Using Immersive Environments in E-Mental Health Rehabilitation Programs Directed to Future Health Professionals to Promote Empathy and Health Literacy about Schizophrenia
Abstract
1. Introduction
1.1. Mental Health Literacy
1.2. The Sense of Presence in Immersive Environments
- Perceptual Realism: The fidelity of sensory information in VR, including visual, auditory, and haptic feedback, greatly influences the sense of presence. High-quality graphics, spatial audio, and responsive haptic feedback contribute to a more immersive experience.
- Immersion: The extent to which participants can suspend disbelief and become fully engaged with the virtual environment is a crucial factor in generating presence. Immersion often entails a sense of agency, where participants feel in control of their actions within the virtual world.
- Spatial Cues: Accurate spatial mapping, tracking of head and body movements, and consistent feedback from the virtual environment contribute to participants’ sense of presence. These cues help create a coherent and convincing virtual experience.
- Immersion and Engagement: A heightened sense of presence can result in increased participant immersion and emotional engagement within the virtual environment. This enhanced immersion allows participants to emotionally connect with the content.
- Emotional Transfer: In VR, emotions can be transferred from the virtual world to the participant. This transfer is facilitated by the vivid sensory input, including visuals, audio, and haptic feedback, creating a sense of emotional contagion within the virtual space.
- Presence and Realism: The more realistic the virtual environment, the more it can evoke emotional responses. Realistic environments and characters are more likely to elicit emotions such as fear, joy, or empathy.
- Fear and Anxiety: Horror games and simulations can evoke strong feelings of fear and anxiety, often heightened by a strong sense of presence. Participants may feel genuinely threatened, despite being aware that it is a virtual experience.
- Empathy and Compassion: VR can cultivate empathy by enabling participants to embody different characters or immerse themselves in scenarios that evoke compassion, such as witnessing the experiences of refugees or victims of natural disasters.
- Joy and Awe: VR can transport participants to breathtaking landscapes or provide surreal experiences, evoking feelings of joy, awe, and wonder.
- Discomfort and Nausea: While VR can evoke positive emotions, it can also cause discomfort, motion sickness, or anxiety in some individuals, affecting the sense of presence and emotional responses.
- Interaction with the environment: The sense of presence in immersive environments arises from participants feeling like an integral part of the virtual environment. When individuals interact with this environment in a meaningful way, whether in games, simulations, or training, they experience emotions more intensely and authentically [44]. For example, in a virtual reality environment that simulates an amusement park, participants can experience excitement and joy similar to what they would feel in a real park.
- Empathy and emotional connection: In immersive environments, the sense of presence can be so strong that participants develop empathy with virtual characters or simulated situations. This can lead to the creation of emotions such as sympathy, compassion, or anger, depending on the narrative or interactions in the virtual environment [45]. For example, in a simulation of social injustice situations, participants may experience indignation, which can influence their real-world attitudes.
- Learning and therapeutic exposure: In training and therapy contexts, the sense of presence in immersive environments is often utilized to create controlled experiences that evoke desired emotions and attitudes. For example, in exposure therapy for post-traumatic stress disorder (PTSD), an immersive environment can assist patients in safely revisiting traumatic situations, thereby reducing associated anxiety and fear.
- Influence on attitudes and behaviors: The sense of presence experienced in immersive environments can impact participants attitudes and behaviors [46]. If someone undergoes a simulation highlighting the dangers of driving under the influence of alcohol, it can lead to a positive attitude change towards not driving under the influence, ultimately influencing their real-world behavior.
