Analysis of Urinary Incontinence in the Neurogenic Bladder and Its Relationship with the Satisfaction and Lifestyle of People with SCI
Abstract
:1. Introduction
2. Materials and Methods
- -
- Normal urination: voluntary onset of urination without reflex, bladder compression, or stimulation;
- -
- Voluntary bladder reflex stimulation: tapping the bladder area and stretching the body to facilitate drainage;
- -
- Involuntary bladder reflex stimulation: incontinent in diapers or in collector and no perception of urination;
- -
- Bladder compression (straining): abdominal straining and Valsalva maneuver;
- -
- External compression: Credé maneuver and manual pressure in the suprapubic region;
- -
- Intermittent bladder catheterization: periodically inserting a catheter through the urethra into the bladder to allow urine to drain. The technique can be performed by the individual with SCI, known as self-catheterization, or by third parties, known as assisted catheterization;
- -
- Indwelling bladder catheter: a long-term catheter that remains inside the bladder. It can be inserted through the urethra, known as an indwelling transurethral catheter, or surgically inserted through the abdominal wall, known as an indwelling suprapubic catheter;
- -
- Non-continent urinary diversion/ostomy-stoma/diversion of urine through an opening created in the abdomen and Mitrofanoff.
3. Results
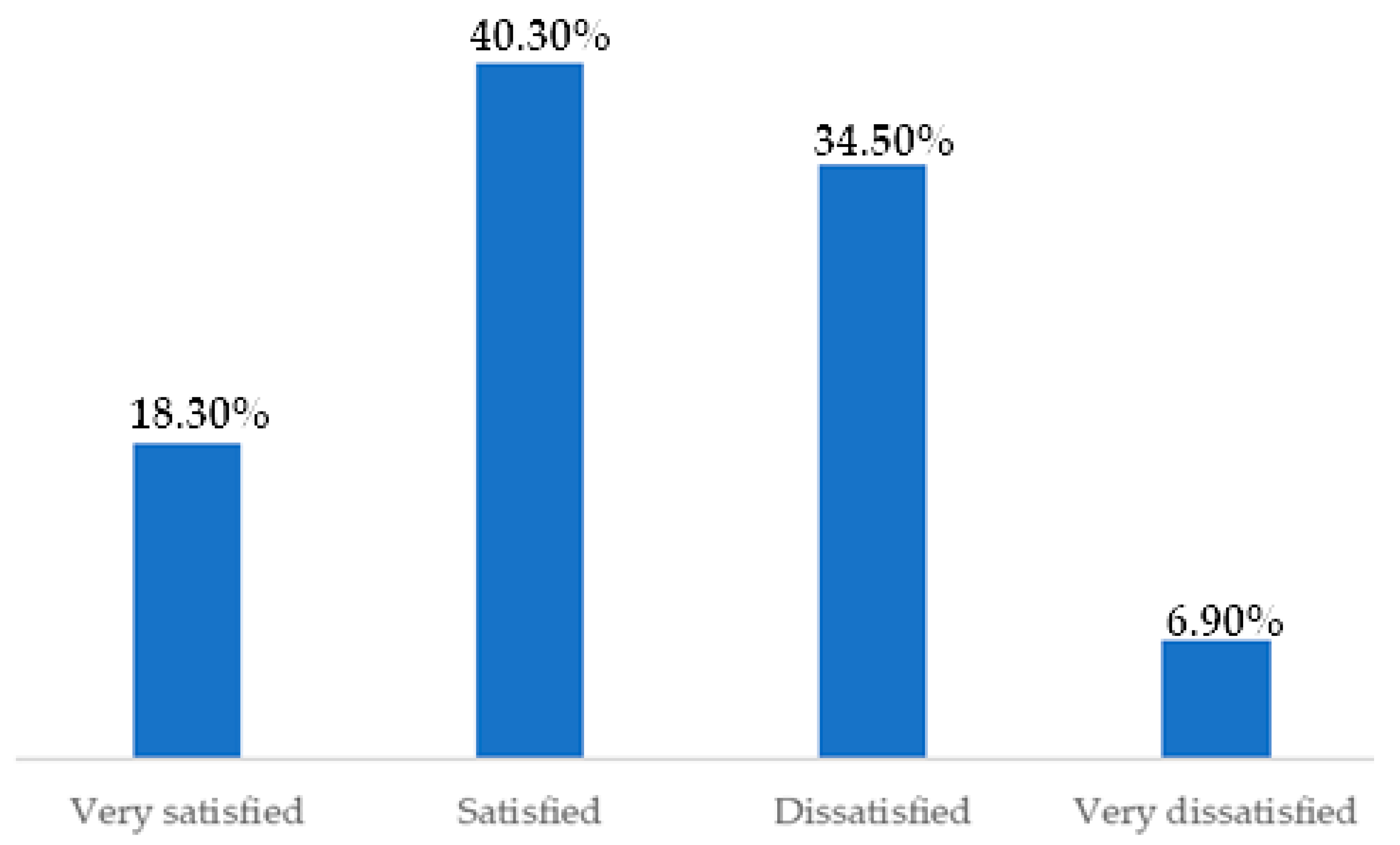
Satisfaction, Lifestyle, and the Relationship with UI
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Taweel, W.; Seyam, R. Neurogenic bladder in spinal cord injury patients. Res. Rep. Urol. 2015, 7, 85–99. [Google Scholar] [CrossRef] [PubMed]
- Cordeiro, A. Tradução, Adaptação e Validação Para o Português Brasileiro do Data Set do Trato Urinário Inferior Para Pessoas com Lesão Medular. Master’s Thesis, Universidade de São Paulo, Ribeirão, Preto, 2017. [Google Scholar]
- Hansen, R.B.; Biering-Sorensen, F.; Kristensen, J.K. Urinary incontinence in spinal cord injured individuals 10–45 years after injury. Spinal Cord. 2010, 48, 27–33. [Google Scholar] [CrossRef]
