A Pilot Study on the Efficacy of an App-Based Rehabilitation Counselling Program after Total Knee Arthroplasty
Abstract
1. Introduction
2. Materials and Methods
2.1. Rehabilitation Group Sessions
2.2. Measurements
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brosseau, L.; Milne, S.; Wells, G.; Tugwell, P.; Robinson, V.; Casimiro, L.; Pelland, L.; Noel, M.-J.; Davis, J.; Drouin, H. Efficacy of continuous passive motion following total knee arthroplasty: A metaanalysis. J. Rheumatol. 2004, 31, 2251–2264. [Google Scholar]
- Mounach, A.; Nouijai, A.; Ghozlani, I.; Ghazi, M.; Achemlal, L.; Bezza, A.; El Maghraoui, A. Risk factors for knee osteoarthritis in Morocco. A case control study. Clin. Rheumatol. 2007, 27, 323–326. [Google Scholar] [CrossRef] [PubMed]
- Kauppila, A.-M.; Kyllönen, E.; Ohtonen, P.; Hämäläinen, M.; Mikkonen, P.; Laine, V.; Siira, P.; Mäki-Heikkilä, P.; Sintonen, H.; Leppilahti, J.; et al. Multidisciplinary rehabilitation after primary total knee arthroplasty: A randomized controlled study of its effects on functional capacity and quality of life. Clin. Rehabil. 2010, 24, 398–411. [Google Scholar] [CrossRef] [PubMed]
- NIH Consensus Panel. NIH Consensus statement on total knee replacement December 8–10, 2003. J. Bone Jt. Surg. Am. 2004, 86, 1328–1335. [Google Scholar] [CrossRef]
- Ethgen, O.; Bruyère, O.; Richy, F.; Dardennes, C.; Reginster, J.-Y. Health-related quality of life in total hip and total knee arthroplasty. J. Bone Jt. Surg. Am. 2004, 86, 963–974. [Google Scholar] [CrossRef]
- Kim, Y.-J.; Kang, H.-Y. Effects of early exercise education using video on exercise knowledge and compliance of elderly patients who undergo total knee replacement surgery. J. Korean Acad. Soc. Nurs. Educ. 2016, 22, 316–325. [Google Scholar] [CrossRef][Green Version]
- Chen, S.-R.; Chen, C.-S.; Lin, P.-C. The effect of educational intervention on the pain and rehabilitation performance of patients who undergo a total knee replacement. J. Clin. Nurs. 2013, 23, 279–287. [Google Scholar] [CrossRef]
