Medical Resource Management in Emergency Hierarchical Diagnosis and Treatment Systems: A Research Framework
Abstract
:1. Introduction
2. Practices of Emergency Medical Resource Management in Representative Countries
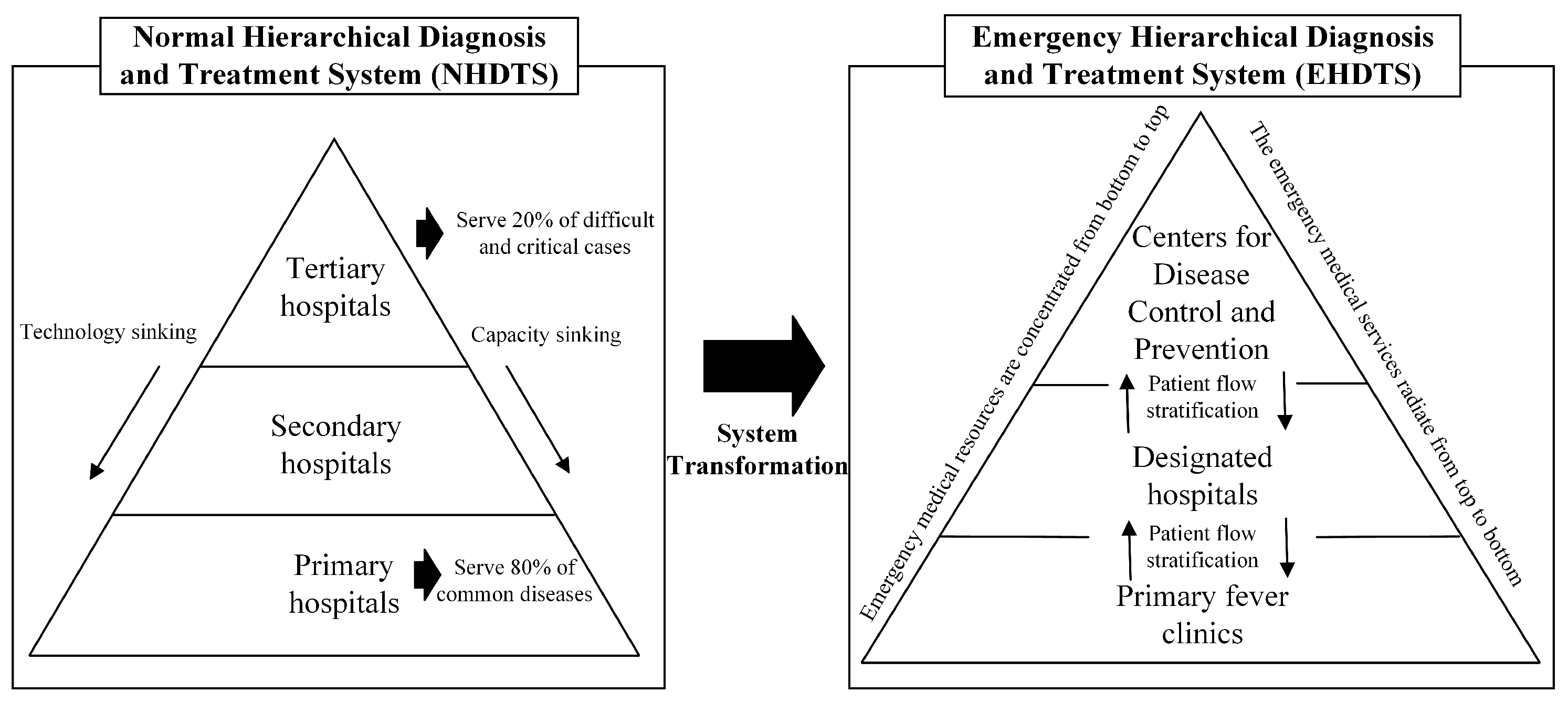
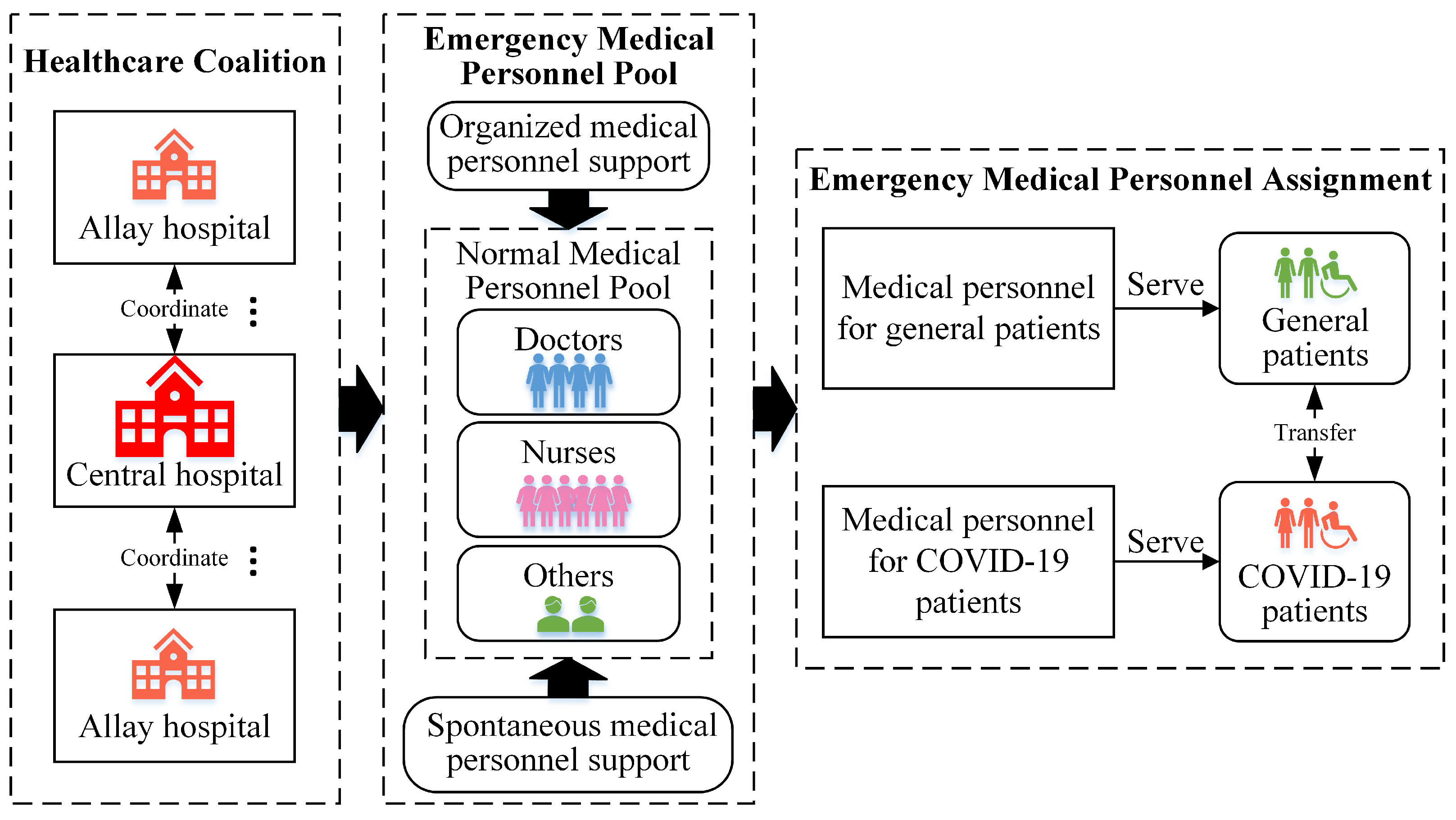
2.1. China
2.2. United States
2.3. Singapore
2.4. Germany
2.5. Summary
3. Literature Review
3.1. Medical Resource Allocation
3.2. Emergency Medical Resource Allocation
3.3. Medical Resource Management in Hierarchical Diagnosis and Treatment Systems
4. A Research Framework of Medical Resource Management in Emergency Hierarchical Diagnosis and Treatment Systems
4.1. Planning of Medical Resources in Emergency Hierarchical Diagnosis and Treatment Systems in the Early Stage of an Epidemic
4.2. Planning of Medical Resources in Emergency Hierarchical Diagnosis and Treatment Systems in the Outbreak Stage of the Epidemic
4.3. Planning of Medical Resources in Emergency Hierarchical Diagnosis and Treatment Systems in the Post-Epidemic Stage
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chowdhury, P.; Paul, S.K.; Kaisar, S.; Moktadir, M.A. COVID-19 pandemic related supply chain studies: A systematic review. Transp. Res. Part E Logist. Transp. Rev. 2021, 148, 102271. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Zhang, Y.; Guo, X. Research on the Equity and Influencing Factors of Medical and Health Resources Allocation in the Context of COVID-19: A Case of Taiyuan, China. Healthcare 2022, 10, 1319. [Google Scholar] [CrossRef] [PubMed]