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Procedures
2.4. Instrumentation
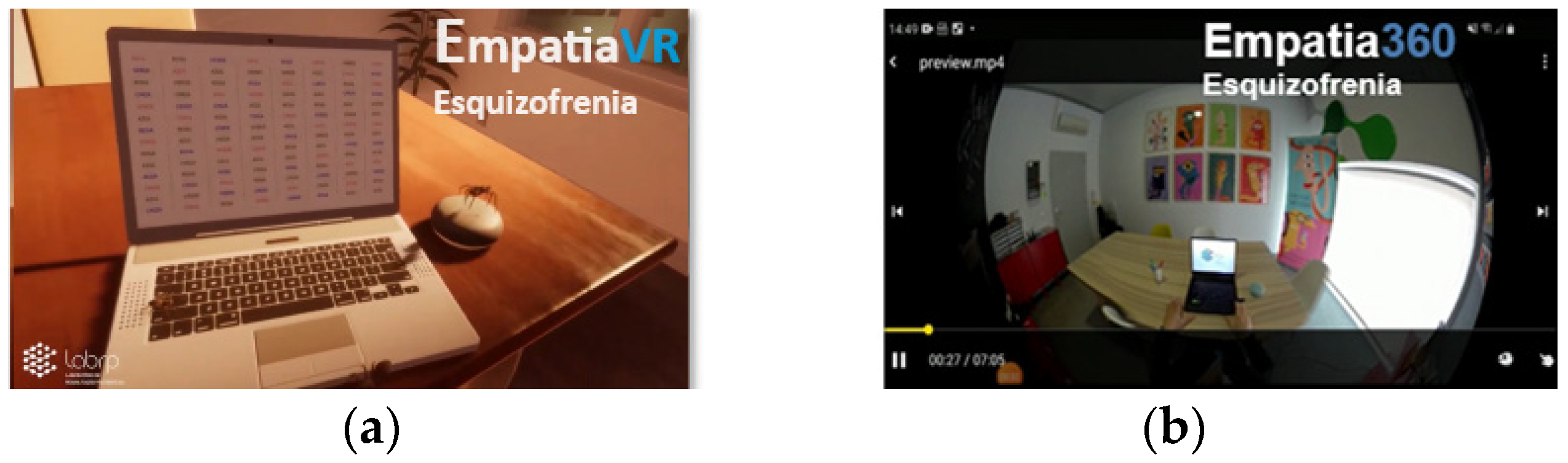
2.4.1. Immersive Environments
2.4.2. Immersive Narrative
- The announcer’s voice indicating and explaining the tasks to be carried out.
- Voices that suggested the participant perform certain actions or discouraged them from the task they were performing.
- Simulated heartbeat and breathing, with sound and intensity gradually increasing throughout the experience.
- Noise from television not tuned to any channel.
- Short periods of blurred vision.
- Movement of the images of the paintings on the wall.
- Glare from windows, lamps, and objects.
- TV screen that turns on and off by itself.
- Spiders that came out from behind the computer and moved across the table towards the participant.
2.4.3. The Virtual Doppelganger Questionnaire
- The dependent measure of “Empathic feelings for people suffering from schizophrenia” uses an index of 12 items. Participants had to rate how well a series of adjectives described their emotions toward people suffering from schizophrenia (rated from 1 = “Not at all”, to 7 = “Extremely”). This measure is related to how the participant felt when thinking about people with schizophrenia (people who hear voices and have delusions that are false ideas or beliefs, even when there is evidence that they are not real). A higher score reflects greater empathy.
- The dependent measure of “The social distance scale” uses an index of 7 items (rated from 0 = “Definitely unwilling” to 3 = “Definitely willing”) and refers to the participant’s interaction with a person with schizophrenia. A decrease in the score reflects a decrease in social distance, suggesting an enhanced interaction with individuals diagnosed with schizophrenia.
- The dependent measure “Attitudes toward people with schizophrenia” uses an index of 7 items (rated in a 9-point scale from 1 = “Strongly disagree” to 9 = “Strongly agree”) and was applied to assess participants attitudes toward people with schizophrenia. A higher score indicates a more positive attitude.
- The simulation evaluation uses an index of 5 items (rated from 9-point scale from 1 = “Strongly disagree” to 7 = “Strongly agree”). This measure was applied after exposure and is related to the reactions of the participant to simulation. A higher score indicates a more positive reaction to the simulation environment.
2.4.4. The Igroup Presence Questionnaire
- The dependent measure of “global presence” uses an index of 1 item (the item G1 was rated from 1 = “not at all” to 5 = “very much”). This measure is related to the feeling of global presence. A higher score indicates a stronger feeling of presence within the virtual environment.
