Comparison of Health Parameters in Postpartum Diastasis Recti: A Randomized Control Trial of SEMG Biofeedback-Assisted Core Strengthening Exercises with Kinesiotaping vs. Non-Assisted Exercises
Abstract
:1. Introduction
2. Materials and Methods
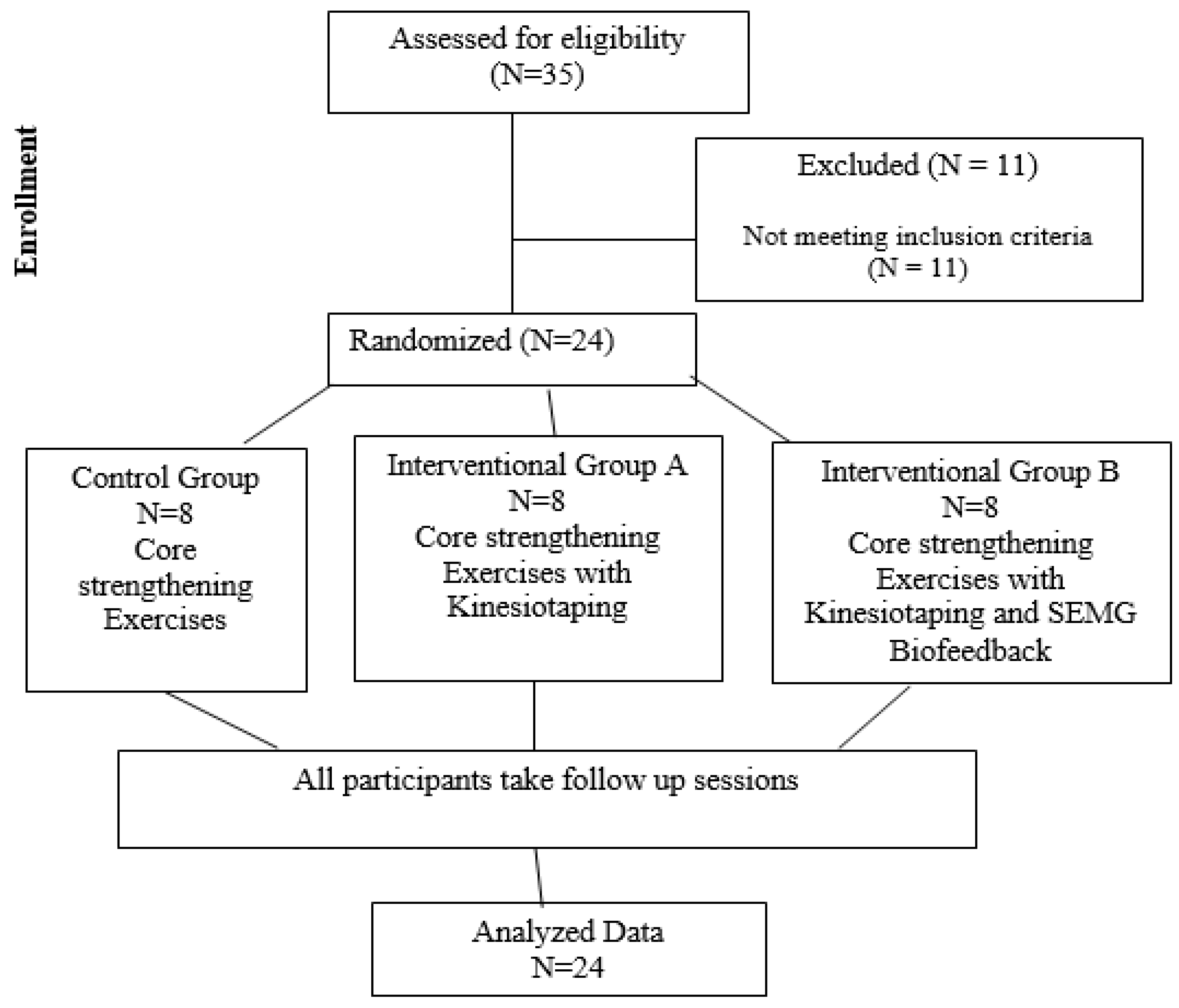
2.1. Study Design
2.2. Ethics
2.3. Sample Size
2.4. Participant Selection and Random Allocation
2.5. Intervention
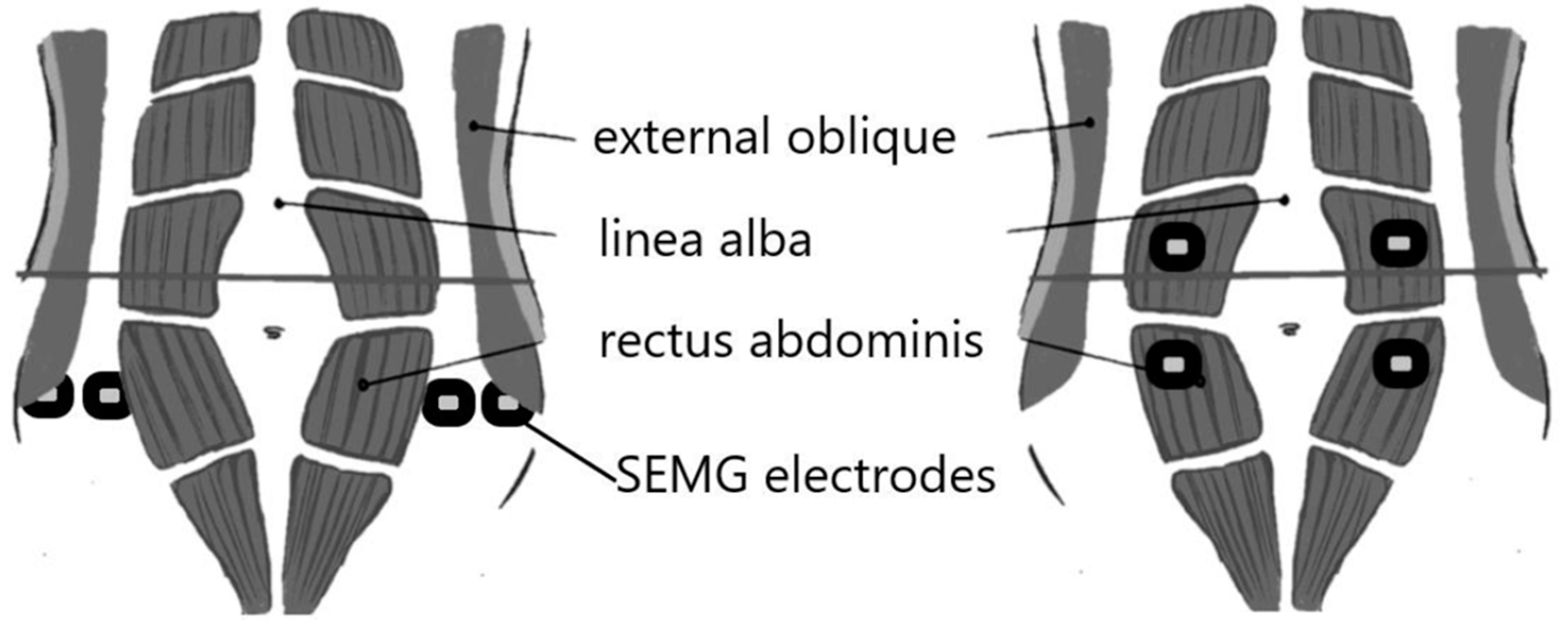
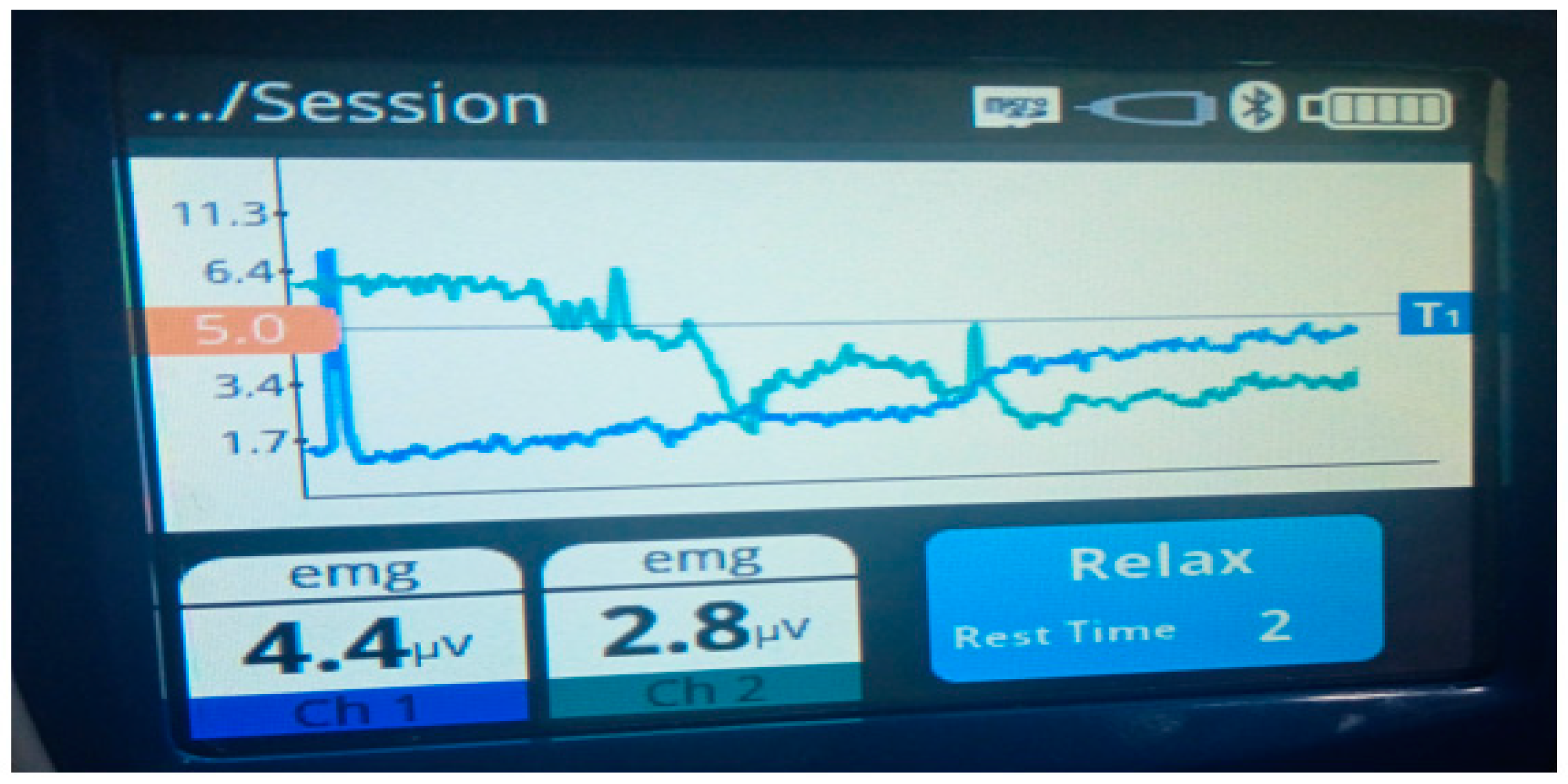
2.6. SEMG Feedback
2.7. Outcome Measures
2.8. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Reinpold, W.; Köckerling, F.; Bittner, R.; Conze, J.; Fortelny, R.; Koch, A.; Kukleta, J.; Kuthe, A.; Lorenz, R.; Stechemesser, B. Classification of rectus diastasis—A proposal by the German Hernia Society (DHG) and the International Endohernia Society (IEHS). Front. Surg. 2019, 6, 1. [Google Scholar] [CrossRef] [PubMed]
- Sperstad, J.B.; Tennfjord, M.K.; Hilde, G.; Ellström-Engh, M.; Bø, K. Diastasis recti abdominis during pregnancy and 12 months after childbirth: Prevalence, risk factors and report of lumbopelvic pain. Br. J. Sports Med. 2016, 50, 1092–1096. [Google Scholar] [CrossRef] [PubMed]
- Da Mota, P.G.F.; Pascoal, A.G.B.A.; Carita AI, A.D.; Bø, K. Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Man. Ther. 2015, 20, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Gluppe, S.B. Diastasis Recti Abdominis: An Issue Postpartum? Ph.D. Thesis, Norwegian School of Sport Sciences, Oslo, Norway, 2023. [Google Scholar]
- Kim, J.H.; Kim, J.Y.; Lee, S.; Lee, S.; Stubbs, B.; Koyanagi, A.; Dragioti, E.; Jacob, L.; Carvalho, A.F.; Radua, J. Environmental risk factors, protective factors, and biomarkers for postpartum depressive symptoms: An umbrella review. Neurosci. Biobehav. Rev. 2022, 140, 104761. [Google Scholar] [CrossRef] [PubMed]