- Scott, D.F. Knee Joint Replacement Surgery: Post-Operative Exercise Program. Available online: https://orthospecialtyclinic.com/wp-content/uploads/2013/04/OSC-Knee-Repl.-Exercise-Pro.pdf (accessed on 17 April 2024).
- Su, W.; Zhou, Y.; Qiu, H.; Hui, W. The effects of preoperative rehabilitation on pain and functional outcome after total knee arthroplasty: A meta-analysis of randomized controlled trials. J. Orthop. Surg. Res. 2022, 17, 175. [Google Scholar] [CrossRef] [PubMed]
- Wirries, N.; Ezechieli, M.; Stimpel, K.; Skutek, M. Impact of continuous passive motion on rehabilitation following total knee arthroplasty. Physiother. Res. Int. 2020, 25, e1869. [Google Scholar] [CrossRef]
- McDonald, D.A.; Siegmeth, R.; Deakin, A.H.; Kinninmonth, A.W.G.; Scott, N.B. An enhanced recovery programme for primary total knee arthroplasty in the United Kingdom—Follow up at one year. Knee 2012, 19, 525–529. [Google Scholar] [CrossRef]
- Stauber, A.; Schüßler, N.; Palmdorf, S.; Schürholz, N.; Bruns, D.; Osterbrink, J.; Nestler, N. RECOVER-E—A mobile app for patients undergoing total knee or hip replacement: Study protocol. BMC Musculoskelet. Disord. 2020, 21, 71. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.L.; Rowlingson, A.J.; Partin, A.W.; Kalish, M.A.; Courpas, G.E.; Walsh, P.C.; Fleisher, L.A. Correlation of postoperative pain to quality of recovery in the immediate postoperative period. Reg. Anesth. Pain. Med. 2005, 30, 516–522. [Google Scholar] [CrossRef] [PubMed]
- De Luca, M.L.; Ciccarello, M.; Martorana, M.; Infantino, D.; Leticia Mauro, G.; Bonarelli, S.; Benedetti, M.G. Pain monitoring and management in a rehabilitation setting after total joint replacement. Medicine 2018, 97, e12484. [Google Scholar] [CrossRef]
- Pronk, Y.; Peters, M.C.W.M.; Sheombar, A.; Brinkman, J.-M. Effectiveness of a mobile eHealth app in guiding patients in pain control and opiate use after total knee replacement: Randomized controlled trial. JMIR Mhealth Uhealth 2020, 8, e16415. [Google Scholar] [CrossRef]
- Bäcker, H.C.; Wu, C.H.; Schulz, M.R.G.; Weber-Spickschen, T.S.; Perka, C.; Hardt, S. App-based rehabilitation program after total knee arthroplasty: A randomized controlled trial. Arch. Orthop. Trauma. Surg. 2021, 141, 1575–1582. [Google Scholar] [CrossRef]