- Salvático, K.T.; Lopes, A.; Davatz, G.C. Atualização Sobre a Assistência de Enfermagem aos Pacientes com Trauma Raquimedular. Rev. Publicadas FIJ-Até 2022, 1, 2–15. Available online: http://portal.fundacaojau.edu.br:8077/journal/index.php/revistasanteriores/article/view/396 (accessed on 9 October 2019).
- Groen, J.; Pannek, J.; Diaz, D.C.; Del Popolo, G.; Gross, T.; Hamid, R.; Blok, B. Summary of European Association of Urology (EAU) Guidelines on Neuro-Urology. Eur. Urol. 2016, 69, 324–333. [Google Scholar] [CrossRef] [PubMed]
- Martins, N.G.; Mussi, H.G.; Queiroz, J.G.V.; de Cunha, B.S.; Santos, F.A.; dos Rodrigues, G.J.R.; Tavares, L.L.; Silva, G.C. Trauma raquimedular e a conduta urológica cirúrgica. Rev. Eletrônica Acervo Saúde 2023, 2, e14777. [Google Scholar] [CrossRef]
- Tang, D.H.; Colayco, D.; Piercy, J.; Patel, V.; Globe, D.; Chancellor, M.B. Impact of urinary incontinence on health-related quality of life, daily activities, and healthcare resource utilization in patients with neurogenic detrusor overactivity. BMC Neurol. 2014, 14, 74. [Google Scholar] [CrossRef]
- Jazayeri, S.B.; Beygi, S.; Shokraneh, F.; Hagen, E.M.; RahimiMovaghar, V. Incidence of traumatic spinal cord injury worldwide: A systematic review. Eur. Spine J. 2015, 24, 905–918. [Google Scholar] [CrossRef]
- Lee, B.B.; Cripps, R.A.; Fitzharris, M.; Wing, P.C. The global map for traumatic spinal cord injury epidemiology: Update 2011, global incidence rate. Spinal Cord 2014, 52, 110–116. [Google Scholar] [CrossRef]
- National Spinal Cord Injury Statistical Center. Facts and Figures at a Glance; Annual Report; University of Alabama at Birmingham: Birmingham, AL, USA, 2020. [Google Scholar]
- Hamid, R.; Averbeck, M.A.; Chiang, H.; Garcia, A.; Al Mousa, R.T.; Oh, S.J.; Del Popolo, G. Epidemiology and pathophysiology of neurogenic bladder after spinal cord injury. World J. Urol. 2018, 36, 1517–1527. [Google Scholar] [CrossRef] [PubMed]
- Rabadi, M.H.; Aston, C. Evaluate the impact of neurogenic bladder in veterans with traumatic spinal cord injury. J. Spinal Cord. Med. 2016, 39, 175–179. [Google Scholar] [CrossRef]