- The dependent measure of “spatial presence” uses an index of 5 items, (the items SP1, SP2, SP4 and SP5 were rated from 1 = “fully disagree” to 5 = “fully agree”; the item SP3 was rated from 1 = “did not feel” to 5 = “felt present”). This measure pertains to the participant’s sensation of physical presence within the virtual environment. In the items SP1, SP4 and SP5, a higher score indicates a stronger sense of presence within the virtual environment; in the items SP2 and SP3, a lower higher score indicates a stronger sense of presence within the virtual environment. The calculation of this component is performed as follows:After this calculation, a higher score indicates greater spatial presence.spatial presence = ((SP1 + SP4 + SP5 + G1) + (−1 × SP2 + 6) + (−1 × SP3 + 6))/6
- The dependent measure of “involvement” uses an index of 4 items, (the item INV1 was rated from 1 = “extremely aware” to 5 = “not aware at all”; the items INV2, INV3 and INV4 were rated from 1 = “fully disagree” to 5 = “fully agree”). This measure pertains to the participant’s attention paid to the virtual environment and experienced engagement. In the items INV2 and INV4, a higher score indicates a greater engagement with the immersive environment, in the items INV1 and INV3 a lower score indicates a greater engagement with the immersive environment. The calculation of this component is performed as follows:After this calculation, a higher score indicates greater involvement.involvement = ((INV2 + INV4) + (−1 × INV1 + 6) + (−1 × INV3 + 6))/4
- The dependent measure of “realism” uses an index of 4 items (the item REAL1 was rated from 1 = “completely real” to 5 = “not real at all”; the item REAL2 was rated from 1 = “not consistent” to 5 = “very consistent”; the item REAL3 was rated from 1 = “about as real as an imagined world” to 5 = “indistinguishable from the real world”; the item REAL4 was rated from 1 = “fully disagree” to 5 = “fully agree”). This measure pertains to the participant’s subjective experience of realism encountered in the virtual environment. A higher score indicates a greater realism of the immersive environment. The calculation of this component is performed as follows:realism = (REAL1 + REAL2 + REAL3 + REAL4)/4
2.4.5. Psychophysiological Data
3. Results
3.1. Virtual Doppelganger Questionnaire
3.2. The Igroup Presence Questionnaire
3.3. Physiological Data
4. Discussion
4.1. Virtual Doppelganger Questionnaire
4.2. Igroup Presence Questionnaire
4.3. Heart Rate Signals and Electrodermal Activity
4.4. Limitations
4.5. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jablensky, A. The diagnostic concept of schizophrenia: Its history, evolution, and future prospects. Dialogues Clin. Neurosci. 2010, 12, 271–287. [Google Scholar] [CrossRef] [PubMed]
- Alonso, J.; Buron, A.; Bruffaerts, R.; He, Y.; Posada-Villa, J.; Lepine, J.-P.; Angermeyer, M.C.; Levinson, D. Association of Perceived Stigma and Mood and Anxiety Disorders: Results from the World Mental Health Surveys. Acta Psychiatr. Scand. 2008, 118, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Brohan, E.; Elgie, R.; Sartorius, N.; Thornicroft, G. Self-stigma, empowerment and perceived discrimination among people with schizophrenia in 14 European countries: The GAMIAN-Europe study. Schizophr. Res. 2010, 122, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Link, B.G.; Yang, L.H.; Phelan, J.C.; Collins, P.Y. Measuring mental illness stigma. Schizophr. Bull. 2004, 30, 511–541. [Google Scholar] [CrossRef] [PubMed]