- Correia, F.D.; Nogueira, A.; Magalhães, I.; Guimarães, J.; Moreira, M.; Barradas, I.; Teixeira, L.; Tulha, J.; Seabra, R.; Lains, J.; et al. Home-based rehabilitation with a novel digital biofeedback system versus conventional in-person rehabilitation after total knee replacement: A feasibility study. Sci. Rep. 2018, 8, 11299. [Google Scholar] [CrossRef]
- Dahlberg, L.E.; Dell’Isola, A.; Lohmander, L.S.; Nero, H. Improving osteoarthritis care by digital means—Effects of a digital self-management program after 24- or 48-weeks of treatment. PLoS ONE 2020, 15, e0229783. [Google Scholar] [CrossRef]
- Irvine, A.B.; Russell, H.; Manocchia, M.; Mino, D.E.; Glassen, T.C.; Morgan, R.; Gau, J.M.; Birney, A.J.; Ary, D.V. Mobile-Web app to self-manage low back pain: Randomized controlled trial. J. Med. Internet Res. 2015, 17, e3130. [Google Scholar] [CrossRef]
- Biebl, J.T.; Rykala, M.; Strobel, M.; Bollinger, P.K.; Ulm, B.; Kraft, E.; Huber, S.; Lorenz, A. App-based feedback for rehabilitation exercise correction in patients with knee or hip osteoarthritis: Prospective cohort study. J. Med. Internet Res. 2021, 23, e26658. [Google Scholar] [CrossRef]
- Mecklenburg, G.; Smittenaar, P.; Erhart-Hledik, J.C.; Perez, D.A.; Hunter, S. Effects of a 12-week digital care program for chronic knee pain on pain, mobility, and surgery risk: Randomized controlled trial. J. Med. Internet Res. 2018, 20, e156. [Google Scholar] [CrossRef]
- Aseer, P.A.L.; Maiya, G.A.; Kumar, M.M.; Vijayaraghavan, P.V. Content validation of total knee replacement rehabilitation protocol in Indian population. J. Clin. Diagn. Res. 2017, 11, YC05-9. [Google Scholar] [CrossRef] [PubMed]
- Richter, M.; Trzeciak, T.; Kaczmarek, M. Effect of continuous passive motion on the early recovery outcomes after total knee arthroplasty. Int. Orthop. 2022, 46, 549–553. [Google Scholar] [CrossRef] [PubMed]