- Patel, D.P.; Lenherr, S.M.; Stoffel, J.T.; Elliott, S.P.; Welk, B.; Presson, A.P.; Neurogenic Bladder Research Group. Study protocol: Patient reported outcomes for bladder management strategies in spinal cord injury. BMC Urol. 2017, 17, 95. [Google Scholar] [CrossRef]
- Pelosi, G.; Faleiros, F.; Pereira, M.R.C.; Bimbatti, K.D.F.; Tholl, A.D. Study on the prevalence of neurogenic bladder in Brazilians with traumatic and non-traumatic spinal cord injury. J. Spinal Cord. Med. 2021, 46, 677–681. [Google Scholar] [CrossRef]
- Cruz, T.F.; de Araújo AH, I.M.; Mendes, M.I.D.O.I. Enfrentamento do auto cateterismo vesical no lesionado medular: Uma revisão da literatura. Rev. JRG De Estud. Acadêmicos 2021, 4, 35–50. [Google Scholar]
- Faleiros, F. Pessoas com Lesão Medular no Brasil: O Uso de Mídias Sociais na Investigação do Itinerário Terapêutico, Dificuldades e Anseios por Pesquisas. Tese de Livre-Docência, Escola de Enfermagem de Ribeirão Preto/USP, Ribeirão Preto, Brasil, 2019. [Google Scholar]
- Bolfarine, H.; Bussab, W.O. Elementos de Amostragem; Edgard Blucher: São Paulo, Brazil, 2005. [Google Scholar]
- DeVivo, M.J.; Biering-Sørensen, F.; New, P.; Chen, Y. Standardization of data analysis and reporting of results from the International Spinal Cord Injury Core Data Set. Spinal Cord. 2010, 49, 596–599. [Google Scholar] [CrossRef]
- Tate, D. Development of a measure to assess bowel and bladder dysfunction. In Proceedings of the 4th ISCoS and ASIA Joint Scientific Meeting, Montreal, QC, Canada, 14–16 May 2015. [Google Scholar]
- Braga, D.C.O. Disfunção Vesical na Qualidade de vida de Pessoas com Lesão Medular: Tradução, Adaptação e Validação de um Instrumento. 117 f. Tese (Doutorado em Enfermagem), Faculdade de Farmácia, Odontologia e Enfermagem, Universidade Federal do Ceará, Fortaleza, Brazil, 2018. [Google Scholar]
- Middleton, J.; Ramakrishnan, K.; Cameron, I. Management of the Neurogenic Bladder for Adults with Spinal Cord Injuries. Available online: https://www.researchgate.net/publication/283634117_Management_of_the_Neurogenic_Bladder_for_Adults_with_Spinal_Cord_Injuries (accessed on 9 October 2019).