- Xi, Y.; Ding, Y.; Cheng, Y.; Zhao, J.; Zhou, M.; Qin, S. Evaluation of the medical resource allocation: Evidence from China. Healthcare 2023, 11, 829. [Google Scholar] [CrossRef] [PubMed]
- Moynihan, R.; Sanders, S.; Michaleff, Z.A.; Scott, A.M.; Clark, J.; To, E.J.; Jones, M.; Kitchener, E.; Fox, M.; Johansson, M.; et al. Impact of COVID-19 pandemic on utilisation of healthcare services: A systematic review. BMJ Open 2021, 11, e045343. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Wang, A.; Wang, X.; Cheke, R.A.; Xiao, Y.; Tang, S. Impact of hospital bed shortages on the containment of COVID-19 in Wuhan. Int. J. Environ. Res. Public Health 2020, 17, 8560. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L. Research on the Current Situation of the Allocation of Public Health Human Resources in China. Int. J. Soc. Sci. Educ. Res. 2020, 3, 295–303. [Google Scholar]
- Pan, A.; Liu, L.; Wang, C.; Guo, H.; Hao, X.; Wang, Q.; Huang, J.; He, N.; Yu, H.; Lin, X.; et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA 2020, 323, 1915–1923. [Google Scholar] [CrossRef]
- Liu, W.; Yue, X.G.; Tchounwou, P.B. Response to the COVID-19 epidemic: The Chinese experience and implications for other countries. Int. J. Environ. Res. Public Health 2020, 17, 2304. [Google Scholar] [CrossRef]
- Luo, L.; Wang, Y.; Jiang, P.; Zhuo, M.; Wang, Q. Emergency medical service planning considering dynamic and stochastic demands of infected and non-infected patients during epidemics. J. Oper. Res. Soc. 2024, 75, 705–719. [Google Scholar] [CrossRef]
