Effects of Virtual Reality (VR)-Based Meditation on Sleep Quality, Stress, and Autonomic Nervous System Balance in Nursing Students
Abstract
1. Introduction
2. Materials and Methods
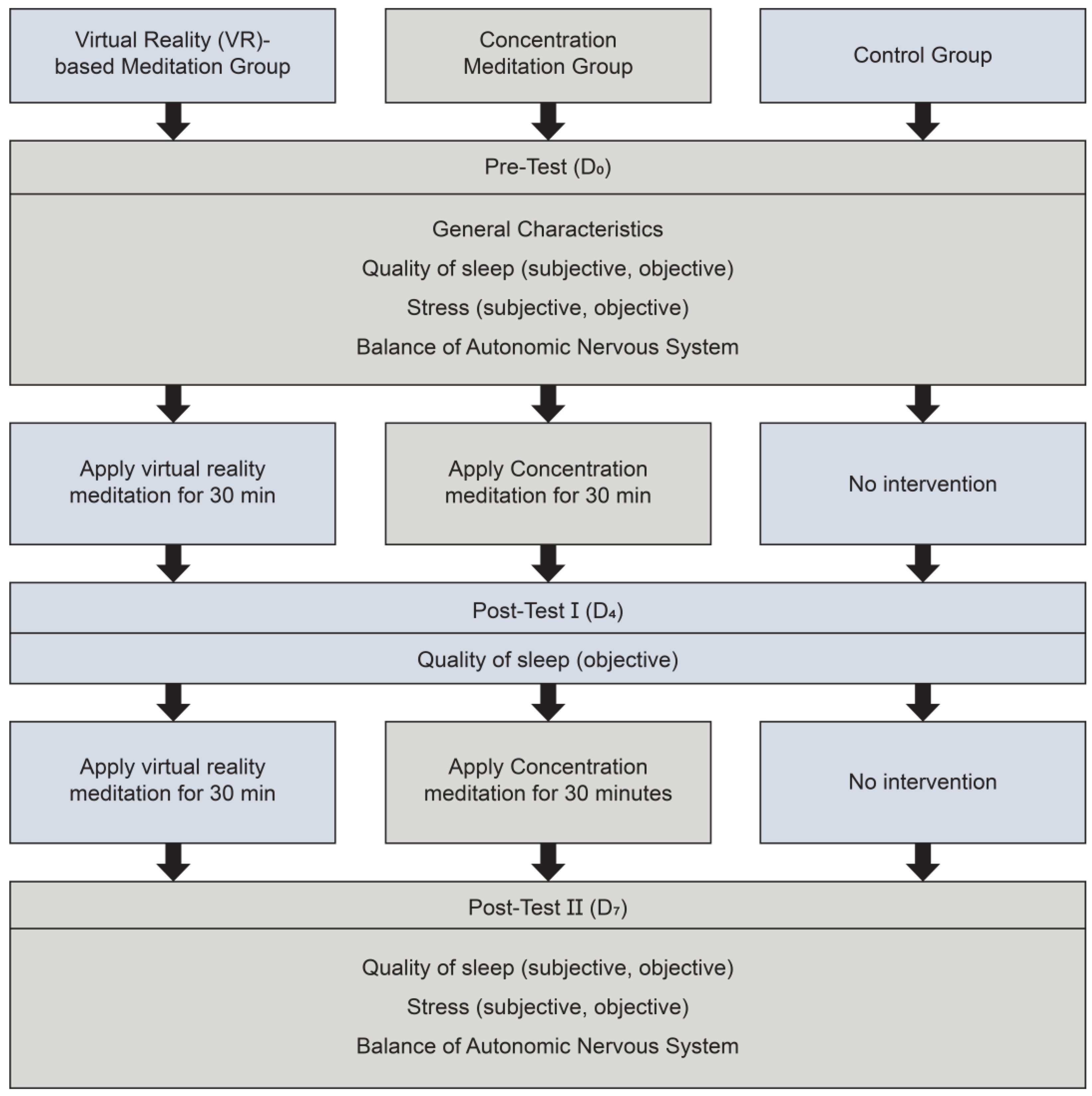
2.1. Research Design
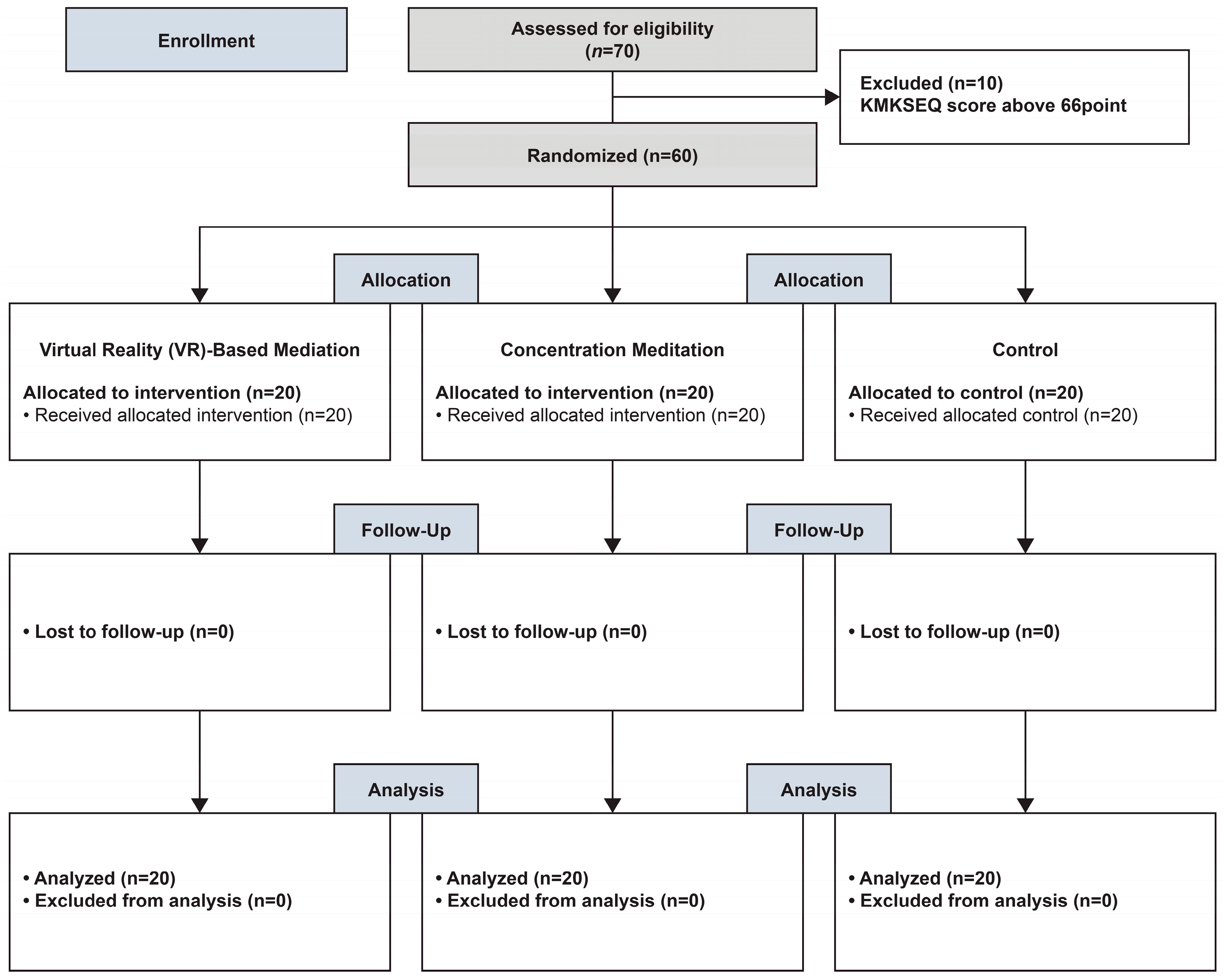
2.2. Participant Selection and Sample Size
2.2.1. Participant Selection
2.2.2. Sample Size
2.3. Randomization and Blinding
2.4. Data Collection
2.5. Experimental Treatment and Procedure
2.5.1. Experimental Treatment
2.5.2. Experimental Procedure
- Experimental Group I.