- Sokunbi, G.; Camino-Willhuber, G.; Paschal, P.K.; Olufade, O.; Hussain, F.S.; Shue, J.; Abjornson, C.; Zelenty, W.D.; Lebl, D.R.; Cammisa, F.P. Is diastasis recti abdominis associated with low back pain? A systematic review. World Neurosurg. 2023, 174, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Zhao, X.; Hu, Y. Rehabilitations for maternal diastasis recti abdominis: An update on therapeutic directions. Heliyon 2023, 9, E20956. [Google Scholar] [CrossRef] [PubMed]
- Field, M.; Molesworth, C.; Kaplan, E. Hernia recurrence, chronic pain and infection in patients undergoing open repair of ventral hernia or divarication of rectus abdominus with monofilament poly-4-hydroxybutyrate mesh: A retrospective, patient-report case series. Br. J. Surg. 2024, 111, znae122-298. [Google Scholar] [CrossRef]
- Benjamin, D.R.; Frawley, H.C.; Shields, N.; Peiris, C.L.; van de Water, A.T.; Bruder, A.M.; Taylor, N.F. Conservative interventions may have little effect on reducing diastasis of the rectus abdominis in postnatal women–A systematic review and meta-analysis. Physiotherapy 2023, 119, 54–71. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.; Park, S.; Koyanagi, A.; Yang, J.W.; Jacob, L.; Yon, D.K.; Lee, S.W.; Kim, M.S.; Shin, J.I.; Smith, L. Effects of exogenous melatonin supplementation on health outcomes: An umbrella review of meta-analyses based on randomized controlled trials. Pharmacol. Res. 2022, 176, 106052. [Google Scholar] [CrossRef] [PubMed]
- Mommers, E.H.; Ponten, J.E.; Al Omar, A.K.; de Vries Reilingh, T.S.; Bouvy, N.D.; Nienhuijs, S.W. The general surgeon’s perspective of rectus diastasis. A systematic review of treatment options. Surg. Endosc. 2017, 31, 4934–4949. [Google Scholar] [CrossRef] [PubMed]
- Shohaimi, S.; Husain, N.R.N.; Zaki, F.M.; Atan, I.K. Split tummy exercise program for reducing diastasis recti in postpartum primigravidae: A randomized controlled trial. Korean J. Fam. Med. 2023, 44, 102. [Google Scholar] [CrossRef] [PubMed]
- Yuan, S.; Li, Y.; Li, Q.; Fan, L.; Zhou, J. Surgery versus non-surgery interventions on rectus abdominis diastasis with or without hernias: A systematic review. Indian J. Surg. 2021, 84, 7–20. [Google Scholar] [CrossRef]