- Dhungana, S.; Tulachan, P.; Chapagai, M.; Pant, S.B.; Lama, P.Y.; Upadhyaya, S. Internalized stigma in patients with schizophrenia: A hospital-based cross-sectional study from Nepal. PLoS ONE 2022, 17, e0264466. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Lee, M.T.Y.; Chiu, M.Y.L.; Kleinman, A. Experience of social stigma by people with schizophrenia in Hong Kong. Br. J. Psychiatry 2005, 186, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Hoftman, G.D. The Burden of Mental Illness Beyond Clinical Symptoms: Impact of Stigma on the Onset and Course of Schizophrenia Spectrum Disorders. Am. J. Psychiatry Resid. J. 2016, 11, 5–7. [Google Scholar] [CrossRef]
- Prokop-Dorner, A.; Flis, M. Experience of courtesy stigma among relatives of individuals with schizophrenia—A qualitative study. Psychiatr. Pol. 2021, 55, 835–850. [Google Scholar] [CrossRef] [PubMed]
- Fung, K.M.T.; Tsang, H.W.H.; Corrigan, P.W. Self-stigma of people with schizophrenia as predictor of their adherence to psychosocial treatment. Psychiatr. Rehabil. J. 2008, 32, 95–104. [Google Scholar] [CrossRef]
- Fresán, A.; Robles-García, R.; Martínez-López, N.; Tovilla-Zárate, C.A.; Madrigal, E. Stigma and perceived aggression towards schizophrenia in female students of medicine and psychology. Salud Ment. 2018, 41, 207–212. [Google Scholar] [CrossRef]
- Rössler, W. The stigma of mental disorders: A millennia-long history of social exclusion and prejudices. EMBO Rep. 2016, 17, 1250–1253. [Google Scholar] [CrossRef]
- Rivera-Segarra, E.; Varas-Díaz, N.; Santos-figueroa, A. “That’s all Fake”: Health professionals stigma and physical healthcare of people living with Serious Mental Illness. PLoS ONE 2019, 14, e0226401. [Google Scholar] [CrossRef] [PubMed]
- Valery, K.; Prouteau, A. EPV0826 Comprehensive rehabilitation and resocialization in mental health care after surgery of head and neck tumors EPV0825 Schizophrenia stigma in mental health professionals and associated factors: A systematic review EPV0828 Paralization and online a. Eur. Psychiatry 2022, 65, S617. [Google Scholar] [CrossRef]
- Tesfaw, G.; Kibru, B.; Ayano, G. Prevalence and factors associated with higher levels of perceived stigma among people with schizophrenia Addis Ababa. Int. J. Ment. Health Syst. 2020, 14, 19. [Google Scholar] [CrossRef] [PubMed]
- Queirós, R.V.; Santos, V.; Madeira, N. Decrease in Stigma Towards Mental Illness in Portuguese Medical Students After a Psychiatry Course Redução do Estigma Face à Doença Mental Após Frequência de Aulas de Psiquiatria em Estudantes de Medicina Portugueses. Acta Med. Port. 2021, 34, 498–506. [Google Scholar] [CrossRef] [PubMed]
- Saguem, B.N.; Rhouma, A.; Nakhli, J. Stigma of mental illness and its association with empathic abilities in mental health trainees. Stigma Health 2022, 7, 423–431. [Google Scholar] [CrossRef]
- Knolhoff, Q.A. The Role of Contact and Empathy in Stigma toward Individuals with Mental Illness among Mental Health and Non-Mental Health Professionals. Master’s Thesis, Eastern Illinois University, Charleston, IL, USA, 2018. [Google Scholar]
