Syndromic Surveillance in Public Health Emergencies: A Systematic Analysis of Cases Related to Exposure to 2023 Floodwaters in Romagna, Italy
Abstract
1. Introduction
2. Materials and Methods
2.1. Population
2.2. Forms and Data Collection
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Agency for Territorial Security and Civil Protection, Emilia-Romagna Region. Alert of 2 May 2023. Available online: https://protezionecivile.regione.emilia-romagna.it/notizie/2023/maggio/2-maggio-3-maggio-allerta-rossa-arancio-gialla-idro-idrogeo-vento (accessed on 31 August 2024).
- Higher Institute for Environmental Protection and Research. Flood in Emilia-Romagna: Record Rainfall, Rivers and Waterways Overflowed. Available online: https://www.isprambiente.gov.it/it/archivio/notizie-e-novita-normative/notizie-ispra/2023/05/maltempo-in-emilia-romagna-piogge-record-fiumi-e-corsi-dacqua-esondati (accessed on 31 August 2024).
- Emilia-Romagna Region. Post-Flood: Here Is the Report of the Technical-Scientific Commission. Available online: https://www.regione.emilia-romagna.it/notizie/2023/dicembre/post-alluvione-ecco-il-rapporto-della-commissione-tecnico-scientifica-201cin-emilia-romagna-un-evento-senza-precedenti-nella-storia-osservata201d (accessed on 31 August 2024).
- Save the Children. Flood in Emilia-Romagna. Available online: https://www.savethechildren.it/blog-notizie/alluvione-emilia-romagna#:~:text=Dagli%20ultimi%20aggiornamenti%2C%20l’alluvione,risultano%20attive%20oltre%20900%20frane (accessed on 31 August 2024).
- Agency for Environment, Energy and Prevention, Emilia-Romagna Region. Ecoscienza—Issue 5 of 2023. Available online: https://www.arpae.it/it/ecoscienza/numeri-ecoscienza/anno-2023/numero-5-anno-2023 (accessed on 13 August 2024).
- Italian National Institute of Health. Available online: https://www.iss.it/-/in-zone-alluvionate-è-opportuno-seguire-le-indicazioni-delle-autorità-sanitarie (accessed on 31 August 2024).
- Italian Ministry of Health. Available online: https://www.salute.gov.it/portale/news/p3_2_1_1_1.jsp?lingua=italiano&menu=notizie&p=dalministero&id=6265 (accessed on 13 August 2024).
- Lai, H.; Hales, S.; Woodward, A.; Walker, C.; Marks, E.; Pillai, A.; Chen, R.X.; Morton, S.M. Effects of Heavy Rainfall on Waterborne Disease Hospitalizations among Young Children in Wet and Dry Areas of New Zealand. Environ. Int. 2020, 145, 106136. [Google Scholar] [CrossRef] [PubMed]
- Tornevi, A.; Axelsson, G.; Forsberg, B. Association between Precipitation Upstream of a Drinking Water Utility and Nurse Advice Calls Relating to Acute Gastrointestinal Illnesses. PLoS ONE 2013, 8, e69918. [Google Scholar] [CrossRef] [PubMed]
- Saulnier, D.D.; Brolin Ribacke, K.; von Schreeb, J. No Calm After the Storm: A Systematic Review of Human Health Following Flood and Storm Disasters. Prehosp. Disaster Med. 2017, 32, 568–579. [Google Scholar] [CrossRef] [PubMed]
- Weilnhammer, V.; Schmid, J.; Mittermeier, I.; Schreiber, F.; Jiang, L.; Pastuhovic, V.; Herr, C.; Heinze, S. Extreme Weather Events in Europe and Their Health Consequences—A Systematic Review. Int. J. Hyg. Environ. Health 2021, 233, 113688. [Google Scholar] [CrossRef] [PubMed]
- Jakubicka, T.; Vos, F.; Phalkey, R.; Guha-Sapir, D.; Marx, M. Health Impacts of Floods in Europe: Data Gaps and Information Needs from a Spatial Perspective; Centre for Research on the Epidemiology of Disasters (CRED): Brussels, Belgium, 2010. [Google Scholar]
- Mason, V.; Andrews, H.; Upton, D. The Psychological Impact of Exposure to Floods. Psychol. Health Med. 2010, 15, 61–73. [Google Scholar] [CrossRef] [PubMed]
- Mulchandani, R.; Armstrong, B.; Beck, C.R.; Waite, T.D.; Amlôt, R.; Kovats, S.; Leonardi, G.; Rubin, G.J.; Oliver, I. The English National Cohort Study of Flooding & Health: Psychological Morbidity at Three Years of Follow Up. BMC Public Health 2020, 20, 321. [Google Scholar]
- Alifu, H.; Hirabayashi, Y.; Imada, Y.; Shiogama, H. Enhancement of River Flooding Due to Global Warming. Sci. Rep. 2022, 12, 20687. [Google Scholar] [CrossRef] [PubMed]
- Alhudiri, I.; Zaghdani, A.A.; El Meshri, S.E.; Elmaghrabi, A.; Elzagheid, A. Libya Floods: Preventing a Public Health Crisis. The Lancet 2023, 402, 1854. [Google Scholar] [CrossRef] [PubMed]
- The International Rescue Committee. Libya: The IRC Warns of Public Health Crisis in Flood Affected Areas. Available online: https://www.rescue.org/uk/press-release/libya-irc-warns-public-health-crisis-flood-affected-areas (accessed on 31 August 2024).