- Mau-Moeller, A.; Behrens, M.; Finze, S.; Bruhn, S.; Bader, R.; Mittelmeier, W. The effect of continuous passive motion and sling exercise training on clinical and functional outcomes following total knee arthroplasty: A randomized active-controlled clinical study. Health Qual. Life Outcomes 2014, 12, 68. [Google Scholar] [CrossRef] [PubMed]
- Piqueras, M.; Marco, E.; Coll, M.; Escalada, F.; Ballester, A.R.; Cinca, C.; Belmonte, R.; Muniesa, J.M. Effectiveness of an interactive virtual telerehabilitation system in patients after total knee arthoplasty: A randomized controlled trial. J. Rehabil. Med. 2013, 45, 392–396. [Google Scholar] [CrossRef]
- Duong, V.; Robbins, S.R.; Dennis, S.; Venkatesha, V.; Ferreira, M.L.; Hunter, D.J. Combined digital interventions for pain reduction in patients undergoing knee replacement: A randomized clinical trial. JAMA Netw. Open 2023, 6, e2333172. [Google Scholar] [CrossRef]

| Variable | Group A (n = 14) | Group B (n = 14) | Group C (n = 14) | p Value |
|---|---|---|---|---|
| Age (yr) | 69.54 ± 6.63 | 69.08 ± 6.09 | 66.38 ± 7.26 | n.s. |
| Height (cm) | 155.77 ± 8.69 | 159.00 ± 6.81 | 164.08 ± 7.51 | n.s. |
| Weight (kg) | 63.46 ± 9.79 | 66.54 ± 11.82 | 71.31 ± 12.33 | n.s. |
| BMI: Weight (kg)/Height (m2) | 26.09 ± 2.82 | 26.18 ± 3.26 | 26.44 ± 4.11 | n.s. |
| Index | Exercise | Intensity | |
|---|---|---|---|
| Rehabilitation training based on a guideline leaflet (A) | 1–2 weeks | Ham stretching | 10 reps × 3 sets |
| 60 min, 3 times a week | Ankle pump | 100 reps | |
| Knee extension stretching | 0°–90°/50 reps | ||
| Front SLR | 10 reps × 3 sets | ||
| Side SLR | 10 reps × 3 sets | ||
| Back SLR | 10 reps × 3 sets | ||
| SAQ | 10 reps × 3 sets | ||
| 2 LAQ | 10 reps × 3 sets | ||
| Calf raise | 10 reps × 3 sets | ||
| Chair squat | 10 reps × 3 sets | ||
| 3–6 weeks | Band ham stretching | (10 s × 10 reps) × 3 sets | |
| 60 min, 3 times a week | Ankle pump | 0°–90°/50 reps | |
| Knee extension stretching | 10 reps × 3 sets | ||
| Pocket front SLR | 10 reps × 3 sets | ||
| Pocket side SLR | 10 reps × 3 sets | ||
| Pocket back SLR | 10 reps × 3 sets | ||
| Pocket SAQ | 10 reps × 3 sets | ||
| Pocket LAQ | 10 reps × 3 sets | ||