- Experimental Group II.
- Control Group.
2.6. Research Tools
2.6.1. Sleep Quality
2.6.2. Stress
2.6.3. Autonomic Nervous System Balance
2.7. Data Analysis
- Participants’ general characteristics were analyzed by frequency, error, percentage, mean, and standard deviation; homogeneity was analyzed using a χ2-test and a one-way ANOVA.
- The homogeneity of the pre-intervention dependent variables of experimental group I, experimental group II, and the control group was analyzed using one-way ANOVA.
- A one-way ANOVA was used to test differences in sleep quality, stress, and ANS balance between the VR-based meditation, concentration meditation, and control groups. Further, Duncan’s test was used post hoc to test significant results. We used a repeated-measures ANOVA to verify the difference in effects caused by the change from pre- to post-intervention.
2.8. Ethical Considerations
3. Results
3.1. Homogeneity Testing of Participants’ Pre-Intervention Characteristics and Dependent Variables
3.2. Effects of Virtual Reality-Based Meditation on Sleep Quality
3.3. Effects of Virtual Reality-Based Meditation on Stress
3.4. Effects of Virtual Reality-Based Meditation on Autonomic Nervous System Balance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chang, E.B. The Mediating Effect of Interpersonal Problems in the Relationship between Maladaptive Perfectionism and Academic Burnout among College students. Korean J. Youth Stud. 2019, 26, 29–56. [Google Scholar] [CrossRef]
- Hwang, S.Y. Exploring the Decision-Making Process of Academic Persistence in University Students Who suffered a Dropping-out Crisis. Educ. Cult. 2020, 26, 327–352. [Google Scholar] [CrossRef]
- Lee, E.H. Effect of resilience on academic burnout of nursing students. J. Korea Acad.-Ind. Coop. Soc. 2019, 20, 178–187. [Google Scholar] [CrossRef]
- Yang, S.K.; Jung, M.R. The influences of academic-burnout, self-efficacy, major satisfaction on nursing professionalism in nursing students. Korean Assoc. Learn.-Centered Curric. Instr. 2016, 16, 613–629. [Google Scholar] [CrossRef]
- Ha, Y.J.; Park, S.Y.; Cho, H.J.; Yang, B.R.; Cha, Y.J.; Nam, S.A.; Hwang, J.; Kim, I.; Kim, I. Effects of white noise on nursing students’ stress and sleep quality during clinical practice. Nurs. Healthc. Sci. 2023, 22, 31–37. [Google Scholar] [CrossRef]
- Okano, K.; Kaczmarzyk, J.R.; Dave, N.; Gabrieli, J.D.E.; Grossman, J.C. Sleep quality, duration, and consistency are associated with better academic performance in college students. npj Sci. Learn. 2019, 4, 16. [Google Scholar] [CrossRef]
- Suh, M.H. Differences in heart rate variability depending on sex, level of stress, anxiety, and depression among college students: On the basis of neurovisceral integration model. J. Korean Biol. Nurs. Sci. 2021, 23, 22–30. [Google Scholar] [CrossRef]
