Robotics in Physical Rehabilitation: Systematic Review
Abstract
:1. Introduction
- Exploring the diversity of robotic technologies applied in motor recovery, from exoskeletons and robotic arms to personal assistant robots and brain–computer interfaces;
- Analyzing the advantages and limitations of each category of robotic systems in the specific context of motor recovery;
- Investigating the technical, economic, social, and cultural barriers that may limit access to or acceptance of robotic technology for motor recovery;
- Identifying facilitating factors that promote the adoption of robotic technologies, including funding initiatives, training programs for medical staff, and awareness campaigns.
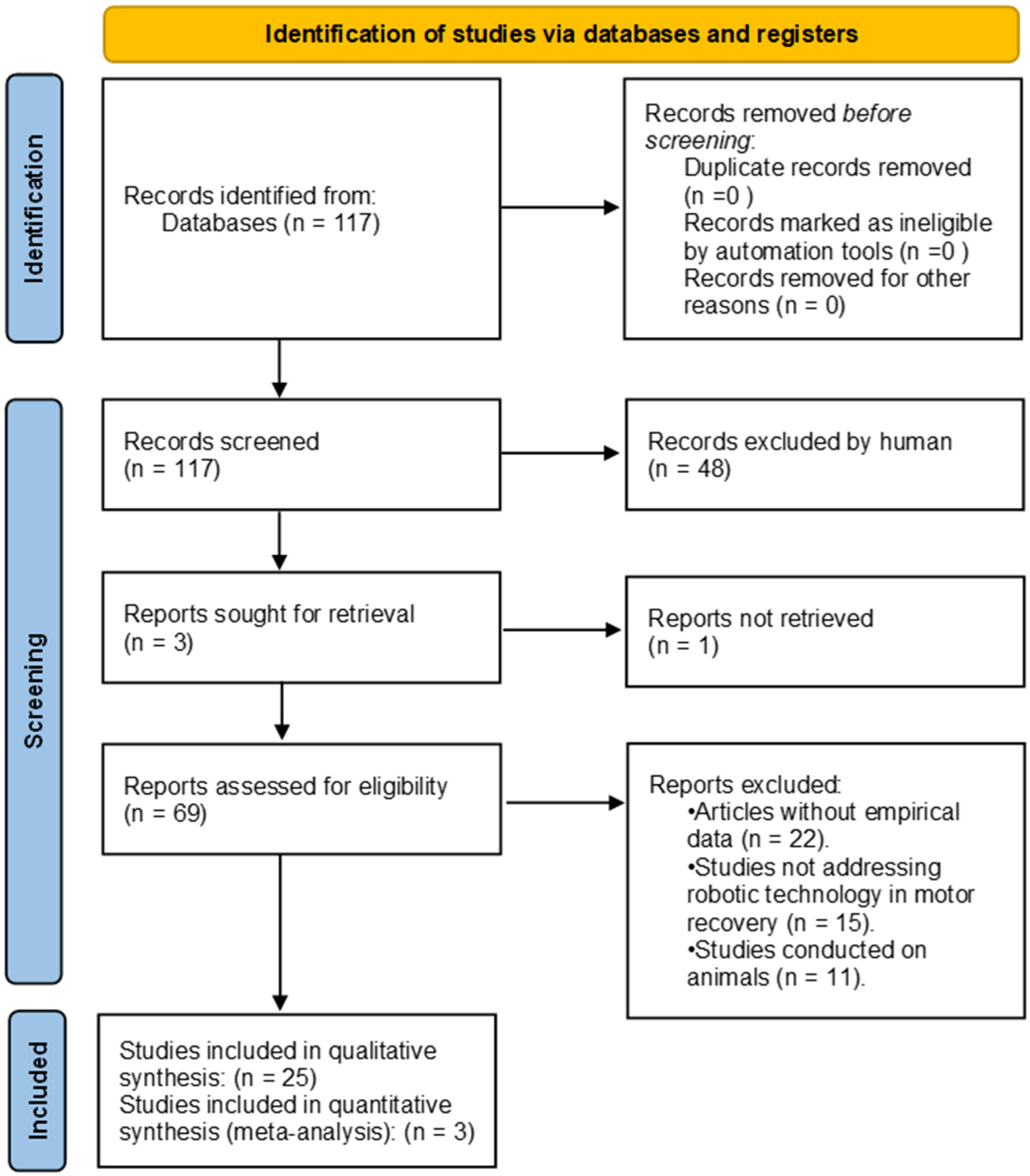
2. Materials and Methods
2.1. Literature Search
2.2. Inclusion and Exclusion Criteria
- Inclusion criteria: studies published within the last 15 years, focused on the use of robotic systems in motor recovery or patient care for people with physical disabilities, reviewing and analyzing published solutions with empirical data;
- Exclusion criteria: articles without empirical data, studies that did not specifically address the use of robotic technology in motor recovery or care for physically disabled patients, and studies conducted on animals or that did not involve human subjects.