- Ahern, M.; Kovats, R.S.; Wilkinson, P.; Few, R.; Matthies, F. Global Health Impacts of Floods: Epidemiologic Evidence. Epidemiol. Rev. 2005, 27, 36–46. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control (ECDC). Extreme Rainfall and Catastrophic Floods in Western Europe—29 July 2021; ECDC: Stockholm, Sweden, 2021. [Google Scholar]
- Italian National Institute of Health. RespiVirNet—Integrated Surveillance of Respiratory Viruses. Available online: https://respivirnet.iss.it/Default.aspx (accessed on 13 August 2024).
- U.S. Center for Disease Control and Prevention. Disaster-Related Morbidity and Mortality Surveillance. Available online: https://www.cdc.gov/environmental-health-response-and-recovery/php/about/mortality-surveillance.html?CDC_AAref_Val=https://www.cdc.gov/disasters/surveillance/index.html (accessed on 13 August 2024).
- Paterson, D.L.; Wright, H.; Harris, P.N. Health Risks of Flood Disasters. Clin. Infect. Dis. 2018, 67, 1450–1454. [Google Scholar] [CrossRef] [PubMed]
- Najibi, N.; Devineni, N. Recent Trends in the Frequency and Duration of Global Floods. Earth Syst. Dynam. 2018, 9, 757–783. [Google Scholar] [CrossRef]
- Mulder, A.C.; Pijnacker, R.; de Man, H.; van de Kassteele, J.; van Pelt, W.; Mughini-Gras, L. “Sickenin’ in the Rain”—Increased Risk of Gastrointestinal and Respiratory Infections After Urban Pluvial Flooding in a Population-Based Cross-Sectional Study in the Netherlands. BMC Infect. Dis. 2019, 19, 377. [Google Scholar] [CrossRef] [PubMed]
- Waite, T.D.; Chaintarli, K.; Beck, C.R.; Bone, A.; Amlôt, R.; Kovats, S.; Reacher, M.; Armstrong, B.; Leonardi, G.; Rubin, G.J.; et al. The English National Cohort Study of Flooding and Health: Cross-Sectional Analysis of Mental Health Outcomes at Year One. BMC Public Health 2017, 17, 129. [Google Scholar] [CrossRef] [PubMed]
- Reacher, M.; McKenzie, K.; Lane, C.; Nichols, T.; Kedge, I.; Iversen, A.; Hepple, P.; Walter, T.; Laxton, C.; Simpson, J. Lewes Flood Action Recovery Team. Health Impacts of Flooding in Lewes: A Comparison of Reported Gastrointestinal and Other Illness and Mental Health in Flooded and Non-Flooded Households. Commun. Dis. Public Health 2004, 7, 56–63. [Google Scholar]