- He, X.; Luo, L.; Tang, X.; Wang, Q. Optimizing Large-Scale COVID-19 Nucleic Acid Testing with a Dynamic Testing Site Deployment Strategy. Healthcare 2023, 11, 393. [Google Scholar] [CrossRef]
- Holshue, M.L.; DeBolt, C.; Lindquist, S.; Lofy, K.H.; Wiesman, J.; Bruce, H.; Spitters, C.; Ericson, K.; Wilkerson, S.; Tural, A.; et al. First case of 2019 novel coronavirus in the United States. N. Engl. J. Med. 2020, 382, 929–936. [Google Scholar] [CrossRef] [PubMed]
- Michigan Gov. MDHHS activates Community Health Emergency Coordination Center in Response to 2019 Novel Coronavirus Local Health Departments Coordinating with State to Proactively Protect Public Health. 2020. Available online: https://www.michigan.gov/som/0,4669,7-192-29942_34762-518776--,00.html (accessed on 31 March 2024).
- Emanuel, E.J.; Persad, G.; Upshur, R.; Thome, B.; Parker, M.; Glickman, A.; Zhang, C.; Boyle, C.; Smith, M.; Phillips, J.P. Fair allocation of scarce medical resources in the time of COVID-19. N. Engl. J. Med. 2020, 382, 2049–2055. [Google Scholar] [CrossRef] [PubMed]
- Gaglione, D.; Braca, P.; Millefiori, L.M.; Soldi, G.; Forti, N.; Marano, S.; Willett, P.K.; Pattipati, K.R. Adaptive Bayesian learning and forecasting of epidemic evolution—Data analysis of the COVID-19 outbreak. IEEE Access 2020, 8, 175244–175264. [Google Scholar] [CrossRef]
- Facilities & Services. National Center of Infectious Diseases. 2020. Available online: https://www.ncid.sg/Facilities-Services/Pages/default.aspx (accessed on 31 March 2024).