- Vaghee, S.; Hashemi, B.M.; Lotfabadi, M.K.; Salarhaji, A.; Vaghei, N.; Feizi, M. The Relationship between Empathy and Stigma towards Psychiatric Disorders among Nursing Students. Future Med. Educ. J. 2018, 8, 38–43. [Google Scholar] [CrossRef]
- Riess, H. The Science of Empathy. J. Patient Exp. 2017, 4, 74–77. [Google Scholar] [CrossRef] [PubMed]
- Ringwald, W.R.; Wright, A.G.C. The affiliative role of empathy in everyday interpersonal interactions. Eur. J. Pers. 2021, 35, 197–211. [Google Scholar] [CrossRef]
- Moudatsou, M.; Stavropoulou, A.; Philalithis, A.; Koukouli, S. The Role of Empathy in Health and Social Care Professionals. Healthcare 2020, 8, 26. [Google Scholar] [CrossRef]
- Yu, C.C.; Tan, L.; Le, M.K.; Tang, B.; Liaw, S.Y.; Tierney, T.; Ho, Y.Y.; Lim, E.E.; Lim, D.; Ng, R.; et al. The development of empathy in the healthcare setting: A qualitative approach. BMC Med. Educ. 2022, 22, 245. [Google Scholar] [CrossRef] [PubMed]
- Formosa, N.J.; Morrison, B.W.; Hill, G.; Stone, D. Testing the efficacy of a virtual reality-based simulation in enhancing users’ knowledge, attitudes, and empathy relating to psychosis. Aust. J. Psychol. 2020, 70, 57–65. [Google Scholar] [CrossRef]
- Marques, A.J.; Veloso Gomes, P.; Pimenta, R.; Pereira, A.S.; Silva, C.F. Impact of a Virtual Reality-Based Simulation on Empathy and Attitudes Toward Schizophrenia. Front. Psychol. 2022, 13, 814984. [Google Scholar] [CrossRef] [PubMed]
- Tay, J.L.; Xie, H.; Sim, K. Effectiveness of Augmented and Virtual Reality-Based Interventions in Improving Knowledge, Attitudes, Empathy and Stigma Regarding People with Mental Illnesses—A Scoping Review. J. Pers. Med. 2023, 13, 112. [Google Scholar] [CrossRef] [PubMed]
- Zare-bidaki, M.; Ehteshampour, A.; Reisaliakbarighomi, M.; Mazinani, R.; Ardakani, M.; Mirabzadeh, A.; Alikhani, R.; Noroozi, M.; Momeni, F.; Samani, A.; et al. Evaluating the Effects of Experiencing Virtual Reality Simulation of Psychosis on Mental Illness Stigma, Empathy, and Knowledge in Medical Students. Front. Psychiatry 2022, 13, 880331. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, D.; McKechnie, J.; Edgerton, E.; Wilson, C. Immersive Virtual Reality as a Pedagogical Tool in Education: A Systematic Literature Review of Quantitative Learning Outcomes and Experimental Design; Springer: Berlin/Heidelberg, Germany, 2021; Volume 8. [Google Scholar]
- Wu, Y.; Zhang, M.; Li, X.; Gan, Y.; Zhao, C. Augment Reality-Based Teaching Practice. Biomed. Eng. Educ. 2021, 1, 237–241. [Google Scholar] [CrossRef]
- Lee, Y.; Kim, S.K.; Eom, M. Usability of mental illness simulation involving scenarios with patients with schizophrenia via immersive virtual reality: A mixed methods study. PLoS ONE 2020, 15, e0238437. [Google Scholar] [CrossRef]
- Ando, S.; Clement, S.; Barley, E.A.; Thornicroft, G. The simulation of hallucinations to reduce the stigma of schizophrenia: A systematic review. Schizophr. Res. 2011, 133, 8–16. [Google Scholar] [CrossRef]
- Jorm, A.F.; Korten, A.E.; Jacomb, P.A.; Christensen, H.; Rodgers, B.; Pollitt, P. “Mental health literacy”: A survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med. J. Aust. 1997, 166, 182–186. [Google Scholar] [CrossRef]
- Jorm, A. Mental health literacy. Public knowledge and beliefs about mental disorders. Br. J. Psychiatry 2000, 177, 396–401. [Google Scholar] [CrossRef]