- Durkin, M.S.; Khan, N.; Davidson, L.L.; Zaman, S.S.; Stein, Z.A. The Effects of a Natural Disaster on Child Behaviour: Evidence for Posttraumatic Stress. Am. J. Public Health 1993, 83, 1549–1553. [Google Scholar] [CrossRef] [PubMed]
- Bokszczanin, A. Long-Term Negative Psychological Effects of a Flood on Adolescents. Pol. Psychol. Bull. 2002, 33, 55–61. [Google Scholar]
- Russoniello, C.V.; Skalko, T.K.; O’Brien, K.; McGhee, S.A.; Bingham-Alexander, D.; Beatley, J. Childhood Posttraumatic Stress Disorder and Efforts to Cope After Hurricane Floyd. Behav. Med. 2002, 28, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Min, S.-K.; Zhang, X.; Zwiers, F.W.; Hegerl, G.C. Human Contribution to More-Intense Precipitation Extremes. Nature 2011, 470, 378–381. [Google Scholar] [CrossRef] [PubMed]
- Harcourt, S.E.; Morbey, R.A.; Loveridge, P.; Carrilho, L.; Baynham, D.; Povey, E.; Fox, P.; Rutter, J.; Moores, P.; Tiffen, J.; et al. Developing and Validating a New National Remote Health Advice Syndromic Surveillance System in England. J. Public Health 2017, 39, 184–192. [Google Scholar] [CrossRef] [PubMed]
| Symptomatic | Rate × 1000 Population | ||
|---|---|---|---|
| Individuals | Estimate | 95% CI | |
| All (n = 24,433) | |||
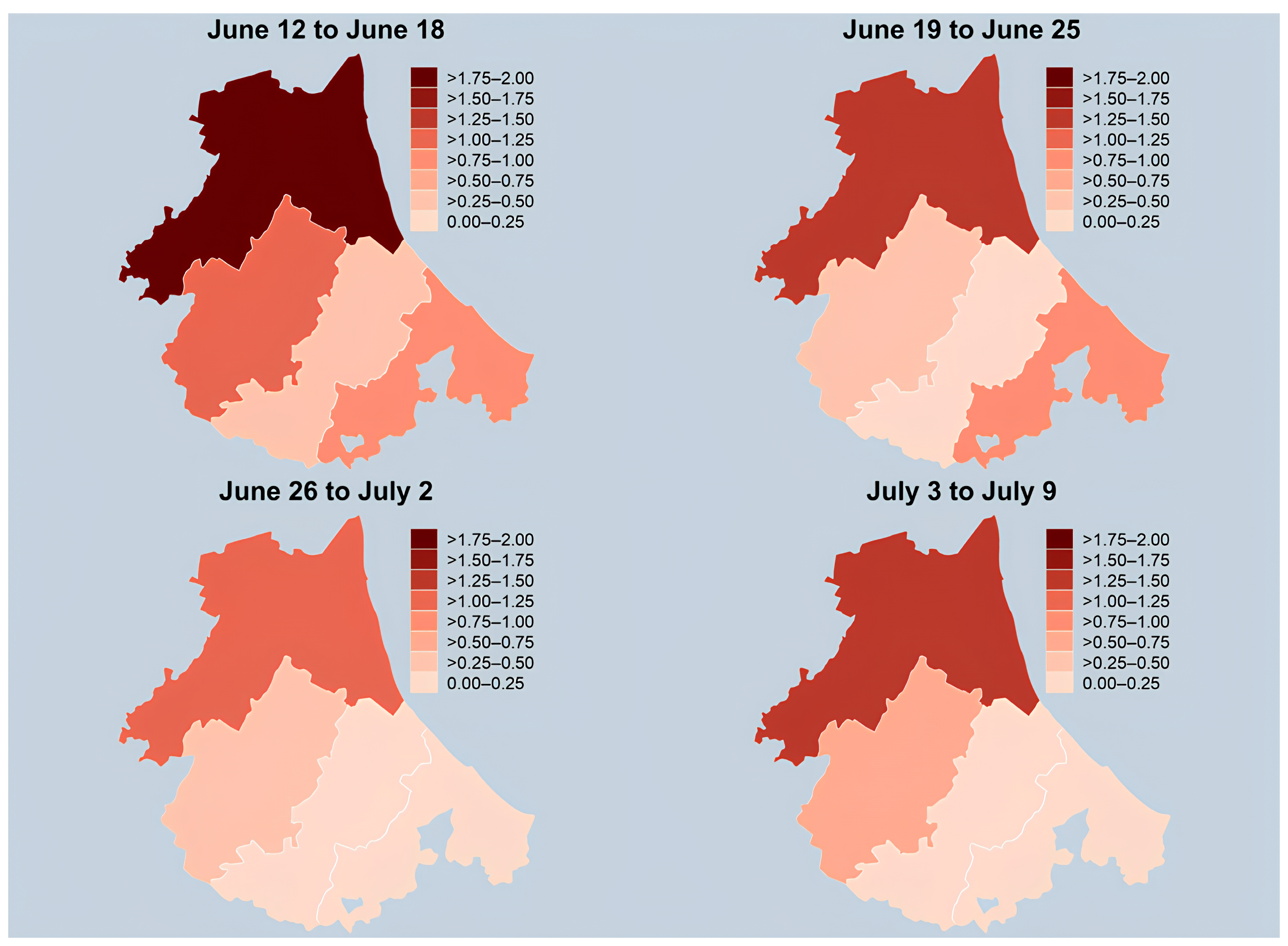
| Week 1 (12 June to 18 June) | 30 | 1.23 | 0.83, 1.75 |
| Week 2 (19 June to 25 June) | 21 | 0.86 | 0.53, 1.31 |
| Week 3 (26 June to 2 July) | 16 | 0.65 | 0.37, 1.06 |
| Week 4 (3 July to 9 July) | 19 | 0.78 | 0.47, 1.21 |
| Weeks 1–4 (12 June to 9 July) | 86 | 3.52 | 2.82, 4.35 |
| Weekly avg. (12 June to 9 July) | 21.5 | 0.88 | 0.70, 1.09 |
| Ravenna (n = 9585) | |||
| Week 1 (12 June to 18 June) | 18 | 1.88 | 1.11, 2.97 |
| Week 2 (19 June to 25 June) | 14 | 1.46 | 0.80, 2.45 |
| Week 3 (26 June to 2 July) | 12 | 1.25 | 0.65, 2.19 |
| Week 4 (3 July to 9 July) | 14 | 1.46 | 0.80, 2.45 |
| Weeks 1–4 (12 June to 9 July) | 58 | 6.05 | 4.59, 7.82 |
| Weekly avg. (12 June to 9 July) | 14.5 | 1.51 | 1.15, 1.96 |