- SPH Media Limited. Singapore Ramps up Facilities, Manpower for Coronavirus Battle. 2020. Available online: https://www.straitstimes.com/singapore/singapore-ramps-up-facilities-manpower-for-coronavirus-battle (accessed on 31 March 2024).
- Robert Koch Institute. Täglicher Lagebericht des RKI zur Coronavirus-Krankheit-2019. 2020. Available online: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020-05-07-de.pdf?__blob=publicationFile (accessed on 31 March 2024).
- Statistisches Bundesamt. Statistisches Jahrbuch 2019—Kapitel 4 Gesundheit. 2019. Available online: https://www.destatis.de/DE/Themen/Querschnitt/Jahrbuch/jb-gesundheit.pdf?__blob=publicationFile (accessed on 31 March 2024).
- Robert Koch Institute. Aufgaben der Kompetenzzentren in Deutschland. 2023. Available online: https://www.rki.de/DE/Content/Institut/institut_node (accessed on 31 March 2024).
- Smith-Daniels, V.L.; Schweikhart, S.B.; Smith-Daniels, D.E. Capacity management in health care services: Review and future research directions. Decis. Sci. 1988, 19, 889–919. [Google Scholar] [CrossRef]
- Jack, E.P.; Powers, T.L. A review and synthesis of demand management, capacity management and performance in health-care services. Int. J. Manag. Rev. 2009, 11, 149–174. [Google Scholar] [CrossRef]
- Lisac, M.; Blum, K.; Schlette, S. Changing long-established structures for more competition and stronger coordination: Health care reform in Germany in the new millennium. Intereconomics 2008, 43, 184–189. [Google Scholar] [CrossRef]
- Tobin-Tyler, E. In allocating scarce health care resources during COVID-19, don’t forget health justice. Health Affairs Forefront, 25 April 2020. [Google Scholar]
- Skedgel, C.; Wailoo, A.; Akehurst, R. Societal preferences for distributive justice in the allocation of health care resources: A latent class discrete choice experiment. Med. Decis. Mak. 2015, 35, 94–105. [Google Scholar] [CrossRef]
- Pu, L. Fairness of the distribution of public medical and health resources. Front. Public Health 2021, 9, 768728. [Google Scholar] [CrossRef] [PubMed]
- Jeon, B.Y.; Choi, S.M.; Kim, C.Y. Socioeconomic equity in regional distribution of health care resources in Korea. Health Policy Manag. 2012, 22, 85–108. [Google Scholar] [CrossRef]
- Monteiro, T.; Meskens, N.; Wang, T. Surgical scheduling with antagonistic human resource objectives. Int. J. Prod. Res. 2015, 53, 7434–7449. [Google Scholar] [CrossRef]
- Prot, D.; Lapègue, T.; Bellenguez-Morineau, O. A two-phase method for the shift design and personnel task scheduling problem with equity objective. Int. J. Prod. Res. 2015, 53, 7286–7298. [Google Scholar] [CrossRef]
- Wang, J.; Guo, H.; Bakker, M.; Tsui, K.L. An integrated approach for surgery scheduling under uncertainty. Comput. Ind. Eng. 2018, 118, 1–8. [Google Scholar] [CrossRef]
- Yemeke, T.T.; Kiracho, E.E.; Mutebi, A.; Apolot, R.R.; Ssebagereka, A.; Evans, D.R.; Ozawa, S. Health versus other sectors: Multisectoral resource allocation preferences in Mukono district, Uganda. PLoS ONE 2020, 15, e0235250. [Google Scholar] [CrossRef] [PubMed]
- Yi, M.; Peng, J.; Zhang, L.; Zhang, Y. Is the allocation of medical and health resources effective? Characteristic facts from regional heterogeneity in China. Int. J. Equity Health 2020, 19, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Caunhye, A.M.; Nie, X.; Pokharel, S. Optimization models in emergency logistics: A literature review. Socio-Econ. Plan. Sci. 2012, 46, 4–13. [Google Scholar] [CrossRef]
- Dasaklis, T.K.; Pappis, C.P.; Rachaniotis, N.P. Epidemics control and logistics operations: A review. Int. J. Prod. Econ. 2012, 139, 393–410. [Google Scholar] [CrossRef]