- Gluppe, S.L.; Engh, A.M.E.; Bø, K. Curl-up exercises improve abdominal muscle strength without worsening inter-recti distance in women with diastasis recti abdominis postpartum: A randomised controlled trial. J. Physiother. 2023, 69, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Davari, S.; Bagherpour, T.; Nemati, N. Comparison of the Effect of Pilates and Core Stability Exercises on Diastasis Recti and the Structural Component in Abdominis Muscles of Primiparous Mothers. J. Paramed. Sci. Rehabil. 2023, 12, 7–18. [Google Scholar]
- Skoura, A.; Billis, E.; Papanikolaou, D.T.; Xergia, S.; Tsarbou, C.; Tsekoura, M.; Kortianou, E.; Maroulis, I. Diastasis Recti Abdominis Rehabilitation in the Postpartum Period: A Scoping Review of Current Clinical Practice. Int. Urogynecol. J. 2024, 35, 491–520. [Google Scholar] [CrossRef]
- Rahmati, M.; Lee, S.; Yon, D.K.; Lee, S.W.; Udeh, R.; McEvoy, M.; Oh, H.; Butler, L.; Keyes, H.; Barnett, Y. Physical activity and prevention of mental health complications: An umbrella review. Neurosci. Biobehav. Rev. 2024, 160, 105641. [Google Scholar] [CrossRef] [PubMed]
- Kaya, A.K.; Menek, M.Y. Comparison of the efficiency of core stabilization exercises and abdominal corset in the treatment of postpartum diastasis recti abdominis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2023, 285, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Jobanputtra, Y.; Patil, S. Immediate effect of Kinesio Taping on Lumbopelvic stability in postpartum women with Diastasis Recti: A review. Cureus 2023, 15, e33347. [Google Scholar] [CrossRef] [PubMed]
- Kulli, H.D.; Alpay, K. Acute Effects of Kinesio Taping on Women with Diastasis Recti Abdominis. Age (Year) 2023, 32, 4–6. [Google Scholar]
- Pawar, P.A.; Yeole, U.L.; Navale, M.; Patil, K. Effect of kinesiotaping on diastasis recti in post-partum women. Indian J. Public Health Res. Dev. 2020, 11, 692–697. [Google Scholar]