- Coren, S. Sleep health and its assessment and management in physical therapy practice: The evidence. Physiother. Theory Pract. 2009, 25, 442–452. [Google Scholar] [CrossRef]
- Kim, L. Stress, Sleep physiology, and related insomnia disorders. J. Korean Med. Assoc. 2010, 53, 707–716. [Google Scholar] [CrossRef][Green Version]
- Koo, D.L.; Kim, J.H. The Physiology of normal sleep. Hanyang Med. Rev. 2013, 33, 190–196. [Google Scholar] [CrossRef]
- Kreitzer, M.J.; Koithan, M. Integrative Nursing; Oxford University Press: Oxford, UK, 2014. [Google Scholar]
- Lee, S.J.; Kim, J.K. Inflammation and insufficient or disordered sleep. Korean J. Clin. Lab. Sci. 2015, 47, 97–104. [Google Scholar] [CrossRef]
- Luyster, F.S.; Strollo, P.J.; Zee, P.C.; Walsh, J.K. Boards of Directors of the American Academy of Sleep Medicine and the Sleep Research Society. Sleep: A health imperative. Sleep 2012, 35, 727–734. [Google Scholar] [CrossRef]
- Lim, J.H.; Nam, J.J.; Kim, M.J.; Lee, O.S.; Sim, B.H.; Lee, S.M. Factors influencing Academic Stress among Nursing Students who experienced COVID-19. J. Converg. Cult. Technol. 2023, 9, 445–455. [Google Scholar] [CrossRef]
- Kim, I.; Choi, H.J.; Kim, B.J. Psychometric properties of Korean version of modified Leeds Sleep evaluation questionnaire (KMLSEQ). Korean J. Rehabil. Nurs. 2014, 17, 10–17. [Google Scholar] [CrossRef][Green Version]
- Lee, J.K.; Jang, K.D.; Kim, J.K. The effects of college life stress and academic self-efficacy on major satisfaction in nursing students. J. Edutainment 2023, 5, 151–161. [Google Scholar] [CrossRef]
- Park, B.R. Anatomy and physiology of the autonomic nervous system. Res. Vestib. Sci. 2017, 16, 101–107. [Google Scholar] [CrossRef][Green Version]
- Lee, H.Y.; Kwak, Y.S.; Koo, B.H.; Kim, K.S.; Kim, S.J. Meditation and Medicine; Hakjisa: Seoul, Republic of Korea, 2022. [Google Scholar]
- Huh, H.J.; Han, S.B.; Park, Y.N.; Chae, J.H. Clinical implication of meditation in psychiatry: Focused on mindfulness meditation. J. Korean Neuropsychiatr. Assoc. 2015, 54, 406–417. [Google Scholar] [CrossRef]
- Kwack, Y.S.; Moon, D.S. Clinical application of meditation in children and adolescents. J. Korean Neuropsychiatr. Assoc. 2020, 59, 36–43. [Google Scholar] [CrossRef]
- Lee, S.H. Professional report Meditation and brain waves. Brain 2015, 50, 32–39. [Google Scholar]
- Lee, S.H. Professional report Meditation, changes in brain function and structure. Brain 2015, 52, 42–51. [Google Scholar]
- Han, Y.J.; Kim, K.S.; Moon, S.J.; Joo, H.S.; Choi, Y.J. The effect of video content on individual emotional improvement. Acad. J. Vis. Cult. Contents Res. 2021, 24, 407–449. [Google Scholar] [CrossRef]
- Kim, M.G.; Han, G.G. Effectiveness of 360-degree Virtual Reality Video as Community Simulation Learning for Students with Severe and Multiple Disabilities. Korean J. Phy Mult. Health Disabil. 2019, 62, 231–256. [Google Scholar] [CrossRef]
