Oral Health-Related Quality of Life among Refugees: A Questionnaire-Based Study
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design and Ethics Statement
2.2. Data Collection
2.3. Questionnaire Design
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Harper, D. Online Etymology Dictionary. 2023. Available online: https://www.etymonline.com/word/asylum (accessed on 1 May 2024).
- Loescher, G. ‘Refugees: A Short History’, Refugees: A Very Short Introduction, Very Short Introductions; Oxford Academic: Oxford, UK, 2021. [Google Scholar]
- UNHCR. Global Trends Report, Forced Displacement in 2022. Available online: https://www.unhcr.org/sites/default/files/2023-06/global-trends-report-2022.pdf (accessed on 30 July 2024).
- Größte Herkunftsländer von Flüchtlingen 2022. 2023. Available online: https://de.statista.com/statistik/daten/studie/186108/umfrage/herkunftslaender-von-fluechtlingen (accessed on 1 May 2024).
- Cousins, S. Experts sound alarm as Syrian crisis fuels spread of tuberculosis. BMJ 2014, 349, g7397. [Google Scholar] [CrossRef] [PubMed]
- Sá, F.H.L.; Waikamp, V.; Freitas, L.H.M.; Baeza, F.L.C. Mental health outcomes in Syrian refugees: A systematic review. Int. J. Soc. Psychiatry 2022, 68, 933–953. [Google Scholar] [CrossRef] [PubMed]
- Turner, R.; PLOS Medicine editors. Migrants and refugees: Improving health and well-being in a world on the move. PLoS Med. 2019, 16, e1002876. [Google Scholar] [CrossRef] [PubMed]
- Javanbakht, A.; Grasser, L.R.; Kim, S.; Arfken, C.L.; Nugent, N. Perceived health, adversity, and posttraumatic stress disorder in Syrian and Iraqi refugees. Int. J. Soc. Psychiatry 2022, 68, 118–128. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Satomai, I.; Mansfield, C.J. Oral Health in North Carolina: Relationship with General Health and Behavioral Risk Factors. North Carol. Med. J. 2015, 76, 142–147. [Google Scholar]
- Saltaji, H. Oral health consequences of the crisis in Syria. Br. Dent. J. 2015, 219, 49. [Google Scholar] [CrossRef] [PubMed]
- Kisely, S. No Mental Health without Oral Health. Can. J. Psychiatry 2016, 61, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Network, V.R.H. Oral Health 2023. Available online: https://refugeehealthnetwork.org.au/?s=oral (accessed on 1 May 2024).
- Ronald, C.; Southall, D. Refugee Health: An Approach to Emergency Situations. BMJ 1999, 318. [Google Scholar] [CrossRef] [PubMed]
- Roucka, T.M. Access to dental care in two long-term refugee camps in western Tanzania; programme development and assessment. Int. Dent. J. 2011, 61, 109–115. [Google Scholar] [CrossRef]