| Calf raise | 10 reps × 3 sets | ||
| Viking walking exercise | 10 reps × 3 sets | ||
| Wall squat | 10 reps × 3 sets | ||
| 7–12 weeks | Band ham stretching | 10 reps × 3 sets | |
| 60 min, 3 times a week | Foam roller quad release | 50 reps | |
| Foam roller TFL release | 50 reps | ||
| Foam roller and release | 50 reps | ||
| Weight knee extension | 10 reps × 3 sets | ||
| Single stand hip flex | 10 reps × 3 sets | ||
| One leg squat | 10 reps × 3 sets | ||
| One leg Y squat | 10 reps × 3 sets | ||
| Cool down | |||
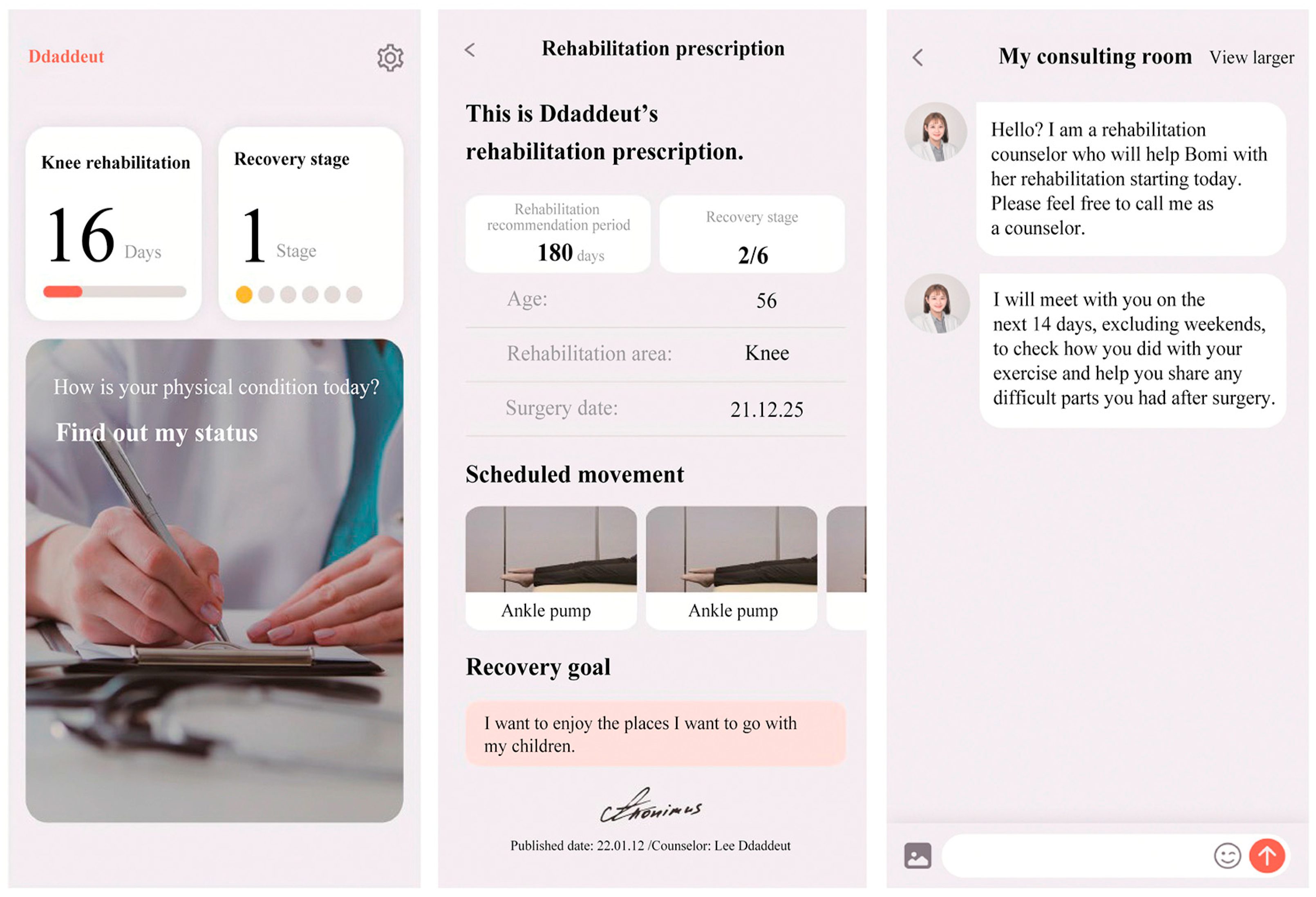
| App-based rehabilitation counselling program (B) | Until 12 weeks after discharge | Same as the above exercises Through 1:1 messenger, a professional counsellor checks the exercise method and progress according to the individual and encourages carrying out the exercises | |
| CPM, App-based rehabilitation counselling program (C) | 1–2 weeks 20–30 min, 3 times a week | 0°–100° | |
| 3–6 weeks 20–30 min, 3 times a week Until 12 weeks Same as the above exercises | 0°–140° | ||
| Preoperation | Postoperation, 2 Months | Postoperation, 3 Months | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group A (n = 14) | Group B (n = 14) | Group C (n = 14) | p Value † | Group A (n = 14) | Group B (n = 14) | Group C (n = 14) | p Value † | Group A (n = 14) | Group B (n = 14) | Group C (n = 14) | p Value † | p Values ‡ (Post Hoc by Scheffe) | |
| Muscle torque at 60°/s | |||||||||||||
| Peak torque at extension (N-m) | 34.55 ± 20.17 | 60.46 ± 37.09 | 54.79 ± 6.91 | 0.845 | 31.48 ± 12.53 | 46.78 ± 35.96 | 66.21 ± 400.01 | 0.041 * | 48.20 ± 20.51 | 60.78 ± 27.09 | 78.34 ± 40.48 | 0.043 * | A < C |
| Peak torque at flexion (N-m) | 34.95 ± 13.82 | 26.93 ± 21.44 | 30.49 ± 27.06 | 0.667 | 14.76 ± 12.54 | 32.66 ± 26.37 | 42.24 ± 29.08 | 0.014 * | 38.07 ± 26.27 | 28.61 ± 16.91 | 63.23 ± 44.95 | 0.018 * | A < C |
| Muscle torque at 180°/s | |||||||||||||
| Peak torque at extension (N-m) | 47.65 ± 14.71 | 42.81 ± 25.60 | 37.45 ± 34.57 | 0.644 | 20.27 ± 15.65 | 36.87 ± 31.29 | 39.63 ± 27.15 | 0.109 | 44.79 ± 19.93 | 36.44 ± 15.23 | 62.01 ± 46.49 | 0.090 | |