2.3. Data Extraction
2.4. Quality Assessment
2.5. Risk of Bias
2.6. Data Synthesis
3. Classification of Robotic Systems for the Rehabilitation and Care of Patients with Disabilities
3.1. The Diversity of Robotic Technologies Applied in Motor Rehabilitation, Including Exoskeletons, Robotic Arms, Personal Assistant Robots, and Brain–Computer Interfaces
- Type of assistance:
- In upper limb motor rehabilitation, devices that are designed to assist and improve the motor function of the arms and hands are used, providing repetitive and controlled exercises that aid in recovery after strokes or other conditions. Examples include InMotion robotic arms, the ARMin exoskeleton, and robotic gloves such as HandSOME.
- In lower limb motor rehabilitation, robotic lower limb systems facilitate gait rehabilitation by supporting the body weight and guiding leg movements in a way that mimics natural walking. Examples include Lokomat and the ReWalk exoskeleton.
- Some robotic systems are designed to help people with reduced mobility to perform various daily activities, such as feeding, dressing, and handling objects. Examples include the PR2 personal assistance robot and the JACO robotic system.
- Some interactive robots, such as NAO and Pepper, and the PARO robot are used to improve social interaction and communication skills, especially among individuals with autism or neurodegenerative conditions. These robots are intended to enhance social and emotional skills, provide cognitive stimulation, improve well-being, and reduce feelings of isolation.
- Type of rehabilitation therapy:
- In passive rehabilitation therapy, the robot guides the patient’s limb through a range of motions without the patient exerting any effort. This approach is essential in the early stages of rehabilitation when the patient has limited mobility or reduced muscle strength.
- In active rehabilitation therapy, the patient initiates the movement, and the robot helps only when necessary. This method stimulates neuroplasticity and encourages the relearning of motor skills through active practice.
- Bilateral rehabilitation therapy involves the simultaneous use of both limbs, where the activity of a healthy limb is mirrored or assisted by the robot on the affected limb. This type of therapy is used to improve coordination and movement symmetry between the upper or lower limbs.
- User interaction mode:
- Direct interfaces allow users to interact directly with the device through physical buttons, touchpads, or gesture control. This includes rehabilitation systems that use touch screens or motion sensors to capture and respond to user actions, such as the HapticMaster Robotic Arm system.
- Neuromotor interfaces use the patient’s neurological signals for control, such as brain–computer interfaces (BCI) that enable robotic control through brain activity, facilitating rehabilitation for individuals with very limited movements, or EMG (electromyographic) sensors that detect the user’s movement intentions.
- AI adaptation-powered interfaces automatically adapt to the user’s needs without direct intervention, using artificial intelligence algorithms to optimize therapy. These interfaces adjust the level of assistance or resistance according to the user’s progress, such as rehabilitation systems that use machine learning to customize therapeutic exercises.
- Location of use:
- Robots used in hospital clinics or rehabilitation centers are designed to provide intensive care under the direct supervision of specialists. As an example, the BRAVO exoskeleton for upper limb rehabilitation is used in clinical environments.
- Some robotized systems have been adapted for use at home, providing patients the opportunity to continue therapy in the comfort of their own residence. For example, robotic gloves like HandSOME are used to improve hand dexterity.
- Robotic systems for parameterized and remotely controlled therapy by specialists through IoT technologies can be used in a teletherapy context.
- Mechanical structure:
- End-effector structured devices focus on interaction with one or more specific parts of the body (end effectors) such as the hands, legs, or head. They are used in specific rehabilitation exercises, providing assisted movement and sensory feedback. The Bi-Manu-Track is an example of an end-effector device.
- Exoskeletons are external robotic devices that are mounted on the body, providing motor support and assistance to people with disabilities. They are especially used for rehabilitating patients with paralysis or muscle weakness, facilitating movement of the upper or lower limbs through mechanical support and sometimes electrical stimulation. Examples of exoskeletons include ARMin III and T-WREX.
- Wearable robotics are lightweight and flexible devices that can be worn on the body, providing continuous support in daily activities or rehabilitation exercises. They are ideal for long-term use, especially in home environments.
- Soft robotics use flexible and adaptable materials that mimic the natural movements of the human body. This category is designed to provide safer and more comfortable interaction with the user, making it ideal for patients requiring gentle therapy and support in precision movements.
- Type of actuators:
- Electric motors (AC/DC) are the most common in robotic systems due to their precise control over speed and position. They are ideal for rehabilitation exercises that require fine adjustments of movement.
- Hydraulic and pneumatic motors provide significant force and are often used in exoskeletons or other devices that require support for body weight. However, they are less precise than electric motors and can be more challenging to control.