| Forlì (n = 6809) | |||
| Week 1 (12 June to 18 June) | 7 | 1.03 | 0.41, 2.12 |
| Week 2 (19 June to 25 June) | 3 | 0.44 | 0.09, 1.29 |
| Week 3 (26 June to 2 July) | 3 | 0.44 | 0.09, 1.29 |
| Week 4 (3 July to 9 July) | 4 | 0.59 | 0.16, 1.50 |
| Weeks 1–4 (12 June to 9 July) | 17 | 2.50 | 1.45, 4.00 |
| Weekly avg. (12 June to 9 July) | 4.3 | 0.62 | 0.36, 1.00 |
| Cesena (n = 4171) | |||
| Week 1 (12 June to 18 June) | 2 | 0.48 | 0.06, 1.73 |
| Week 2 (19 June to 25 June) | 1 | 0.24 | 0.01, 1.34 |
| Week 3 (26 June to 2 July) | 1 | 0.24 | 0.01, 1.34 |
| Week 4 (3 July to 9 July) | 1 | 0.24 | 0.01, 1.34 |
| Weeks 1–4 (12 June to 9 July) | 5 | 1.20 | 0.39, 2.80 |
| Weekly avg. (12 June to 9 July) | 1.3 | 0.30 | 0.10, 0.70 |
| Rimini (n = 3868) | |||
| Week 1 (12 June to 18 June) | 3 | 0.78 | 0.16, 2.27 |
| Week 2 (19 June to 25 June) | 3 | 0.78 | 0.16, 2.27 |
| Week 3 (26 June to 2 July) | 0 | 0.00 | 0.00, 0.95 |
| Week 4 (3 July to 9 July) | 0 | 0.00 | 0.00, 0.95 |
| Weeks 1–4 (12 June to 9 July) | 6 | 1.55 | 0.57, 3.38 |
| Weekly avg. (12 June to 9 July) | 1.5 | 0.39 | 0.14, 0.84 |
| Symptomatic | Rate × 1000 Population | ||
|---|---|---|---|
| Individuals | Estimate | 95% CI | |
| All (n = 9170) | |||
| Week 1 (12 June to 18 June) | 30 | 3.27 | 2.21, 4.67 |
| Week 2 (19 June to 25 June) | 27 | 2.94 | 1.94, 4.28 |
| Week 3 (26 June to 2 July) | 35 | 3.82 | 2.66, 5.31 |
| Week 4 (3 July to 9 July) | 25 | 2.73 | 1.76, 4.02 |
| Weeks 1–4 (12 June to 9 July) | 117 | 12.76 | 10.55, 15.29 |
| Weekly avg. (12 June to 9 July) | 29.3 | 3.19 | 2.64, 3.82 |
| Ravenna (n = 3209) | |||
| Week 1 (12 June to 18 June) | 6 | 1.87 | 0.69, 4.07 |
| Week 2 (19 June to 25 June) | 5 | 1.56 | 0.51, 3.64 |
| Week 3 (26 June to 2 July) | 15 | 4.67 | 2.62, 7.71 |
| Week 4 (3 July to 9 July) | 10 | 3.12 | 1.49, 5.73 |
| Weeks 1–4 (12 June to 9 July) | 36 | 11.22 | 7.86, 15.53 |
| Weekly avg. (12 June to 9 July) | 9.0 | 2.80 | 1.96, 3.88 |
| Forlì (n = 3362) | |||
| Week 1 (12 June to 18 June) | 14 | 4.16 | 2.28, 6.99 |
| Week 2 (19 June to 25 June) | 10 | 2.97 | 1.43, 5.47 |