- Salim, N.A.; ElSa’aideh, B.B.; Maayta, W.A.; Hassona, Y.M. Dental services provided to Syrian refugee children in Jordan: A retrospective study. Spec. Care Dentist. 2020, 40, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Zinah, E.; Al-Ibrahim, H.M. Oral health problems facing refugees in Europe: A scoping review. BMC Public Health 2021, 21, 1207. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Heydecke, G. Patientenbasierte Messgrössen: Mundgesundheitsbezogene Lebensqualität. Swiss Dental J. 2002, 112, 6. [Google Scholar]
- Spura, A.; Kleinke, M.; Robra, B.P.; Ladebeck, N. Wie erleben Asylsuchende den Zugang zu medizinischer Versorgung? [How do asylum seekers experience access to medical care?]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2017, 60, 462–470. (In German) [Google Scholar] [CrossRef] [PubMed]
- Slade, G.D.; Spencer, A.J. Development and evaluation of the Oral Health Impact Profile. Community Dent. Health 1994, 11, 3–11. [Google Scholar] [PubMed]
- John, M.T.; Miglioretti, D.L.; LeResche, L.; Koepsell, T.D.; Hujoel, P.; Micheelis, W. German short forms of the Oral Health Impact Profile. Community Dent. Oral Epidemiol. 2006, 34, 277–288. [Google Scholar] [CrossRef] [PubMed]
- John, M.T.; Micheelis, W.; Biffar, R. Normwerte mundgesundheitsbezogener Lebensqualität für Kurzversionen des Oral Health, Impact Profile. Schweiz Monatsschr Zahnmed 2004, 114, 784–791. [Google Scholar] [PubMed]
- Reissmann, D.R. Methodological considerations when measuring oral health-related quality of life. J. Oral Rehabil. 2021, 48, 233–245. [Google Scholar] [CrossRef] [PubMed]
- Solyman, M.; Schmidt-Westhausen, A.M. Oral health status among newly arrived refugees in Germany: A cross-sectional study. BMC Oral Health 2018, 18, 132. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
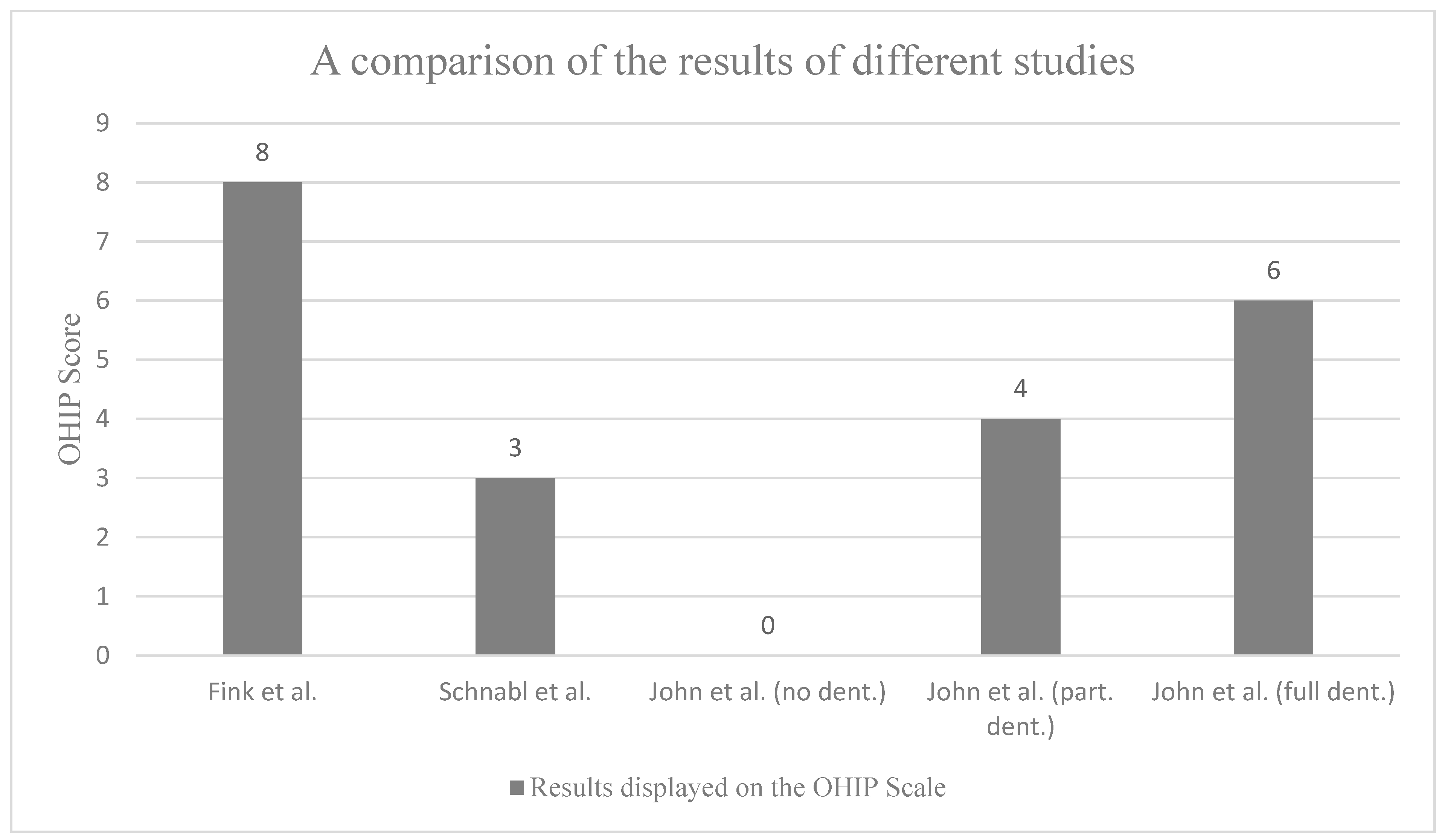
- Schnabl, D.; Sandbichler, P.; Neumaier, M.; Girstmair, J.; Barbieri, F.; Kapferer-Seebacher, I.; Steiner, R.; Laimer, J.; Grunert, I. Dental Students’ Oral Health-Related Quality of Life and Temporomandibular Dysfunction-Self-Rating versus Clinical Assessment. Healthcare 2021, 9, 1348. [Google Scholar] [CrossRef] [PubMed]
- Agudelo-Suárez, A.A.; Vivares-Builes, A.M.; Muñoz-Pino, N.; Martínez-Martínez, J.M.; Reid, A.; Ronda-Pérez, E. Oral Health-Related Quality of Life in Native and Immigrant Populations in the PELFI Study in Spain. Int. J. Environ. Res. Public Health 2019, 16, 1796. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Saadeh, R.; Cappelli, D.; Bober-Moken, I.; Cothron, A.; de la Torre, M. Assessing Oral Health Status, Practices, and Access to Care among War-Affected Refugees Living in San Antonio, Texas. Eur. J. Dent. 2020, 14, 371–379. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Navabi, N.; Nakhaee, N.; Mirzadeh, A. Validation of a Persian Version of the Oral Health Impact Profile (OHIP-14). Iran J. Public Health 2010, 39, 135–139. [Google Scholar] [PubMed]