- Wyndaele, J.-J. The management of neurogenic lower urinary tract dysfunction after spinal cord injury. Nat. Rev. Urol. 2016, 13, 705–714. [Google Scholar] [CrossRef] [PubMed]
- Drake, M.J.; Apostolidis, A.; Cocci, A.; Emmanuel, A.; Gajewski, J.B.; Harrison, S.C.; Heesakkers, J.P.; Lemack, G.E.; Madersbacher, H.; Panicker, J.N.; et al. Neurogenic lower urinary tract dysfunction: Clinical management recommendations of the Neurologic Incontinence committee of the fifth International Consultation on Incontinence 2013. Neurourol. Urodyn. 2016, 35, 657–665. [Google Scholar] [CrossRef] [PubMed]
- Elmelund, M.; Klarskov, N.; Biering-Sørensen, F. Prevalence of urinary incontinence in women with spinal cord injury. Spinal Cord. 2018, 56, 1124–1133. [Google Scholar] [CrossRef] [PubMed]
- Biering-Sørensen, F.; Kennelly, M.; Kessler, T.M.; Linsenmeyer, T.; Pannek, J.; Vogel, L.; Wyndaele, J.-J. International Spinal Cord Injury Lower Urinary Tract Function Basic Data Set (version 2.0). Spinal Cord. Ser. Cases 2018, 4, 60. [Google Scholar] [CrossRef]
- Liu, C.-W.; Attar, K.H.; Gall, A.; Shah, J.; Craggs, M. The relationship between bladder management and health-related quality of life in patients with spinal cord injury in the UK. Spinal Cord. 2009, 48, 319–324. [Google Scholar] [CrossRef]
- Hicken, B.L.; Putzke, J.D.; Richards, J.S. Bladder management and quality of life after spinal cord injury. Am. J. Phys. Med. Rehabil. 2001, 80, 916–919. [Google Scholar] [CrossRef]
- Nascimento, J. Cateterismo intermitente limpo: Estratégia para o cuidado ao lesado medular em serviço ambulatorial de reabilitação. In Proceedings of the Congresso Paulista De Estomaterapia, Online, 11–12 October 2020; Available online: https://anais.sobest.com.br/cpe/article/view/23 (accessed on 1 March 2021).
- Machado, W.C.A. Enfermagem de reabilitação: Uma questão de demanda da sociedade e lacuna no âmbito da saúde coletiva e enfermagem internacional. Enferm. Bras. 2023, 22, 1–5. [Google Scholar] [CrossRef]
- Cooper, J.; Chisolm, D.; McLeod, D.J. Sociodemographic Characteristics, Health Literacy, and Care Compliance in Families with Spina Bifida. Glob. Pediatr. Health 2017, 4, 2333794X17745765. [Google Scholar] [CrossRef] [PubMed]