| Peak torque at flexion (N-m) | 24.44 ± 12.60 | 18.54 ± 14.33 | 21.50 ± 22.25 | 0.698 | 10.54 ± 10.88 | 20.81 ± 23.40 | 22.88 ± 22.25 | 0.219 | 28.21 ± 20.07 | 18.35 ± 12.56 | 49.29 ± 36.41 | 0.008 ** | A > C |
| Preoperation | Postoperation, 2 Months | Postoperation, 3 Months | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group A (n = 14) | Group B (n = 14) | Group C (n = 14) | p Value † | Group A (n = 14) | Group B (n = 14) | Group C (n = 14) | p Value † | Group A (n = 14) | Group B (n = 14) | Group C (n = 14) | p Value † | p Values ‡ (Post Hoc by Scheffe) | |
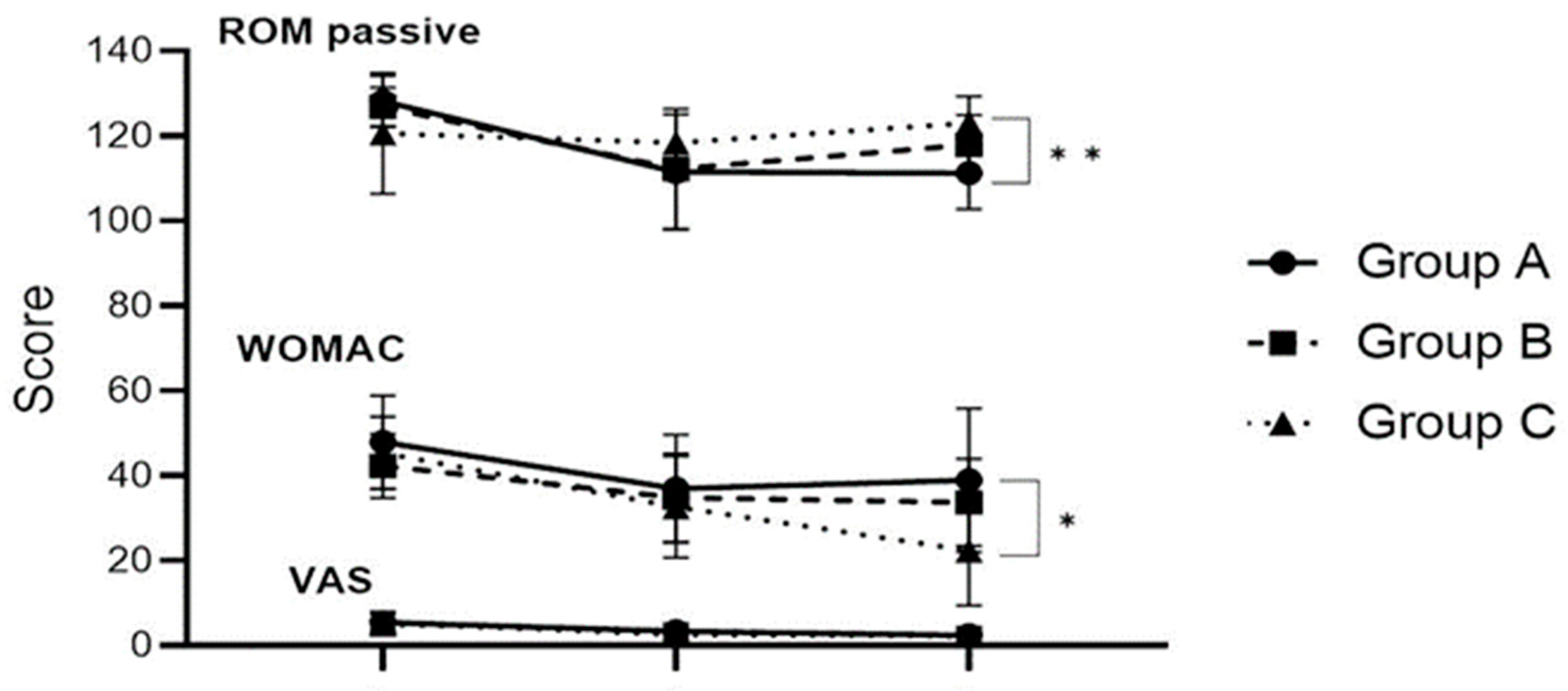
| ROM passive | 128.13 ± 5.94 | 126.82 ± 4.62 | 120.56 ± 14.24 | 0.195 | 111.50 ± 13.55 | 112.14 ± 14.10 | 118.33 ± 2.42 | 0.449 | 111.25 ± 8.56 | 117.86 ± 6.99 | 123.00 ± 6.33 | 0.004 ** | A < C |
| WOMAC | 47.91 ± 10.99 | 42.29 ± 7.63 | 45.31 ± 8.48 | 0.307 | 36.91 ± 12.68 | 34.77 ± 10.36 | 32.62 ± 11.94 | 0.669 | 38.91. ± 16.89 | 33.69 ± 10.25 | 22.38 ± 12.95 | 0.012 * | A > C |
| VAS | 5.45 ± 2.42 | 5.00 ± 1.18 | 5.31 ± 1.93 | 0.822 | 3.36 ± 1.80 | 3.46 ± 1.27 | 2.54 ± 1.39 | 0.240 | 2.38 ± 1.94 | 2.15 ± 1.14 | 2.23 ± 1.83 | 0.938 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, S.-H.; Kong, S.-H. A Pilot Study on the Efficacy of an App-Based Rehabilitation Counselling Program after Total Knee Arthroplasty. Healthcare 2024, 12, 1329. https://doi.org/10.3390/healthcare12131329
Han S-H, Kong S-H. A Pilot Study on the Efficacy of an App-Based Rehabilitation Counselling Program after Total Knee Arthroplasty. Healthcare. 2024; 12(13):1329. https://doi.org/10.3390/healthcare12131329
Chicago/Turabian StyleHan, Sang-Ho, and Se-Hee Kong. 2024. "A Pilot Study on the Efficacy of an App-Based Rehabilitation Counselling Program after Total Knee Arthroplasty" Healthcare 12, no. 13: 1329. https://doi.org/10.3390/healthcare12131329
APA StyleHan, S.-H., & Kong, S.-H. (2024). A Pilot Study on the Efficacy of an App-Based Rehabilitation Counselling Program after Total Knee Arthroplasty. Healthcare, 12(13), 1329. https://doi.org/10.3390/healthcare12131329