- Banihashem Rad, S.A.; Esteves Oliveira, M.; Maklennan, A.; Castiglia, P.; Campus, G. Higher prevalence of dental caries and periodontal problems among refugees: A scoping review. J. Glob. Health 2023, 13, 04111. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Worbs, S.; Rother, N.; Kreienbrink, A. Syrische Migranten in Deutschland als bedeutsame neue Bevölkerungsgruppe. Informationsdienst Soz. Indik. 2019, 61, 2–6. [Google Scholar]
- Thirunavukkarasu, A.; Alotaibi, A.; Al-Hazmi, A.; ALruwaili, B.; Alomair, M.; Alshaman, W.; Alshaman, W.H.; Alkhamis, A.M. Assessment of Oral Health-Related Quality of Life and Its Associated Factors among the Young Adults of Saudi Arabia: A Multicenter Study. Biomed. Res. Int. 2022, 2022, 5945518. [Google Scholar] [CrossRef]
- Aarabi, G.; Reissmann, D.R.; Seedorf, U.; Becher, H.; Heydecke, G.; Kofahl, C. Oral health and access to dental care—A comparison of elderly migrants and non-migrants in Germany. Ethn. Health 2017, 23, 703–717. [Google Scholar] [CrossRef] [PubMed]
- Haj-Younes, J.; Strømme, E.; Igland, J.; Abildsnes, E.; Kumar, B.; Hasha, W.; Diaz, E. Use of health care services among Syrian refugees migrating to Norway: A prospective longitudinal study. BMC Health Serv. Res. 2021, 21, 572. [Google Scholar] [CrossRef]
- Koçak, A.; Vergiveren, Ö. Group-Based Communication: Contents and Practices of WhatsApp Group Use by Generations and Genders. Online J. Commun. Media Technol. 2019, 9, e201922. [Google Scholar] [CrossRef]
- Park, K.; Murphy, S.; Mcgrath, C.; Ging, D. The Impact of the Use of Social Media on Women and Girls; European Union: Maastricht, The Netherlands, 2023. [Google Scholar]
| Age (years) | Median (IQR) | 23 (20–29) |
| Minimum | 15 | |
| Maximum | 75 | |
| Sex | Male | 32.1% |
| Female | 66.2% | |
| Not applicable | 1.7% | |
| Country of origin | North Africa (Libya, Egypt, Morocco, Tunisia, Algeria, Sudan) | 4% |
| East Africa (South Sudan, Tanzania) | 0.4% | |
| Arabian Peninsula (Yemen, Qatar, Oman, Saudi Arabia, United Arab Emirates, Kuwait) | 3.1% | |
| Middle East (Iraq, Jordan, Lebanon, Syria, Israel) | 83.9% | |
| Not applicable | 0.8% |
| Domains | OHIP Scores Median (IQR) | OHIP Questions | Never (%) | Hardly (%) | Now and Then (%) | Often (%) | Very Often (%) |
|---|---|---|---|---|---|---|---|
| Total OHIP-14 | 8 (2–17) | ||||||
| Domain 1: Functional limitation | 0 (0–1) | Had difficulties pronouncing words | 78.6 | 10.2 | 6.0 | 3.5 | 1.7 |
| Felt limitation in sense of taste | 84.3 | 10.2 | 3.5 | 0.7 | 1.2 | ||