- Oliva-Lozano, J.M.; Muyor, J.M. Core muscle activity during physical fitness exercises: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 4306. [Google Scholar] [CrossRef] [PubMed]
- Voorham, J.C.; De Wachter, S.; Van den Bos, T.W.; Putter, H.; Lycklama à Nijeholt, G.A.; Voorham-van der Zalm, P. The effect of EMG biofeedback assisted pelvic floor muscle therapy on symptoms of the overactive bladder syndrome in women: A randomized controlled trial. J. Neurourol. Urodyn. 2017, 36, 1796–1803. [Google Scholar] [CrossRef] [PubMed]
- Liang, P.; Liang, M.; Shi, S.; Liu, Y.; Xiong, R. Rehabilitation programme including EMG-biofeedback-assisted pelvic floor muscle training for rectus diastasis after childbirth: A randomised controlled trial. Physiotherapy 2022, 117, 16–21. [Google Scholar] [CrossRef]
- Situt, G.; Kanase, S. Effectiveness of NMES and taping on Diastasis Recti in postnatal women. J. Ecophysiol. Occup. Health 2021, 21, 105–111. [Google Scholar] [CrossRef]
- Hicks, G.E.; Fritz, J.M.; Delitto, A.; McGill, S.M. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch. Phys. Med. Rehabil. 2005, 86, 1753–1762. [Google Scholar] [CrossRef] [PubMed]
- Lee, N.; Bae, Y.-H.; Fong, S.S.; Lee, W.-H. Effects of Pilates on inter-recti distance, thickness of rectus abdominis, waist circumference and abdominal muscle endurance in primiparous women. BMC Women’s Health 2023, 23, 626. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, D.R.; Frawley, H.C.; Shields, N.; Georgiou, C.; Taylor, N.F. Establishing measurement properties in the assessment of inter-recti distance of the abdominal muscles in a postnatal women. Musculoskelet. Sci. Pract. 2020, 49, 102202. [Google Scholar] [CrossRef] [PubMed]
- Zamani, Y.S.; Moradian, M.; Eftekharsadat, B.; Safiri, S.; Mirghafourvand, M.; Hasanpour, S.; Bani, S. The Effect of Kinesio Taping on Abdominal Muscles Disorders in Postpartum: A Systematic Review and Meta-Analysis. 2023. Available online: https://www.researchsquare.com/article/rs-2965014/v1 (accessed on 29 July 2024).