- Functional electrical stimulation (FES) involves applying electrical impulses to muscles to induce muscle contractions. It is used in combination with robotic devices to improve muscle strength and facilitate motor retraining.
- Control structure:
- Open-loop controls are used in the initial stages of rehabilitation, where precise control is less critical. These systems operate without direct feedback, applying control actions based on a predefined set of instructions without adjusting them in real time.
- Closed-loop PID controls (proportional–integral–derivative) are widely used due to their simplicity and ability to provide stable and efficient control for a variety of tasks.
- Robust control applied in robotic rehabilitation systems utilizes a fractional approach to control a seven degrees of freedom (DoF) exoskeleton, providing efficient management of friction dynamics and disturbances. The main advantage is its advanced ability to withstand uncertainties, parameter changes, and perturbations, such as a patient’s hand tremors.
- Adaptive control with active disturbance rejection (ADRC) modifies its behavior to adapt to changes in system parameters or uncertain parameters. It is preferred for its ability to simplify the control system while providing advanced disturbance and uncertainty rejection capabilities.
- Hybrid control combines elements of open and closed loop systems, providing flexibility in treatment by adapting to different stages of rehabilitation.
- The type of control structure is not the primary focus of this work, as all identified types have proven to be effective.
- Control inputs:
- Transducers for the forces and torques applied by the patient or the robot provide feedback for adjusting assistance. The major advantage arises in the measurement or generation of torque moments, which can be very precisely achieved in robotic systems compared to traditional manual therapy, where this aspect is subjective.
- Optical encoders are used to measure position and angular speed, ensuring precise motion control.
- EMG (electromyographic) signals capture muscle activity to initiate or guide robotic movement, facilitating a more natural and intuitive interaction with the user.
- Pressure measurements help determine the applied force and appropriately adjust the assistance in the case of hydraulic or pneumatic actuators.
3.2. Analysis of the Advantages and Limitations of Each Category of Robotic Systems
- Exoskeleton: Advantages, mobility support and intensive rehabilitation; Limitations, high cost and high weight.
- Robotic arms: Advantages, precision in fine movements; Limitations, the need for controlled and stable space for use.
3.3. Investigation of Technical, Economic, Social, and Cultural Barriers
- Technical: Need for constant calibration and maintenance.
- Economic: Limited budgets of medical institutions.
- Social: Negative perception of advanced technology in traditional communities.
3.4. Identifying Facilitative Factors for the Adoption of Robotic Technologies
- Funding: Government grants for the acquisition of robotic equipment.
- Training programs: Specialized courses for therapists and biomedical engineers.
- Awareness campaigns: Educational programs in the media and medical conferences.
4. Results
5. Discussion and Conclusions
5.1. Discussion
5.1.1. Full Brain–Computer Interface (BCI) Integration
5.1.2. Personalizing Robotic Therapies
5.1.3. Accessibility and Costs of Robotic Systems
5.1.4. Integration into Clinical Practice
5.1.5. Long-Term Evaluation of the Effectiveness of Robotic Therapies
5.1.6. Social and Cultural Acceptance of Robotic Technologies
5.2. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. World Report on Disability. Available online: https://www.who.int/health-topics/disability#tab=tab_1 (accessed on 13 February 2024).
- Ayerbe, L.; Ayis, S.; Wolfe, C.D.A.; Rudd, A.G. Natural history, predictors and outcomes of depression after stroke: Systematic review and meta-analysis. Br. J. Psychiatry 2013, 202, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Vélez-Guerrero, M.A.; Callejas-Cuervo, M.; Mazzoleni, S. Artificial Intelligence-Based Wearable Robotic Exoskeletons for Upper Limb Rehabilitation: A Review. Sensors 2021, 21, 2146. [Google Scholar] [CrossRef]
- The Project. Available online: http://www.ddskills.eu/THE-PROJECT (accessed on 15 February 2024).