| Domain 2: Physical pain | 2 (0–4) | Felt pain in oral region | 34.4 | 21.4 | 28.4 | 8.0 | 7.7 |
| Felt uncomfortable eating certain foods | 53.4 | 14.7 | 20.0 | 6.0 | 6.0 | ||
| Domain 3: Psychological discomfort | 1 (0–3) | Felt insecure related to your teeth or dentures | 46.1 | 16.0 | 23.7 | 6.7 | 7.5 |
| Felt tense | 61.3 | 15.0 | 13.2 | 5.2 | 5.2 | ||
| Domain 4: Physical disability | 1 (0–3) | Felt diet has been unsatisfactory | 58.6 | 8.0 | 17.0 | 7.7 | 8.7 |
| Had to interrupt meals | 59.6 | 17.5 | 15.2 | 4.5 | 3.2 | ||
| Domain 5: Psychological disability | 1 (0–3) | Had difficulties relaxing | 56.6 | 13.0 | 16.5 | 7.5 | 6.5 |
| Felt embarrassed | 58.4 | 12.7 | 13.7 | 8.0 | 7.2 | ||
| Domain 6: Social disability | 0 (0–3) | Felt irritated by others | 63.1 | 11.7 | 13.0 | 5.5 | 6.7 |
| Had difficulty with daily routine | 66.3 | 14.2 | 12.0 | 4.2 | 3.2 | ||
| Domain 7: Handicap | 0 (0–2) | Felt life in general less satisfying | 61.8 | 11.0 | 15.2 | 4.5 | 7.5 |
| Been totally unable to function | 78.3 | 10.5 | 6.2 | 2.5 | 2.5 |
| Overall | OHIP 0–2 | OHIP 3–8 | OHIP 9–17 | OHIP > 18 | p | |
|---|---|---|---|---|---|---|
| Professional cleaning 1×/year | 59.9% | 63.0% | 62.3% | 62.6% | 53.1% | 0.239 |
| Brushing at least 2×/day | 52.1% | 55.6% * | 58.5% * | 43.3% * | 44.8% * | 0.035 * |
| Manual toothbrush at least 2×/day | 44.9% | 44.5% | 50.0% | 36.3% | 43.8% | 0.258 |
| Electric toothbrush at least 2×/day | 11.0% | 13.0% | 10.3% | 9.9% | 5.2% | 0.274 |
| Interdental cleaning at least 1×/day | 33.8% | 28.2% | 38.2% | 38.1% | 27.5% | 0.952 |
| Interdental brushes at least 1×/day | 19.8% | 16.7% | 23.6% | 25.3% | 14.0% | 0.399 |
| Tooth floss at least 1×/day | 16.3% | 15.7% | 17.9% | 18.7% | 11.4% | 0.254 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fink, K.; Alkayed, K.; Schwindling, F.S.; Wiesmüller, V. Oral Health-Related Quality of Life among Refugees: A Questionnaire-Based Study. Healthcare 2024, 12, 1525. https://doi.org/10.3390/healthcare12151525
Fink K, Alkayed K, Schwindling FS, Wiesmüller V. Oral Health-Related Quality of Life among Refugees: A Questionnaire-Based Study. Healthcare. 2024; 12(15):1525. https://doi.org/10.3390/healthcare12151525
Chicago/Turabian StyleFink, Katharina, Kais Alkayed, Franz Sebastian Schwindling, and Vera Wiesmüller. 2024. "Oral Health-Related Quality of Life among Refugees: A Questionnaire-Based Study" Healthcare 12, no. 15: 1525. https://doi.org/10.3390/healthcare12151525
APA StyleFink, K., Alkayed, K., Schwindling, F. S., & Wiesmüller, V. (2024). Oral Health-Related Quality of Life among Refugees: A Questionnaire-Based Study. Healthcare, 12(15), 1525. https://doi.org/10.3390/healthcare12151525