- Yoo, B.J. Overview of virtual reality, augmented reality and mixed reality. J. Korea Robot. Soc. 2018, 15, 3–7. [Google Scholar]
- Zambotti, M.D.; Yuksel, D.; Kiss, O.; Barresi, G.; Arra, N.; Volpe, L.; King, C.; Baker, F.C. A virtual reality-based mind–body approach to downregulate psychophysiological arousal in adolescent insomnia. Digit. Health 2022, 8, 20552076221107887. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.M.; Wu Chueh, M.T.; Lai, Y.J. Meditation practice improves short-term changes in heart rate variability. Int. J. Environ. Res. Public Health 2020, 17, 2128. [Google Scholar] [CrossRef] [PubMed]
- Bamber, M.D.; Kraenzle Schneider, J.K. Mindfulness-based meditation to decrease stress and anxiety in college students: A narrative synthesis of the research. Educ. Res. Rev. 2016, 18, 1–32. [Google Scholar] [CrossRef]
- Kim, K.N.; Son, H.G.; Park, H.J. Effects of mindfulness meditation program on sleep, depression and quality of life in the institutionalized elderly women. Korean J. Health Serv. Manag. 2014, 8, 157–168. [Google Scholar] [CrossRef]
- Chavez, L.J.; Kelleher, K.; Slesnick, N.; Holowacz, E.; Luthy, E.; Moore, L.; Ford, J. Virtual reality meditation among youth experiencing homelessness: Pilot randomized controlled trial of feasibility. JMIR Ment. Health 2020, 7, e18244. [Google Scholar] [CrossRef] [PubMed]
- Han, H.Y.; Jo, H.I. SEONMEDI VR Natural Meditation Program for University Students Experiencing Psychological Difficulties During the Pandemic: Effects on Heart Rate Variability, Perceived Stress, and Self-Compassion. Korean Assoc. Learn.-Centered Curric. Instr. 2023, 23, 363–381. [Google Scholar] [CrossRef]
- Lee, S.Y.; Kang, J. Effect of virtual reality meditation on sleep quality of intensive care unit patients: A randomised controlled trial. Intensive Crit. Care Nurs. 2020, 59, 102849. [Google Scholar] [CrossRef]
- Arsad, F.S.; Hod, R.; Ahmad, N.; Baharom, M.; Ja’afar, M.H. Assessment of indoor thermal comfort temperature and related behavioural adaptations: A systematic review. Environ. Sci. Pollut. Res. 2023, 30, 73137–73149. [Google Scholar] [CrossRef] [PubMed]
- Korean Statistical Information Service. Actor and action rates by time zone. In Life Time Survey; Korean Statistical Information Service: Gwangju, Republic of Korea, 2019. [Google Scholar]
- Kim, Y.S.; Chung, E.Y.; Kim, J.N.; Seo, Y.J. The effect of emotional labor on job stress, burnout and job satisfaction of hospital nurses. J. Korean Public. Health Res. 2014, 40, 75–88. [Google Scholar]
- Parrott, A.C.; Hindmarch, I. Factor analysis of a sleep evaluation questionnaire. Psychol. Med. 1978, 8, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Shin, C.M.; Ko, Y.H.; Im, J.H. The reliability and validity studies of the Korean version of the perceived stress scale. Psychosom. Med. 2012, 20, 127–134. [Google Scholar]