- Caunhye, A.M.; Zhang, Y.; Li, M.; Nie, X. A location-routing model for prepositioning and distributing emergency supplies. Transp. Res. Part E Logist. Transp. Rev. 2016, 90, 161–176. [Google Scholar] [CrossRef]
- Caunhye, A.M.; Nie, X. A stochastic programming model for casualty response planning during catastrophic health events. Transp. Sci. 2018, 52, 437–453. [Google Scholar] [CrossRef]
- Wang, Q.; Nie, X. A stochastic programming model for emergency supply planning considering traffic congestion. IISE Trans. 2019, 51, 910–920. [Google Scholar] [CrossRef]
- Wang, Q.; Nie, X. A stochastic programming model for emergency supply planning considering transportation network mitigation and traffic congestion. Socio-Econ. Plan. Sci. 2022, 79, 101119. [Google Scholar] [CrossRef]
- Wang, Q.; Reed, A.; Nie, X. Joint initial dispatching of official responders and registered volunteers during catastrophic mass-casualty incidents. Transp. Res. Part E Logist. Transp. Rev. 2022, 159, 102648. [Google Scholar] [CrossRef]
- Wang, Q.; Nie, X. A location-inventory-routing model for distributing emergency supplies. Transp. Res. Part E Logist. Transp. Rev. 2023, 175, 103156. [Google Scholar] [CrossRef]
- Yang, W.; Caunhye, A.M.; Zhuo, M.; Wang, Q. Integrated planning of emergency supply pre-positioning and victim evacuation. Socio-Econ. Plan. Sci. 2024, 95, 101965. [Google Scholar] [CrossRef]
- Ren, Y.; Ordóñez, F.; Wu, S. Optimal resource allocation response to a smallpox outbreak. Comput. Ind. Eng. 2013, 66, 325–337. [Google Scholar] [CrossRef]
- Araz, O.M.; Fowler, J.W.; Nafarrate, A.R. Optimizing service times for a public health emergency using a genetic algorithm: Locating dispensing sites and allocating medical staff. IIE Trans. Healthc. Syst. Eng. 2014, 4, 178–190. [Google Scholar] [CrossRef]
- Steiner, M.T.A.; Datta, D.; Neto, P.J.S.; Scarpin, C.T.; Figueira, J.R. Multi-objective optimization in partitioning the healthcare system of Parana State in Brazil. Omega 2015, 52, 53–64. [Google Scholar] [CrossRef]
- Yarmand, H.; Ivy, J.S.; Denton, B.; Lloyd, A.L. Optimal two-phase vaccine allocation to geographically different regions under uncertainty. Eur. J. Oper. Res. 2014, 233, 208–219. [Google Scholar] [CrossRef]
- Mete, H.O.; Zabinsky, Z.B. Stochastic optimization of medical supply location and distribution in disaster management. Int. J. Prod. Econ. 2010, 126, 76–84. [Google Scholar] [CrossRef]
- Koonin, L.M.; Pillai, S.; Kahn, E.B.; Moulia, D.; Patel, A. Strategies to inform allocation of stockpiled ventilators to healthcare facilities during a pandemic. Health Secur. 2020, 18, 69–74. [Google Scholar] [CrossRef]
- Rachaniotis, N.P.; Dasaklis, T.K.; Pappis, C.P. A deterministic resource scheduling model in epidemic control: A case study. Eur. J. Oper. Res. 2012, 216, 225–231. [Google Scholar] [CrossRef]
- Lee, B.Y.; Brown, S.T.; Korch, G.W.; Cooley, P.C.; Zimmerman, R.K.; Wheaton, W.D.; Zimmer, S.M.; Grefenstette, J.J.; Bailey, R.R.; Assi, T.M.; et al. A computer simulation of vaccine prioritization, allocation, and rationing during the 2009 H1N1 influenza pandemic. Vaccine 2010, 28, 4875–4879. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; de Véricourt, F.; Sun, P. Decentralized resource allocation to control an epidemic: A game theoretic approach. Math. Biosci. 2009, 222, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Koyuncu, M.; Erol, R. Optimal resource allocation model to mitigate the impact of pandemic influenza: A case study for Turkey. J. Med. Syst. 2010, 34, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Deng, Y.; Yuan, Z.; Zhang, C.; Zhang, F.; Cai, Q.; Gao, C.; Kurths, J. How to optimize the supply and allocation of medical emergency resources during public health emergencies. Front. Phys. 2020, 8, 383. [Google Scholar] [CrossRef]