- Krebs, H.I.; Volpe, B.T. Rehabilitation robotics: Technology and application. J. NeuroEng. Rehabil. 2015, 12, 1. [Google Scholar]
- Fareh, R.; Elsabe, A.; Baziyad, M.; Kawser, T.; Brahmi, B.; Rahman, M.H. A Review of the Advancements in Robotic Upper Extremity Rehabilitation. Sensors 2023, 23, 5054. [Google Scholar] [CrossRef]
- Yoo, S.D.; Lee, H.H. The Effect of Robot-Assisted Training on Arm Function, Walking, Balance, and Activities of Daily Living After Stroke: A Systematic Review and Meta-Analysis. Brain Neurorehabil. 2023, 16, 24. [Google Scholar] [CrossRef] [PubMed]
- Veerbeek, J.M.; Langbroek-Amersfoort, A.C.; van Wegen, E.E.; Meskers, C.G.; Kwakkel, G. Effects of Robot-Assisted Therapy for the Upper Limb After Stroke: A Systematic Review and Meta-analysis. Neurorehabil. Neural Repair 2017, 31, 107–121. [Google Scholar] [CrossRef] [PubMed]
- Johansen, T.; Sørensen, L.; Kolskår, K.K.; Strøm, V.; Wouda, M.F. Effectiveness of robot-assisted arm exercise on arm and hand function in stroke survivors—A systematic review and meta-analysis. J. Rehabil. Assist. Technol. Eng. 2023, 26910, 20556683231183639. [Google Scholar] [CrossRef]
- Grigoras, A.V.; Ignat, B.; Poboroniuc, M.S.; Popescu, D.; Popescu, C.D. State of the Art and Efficiency of Robotic Therapy in Upper Limb Rehabilitation: A Literature Review. Rom. J. Neurol. 2015, 14, 175–181. [Google Scholar] [CrossRef]
- Akbari, A.; Haghverd, F.; Behbahani, S. Robotic Home-Based Rehabilitation Systems Design: From a Literature Review to a Conceptual Framework for Community-Based Remote Therapy During COVID-19 Pandemic. Front. Robot. AI 2021, 8, 612331. [Google Scholar] [CrossRef]
- Nazar, P.S.; Pott, P.P. Ankle Rehabilitation Robotic Systems for domestic use—A systematic review. Curr. Dir. Biomed. Eng. 2022, 8, 65–68. [Google Scholar] [CrossRef]
- Kalra, R.; Gupta, M.A. Review on Potential of Robotic Rehabilitation in Health Care System. Int. J. Med. Sci. Clin. Invent. 2021, 8, 5392–5413. [Google Scholar] [CrossRef]
- Warutkar, V.; Dadgal, R.; Mangulkar, U.R. Use of Robotics in Gait Rehabilitation Following Stroke: A Review. Cureus 2022, 14, 4. [Google Scholar] [CrossRef]
- Krzyżańska, A.; Dziurda, M.; Maćkowiak, M.; Michalak, M.; Jóźwiak, M. Effect of robot-assisted gait training on functional capabilities in individuals with cerebral palsy: A systematic review and meta-analysis. Rheumatol. Forum 2024, 10, 61–71. [Google Scholar] [CrossRef]
- Gandolfi, M.; Mazzoleni, S.; Morone, G.; Iosa, M.; Galletti, F.; Smania, N. The role of feedback in the robotic-assisted upper limb rehabilitation in people with multiple sclerosis: A systematic review. Expert. Rev. Med. Devices 2023, 20, 35–44. [Google Scholar] [CrossRef]
- Gonzalez, A.; Garcia, L.; Kilby, J.; McNair, P. Robotic devices for pediatric rehabilitation: A review of design features. BioMed Eng. OnLine 2021, 20, 89. [Google Scholar] [CrossRef]
- Fiore, S.; Battaglino, A.; Sinatti, P.; Sánchez-Romero, E.; Ruiz-Rodríguez, I.; Manca, M.; Gargano, S.; Villafañe, J. The effectiveness of robotic rehabilitation for the functional recovery of the upper limb in post-stroke patients: A systematic review. Retos 2023, 50, 91–101. [Google Scholar] [CrossRef]
- Basteris, A.; Nijenhuis, S.M.; Stienen, A.H.; Buurke, J.H.; Prange, G.B.; Amirabdollahian, F. Training modalities in robot-mediated upper limb rehabilitation in stroke: A framework for classification based on a systematic review. J. Neuroeng. Rehabil. 2014, 11, 111. [Google Scholar] [CrossRef] [PubMed]
- Onose, G.; Popescu, N.; Munteanu, C.; Ciobanu, V.; Sporea, C.; Mirea, M.-D.; Daia, C.; Andone, I.; Spînu, A.; Mirea, A. Mobile Mechatronic/Robotic Orthotic Devices to Assist-Rehabilitate Neuromotor Impairments in the Upper Limb: A Systematic and Synthetic Review. Front. Neurosci. 2018, 12, 577. [Google Scholar] [CrossRef]