- Kim, B.S.; Min, J.A. Utilization and Interpretation of HRV (Heart Rate Variability) in Stress Clinics, 3–11; Panmun Education: Seoul, Republic of Korea, 2015. [Google Scholar]
- Kanchibhotla, D.; Parekh, S.G.; Harsora, P.; Kulkarni, S. Improvements in sleep quality and duration following a meditation retreat: An open-trial pilot study. Sleep. Vigil. 2021, 5, 275–280. [Google Scholar] [CrossRef]
- Rusch, H.L.; Rosario, M.; Levison, L.M.; Olivera, A.; Livingston, W.S.; Wu, T.; Gill, J.M. The effect of mindfulness meditation on sleep quality: A systematic review and meta-analysis of randomized controlled trials. Ann. N. Y. Acad. Sci. 2019, 1445, 5–16. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Lee, O.E.K.; Feng, F.; Vitiello, M.V.; Wang, W.; Benson, H.; Fricchione, G.L.; Denninger, J.W. The effect of meditative movement on sleep quality: A systematic review. Sleep. Med. Rev. 2016, 30, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.W.; Kwong, E.; Lan, X.Y.; Jiang, X.Y. The effect of a meditative movement intervention on quality of sleep in the elderly: A systematic review and meta-analysis. J. Altern. Complement. Med. 2015, 21, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Patrick, H.; Williams, G.C. Self-determination theory: Its application to health behavior and complementarity with motivational interviewing. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 18. [Google Scholar] [CrossRef] [PubMed]
- Carskadon, M.A.; Dement, W.C. Normal human sleep: An overview. Princ. Pract. Sleep. Med. 2005, 4, 13–23. [Google Scholar]
- Roomkham, S.; Lovell, D.; Cheung, J.; Perrin, D. Promises and challenges in the use of consumer-grade devices for sleep monitoring. IEEE Rev. Biomed. Eng. 2018, 11, 53–67. [Google Scholar] [CrossRef] [PubMed]
- Jarvelin-pasanen, S.; Sinikallio, S.; Tarvaine, T.P. Heart rate variability and occupational stress-systematic review. Ind. Health 2018, 56, 500–511. [Google Scholar] [CrossRef] [PubMed]
- Selye, H. The Stress of Life, Rev; McGraw-Hill: New York, NY, USA, 1978. [Google Scholar]
- Maples-Keller, J.L.; Yasinski, C.; Manjin, N.; Rothbaum, B.O. Virtual reality-enhanced extinction of phobias and post-traumatic stress. Neurotherapeutics 2017, 14, 554–563. [Google Scholar] [CrossRef] [PubMed]
- Villani, D.; Riva, F.; Riva, G. New technologies for relaxation: The role of presence. Int. J. Stress. Manag. 2007, 14, 260–274. [Google Scholar] [CrossRef]
- Shearer, A.; Hunt, M.; Chowdhury, M.; Nicol, L. Effects of a brief mindfulness meditation intervention on student stress and heart rate variability. Int. J. Stress. Manag. 2016, 23, 232–254. [Google Scholar] [CrossRef]