- Jorm, A.F. The concept of mental health literacy. In International Handbook of Health Literacy: Research, Practice and Policy Across the Life-Span; Okan, O., Bauer, U., Levin-zamir, D., Pinheiro, P., Sørensen, K., Eds.; Policy Press: Bristol, UK, 2019; pp. 53–66. [Google Scholar]
- Hojat, M. Empathy in Patient Care: Antecedents, Development, Measurement, and Outcomes; Springer: New York, NY, USA, 2007. [Google Scholar]
- Guidi, C.; Traversa, C. Empathy in patient care: From ‘Clinical Empathy’ to ‘Empathic Concern’. Med. Health Care Philos. 2021, 24, 573–585. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, I.P.; Dores, A.R. Clinical Communication in Rehabilitation. Int. J. Environ. Res. Public Health 2022, 19, 7268. [Google Scholar] [CrossRef] [PubMed]
- Diemer, J.; Alpers, G.W.; Peperkorn, H.M.; Shiban, Y.; Mühlberger, A. The impact of perception and presence on emotional reactions: A review of research in virtual reality. Front. Psychol. 2015, 6, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Vives, M.V.; Slater, M. From presence to consciousness through virtual reality. Nat. Rev. Neurosci. 2005, 6, 332–339. [Google Scholar] [CrossRef] [PubMed]
- Bohil, C.; Owen, C.; Jeong, E.; Alicea, B.; Biocca, F. Virtual Reality and Presence. In 21st Century Communication: A Reference Handbook; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2009; pp. 534–542. [Google Scholar]
- Slater, M.; Wilbur, S. A Framework for Immersive Virtual Environments (FIVE): Speculations on the Role of Presence in Virtual Environments. Presence Teleoperators Virtual Environ. 1997, 6, 603–616. [Google Scholar] [CrossRef]
- Riva, G.; Mantovani, F. Being There: Understanding the Feeling of Presence in a Synthetic Environment and its Potential for Clinical Change. In Virtual Reality in Psychological, Medical and Pedagogical Applications; InTech: London, UK, 2012; pp. 3–34. [Google Scholar]
- Huang, M.; Alessi, N. Presence as an Emotional Experience. In Studies in Health Technology and Informatics; IOS Press: Amsterdam, The Netherlands, 1999; Volume 62, pp. 148–153. [Google Scholar]
- Somarathna, R.; Bednarz, T.; Mohammadi, G. Virtual Reality for Emotion Elicitation—A Review. IEEE Trans. Affect. Comput. 2021, 14, 2626–2645. [Google Scholar] [CrossRef]
- Fjærtoft, T.; Karlsen, H.R.; Langvik, E.; Saksvik-lehouillier, I. The effect of immersion on sense of presence and affect when experiencing an educational scenario in virtual reality: A randomized controlled study. Heliyon 2023, 9, e17196. [Google Scholar] [CrossRef]
- Rueda, J.; Lara, F. Virtual Reality and Empathy Enhancement: Ethical Aspects. Front. Robot. AI 2020, 7, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Fox, J.; Christy, K.R.; Vang, M.H. The Experience of Presence in Persuasive Virtual Environments. In Interacting with Presence; De Gruyter Open: Warsaw, Poland, 2014; pp. 164–178. [Google Scholar]
- Andrews, J.; Likis, F.E. Study Design Algorithm. J. Low. Genit. Tract Dis. 2015, 19, 364–368. [Google Scholar] [CrossRef]
- Kalyanaraman, S.; Penn, D.L.; Ivory, J.D.; Judge, A. The virtual doppelganger: Effects of a virtual reality simulator on perceptions of schizophrenia. J. Nerv. Ment. Dis. 2010, 198, 437–443. [Google Scholar] [CrossRef]
- Vasconcelos Raposo, J.; Bessa, M.; Melo, M.; Barbosa, L.; Rodrigues, R.; Teixeira, C.; Cabral, L.; Sousa, A. Adaptation and Validation of the Igroup Presence Questionnaire (IPQ) in a Portuguese Sample. Presence Teleoperators Virtual Environ. 2016, 25, 191–203. [Google Scholar] [CrossRef]