- Khobragade, S.; Naqvi, W.; Dhankar, S.; Jungade, S. Impact of K-Taping on sacroiliac joint pain in women after full-term normal delivery. J. Datta Meghe Inst. Med. Sci. Univ. 2019, 14, 352–355. [Google Scholar]
- Criswell, E. Cram’s Introduction to Surface Electromyography; Jones & Bartlett Publishers: Burlington, MA, USA, 2010. [Google Scholar]
- Frizziero, A.; Pellizzon, G.; Vittadini, F.; Bigliardi, D.; Costantino, C. Efficacy of core stability in non-specific chronic low back pain. J. Funct. Morphol. Kinesiol. 2021, 6, 37. [Google Scholar] [CrossRef] [PubMed]
- Thabet, A.A.; Alshehri, M.A. Efficacy of deep core stability exercise program in postpartum women with diastasis recti abdominis: A randomised controlled trial. J. Musculoskelet. Neuronal Interact. 2019, 19, 62. [Google Scholar] [PubMed]
- Izydorczyk, B.; Walenista, W.; Kamionka, A.; Lizińczyk, S.; Ptak, M. Connections Between Perceived Social Support and the Body Image in the Group of Women With Diastasis Recti Abdominis. Front. Psychol. 2021, 12, 707775. [Google Scholar] [CrossRef]
| Variable | Control Group (Mean ± SD) | C.I 95% | Interventional A (Mean ± SD) | C.I 95% | Interventional B (Mean ± SD) | C.I 95% | F Value | p-Value |
|---|---|---|---|---|---|---|---|---|
| Age (years) | 26.7 ± 5.23 | 22.37 to 31.12 | 26.7 ± 4.43 | 23.04 to 30.45 | 28.7 ± 5.47 | 24.18 to 33.32 | 0.416 | 0.597 |
| Height (cm) | 151.7 ± 3.64 | 148.67 to 154.77 | 162.8 ± 5.04 | 158.65 to 167.08 | 159.1 ± 8.52 | 152.04 to 166.31 | 6.94 | 0.007 * |
| Weight (kg) | 53.3 ± 11.0 | 44.14 to 62.61 | 63.5 ± 8.89 | 56.06 to 70.94 | 60.3 ± 12.5 | 49.87 to 70.88 | 1.79 | 0.137 |
| BMI (kg/m2) | 22.4 ± 2.81 | 20.07 to 24.78 | 23.8 ± 2.76 | 21.49 to 26.11 | 25.4 ± 4.82 | 21.42 to 29.48 | 1.41 | 0.437 |
| Inter-rectus distance | ||||||||
| At umbilicus level (cm) | 2.65 ± 0.28 | 2.42 to 2.89 | 2.50 ± 0.29 | 2.26 to 2.74 | 2.22 ± 0.37 | 1.91 to 2.54 | 3.82 | 0.038 * |
| Above umbilicus level (cm) | 2.74 ± 0.25 | 2.52 to 2.96 | 2.56 ± 0.327 | 2.29 to 2.84 | 2.28 ± 0.37 | 1.97 to 2.60 | 3.96 | 0.035 * |
| Below umbilicus level (cm) | 2.37 ± 0.19 | 2.21 to 2.54 | 2.28 ± 0.29 | 2.03 to 2.53 | 2.11 ± 0.39 | 1.78 to 2.45 | 1.42 | 0.262 |
| Quality of life | ||||||||
| Role limitation due to physical problems | 44.37 ± 25.41 | 23.13 to 65.62 | 92.50 ± 11.34 | 83.02 to 101.97 | 91.87 ± 15.56 | 78.86 to 104.89 | 9.313 | 0.001 * |
| Role limitation due to emotional problems | 82.27 ± 27.62 | 59.18 to 105.37 | 88.75 ± 31.81 | 62.15 to 115.35 | 85.83 ± 29.04 | 61.56 to 110.12 | 0.096 | 0.909 |
| Energy | 46.25 ± 10.93 | 37.11 to 55.39 | 70.62 ± 19.16 | 54.60 to 86.65 | 66.25 ± 14.58 | 54.06 to 78.44 | 5.79 | 0.010 * |
| Physical functioning | 65.62 ± 15.45 | 52.70 to 78.54 | 91.87 ± 10.99 | 82.68 to 101.07 | 90.00 ± 13.88 | 78.39 to 101.61 | 9.313 | 0.001 * |
