRef]
- Nystad, T.W.; Fenstad, A.M.; Havelin, L.I.; Furnes, O.; Skredderstuen, A.K.; Fevang, B.T.S. SAT0061 Reduction in Joint Replacement Surgery in Patients with Reumatoid Arthritis. Ann. Rheum. Dis. 2014, 73, 611–612. [Google Scholar] [CrossRef]
- Klug, A.; Gramlich, Y.; Buckup, J.; Schweigkofler, U.; Hoffmann, R.; Schmidt-Horlohe, K. Trends in total elbow arthroplasty: A nationwide analysis in Germany from 2005 to 2014. Int. Orthop. 2018, 42, 883–889. [Google Scholar] [CrossRef] [PubMed]
- Klug, A.; Herrmann, E.; Fischer, S.; Hoffmann, R.; Gramlich, Y. Projections of Primary and Revision Shoulder Arthroplasty until 2040: Facing a Massive Rise in Fracture-Related Procedures. J. Clin. Med. 2021, 10, 5123. [Google Scholar] [CrossRef] [PubMed]
- Alabdulrazzaq, H.; Alenezi, M.N.; Rawajfih, Y.; Alghannam, B.A.; Al-Hassan, A.A.; Al-Anzi, F.S. On the accuracy of ARIMA based prediction of COVID-19 spread. Results Phys. 2021, 27, 104509. [Google Scholar] [CrossRef]
- Park, J.G.; Cho, N.S.; Song, J.H.; Lee, D.S.; Rhee, Y.G. Clinical outcomes of semiconstrained total elbow arthroplasty in patients who were forty years of age or younger. JBJS 2015, 97, 1781–1791. [Google Scholar] [CrossRef]
- Sjögren, K.; Stjernberg, L. A gender perspective on factors that influence outdoor recreational physical activity among the elderly. BMC Geriatr. 2010, 10, 34. [Google Scholar] [CrossRef]
- Melton, L.J., 3rd. The prevalence of osteoporosis: Gender and racial comparison. Calcif. Tissue Int. 2001, 69, 179–181. [Google Scholar] [CrossRef]
- Dorbritz, J. Germany: Family Diversity with Low Actual and Desired Fertility. Demogr. Res. 2008, 19, 557–598. [Google Scholar] [CrossRef]
- Kappenschneider, T.; Maderbacher, G.; Weber, M.; Greimel, F.; Holzapfel, D.; Parik, L.; Schwarz, T.; Leiss, F.; Knebl, M.; Reinhard, J.; et al. Special orthopaedic geriatrics (SOG)—A new multiprofessional care model for elderly patients in elective orthopaedic surgery: A study protocol for a prospective randomized controlled trial of a multimodal intervention in frail patients with hip and knee replacement. BMC Musculoskelet. Disord. 2022, 23, 1079. [Google Scholar] [CrossRef]
- Charissoux, J.L.; Vergnenegre, G.; Pelissier, M.; Fabre, T.; Mansat, P.; Sofcot. Epidemiology of distal humerus fractures in the elderly. Orthop. Traumatol. Surg. Res. 2013, 99, 765–769. [Google Scholar] [CrossRef]
- Macken, A.A.; Prkic, A.; Kodde, I.F.; Lans, J.; Chen, N.C.; Eygendaal, D. Global trends in indications for total elbow arthroplasty: A systematic review of national registries. EFORT Open Rev. 2020, 5, 215–220. [Google Scholar] [CrossRef]
- Stone, A.; Chan, G.; Sinclair, L.; Phadnis, J. Elbow arthroplasty in trauma-current concepts review. J. Orthop. 2023, 35, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Celli, A.; Paroni, C.; Bonucci, P.; Celli, L. Total elbow arthroplasty for acute distal humeral fractures with humeral condyle resection or retention: A long-term follow-up study. JSES Int. 2021, 5, 797–803. [Google Scholar] [CrossRef]
- Loisel, F.; Amar, Y.; Rochet, S.; Obert, L. Distal humerus fracture in older patients: ORIF vs. total elbow arthroplasty. Orthop. Traumatol. Surg. Res. 2024, 110, 103759. [Google Scholar] [CrossRef] [PubMed]
- Jin, Z.; Wang, D.; Zhang, H.; Liang, J.; Feng, X.; Zhao, J.; Sun, L. Incidence trend of five common musculoskeletal disorders from 1990 to 2017 at the global, regional and national level: Results from the global burden of disease study 2017. Ann. Rheum. Dis. 2020, 79, 1014–1022. [Google Scholar] [CrossRef] [PubMed]
- Sizova, L. Approaches to the treatment of early rheumatoid arthritis with disease-modifying antirheumatic drugs. Br. J. Clin. Pharmacol. 2008, 66, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Harb, M.A.; Solow, M.; Newman, J.M.; Sodhi, N.; Pivec, R.; George, J.; Sultan, A.A.; Khlopas, A.; Shah, N.V.; Roche, M.W. Have the annual trends of total knee arthroplasty in rheumatoid arthritis patients changed? J. Knee Surg. 2018, 31, 841–845. [Google Scholar] [CrossRef] [PubMed]