- Savachkin, A.; Uribe, A. Dynamic redistribution of mitigation resources during influenza pandemics. Socio-Econ. Plan. Sci. 2012, 46, 33–45. [Google Scholar] [CrossRef]
- Mills, A.F.; Argon, N.T.; Ziya, S. Resource-based patient prioritization in mass-casualty incidents. Manuf. Serv. Oper. Manag. 2013, 15, 361–377. [Google Scholar] [CrossRef]
- Sung, I.; Lee, T. Optimal allocation of emergency medical resources in a mass casualty incident: Patient prioritization by column generation. Eur. J. Oper. Res. 2016, 252, 623–634. [Google Scholar] [CrossRef]
- Al-Shamsi, H.O.; Alhazzani, W.; Alhuraiji, A.; Coomes, E.A.; Chemaly, R.F.; Almuhanna, M.; Wolff, R.A.; Ibrahim, N.K.; Chua, M.L.; Hotte, S.J.; et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) pandemic: An international collaborative group. Oncologist 2020, 25, e936–e945. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Peng, S.; Xu, M. Emergency logistics network design based on space–time resource configuration. Knowl.-Based Syst. 2021, 223, 107041. [Google Scholar] [CrossRef]
- Wall, A.E.; Pruett, T.; Stock, P.; Testa, G. Coronavirus disease 2019: Utilizing an ethical framework for rationing absolutely scarce health-care resources in transplant allocation decisions. Am. J. Transplant. 2020, 20, 2332–2336. [Google Scholar] [CrossRef]
- Liu, Y.; Salwi, S.; Drolet, B.C. Multivalue ethical framework for fair global allocation of a COVID-19 vaccine. J. Med. Ethics 2020, 46, 499–501. [Google Scholar] [CrossRef] [PubMed]
- Tolchin, B.; Hull, S.C.; Kraschel, K. Triage and justice in an unjust pandemic: Ethical allocation of scarce medical resources in the setting of racial and socioeconomic disparities. J. Med. Ethics 2021, 47, 200–202. [Google Scholar] [CrossRef] [PubMed]
- Zaric, G.S.; Brandeau, M.L. Resource allocation for epidemic control over short time horizons. Math. Biosci. 2001, 171, 33–58. [Google Scholar] [CrossRef] [PubMed]
- Sun, P.; Yang, L.; De Véricourt, F. Selfish drug allocation for containing an international influenza pandemic at the onset. Oper. Res. 2009, 57, 1320–1332. [Google Scholar] [CrossRef]
- Marckmann, G.; Neitzke, G.; Schildmann, J.; Michalsen, A.; Dutzmann, J.; Hartog, C.; Jöbges, S.; Knochel, K.; Michels, G.; Pin, M.; et al. Decisions on the allocation of intensive care resources in the context of the COVID-19 pandemic: Clinical and ethical recommendations of DIVI, DGINA, DGAI, DGIIN, DGNI, DGP, DGP and AEM. German version. Med.-Klin.-Intensivmed. Und Notfallmedizin 2020, 115, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Worby, C.J.; Chang, H.H. Face mask use in the general population and optimal resource allocation during the COVID-19 pandemic. Nat. Commun. 2020, 11, 4049. [Google Scholar] [CrossRef] [PubMed]
- Ford, T.; Curiale, G.; Nguyen, T.N.; Aparicio, H.; Hamlyn, E.K.; Gangadhara, S.; Cervantes-Arslanian, A.M.; Greer, D.; Romero, J.R.; Shulman, J.G. Optimization of resources and modifications in acute ischemic stroke care in response to the global COVID-19 pandemic. J. Stroke Cerebrovasc. Dis. 2020, 29, 104980. [Google Scholar] [CrossRef]
- Hou, C.; Jiang, H. Methodology of emergency medical logistics for multiple epidemic areas in public health emergency. PLoS ONE 2021, 16, e0253978. [Google Scholar] [CrossRef]
- Barr, B.; Bambra, C.; Whitehead, M. The impact of NHS resource allocation policy on health inequalities in England 2001–2011: Longitudinal ecological study. BMJ 2014, 348, g3231. [Google Scholar] [CrossRef]