| Social functioning | 56.12 ± 14.88 | 44.68 to 69.57 | 66.81 ± 27.35 | 44.99 to 90.64 | 68.12 ± 22.22 | 56.85 to 92.28 | 0.710 | 0.503 |
| Body pain | 60.00 ± 20.08 | 43.21 to 76.79 | 83.75 ± 12.67 | 73.15 to 94.35 | 88.12 ± 13.00 | 77.25 to 98.99 | 7.494 | 0.003 * |
| General health | 57.50 ± 11.95 | 47.51 to 67.49 | 81.25 ± 12.74 | 70.59 to 91.91 | 80.12 ± 14.74 | 67.80 to 92.45 | 8.245 | 0.002 * |
| Core strength | ||||||||
| Trunk flexion (s) | 10.00 ± 2.01 | 8.31 to 11.68 | 16.06 ± 7.48 | 9.86 to 22.26 | 16.1 ± 6.99 | 10.25 to 21.95 | 2.739 | 0.088 |
| Trunk extension (s) | 8.81 ± 2.64 | 6.60 to 11.02 | 12.87 ± 4.96 | 8.73 to 17.02 | 13.50 ± 6.60 | 7.98 to 19.02 | 2.066 | 0.152 |
| Right side plank (s) | 8.37 ± 2.91 | 5.95 to 10.81 | 12.10 ± 6.16 | 6.95 to 17.25 | 10.18 ± 4.78 | 6.19 to 14.18 | 1.201 | 0.321 |
| Left side plank (s) | 8.46 ± 2.7 | 6.18 to 10.74 | 11.81 ± 5.7 | 6.99 to 16.62 | 10.06 ± 4.78 | 6.06 to 14.06 | 1.061 | 0.364 |
| Variable | Groups | Mean ± SD | Mean Δ | C.I 95% | p-Value |
|---|---|---|---|---|---|
| At umbilicus level | Control | 2.65 ± 0.28 | 0.154 | −2.472 to 0.555 | 0.605 |
| Intervention A | 2.50 ± 0.29 | ||||
| Control | 2.65 ± 0.28 | 0.433 | 0.032 to 0.835 | 0.032 * | |
| Intervention B | 2.22 ± 0.37 | ||||
| Intervention A | 2.50 ± 0.29 | 0.280 | −1.209 to 0.680 | 0.207 | |
| Intervention B | 2.22 ± 0.37 | ||||
| Above umbilicus level | Control | 2.74 ± 0.25 | 0.175 | −2.335 to 0.583 | 0.537 |
| Intervention A | 2.56 ± 0.327 | ||||
| Control | 2.74 ± 0.25 | 0.452 | 0.044 to 0.861 | 0.028 * | |
| Intervention B | 2.28 ± 0.37 | ||||
| Intervention A | 2.56 ± 0.327 | 0.277 | −0.131 to 0.686 | 0.224 | |
| Intervention B | 2.28 ± 0.37 | ||||
| Physical functioning | Control | 65.62 ± 15.45 | −26.250 | −43.356 to −9.144 | 0.002 * |
| Intervention A | 91.87 ± 10.99 | ||||
| Control | 65.62 ± 15.45 | −24.375 | −41.480 to −7.269 | 0.005 * | |
| Intervention B | 90.00 ± 13.88 | ||||
| Intervention A | 91.87 ± 10.99 | 1.87 | −15.230 to 18.980 | 0.959 | |
| Intervention B | 90.00 ± 13.88 | ||||
| Role limitations due to physical problems | Control | 44.37 ± 25.41 | −48.125 | −71.329 to −22.921 | 0.012 * |
| Intervention A | 92.50 ± 11.34 | ||||
| Control | 44.37 ± 25.41 | −47.500 | −70.703 to −24.296 | 0.006 * | |
| Intervention B | 91.87 ± 15.56 | ||||
| Intervention A | 92.50 ± 11.34 | 0.625 | −22.57 to 23.829 | 0.952 | |
| Intervention B | 91.87 ± 15.56 | ||||
| Energy | Control | 46.25 ± 10.93 | −24.375 | −43.620 to −5.131 | 0.012 * |
| Intervention A | 70.62 ± 19.16 | ||||
| Control | 46.25 ± 10.93 | −20.000 | −39.245 to −0.755 | 0.041 * | |
| Intervention B | 66.25 ± 14.58 | ||||
| Intervention A | 70.62 ± 19.16 | 4.375 | −14.870 to 23.620 | 0.836 | |
| Intervention B | 66.25 ± 14.58 | ||||
| Body pain | Control | 60.00 ± 20.08 | −23.750 | −43.456 to −4.044 | 0.017 * |