- Yasui, T.; Nishino, J.; Kadono, Y.; Matsui, T.; Nakamura, K.; Tanaka, S.; Tohma, S. Impact of biologics on the prevalence of orthopedic surgery in the National Database of Rheumatic Diseases in Japan. Mod. Rheumatol. 2010, 20, 233–237. [Google Scholar] [CrossRef]
- Singh, J.A.; Yu, S.; Chen, L.; Cleveland, J.D. Rates of Total Joint Replacement in the United States: Future Projections to 2020-2040 Using the National Inpatient Sample. J. Rheumatol. 2019, 46, 1134–1140. [Google Scholar] [CrossRef]
- Dissanayake, K.; Jayasinghe, C.; Wanigasekara, P.; Sominanda, A. Potential applicability of cytokines as biomarkers of disease activity in rheumatoid arthritis: Enzyme-linked immunosorbent spot assay-based evaluation of TNF-α, IL-1β, IL-10 and IL-17A. PLoS ONE 2021, 16, e0246111. [Google Scholar] [CrossRef]
- Kiradzhiyska, D.D.; Mantcheva, R.D. Overview of biocompatible materials and their use in medicine. Folia Medica 2019, 61, 34–40. [Google Scholar] [CrossRef]
- Song, J.; Winkeljann, B.; Lieleg, O. Biopolymer-based coatings: Promising strategies to improve the biocompatibility and functionality of materials used in biomedical engineering. Adv. Mater. Interfaces 2020, 7, 2000850. [Google Scholar] [CrossRef]
- Kermavnar, T.; Shannon, A.; O’Sullivan, K.J.; McCarthy, C.; Dunne, C.P.; O’Sullivan, L.W. Three-Dimensional Printing of Medical Devices Used Directly to Treat Patients: A Systematic Review. 3d Print. Addit. Manuf. 2021, 8, 366–408. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.M.Y.; Wong, P.Y.; Liu, C.; Chung, Y.L.; Wong, K.C.; Tso, C.Y.; Chow, S.K.-H.; Cheung, W.-H.; Yung, P.S.-H.; Chui, C.S. 3D printing in orthopaedic surgery: A scoping review of randomized controlled trials. Bone Jt. Res. 2021, 10, 807–819. [Google Scholar] [CrossRef] [PubMed]
- Zheng, G.; Li, S. Computational Radiology for Orthopaedic Interventions; Springer: Berlin/Heidelberg, Germany, 2016. [Google Scholar]
- Tanji, A.; Nagura, T.; Iwamoto, T.; Matsumura, N.; Nakamura, M.; Matsumoto, M.; Sato, K. Total elbow arthroplasty using an augmented reality–assisted surgical technique. J. Shoulder Elb. Surg. 2022, 31, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Hemmann, P.; Ziegler, P.; Konrads, C.; Ellmerer, A.; Klopfer, T.; Schreiner, A.J.; Bahrs, C. Trends in fracture development of the upper extremity in Germany-a population-based description of the past 15 years. J. Orthop. Surg. Res. 2020, 15, 65. [Google Scholar] [CrossRef] [PubMed]
- Europe, A. Looking at the Lives of Older People in the EU; Publications Office of the European Union: Luxbembourg, 2020. [Google Scholar]
- Viveen, J.; Prkic, A.; Koenraadt, K.L.; Kodde, I.F.; The, B.; Eygendaal, D. Clinical and radiographic outcome of revision surgery of total elbow prosthesis: Midterm results in 19 cases. J. Shoulder Elb. Surg. 2017, 26, 716–722. [Google Scholar] [CrossRef] [PubMed]
- Davey, M.S.; Hurley, E.T.; Gaafar, M.; Molony, D.; Mullett, H.; Pauzenberger, L. Long-term outcomes of total elbow arthroplasty: A systematic review of studies at 10-year follow-up. J. Shoulder Elb. Surg. 2021, 30, 1423–1430. [Google Scholar] [CrossRef] [PubMed]
- Maman, D.; Weishahe, N.; Norman, D.; Keren, Y.; Yelton, M.; Trior, Y.; Apt, E.A.; Peskin, B.; Ghrayeb, N.; Shapira, J. Outcomes of Total Elbow Arthroplasty in Trauma Patients Compared with Patients Following Fixation of Distal Humerus Fractures. Preprints 2022. [Google Scholar] [CrossRef]
- Siala, M.; Laumonerie, P.; Hedjoudje, A.; Delclaux, S.; Bonnevialle, N.; Mansat, P. Outcomes of semiconstrained total elbow arthroplasty performed for arthritis in patients under 55 years old. J. Shoulder Elbow Surg. 2020, 29, 859–866. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).