- Pignone, M.; DeWalt, D.A.; Sheridan, S.; Berkman, N.; Lohr, K.N. Interventions to improve health outcomes for patients with low literacy: A systematic review. J. Gen. Intern. Med. 2005, 20, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Romo, P.G.B.; Smith, C.P.; Cox, A.; Averbeck, M.A.; Dowling, C.; Beckford, C.; Cameron, A.P. Non-surgical urologic management of neurogenic bladder after spinal cord injury. Word J. Urol. 2018, 36, 1555–1568. [Google Scholar] [CrossRef] [PubMed]
- Myers, J.B.; Lenherr, S.M.; Stoffel, J.T.; Elliott, S.P.; Presson, A.P.; Zhang, C.; Welk, B. Patient reported bladder-related symptoms and quality of life after spinal cord injury with different bladder management strategies. J. Urol. 2019, 202, 574–584. [Google Scholar] [CrossRef] [PubMed]
- Braaf, S.; Lennox, A.; Nunn, A.; Gabbe, B. Social activity and relationship changes experienced by people with bowel and bladder dysfunction following spinal cord injury. Spinal Cord. 2017, 55, 679–686. [Google Scholar] [CrossRef] [PubMed]
- Faleiros, F.; de Oliveira Braga, D.C.; Schoeller, S.D.; Henriques, S.H.; Cunha, N.B.F.; Videira, L.G.N.; da Silva Grillo, A.C.L. Surveying people with spinal cord injuries in Brazil to ascertain research priorities. Sci Rep. 2023, 13, 654. [Google Scholar] [CrossRef]
| Bladder-Emptying Method | Main Method | Complementary Method | ||
|---|---|---|---|---|
| N | % | N | % | |
| Normal urination | 32 | 11 | 2 | 0.7 |
| Voluntary and involuntary bladder reflex triggering | 14 | 5.1 | 2 | 0.7 |
| Bladder compression through forced effort (abdominal pressure and Valsalva maneuver) and external compression (Credé maneuver and manual pressure in the suprapubic region) | 16 | 4.5 | 11 | 3.4 |
| Clean intermittent catheterization (self-catheterization and assisted catheterization) | 214 | 74.1 | 7 | 2.4 |
| Indwelling transurethral and suprapubic bladder catheterization | 11 | 3.7 | - | - |
| Non-continent urinary diversion/ostomy | 1 | 0.3 | - | - |
| Management Method\Incontinence | Yes | No | p-Value | OR | CI 95% | ||
|---|---|---|---|---|---|---|---|
| N | % | N | % | ||||
| Normal urination | 13 | 38.2 | 21 | 61.8 | 0.046 1 | 2.23 | [1.08; 4.77] |
| Bladder reflex triggering | 13 | 86.7 | 2 | 13.3 | 0.015 2 | 0.18 | [0.03; 0.67] |
| Bladder compression | 15 | 55.5 | 12 | 44.5 | 0.999 1 | 1.01 | [0.45; 2.23] |
| Intermittent catheterization | 130 | 59.1 | 90 | 40.9 | 0.054 1 | 0.56 | [0.32; 0.97] |
| Causes of Dissatisfaction with Bladder-Emptying Routine | N | % |
|---|---|---|
| Difficulties related to bladder-emptying method | 59 | 49.1 |
| Related to UI | 50 | 41.7 |