| Week 3 (26 June to 2 July) | 7 | 2.08 | 0.84, 4.29 |
| Week 4 (3 July to 9 July) | 8 | 2.38 | 1.03, 4.69 |
| Weeks 1–4 (12 June to 9 July) | 39 | 11.60 | 8.25, 15.86 |
| Weekly avg. (12 June to 9 July) | 9.8 | 2.90 | 2.06, 3.96 |
| Rimini (n = 2599) | |||
| Week 1 (12 June to 18 June) | 10 | 3.85 | 1.85, 7.08 |
| Week 2 (19 June to 25 June) | 12 | 4.62 | 2.39, 8.07 |
| Week 3 (26 June to 2 July) | 13 | 5.00 | 2.66, 8.55 |
| Week 4 (3 July to 9 July) | 7 | 2.69 | 1.08, 5.55 |
| Weeks 1–4 (12 June to 9 July) | 42 | 16.16 | 11.65, 21.84 |
| Weekly avg. (12 June to 9 July) | 10.5 | 4.04 | 2.91, 5.46 |
| 16 May to 11 June 2023 | 12 June to 9 July 2023 | |||
|---|---|---|---|---|
| Cases | Rate × 1000 Pop. | Cases | Rate × 1000 Pop. | |
| (95% CI) | (95% CI) | |||
| Skin infection | ||||
| All | 17 * | 0.80 (0.47, 1.28) | 8 | 0.33 (0.14, 0.65) |
| Ravenna | 7 * | 1.10 (0.44, 2.26) | 5 | 0.52 (0.17, 1.22) |
| Forlì | 6 | 0.88 (0.32, 1.92) | 1 | 0.15 (0.00, 0.82) |
| Cesena | 4 | 0.96 (0.26, 2.46) | 1 | 0.24 (0.01, 1.34) |
| Rimini | 0 | 0.00 (0.00, 0.95) | 1 | 0.26 (0.01, 1.44) |
| Diarrhea, vomiting or abdominal pain | ||||
| All | 48 * | 2.26 (1.67, 3.00) | 26 | 1.06 (0.70, 1.56) |
| Ravenna | 22 * | 3.45 (2.16, 5.22) | 19 | 1.98 (1.19, 3.10) |
| Forlì | 13 | 1.91 (1.02, 3.26) | 5 | 0.73 (0.24, 1.71) |
| Cesena | 13 | 3.12 (1.66, 5.33) | 0 | 0.00 (0.00, 0.88) |
| Rimini | 0 | 0.00 (0.00, 0.95) | 2 | 0.52 (0.06, 1.87) |
| Chest congestion, cough or suspected pneumonia | ||||
| All | 26 * | 1.23 (0.80, 1.79) | 36 | 1.47 (1.03, 2.04) |
| Ravenna | 11 * | 1.73 (0.86, 3.09) | 25 | 2.61 (1.69, 3.85) |
| Forlì | 10 | 1.47 (0.70, 2.70) | 5 | 0.73 (0.24, 1.71) |
| Cesena | 5 | 1.20 (0.39, 2.80) | 3 | 0.72 (0.15, 2.10) |
| Rimini | 0 | 0.00 (0.00, 0.95) | 3 | 0.78 (0.16, 2.27) |
| Conjunctivitis (Eye infection) | ||||
| All | 18 * | 0.85 (0.50, 1.34) | 5 | 0.20 (0.07, 0.48) |
| Ravenna | 10 * | 1.57 (0.75, 2.88) | 4 | 0.42 (0.11, 1.07) |
| Forlì | 6 | 0.88 (0.32, 1.92) | 1 | 0.15 (0.00, 0.82) |
| Cesena | 2 | 0.48 (0.06, 1.73) | 0 | 0.00 (0.00, 0.88) |
| Rimini | 0 | 0.00 (0.00, 0.95) | 0 | 0.00 (0.00, 0.95) |