- Nesvold, A.; Fagerland, M.W.; Davanger, S.; Ellingsen, Ø.; Solberg, E.E.; Holen, A.; Sevre, K.; Atar, D. Increased heart rate variability during nondirective meditation. Eur. J. Prev. Cardiol. 2012, 19, 773–780. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.J. Health Life autonomic nervous system. Electr. J. 2010, 71–72. [Google Scholar]
| Selection Criteria |
|
| Exclusion Criteria |
|
| Characteristic | Category | VRM. G (n = 20) | CM. G (n = 20) | Cont. G (n = 20) | χ2 or F | p |
|---|---|---|---|---|---|---|
| Mean ± SD or N (%) | Mean ± SD or N (%) | Mean ± SD or N (%) | ||||
| Age (years) | 21.6 ± 1.47 | 21.75 ± 1.48 | 22.35 ± 1.35 | 1.533 | 0.225 | |
| Sex | Male | 5 (25%) | 7 (35%) | 7 (35%) | 0.296 | 0.745 |
| Female | 15 (75%) | 13 (65%) | 13 (65%) | |||
| Grade | 1 Grade | 2 (10%) | 0 (0%) | 1 (5%) | 1.868 | 0.164 |
| 2 Grade | 6 (30%) | 6 (30%) | 1 (5%) | |||
| 3 Grade | 11 (55%) | 11 (55%) | 16 (80%) | |||
| 4 Grade | 1 (5%) | 3 (15%) | 2 (10%) | |||
| Sleep duration (h/day) | 4–6 | 8 (40%) | 8 (40%) | 7 (35%) | 0.060 | 0.942 |
| 6–8 | 12 (60%) | 11 (55%) | 11 (55%) | |||
| over 8 | 0 (0%) | 1 (5%) | 2 (10%) | |||
| Medication status | Yes | 0 (0%) | 0 (0%) | 0 (0%) | ||
| No | 20 (100%) | 20 (100%) | 20 (100%) | |||
| Underlying disease | Yes | 0 (0%) | 0 (0%) | 0 (0%) | ||
| No | 20 (100%) | 20 (100%) | 20 (100%) | |||
| Vital sign | SBP | 114.65 ± 8.18 | 111.50 ± 7.96 | 115.70 ± 9.56 | 1.292 | 0.283 |
| DBP | 69.15 ± 11.00 | 72.50 ± 8.31 | 75.80 ± 7.92 | 2.625 | 0.081 | |
| Heart rate | 80.70 ± 7.22 | 82.60 ± 5.52 | 79.70 ±6.02 | 1.096 | 0.341 | |
| KMLSEQ | 46.60 ± 7.05 | 45.95 ± 8.86 | 47.70 ± 7.19 | 0.261 | 0.771 | |
| WASO (min) | 51.25 ± 18.60 | 50.65 ± 8.28 | 51.95 ± 10.31 | 0.049 | 0.952 | |
| SE (%) | 83.76 ± 5.53 | 83.97 ± 1.80 | 83.69 ± 2.03 | 0.035 | 0.966 | |
| DST (%) | 13.95 ± 2.31 | 14.50 ± 1.88 | 14.25 ± 1.41 | 0.420 | 0.659 | |
| PSS | 2.83 ± 0.69 | 2.91 ± 0.44 | 2.73 ± 0.39 | 0.600 | 0.552 | |
| SI | 4.65 ± 1.53 | 4.35 ± 1.23 | 5.10 ± 1.17 | 1.643 | 0.203 | |
| HRV | 7.66 ± 0.87 | 8.11 ± 1.31 | 8.28 ± 1.27 | 1.478 | 0.237 | |
| Variable | VRM. G (n = 20) | CM. G (n = 20) | Cont. G (n = 20) | F | p | |
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ±SD | Mean ± SD | ||||
| KMLSEQ | D0 | 46.60 ± 7.05 | 45.95 ± 8.86 | 47.70 ± 7.19 | 0.261 | 0.771 |
| D7 | 61.35 ± 14.00 | 52.20 ± 9.32 | 45.45 ± 6.19 | 10.400 | <0.001 | |
| Difference (D7 − D0) | 14.75 ± 14.57 | 6.25 ± 12.19 | −2.25 ± 10.64 | 10.179 | <0.001 | |
| Variable | VRM. G (n = 20) | CM. G (n = 20) | Cont. G (n = 20) | F | p | F (p) † | |
|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | |||||
| WASO (min) | D0 | 51.25 ± 18.60 | 50.65 ± 8.28 | 51.95 ± 10.31 | 0.049 | 0.952 | Time 0.120 (0.887) Group 8.106 (0.001) G × T 2.387 (0.055) |
| D4 | 48.90 ± 15.16 | 50.20 ± 4.46 | 57.30 ± 7.97 | 3.916 | 0.025 | ||