- Veloso Gomes, P.; Marques, A.; Donga, J.; Sá, C.; Correia, A.; Pereira, J. Adaptive model for biofeedback data flows management in the design of interactive immersive environments. Appl. Sci. 2021, 11, 5067. [Google Scholar] [CrossRef]
- Marôco, J. Análise Estatística com o SPSS Statistics, 7th ed.; ReportNumber: Pêro Pinheiro, Portugal, 2018. [Google Scholar]
- Trenerry, M.; Crosson, B.; DeBoe, J.; Leber, W. Stroop Neuropsychological Screening Test; Psychological Assessment Resources: Lutz, FL, USA, 1989. [Google Scholar]
- Schubert, T.; Friedmann, F.; Regenbrecht, H. The Experience of Presence: Factor Analytic Insights. Presence 2001, 10, 266–281. [Google Scholar] [CrossRef]
- Slater, M.; Usoh, M.; Steed, A. Depth of presence in virtual environments. Presence Teleoperators Virtual Environ. 1994, 3, 130–144. [Google Scholar] [CrossRef]
- Witmer, B.; Singer, M. Measuring Presence in Virtual Environments: A Presence Questionnaire. Presence Teleoperators Virtual Environ. 1998, 7, 225–240. [Google Scholar] [CrossRef]
- Andreassi, J.L. Psychophysiology: Human Behavior and Physiological Response, 5th ed.; Psychology Press: New York, NY, USA, 2006. [Google Scholar]
- Braithwaite, J.J.; Watson, D.G.; Jones, R.; Rowe, M. A Guide for Analysing Electrodermal Activity (EDA) & Skin Conductance Responses (SCRs) for Psychological Experiments. Psychophysiology 2013, 49, 1017–1034. [Google Scholar]
- Groth-Marnat, G.; Jordan Wright, A. Handbook of Psychological Assessment, 6th ed.; Wiley: Hoboken, NJ, USA, 2016. [Google Scholar]
| Equipment | Specifications |
|---|---|
| Computer | CPU: Intel® Core™ i7-9700 K (3.60 GHz–4.90 GHz) Graphics Card: NVIDIA® GeForce® RTX 2080 Ti Memory: 64 GB RAM |
| VR Headset HTC Vive Pro™ | High-resolution Dual AMOLED 3.5 diagonal screens 1440 × 1600 pixels per eye (2880 × 1600 pixels combined) Refresh rate: 90 Hz Field of view: 110 degrees Integrated microphones with 3D Spatial Audio Four SteamVR Base Station 2.0: 10 m × 10 m VIVE Wireless Adapter |
| Equipment | Specifications |
|---|---|
| ECG | Number of Channels: 16 Absolute Maximum Input: ±15 V Operational Input Voltage: ±10 V A/D Resolution: 16 Bits Accuracy (% of FSR): ±0.003 Input Impedance: 1.0 MΩ Amplifier Module Isolation: Provided by the MP unit, isolated clean power CE Marking: EC Low Voltage and EMC Directives Leakage Current: <8 µA (Normal), <400 µA (Single Fault) Fuse: 2 A (fast blow). Memory: 64 GB RAM |
| Galvanic skin response | Signal Type: PPG plus EDA Resolution: PPG: FSR/4096, (4.88 mV); EDA: 0.012 μS (min step) Operational Range: 10 m Transmitter: Ultra-low power, 2.4 GHz bi-directional digital RF transmitter; Rate: 2.000 Hz (between transmitter and receiver) |
| Dimension | Items | Cronbach’s Alpha |
|---|---|---|
| Empathic feelings for people suffering from schizophrenia | 12 | 0.735 |
| Social distance | 7 | 0.870 |
| Attitudes toward people with schizophrenia | 7 | 0.718 |
| Simulation evaluation | 5 | 0.534 |
| Dimension | Immersive Environment | Mean Difference M2-M1 | sd | t | p | Cohen’s D |
|---|---|---|---|---|---|---|
| Empathic feelings | Virtual reality | 0.81 | 1.31 | 0.62 | 0.270 | |
| 360° video | 3.15 | 1.36 | 2.31 | 0.013 | 8.73 | |
| Social distance | Virtual reality | 0.02 | 0.27 | 0.08 | 0.469 | |