- Carpinella, I.; Lencioni, T.; Bowman, T.; Bertoni, R.; Turolla, A.; Ferrarin, M.; Jonsdottir, J. Effects of Robot Therapy on Upper Body Kinematics and Arm Function in Persons Post Stroke: A Pilot Randomized Controlled Trial. J. Neuroeng. Rehabil. 2020, 17, 10. [Google Scholar] [CrossRef] [PubMed]
- Budhota, A.; Chua, K.; Hussain, A.; Kager, S.; Cherpin, A.; Contu, S.; Vishwanath, D.; Kuah, C.; Ng, C.; Yam, L.; et al. Robotic Assisted Upper Limb Training Post Stroke: A Randomized Control Trial Using Combinatory Approach Toward Reducing Workforce Demands. Front. Neurol. 2021, 12, 622014. [Google Scholar] [CrossRef]
- Reis, S.; Bernardo, W.; Oshiro, C.; Krebs, H.; Conforto, A. Effects of Robotic Therapy Associated with Noninvasive Brain Stimulation on Upper-Limb Rehabilitation After Stroke: Systematic Review and Meta-analysis of Randomized Clinical Trials. Neurorehabil. Neural Repair. 2021, 35, 256–266. [Google Scholar] [CrossRef]
- Dehem, S.; Gilliaux, M.; Stoquart, G.; Detrembleur, C.; Jacquemin, G.; Palumbo, S.; Frederick, A.; Lejeune, T. Effectiveness of upper-limb robotic-assisted therapy in the early rehabilitation phase after stroke: A single-blind, randomised, controlled trial. Ann. Phys. Rehabil. Med. 2019, 62, 313–320. [Google Scholar] [CrossRef]
- Bressi, F.; Campagnola, B.; Cricenti, L.; Santacaterina, F.; Miccinilli, S.; Di Pino, G.; Fiori, F.; D’Alonzo, M.; Di Lazzaro, V.; Ricci, L.; et al. Upper limb home-based robotic rehabilitation in chronic stroke patients: A pilot study. Front. Neurorobot. 2023, 16, 1130770. [Google Scholar] [CrossRef]
- Colombo, R.; Pisano, F.; Delconte, C.; Mazzone, A.; Grioni, G.; Castagna, M.; Bazzini, G.; Imarisio, C.; Maggioni, G.; Pistarini, C. Comparison of Exercise Training Effect with Different Robotic Devices for Upper Limb Rehabilitation: A Retrospective Study. Eur. J. Phys. Rehabil. Med. 2017, 53, 240–248. [Google Scholar] [CrossRef]
- Wu, X.; Guarino, P.; Lo, A.C.; Peduzzi, P.; Wininger, M. Long-term Effectiveness of Intensive Therapy in Chronic Stroke. Neurorehabil. Neural Repair. 2015, 30, 583–590. [Google Scholar] [CrossRef]
- Just, F.; Gunz, D.; Duarte, J.; Simonetti, D.; Riener, R.; Rauter, G. Improving Usability of Rehabilitation Robots: Hand Module Evaluation of the ARMin Exoskeleton. In Wearable Robotics: Challenges and Trends; Carrozza, M., Micera, S., Pons, J., Eds.; Springer: Cham, Switzerland, 2019; Volume 22. [Google Scholar]
- Ai, Q.; Liu, Z.; Meng, W.; Liu, Q.; Xie, S.Q. Machine learning in robot assisted upper limb rehabilitation: A focused review. IEEE Trans. Cogn. Dev. Syst. 2023, 15, 2053–2063. [Google Scholar] [CrossRef]
- Ianosi-Andreeva-Dimitrova, A.; Mandru, D.S. Control systems of rehabilitation engineering equipment—A review. In Proceedings of the 2015 E-Health and Bioengineering Conference (EHB), Iasi, Romania, 19–21 November 2015; pp. 1–4. [Google Scholar]
- Pană, C.F.; Popescu, D.; Rădulescu, V.M. Patent Review of Lower Limb Rehabilitation Robotic Systems by Sensors and Actuation Systems Used. Sensors 2023, 23, 6237. [Google Scholar] [CrossRef] [PubMed]
- Boanta, C.; Brișan, C. Estimation of the Kinematics and Workspace of a Robot Using Artificial Neural Networks. Sensors 2022, 21, 8356. [Google Scholar] [CrossRef]
- Tătar, M.O.; Mondal, A.K.; Gupta, M.K. The Kinematic Model of 3 Dof Rehabilitation Robotic Exoskeletons. Robot. Manag. 2013, 2, 26–31. [Google Scholar]
- Shah, M.F.; Hussain, S.; Goecke, R.; Jamwal, P.K. Mechanism Design and Control of Shoulder Rehabilitation Robots: A Review. IEEE Trans. Med. Robot. Bionics 2023, 5, 780–792. [Google Scholar] [CrossRef]
- Dong, M.; Fan, W.; Li, J.; Zhou, X.; Rong, X.; Kong, Y.; Zhou, Y. A New Ankle Robotic System Enabling Whole-Stage Compliance Rehabilitation Training. IEEE/ASME Trans Mechatron. 2021, 3, 1490–1500. [Google Scholar]
- Abdallah, I.B.; Bouteraa, Y. Newly-Designed Wearable Robotic Hand Exoskeleton Controlled by EMG Signals and ROS Embedded Systems. Robotics 2023, 12, 95. [Google Scholar] [CrossRef]