| Intervention A | 83.75 ± 12.67 | ||||
| Control | 60.00 ± 20.08 | −28.125 | −47.831 to −8.419 | 0.005 * | |
| Intervention B | 88.12 ± 13.00 | ||||
| Intervention A | 83.75 ± 12.67 | −4.375 | −24.081 to 15.331 | 0.843 | |
| Intervention B | 88.12 ± 13.00 | ||||
| General health | Control | 57.50 ± 11.95 | −23.750 | −40.384 to −7.116 | 0.005 * |
| Intervention A | 81.25 ± 12.74 | ||||
| Control | 57.50 ± 11.95 | −22.625 | −39.259 to −5.990 | 0.007 * | |
| Intervention B | 80.12 ± 14.74 | ||||
| Intervention A | 81.25 ± 12.74 | 1.125 | −15.509 to 17.759 | 0.984 | |
| Intervention B | 80.12 ± 14.74 |
| Variables | Time | Control Group | Interventional Group A | Interventional Group B | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean Δ | C.I 95% | p-Value | Mean ± SD | Mean Δ | C.I 95% | p-Value | Mean ± SD | Mean Δ | C.I 95% | p-Value | |||
| Inter-rectus distance | At umbilicus level | Pre Rx | 2.74 ± 0.31 | 0.086 | 0.027 to 0.144 | 0.010 | 2.99 ± 0.300 | 0.491 | 0.370 to 0.611 | 0.000 | 2.85 ± 0.40 | 0.633 | 0.365 to 0.902 | 0.001 * |
| Post Rx | 2.6 ± 0.28 | 2.50 ± 0.29 | 2.22 ± 0.37 | |||||||||||
| Above umbilicus level | Pre Rx | 2.95 ± 0.28 | 0.215 | 0.131 to 0.298 | 0.001 | 3.20 ± 0.28 | 0.642 | 0.246 to 0.533 | 0.000 | 3.07 ± 0.34 | 0.781 | 0.546 to 1.015 | 0.000 * | |
| Post Rx | 2.74 ± 0.25 | 2.56 ± 0.33 | 2.28 ± 0.37 | |||||||||||
| Below umbilicus level | Pre Rx | 2.45 ± 0.25 | 0.0762 | 0.024 to 0.127 | 0.010 | 2.67 ± 0.38 | 0.390 | 0.246 to 9.533 | 0.000 | 2.59 ± 0.40 | 0.477 | 0.199 to 0.755 | 0.005 * | |
| Post Rx | 2.37 ± 1.98 | 2.28 ± 0.29 | 2.11 ± 0.39 | |||||||||||
| Core Strength | Trunk Flexion | Pre Rx | 7.47 ± 2.27 | −2.52 | −3.325 to −1.172 | 0.000 | 11.61 ± 7.39 | −4.450 | −5.592 to −3.307 | 0.000 | 10.04 ± 6.35 | −6.062 | −7.429 to −4.696 | 0.000 * |
| Post Rx | 10.0 ± 2.01 | 16.06 ± 7.41 | 16.10 ± 6.99 | |||||||||||
| Trunk Extension | Pre Rx | 5.97 ± 2.52 | −2.83 | −3.842 to −1.832 | 0.000 | 7.65 ± 4.57 | −5.225 | −5.793 to −4.656 | 0.000 | 6.79 ± 5.93 | −6.71 | −9.109 to −4.315 | 0.000 * | |
| Post Rx | 8.81 ± 2.64 | 12.87 ± 4.96 | 13.50 ± 6.60 | |||||||||||
| Right side planks | Pre Rx | 6.18 ± 2.86 | −2.18 | −3.002 to −1.372 | 0.000 | 7.56 ± 5.45 | −4.537 | −5.755 to −3.319 | 0.000 | 4.04 ± 3.74 | −6.150 | −7.443 to −4.855 | 0.000 * | |
| Post Rx | 8.37 ± 2.91 | 12.1 ± 6.16 | 10.19 ± 4.78 | |||||||||||
| Left side planks | Pre Rx | 6.31 ± 2.69 | −2.15 | −2.635 to −1.664 | 0.000 | 7.85 ± 5.64 | −3.96 | −4.968 to −2.956 | 0.000 | 3.37 ± 3.25 | −6.687 | −8.864 to −4.510 | 0.000 * | |
| Post Rx | 8.46 ± 2.73 | 11.81 ± 5.76 | 10.06 ± 4.78 | |||||||||||
| Quality of life | Physical functioning | Pre Rx | 59.37 ± 18.01 | −6.250 | −9.955 to −2.544 | 0.005 | 82.50 ± 16.69 | −9.375 | −14.585 to −4.164 | 0.004 | 77.0 ± 23.71 | −13.000 | −22.288 to −3.711 | 0.013 * |