- Wang, J.J.; Li, Z.P.; Shi, J.J. Hospital referral and capacity strategies in the two-tier healthcare systems. Omega 2021, 100, 102229. [Google Scholar] [CrossRef]
- Wang, Q.; Liu, Z.; Jiang, P.; Luo, L. A stochastic programming model for emergency supplies pre-positioning, transshipment and procurement in a regional healthcare coalition. Socio-Econ. Plan. Sci. 2022, 82, 101279. [Google Scholar] [CrossRef]
- Pan, X.; Song, J.; Zhang, B. Dynamic Resource Allocation in a Hierarchical Appointment System: Optimal Structure and Heuristics. IEEE Trans. Autom. Sci. Eng. 2020, 17, 1501–1515. [Google Scholar] [CrossRef]
- Qiu, Y.; Song, J.; Liu, Z. A simulation optimisation on the hierarchical health care delivery system patient flow based on multi-fidelity models. Int. J. Prod. Res. 2016, 54, 6478–6493. [Google Scholar] [CrossRef]
- Luo, L.; Wan, X.; Wang, Q. A multi-period location–allocation model for integrated management of emergency medical supplies and infected patients during epidemics. Comput. Ind. Eng. 2022, 173, 108640. [Google Scholar] [CrossRef]
- Wichmann, B.; Wichmann, R. Nonparametric estimation of a primary care production function in urban Brazil. Health Econ. Rev. 2020, 10, 1–10. [Google Scholar]
- Zhang, S.; Su, X.; Wang, J.; Chen, M.; Li, C.; Li, T.; Ge, S.; Xia, N. Nucleic acid testing for coronavirus disease 2019: Demand, research progression, and perspective. Crit. Rev. Anal. Chem. 2022, 52, 413–424. [Google Scholar] [CrossRef]
- Mutlu, S.; Benneyan, J.; Terrell, J.; Jordan, V.; Turkcan, A. A co-availability scheduling model for coordinating multi-disciplinary care teams. Int. J. Prod. Res. 2015, 53, 7226–7237. [Google Scholar] [CrossRef]
- Van den Broek, J.; Boselie, P.; Paauwe, J. Cooperative innovation through a talent management pool: A qualitative study on coopetition in healthcare. Eur. Manag. J. 2018, 36, 135–144. [Google Scholar] [CrossRef]
- Fügener, A.; Brunner, J.O.; Podtschaske, A. Duty and workstation rostering considering preferences and fairness: A case study at a department of anaesthesiology. Int. J. Prod. Res. 2015, 53, 7465–7487. [Google Scholar] [CrossRef]
- Mousa, S.K.; Othman, M. The impact of green human resource management practices on sustainable performance in healthcare organisations: A conceptual framework. J. Clean. Prod. 2020, 243, 118595. [Google Scholar] [CrossRef]



| Features | NHDTS | EHDTS |
|---|---|---|
| Demand predictability | Easy, high certainty | Hard, high uncertainty |
| Relevant people | General patients | General patients, infected patients |
| Local medical personnel | Local and non-local medical personnel | |
| Supply shortage risk | Low | High |
| Time urgency | Low | High |
| Inventory | Normal, relatively short term | Emergency, relatively long term |
| Distribution | Regular, no delay | Flexible, delay possible |
| Cross-regional support | Less | More |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luo, L.; Zhang, R.; Zhuo, M.; Shan, R.; Yu, Z.; Li, W.; Wu, P.; Sun, X.; Wang, Q. Medical Resource Management in Emergency Hierarchical Diagnosis and Treatment Systems: A Research Framework. Healthcare 2024, 12, 1358. https://doi.org/10.3390/healthcare12131358
Luo L, Zhang R, Zhuo M, Shan R, Yu Z, Li W, Wu P, Sun X, Wang Q. Medical Resource Management in Emergency Hierarchical Diagnosis and Treatment Systems: A Research Framework. Healthcare. 2024; 12(13):1358. https://doi.org/10.3390/healthcare12131358
Chicago/Turabian StyleLuo, Li, Renshan Zhang, Maolin Zhuo, Renbang Shan, Zhoutianqi Yu, Weimin Li, Peng Wu, Xin Sun, and Qingyi Wang. 2024. "Medical Resource Management in Emergency Hierarchical Diagnosis and Treatment Systems: A Research Framework" Healthcare 12, no. 13: 1358. https://doi.org/10.3390/healthcare12131358