- Xue, L.C.; Noor, A.M.; Zakaria, Z.; Nasir, N.F.M.; Norali, A.N.; Khiruddin, K.D.N. Neurorehabilitation Robot-Assisted for Stroke Recovery: Hybrid Exoskeleton Assistive Limb (HEAL). Indones. J. Electr. Eng. Inform. 2024, 11, 1143–1154. [Google Scholar] [CrossRef]
- Tucan, P.; Vaida, C.; Plitea, N.; Pisla, A.; Carbone, G.; Pisla, D. Risk-Based Assessment Engineering of a Parallel Robot Used in Post-Stroke Upper Limb Rehabilitation. Sustainability 2019, 11, 2893. [Google Scholar] [CrossRef]
- Vaida, C.; Birlescu, I.; Pisla, A.; Ulinici, I.-M.; Tarnita, D.; Carbone, G.; Pisla, D. Systematic Design of a Parallel Robotic System for Lower Limb Rehabilitation. IEEE Access 2020, 99, 34522–34537. [Google Scholar] [CrossRef]
- Major, K.; Major, Z.; Carbone, G.; Pîslă, A.; Vaida, C. Ranges of motion as basis for robot-assisted poststroke rehabilitation. Human. Vet. Med. 2016, 8, 192–196. [Google Scholar]
- Uivarosan, D.; Bungau, S.G.; Nistor-Cseppento, C.D.; Negru, P.A.; Bungau, A.F.; Sabau, A.M.; Tit, D.M.; Uivaraseanu, B.; Radu, A.-F. Application of Robotic Recovery Techniques to Stroke Survivors—Bibliometric Analysis. J. Pers. Med. 2022, 12, 2066. [Google Scholar] [CrossRef]
- Goyal, T.; Hussain, S.; Martinez-Marroquin, E.; Brown, N.A.T.; Jamwal, P.K. Stiffness-Observer-Based Adaptive Control of an Intrinsically Compliant Parallel Wrist Rehabilitation Robot. IEEE Trans. Hum.-Mach. Syst. 2023, 53, 65–74. [Google Scholar] [CrossRef]
- Covaciu, F.; Pisla, A.; Iordan, A.E. Development of a Virtual Reality Simulator for an Intelligent Robotic System Used in Ankle Rehabilitation. Sensors 2021, 4, 1537. [Google Scholar] [CrossRef]
- Chellal, A.A.; Lima, J.; Fernandes, F.P.; Gonçalves, J.; Pacheco, M.; Monteiro, F.C. Overview of Robotic Based System for Rehabilitation and Healthcare. In Optimization, Learning Algorithms and Applications; Springer: Cham, Switzerland, 2021. [Google Scholar]
- Zhang, K.; Chen, X.; Liu, F.; Tang, H.; Wang, J.; Wen, W. System Framework of Robotics in Upper Limb Rehabilitation on Poststroke Motor Recovery. Behav. Neurol. 2018, 2018, 6737056. [Google Scholar] [CrossRef]
- Kyrarini, M.; Lygerakis, F.; Rajavenkatanarayanan, A.; Sevastopoulos, C.; Nambiappan, H.R.; Chaitanya, K.K.; Babu, A.R.; Mathew, J.; Makedon, F. A Survey of Robots in Healthcare. Technologies 2021, 9, 8. [Google Scholar] [CrossRef]
- Madan, R.; Valdez, S.; Kim, D.; Fang, S.; Zhong, L.; Virtue, D.T.; Bhattacharjee, T. A Robot-Assisted Bed Bathing System with Multimodal Perception and Integrated Compliance. In Proceedings of the HRI ‘24: ACM/IEEE International Conference on Human-Robot Interaction, Boulder, CO, USA, 11–15 March 2024. [Google Scholar]
- Zlatintsi, A.; Dometios, A.C.; Kardaris, N.; Rodomagoulakis, I.; Koutras, P.; Papageorgiou, X.; Maragos, P.; Tzafestas, C.S.; Vartholomeos, P.; Hauer, K.; et al. I-Support: A Robotic Platform of an Assistive Bathing Robot. Robot. Auton. Syst. 2020, 126, 103451. [Google Scholar] [CrossRef]
- Hai, N.D.X.; Thinh, N.T. Robotic Mechanism Using Water Jet for Scalp Wash and Massage Servicing Patients Research. Int. J. Robot. 2021, 10, 422–428. [Google Scholar]
- Pons, J.L. Wearable Robots: Biomechatronic Exoskeletons; Willey: Hoboken, NJ, USA, 2008; ISBN 978-0-470-51294-4. [Google Scholar]
- Maciejasz, P.; Eschweiler, J.; Gerlach-Hahn, K.; Jansen-Troy, A.; Leonhardt, S. A survey on robotic devices for upper limb rehabilitation. J. Neuroeng. Rehabil. 2014, 11, 3. [Google Scholar] [CrossRef]
- Proietti, T.; Ambrosini, E.; Pedrocchi, A.; Micera, S. Wearable Robotics for Impaired Upper-Limb Assistance and Rehabilitation: State of the Art and Future Perspectives. IEEE Access 2022, 10, 106117–106134. [Google Scholar] [CrossRef]
- Fugl-Meyer, A.R.; Jääskö, L.; Leyman, I.; Olsson, S.; Steglind, S. The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scand. J. Rehabil. Med. 1975, 7, 13–31. [Google Scholar]