| 360° video | −0.66 | 0.33 | −1.98 | 0.027 | 2.13 | |
| Attitudes | Virtual reality | 1.38 | 0.76 | 1.81 | 0.038 | 5.23 |
| 360° video | 1.29 | 0.73 | 1.75 | 0.044 | 4.74 |
| Dimension | Immersive Environment | Mean Difference | sd | t | p |
|---|---|---|---|---|---|
| Empathic feelings | Virtual reality | −2.34 | 1.89 | −1.23 | 0.110 |
| 360° video | |||||
| Social distance | Virtual reality | 0.68 | 0.42 | 1.61 | 0.056 |
| 360° video | |||||
| Attitudes | Virtual reality | 0.09 | 1.07 | 0.08 | 0.466 |
| 360° video |
| Dimension | Immersive Environment | Mean | sd | t | p |
|---|---|---|---|---|---|
| Simulation evaluation | Virtual reality | 34.47 | 2.34 | 0.42 | 0.338 |
| 360° video | 33.27 | 2.11 |
| Dimension | Immersive Environment | Mean | sd | t | p | Cohen’s D |
|---|---|---|---|---|---|---|
| Spatial presence | Virtual reality | 3.84 | 0.44 | 0.42 | 0.338 | |
| 360° video | 3.59 | 0.67 | ||||
| Involvement | Virtual reality | 3.67 | 0.71 | 2.01 | 0.024 | 0.56 |
| 360° video | 3.61 | 0.50 | ||||
| Realism | Virtual reality | 2.95 | 0.57 | 0.47 | 0.32 | |
| 360° video | 2.75 | 0.63 | ||||
| Global presence | Virtual reality | 3.48 | 0.44 | 1.56 | 0.061 | |
| 360° video | 3.32 | 0.47 |
| Physiological Data | Immersive Environment | N | Average | sd | Coefficient of Variation | p |
|---|---|---|---|---|---|---|
| HR average | Virtual reality | 47 | 98.18 | 14.84 | 0.15 | 0.024 |
| 360° video | 41 | 89.83 | 19.24 | 0.21 | ||
| HR maximum | Virtual reality | 47 | 123.08 | 17.43 | 0.14 | 0.160 |
| 360° video | 41 | 116.99 | 22.80 | 0.19 | ||
| HR minimum | Virtual reality | 47 | 73.48 | 14.38 | 0.20 | 0.239 |
| 360° video | 41 | 69.53 | 16.86 | 0.24 | ||
| EDA peaks | Virtual reality | 47 | 57.66 | 24.95 | 0.43 | 0.024 |
| 360° video | 41 | 68.49 | 17.98 | 0.26 | ||
| EDA amplitude | Virtual reality | 47 | 0.50 | 0.30 | 0.61 | 0.143 |
| 360° video | 41 | 0.40 | 0.29 | 0.71 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Veloso Gomes, P.; Marques, A.; Pereira, J.; Pimenta, R.; Donga, J.; Simões de Almeida, R. Using Immersive Environments in E-Mental Health Rehabilitation Programs Directed to Future Health Professionals to Promote Empathy and Health Literacy about Schizophrenia. Healthcare 2024, 12, 1550. https://doi.org/10.3390/healthcare12151550
Veloso Gomes P, Marques A, Pereira J, Pimenta R, Donga J, Simões de Almeida R. Using Immersive Environments in E-Mental Health Rehabilitation Programs Directed to Future Health Professionals to Promote Empathy and Health Literacy about Schizophrenia. Healthcare. 2024; 12(15):1550. https://doi.org/10.3390/healthcare12151550
Chicago/Turabian StyleVeloso Gomes, Paulo, António Marques, Javier Pereira, Rui Pimenta, João Donga, and Raquel Simões de Almeida. 2024. "Using Immersive Environments in E-Mental Health Rehabilitation Programs Directed to Future Health Professionals to Promote Empathy and Health Literacy about Schizophrenia" Healthcare 12, no. 15: 1550. https://doi.org/10.3390/healthcare12151550
APA StyleVeloso Gomes, P., Marques, A., Pereira, J., Pimenta, R., Donga, J., & Simões de Almeida, R. (2024). Using Immersive Environments in E-Mental Health Rehabilitation Programs Directed to Future Health Professionals to Promote Empathy and Health Literacy about Schizophrenia. Healthcare, 12(15), 1550. https://doi.org/10.3390/healthcare12151550