| Architectural barriers | 19 | 15.8 |
| Psychological difficulties | 13 | 4.5 |
| Related to urinary tract infection | 12 | 4.1 |
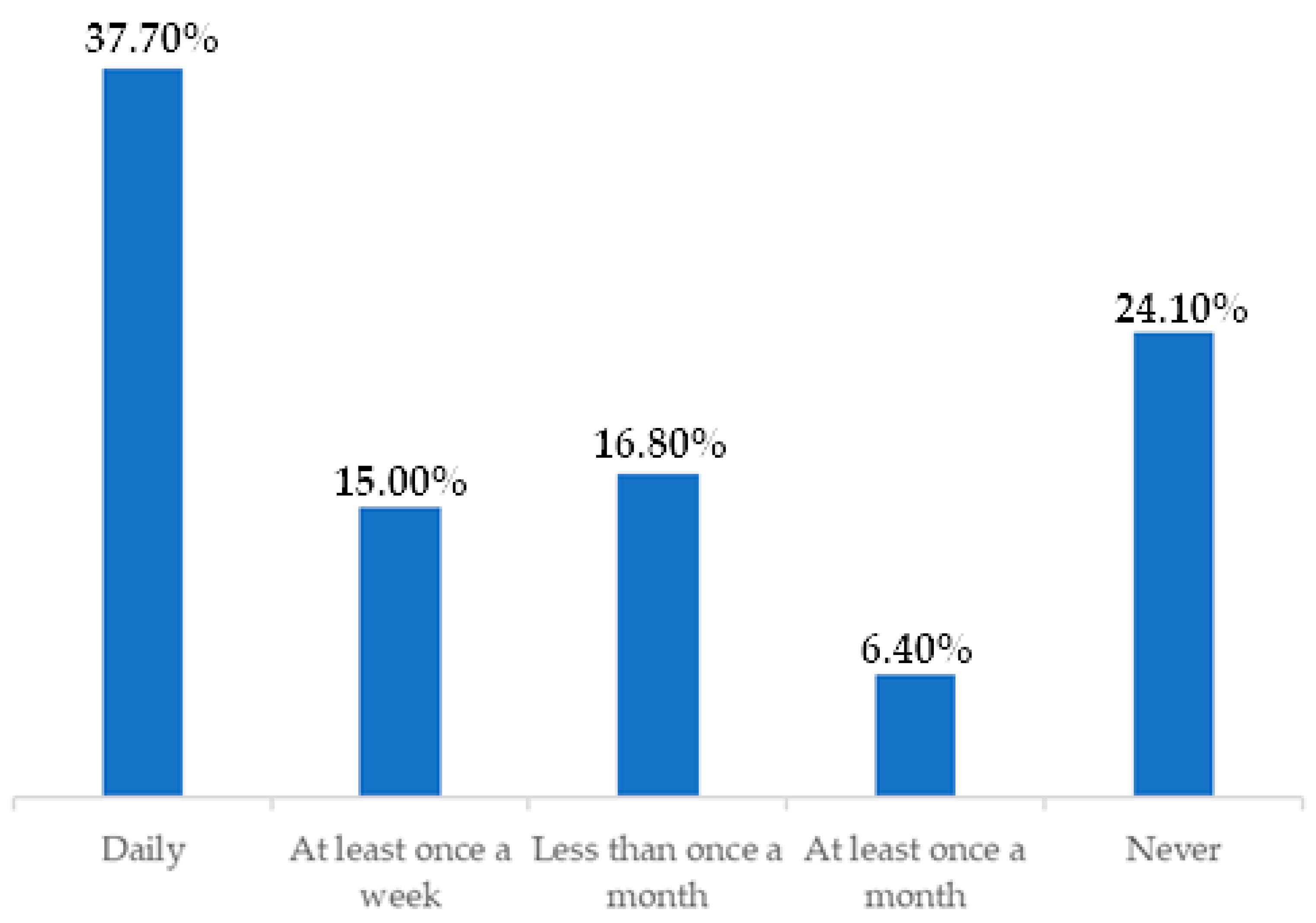
| Lifestyle Changes Due to Urine Leakage | N | % |
|---|---|---|
| None | 58 | 36.0 |
| Less than once a month | 22 | 13.7 |
| At least once a month | 17 | 10.6 |
| At least once a week | 19 | 11.8 |
| Daily | 45 | 28.0 |
| Satisfaction and Lifestyle\Incontinence | Yes | No | p-Value | |||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Effects of bladder problems on QoL | No effect | 16 | 9.9% | 24 | 18.8 | 0.008 |
| Little effect | 37 | 23.0% | 36 | 28.1 | ||
| Some effect | 33 | 20.5% | 32 | 25.0 | ||
| Severe effect | 75 | 46.6% | 36 | 28.1 | ||
| Bladder management prevents me from working outside the home or doing routine activities | Not at all | 55 | 34.2% | 77 | 60.2 | <0.001 |
| Somewhat | 63 | 39.1% | 35 | 27.3 | ||
| Very much | 43 | 26.7% | 16 | 12.5 | ||
| Bladder management negatively affects my personal relationships | Not at all | 61 | 37.9% | 76 | 59.4 | 0.001 |
| Somewhat | 55 | 34.2% | 26 | 20.3 | ||
| Very much | 45 | 28.0% | 26 | 20.3 | ||
| Bladder management negatively affects my social life | Not at all | 56 | 34.8% | 71 | 55.5 | 0.002 |
| Somewhat | 69 | 42.9% | 39 | 30.5% | ||
| Very much | 36 | 22.4% | 18 | 14.1% | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neves Videira, L.G.; Corbo, L.N.; de Avila, M.A.G.; Martins, G.P.; Schoeller, S.D.; Kappler, C.; Faleiros, F. Analysis of Urinary Incontinence in the Neurogenic Bladder and Its Relationship with the Satisfaction and Lifestyle of People with SCI. Healthcare 2024, 12, 1501. https://doi.org/10.3390/healthcare12151501
Neves Videira LG, Corbo LN, de Avila MAG, Martins GP, Schoeller SD, Kappler C, Faleiros F. Analysis of Urinary Incontinence in the Neurogenic Bladder and Its Relationship with the Satisfaction and Lifestyle of People with SCI. Healthcare. 2024; 12(15):1501. https://doi.org/10.3390/healthcare12151501
Chicago/Turabian StyleNeves Videira, Lorena Gomes, Letícia Noelle Corbo, Marla Andreia Garcia de Avila, Giovana Pelosi Martins, Soraia Dornelles Schoeller, Christoph Kappler, and Fabiana Faleiros. 2024. "Analysis of Urinary Incontinence in the Neurogenic Bladder and Its Relationship with the Satisfaction and Lifestyle of People with SCI" Healthcare 12, no. 15: 1501. https://doi.org/10.3390/healthcare12151501