| Post Rx | 69.62 ± 15.45 | 91.87 ± 10.99 | 18.0 ± 13.89 | |||||||||||
| Social functioning | Pre Rx | 56.12 ± 14.88 | −1.000 | −2.611 to 0.611 | 0.186 | 66.81 ± 27.35 | −1.000 | −2.611 to 0.6112 | 0.186 | 68.12 ± 22.22 | −6.437 | −17.184 to 4.309 | 0.200 | |
| Post Rx | 57.12 ± 14.88 | 67.81 ± 27.30 | 74.56 ± 21.18 | |||||||||||
| Role limitations due to emotional problems | Pre Rx | 75.0 ± 38.83 | −7.275 | −18.684 to 4.13 | 0.175 | 83.34 ± 35.63 | −5.412 | −15.276 to 4.451 | 0.236 | 79.16 ± 36.20 | −6.675 | −16.460 to 3.11 | 0.151 | |
| Post Rx | 82.27 ± 27.63 | 88.75 ± 31.81 | 85.83 ± 29.04 | |||||||||||
| Role limitations due to physical problems | Pre Rx | 15.65 ± 35.18 | −28.718 | −42.038 to −15.398 | 0.001 | 75.62 ± 40.12 | −16.875 | −41.242 to 7.492 | 0.146 | 81.25 ± 37.20 | −10.000 | −32.56 to 11.316 | 0.290 | |
| Post Rx | 44.37 ± 25.41 | 92.50 ± 11.34 | 91.87 ± 15.57 | |||||||||||
| Energy | Pre Rx | 43.12 ± 9.23 | −9.312 | −24.71 to 6.091 | 0.011 | 60.62 ± 24.70 | −10.000 | −16.31 to −3.68 | 0.007 | 47.50 ± 15.58 | −18.750 | −22.455 to −15.044 | 0.000 * | |
| Post Rx | 46.25 ± 10.94 | 70.62 ± 19.17 | 66.25 ± 14.57 | |||||||||||
| Body pain | Pre Rx | 53.06 ± 20.03 | −6.937 | −10.543 to −3.331 | 0.003 | 72.94 ± 16.98 | −10.81 | −16.221 to −5.403 | 0.002 | 77.37 ± 22.67 | −10.750 | −20.391 to −1.108 | 0.034 * | |
| Post Rx | 60.0 ± 20.09 | 83.73 ± 12.67 | 88.12 ± 13.0 | |||||||||||
| General health | Pre Rx | 50.0 ± 15.12 | −7.500 | −10.659 to −4.340 | 0.001 | 71.25 ± 14.07 | −10.000 | −13.870 to −6.129 | 0.000 | 64.12 ± 16.61 | −16.000 | −21.399 to −10.600 | 0.000 * | |
| Post Rx | 57.5 ± 11.95 | 61.25 ± 12.75 | 80.12 ± 14.74 | |||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Afzal, U.; Saeed, Q.; Anwar, M.N.; Pervaiz, S.; Shahid, M.; Javed, R.; Ali, M.U.; Lee, S.W. Comparison of Health Parameters in Postpartum Diastasis Recti: A Randomized Control Trial of SEMG Biofeedback-Assisted Core Strengthening Exercises with Kinesiotaping vs. Non-Assisted Exercises. Healthcare 2024, 12, 1567. https://doi.org/10.3390/healthcare12161567
Afzal U, Saeed Q, Anwar MN, Pervaiz S, Shahid M, Javed R, Ali MU, Lee SW. Comparison of Health Parameters in Postpartum Diastasis Recti: A Randomized Control Trial of SEMG Biofeedback-Assisted Core Strengthening Exercises with Kinesiotaping vs. Non-Assisted Exercises. Healthcare. 2024; 12(16):1567. https://doi.org/10.3390/healthcare12161567
Chicago/Turabian StyleAfzal, Ujala, Quratulain Saeed, Muhammad Nabeel Anwar, Sanna Pervaiz, Manahil Shahid, Rimsha Javed, Muhammad Umair Ali, and Seung Won Lee. 2024. "Comparison of Health Parameters in Postpartum Diastasis Recti: A Randomized Control Trial of SEMG Biofeedback-Assisted Core Strengthening Exercises with Kinesiotaping vs. Non-Assisted Exercises" Healthcare 12, no. 16: 1567. https://doi.org/10.3390/healthcare12161567