- Lum, P.S.; Burgar, C.G.; Shor, P.C.; Majmundar, M.; Van der Loos, M. Robot-assisted movement training compared with conventional therapy techniques for the rehabilitation of upper-limb motor function after stroke. Arch. Phys. Med. Rehabil. 2002, 7, 952–959. [Google Scholar] [CrossRef]
- Volpe, B.T.; Krebs, H.I.; Hogan, N.; Edelstein, L.; Diels, C.; Aisen, M. A novel approach to stroke rehabilitation: Robot-aided sensorimotor stimulation. Neurology 2000, 54, 1938–1944. [Google Scholar] [CrossRef]
- Rodgers, H.; Bosomworth, H.; Krebs, H.; van Wijck, F.; Howel, D.; Wilson, N.; Shaw, L. Robot-assisted training for the upper limb after stroke (RATULS): A multicentre randomised controlled trial. Lancet 2019, 394, 51–62. [Google Scholar] [CrossRef]
- Klamroth-Marganska, V.; Blanco, J.; Campen, K.; Curt, A.; Dietz, V.; Ettlin, T.; Felder, M.; Fellinghauer, B.; Guidali, M.; Kollmar, A.; et al. Three-dimensional, task-specific robot therapy of the arm after stroke: A multicentre, parallel-group randomized trial. Lancet Neurol. 2014, 13, 159–166. [Google Scholar] [CrossRef]
- Dziemian, K.; Kiper, A.; Baba, A.; Baldan, F.; Alhelou, M.; Agostini, M.; Turolla, A.; Kiper, P. The effect of robot therapy assisted by surface EMG on hand recovery in post-stroke patients. A pilot study. Med. Rehabil. 2017, 21, 4–10. [Google Scholar] [CrossRef]
- Picelli, A.; Tamburin, S.; Passuello, M.; Waldner, A.; Smania, N. Robot-assisted arm training in patients with Parkinson’s disease: A pilot study. J. Neuroeng. Rehabil. 2014, 11, 28. [Google Scholar] [CrossRef]
- Housman, S.; Le, V.; Rahman, T.; Sanchez, R.; Reinkensmeyer, D. Arm-Training with T-WREX After Chronic Stroke: Preliminary Results of a Randomized Controlled Trial. In Proceedings of the IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 13–15 June 2007. [Google Scholar]
- Lo, A.C.; Guarino, P.D.; Richards, L.G.; Haselkorn, J.K.; Wittenberg, G.F.; Federman, D.G.; Ringer, R.J.; Wagner, T.H.; Krebs, H.I.; Volpe, B.T.; et al. Robot-assisted therapy for long-term upper-limb impairment after stroke. N. Engl. J. Med. 2010, 362, 1772–1783. [Google Scholar] [CrossRef]
- Liao, W.W.; Wu, C.Y.; Hsieh, Y.W.; Lin, K.C.; Chang, W.Y. Effects of robot-assisted upper limb rehabilitation on daily function and real-world arm activity in patients with chronic stroke: A randomized controlled trial. Clin. Rehabil. 2012, 26, 111–120. [Google Scholar] [CrossRef]
- Hwang, C.; Seong, J.; Son, D. Individual finger synchronized robot-assisted hand rehabilitation in subacute to chronic stroke: A prospective randomized clinical trial of efficacy. Clin. Rehabil. 2012, 26, 696–704. [Google Scholar] [CrossRef]
- Hung, C.; Hsieh, Y.; Wu, C.; Lin, K.; Lin, J.; Yeh, L.; Yin, H. Comparative Assessment of Two Robot-Assisted Therapies for the Upper Extremity in People with Chronic Stroke. Am. J. Occup. Ther. 2019, 73, 7301205010p1–7301205010p9. [Google Scholar] [CrossRef]
- Chung, B.P.H. Effectiveness of robotic-assisted gait training in stroke rehabilitation: A retrospective matched control study. Hong Kong Physiother. J. 2017, 36, 10–16. [Google Scholar] [CrossRef]
- Park, J.H.; Shin, Y.I.; You, J.S.H.; Park, M.S. Comparative Effects of Robotic-assisted Gait Training Combined with Conventional Physical Therapy on Paretic Hip Joint Stiffness and Kinematics Between Sub-acute and Chronic Hemiparetic Stroke. Neuro Rehabil. 2018, 42, 181–190. [Google Scholar] [CrossRef]
- Li, Z.; Zhang, X.; Wang, T.; Chen, Y. Use of robotic exoskeletons for gait training after stroke: A systematic review and meta-analysis. J. Neuroeng. Rehabil. 2021, 18, 120. [Google Scholar]
- Mehrholz, J.; Thomas, S.; Kugler, J.; Pohl, M.; Elsner, B. Electromechanical-assisted training for walking after stroke. Cochrane Database Syst. Rev. 2020, 5, CD006185, Update in Cochrane Database Syst Rev. 2020, 10, CD006185. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhao, W.; Wan, C.; Wu, X.; Huang, J.; Wang, X.; Huang, G.; Ding, W.; Chen, Y.; Yang, J.; et al. Exoskeleton rehabilitation robot training for balance and lower limb function in sub-acute stroke patients: A pilot, randomized controlled trial. J. Neuroeng. Rehabil. 2024, 21, 98. [Google Scholar] [CrossRef]