| D7 | 45.85 ± 6.37 | 48.60 ± 7.65 | 59.90 ± 7.93 | 20.540 | <0.001 | ||
| Difference (D7 − D0) | −5.40 ± 20.79 | −2.05 ± 13.11 | 7.98 ± 14.15 | 3.599 | 0.034 | ||
| SE (%) | D0 | 83.76 ± 5.53 | 83.97 ± 1.80 | 83.69 ± 2.03 | 0.035 | 0.966 | Time 0.571 (0.568) Group 15.553 (<0.001) G × T 3.123 (0.018) |
| D4 | 84.46 ± 2.24 | 84.15 ± 1.39 | 81.86 ± 2.07 | 10.794 | <0.001 | ||
| D7 | 85.50 ± 1.44 | 84.70 ± 1.42 | 81.31 ± 1.86 | 39.108 | <0.001 | ||
| Difference (D7 − D0) | 1.74 ± 5.88 | 0.73 ± 2.35 | −2.37 ± 2.48 | 5.954 | 0.004 | ||
| DST (%) | D0 | 13.95 ± 2.31 | 14.50 ± 1.88 | 14.25 ± 1.41 | 0.420 | 0.659 | Time 10.842 (<0.001) Group 11.308 (<0.001) G × T 4.458 (0.002) |
| D4 | 16.40 ± 5.68 | 15.05 ± 1.82 | 13.95 ± 1.64 | 2.362 | 0.103 | ||
| D7 | 19.65 ± 4.31 | 17.00 ± 4.04 | 14.00 ± 1.84 | 12.538 | <0.001 | ||
| Difference (D7 − D0) | 5.70 ± 4.62 | 2.50 ± 4.59 | −0.25 ± 2.69 | 10.698 | <0.001 | ||
| Variable | VRM. G (n = 20) | CM. G (n = 20) | Cont. G (n = 20) | F | p | |
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||||
| PSS | D0 | 2.83 ±0.69 | 2.91 ± 0.44 | 2.73 ± 0.39 | 0.600 | 0.552 |
| D7 | 2.24 ± 0.51 | 2.58 ± 0.45 | 2.69 ± 0.51 | 4.547 | 0.015 | |
| Difference (D7 − D0) | −0.59 ± 0.76 | −0.33 ± 0.56 | −0.04 ± 0.61 | 3.552 | 0.035 | |
| SI | D0 | 4.65 ± 1.53 | 4.35 ± 1.23 | 5.10 ± 1.17 | 1.643 | 0.203 |
| D7 | 2.05 ± 0.75 | 3.50 ± 0.61 | 4.80 ± 1.20 | 47.784 | <0.001 | |
| Difference (D7 − D0) | −2.60 ±1.60 | −0.85 ± 1.42 | −0.30 ± 1.98 | 10.179 | <0.001 | |
| HRV | D0 | 7.66 ± 0.87 | 8.11 ± 1.32 | 8.28 ± 1.27 | 1.478 | 0.237 |
| D7 | 8.65 ± 0.95 | 8.45 ± 1.15 | 7.75 ± 1.36 | 3.301 | 0.044 | |
| Difference (D7 − D0) | 0.99 ± 0.69 | 0.35 ± 0.93 | −0.53 ± 1.24 | 12.126 | <0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, K.-Y.; Hur, M.-H.; Kim, W.-J. Effects of Virtual Reality (VR)-Based Meditation on Sleep Quality, Stress, and Autonomic Nervous System Balance in Nursing Students. Healthcare 2024, 12, 1581. https://doi.org/10.3390/healthcare12161581
Kim K-Y, Hur M-H, Kim W-J. Effects of Virtual Reality (VR)-Based Meditation on Sleep Quality, Stress, and Autonomic Nervous System Balance in Nursing Students. Healthcare. 2024; 12(16):1581. https://doi.org/10.3390/healthcare12161581
Chicago/Turabian StyleKim, Ki-Yong, Myung-Haeng Hur, and Won-Jong Kim. 2024. "Effects of Virtual Reality (VR)-Based Meditation on Sleep Quality, Stress, and Autonomic Nervous System Balance in Nursing Students" Healthcare 12, no. 16: 1581. https://doi.org/10.3390/healthcare12161581
APA StyleKim, K.-Y., Hur, M.-H., & Kim, W.-J. (2024). Effects of Virtual Reality (VR)-Based Meditation on Sleep Quality, Stress, and Autonomic Nervous System Balance in Nursing Students. Healthcare, 12(16), 1581. https://doi.org/10.3390/healthcare12161581