- Kueper, N.; Kim, S.K.; Kirchner, E.A. Avoidance of specific calibration sessions in motor intention recognition for exoskeleton-supported rehabilitation through transfer learning on EEG data. Sci. Rep. 2024, 14, 16690. [Google Scholar] [CrossRef]
- Nicolas-Alonso, L.F.; Gomez-Gil, J. Brain computer interfaces, a review. Sensors 2012, 12, 1211–1279. [Google Scholar] [CrossRef]
- Shih, J.J.; Krusienski, D.J.; Wolpaw, J.R. Brain-computer interfaces in medicine. Mayo Clin. Proc. 2012, 87, 268–279. [Google Scholar] [CrossRef]
- Huang, V.S.; Krakauer, J.W. Robotic neurorehabilitation: A computational motor learning perspective. J. Neuroeng. Rehabil. 2019, 16, 34–46. [Google Scholar] [CrossRef]
- Kwakkel, G.; Kollen, B.J.; Krebs, H.I. Effects of robot-assisted therapy on upper limb recovery after stroke: A systematic review. Neurorehabil. Neural Repair. 2017, 22, 111–121. [Google Scholar] [CrossRef]
- Mehrholz, J.; Pollock, A.; Pohl, M.; Kugler, J.; Elsner, B. Systematic review with network meta-analysis of randomized controlled trials of robotic-assisted arm training for improving activities of daily living and upper limb function after stroke. J. Neuroeng. Rehabil. 2020, 17, 83. [Google Scholar] [CrossRef]
| Type | Description | Reference |
|---|---|---|
| Systematic reviews and meta-analyses | Synthesizes the results from multiple primary research studies on a specific topic, providing a comprehensive assessment of the availability and quality of evidence. Examines the overall effectiveness of robot-assisted therapy in upper limb or gait rehabilitation. | [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20] |
| Randomized Controlled Trials (RCTs), Case and Pilot Studies | Compares the effectiveness of an intervention with a control group in a well-structured setting with randomly selected participants. Directly tests the effects of robot-assisted interventions compared to standard rehabilitation methods. Explores the impact of interventions on individual cases or small groups, providing initial data for further research. Initial use of robotic therapies for specific patients or in preliminary settings. | [21,22,23,24,25,26,27] |
| Exploratory Studies and Technical Development Analyses | Focuses on the development, improvement, and evaluation of technical aspects of robotic devices, including design and implementation. Describes technological innovations in robotic rehabilitation or analyzes specific aspects of system performance. Investigates the potential and practicality of novel approaches in a research setting, often in the early stages. Tests new methodologies or technologies in rehabilitation to determine the viability of more rigorous future studies. | [28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45] |
| Robotic systems for patient care | Investigates robotic systems used for dressing, eating, or washing. | [46,47,48,49] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Banyai, A.D.; Brișan, C. Robotics in Physical Rehabilitation: Systematic Review. Healthcare 2024, 12, 1720. https://doi.org/10.3390/healthcare12171720
Banyai AD, Brișan C. Robotics in Physical Rehabilitation: Systematic Review. Healthcare. 2024; 12(17):1720. https://doi.org/10.3390/healthcare12171720
Chicago/Turabian StyleBanyai, Adriana Daniela, and Cornel Brișan. 2024. "Robotics in Physical Rehabilitation: Systematic Review" Healthcare 12, no. 17: 1720. https://doi.org/10.3390/healthcare12171720
APA StyleBanyai, A. D., & Brișan, C. (2024). Robotics in Physical Rehabilitation: Systematic Review. Healthcare, 12(17), 1720. https://doi.org/10.3390/healthcare12171720