| Otitis (Ear infection) | ||||
| All | 13 * | 0.61 (0.33, 1.05) | 7 | 0.29 (0.12, 0.59) |
| Ravenna | 6 * | 0.94 (0.35, 2.05) | 6 | 0.63 (0.23, 1.36) |
| Forlì | 3 | 0.44 (0.09, 1.29) | 0 | 0.00 (0.00, 0.54) |
| Cesena | 4 | 0.96 (0.26, 2.46) | 1 | 0.24 (0.01, 1.34) |
| Rimini | 0 | 0.00 (0.00, 0.95) | 0 | 0.00 (0.00, 0.95) |
| Fever (> 37.5 °C for ≥ 48 h) | ||||
| All | 26 * | 1.23 (0.80, 1.79) | 12 | 0.49 (0.25, 0.86) |
| Ravenna | 16 * | 2.51 (1.43, 4.08) | 7 | 0.73 (0.29, 1.50) |
| Forlì | 9 | 1.32 (0.60, 2.51) | 3 | 0.44 (0.09, 1.29) |
| Cesena | 1 | 0.24 (0.01, 1.34) | 0 | 0.00 (0.00, 0.88) |
| Rimini | 0 | 0.00 (0.00, 0.95) | 2 | 0.52 (0.06, 1.87) |
| Insomnia, agitation or anxiety | ||||
| All | 36 * | 1.70 (1.19, 2.35) | 4 | 0.16 (0.04, 0.42) |
| Ravenna | 20 * | 3.14 (1.92, 4.84) | 1 | 0.10 (0.00, 0.58) |
| Forlì | 11 | 1.62 (0.81, 2.89) | 3 | 0.44 (0.09, 1.29) |
| Cesena | 5 | 1.20 (0.39, 2.80) | 0 | 0.00 (0.00, 0.88) |
| Rimini | 0 | 0.00 (0.00, 0.95) | 0 | 0.00 (0.00, 0.95) |
| Cases | Rate × 1000 Pop. (95% CI) | |
|---|---|---|
| Skin infection | ||
| All | 13 | 1.42 (0.75, 2.42) |
| Ravenna | 6 | 1.87 (0.69, 4.07) |
| Forlì | 6 | 1.78 (0.65, 3.88) |
| Rimini | 1 | 0.38 (0.01, 2.14) |
| Diarrhea, vomiting or abdominal pain | ||
| All | 22 | 2.40 (1.50, 3.63) |
| Ravenna | 7 | 2.18 (0.88, 4.49) |
| Forlì | 8 | 2.38 (1.03, 4.69) |
| Rimini | 7 | 2.69 (1.08, 5.55) |
| Chest congestion, cough or suspected pneumonia | ||
| All | 52 | 5.67 (4.24, 7.44) |
| Ravenna | 16 | 4.99 (2.85, 8.10) |
| Forlì | 12 | 3.57 (1.84, 6.23) |
| Rimini | 24 | 9.23 (5.92, 13.74) |
| Conjunctivitis (Eye infection) | ||
| All | 5 | 0.55 (0.18, 1.27) |
| Ravenna | 2 | 0.62 (0.08, 2.25) |
| Forlì | 1 | 0.30 (0.01, 1.66) |
| Rimini | 2 | 0.77 (0.09, 2.78) |
| Otitis (Ear infection) | ||
| All | 9 | 0.98 (0.45, 1.86) |
| Ravenna | 2 | 0.62 (0.08, 2.25) |
| Forlì | 5 | 1.49 (0.48, 3.47) |
| Rimini | 2 | 0.77 (0.09, 2.78) |
| Fever (> 37.5 °C for ≥ 48 h) | ||
| All | 35 | 3.82 (2.66, 5.31) |
| Ravenna | 6 | 1.87 (0.69, 4.07) |
| Forlì | 6 | 1.78 (0.65, 3.88) |
| Rimini | 23 | 8.85 (5.61, 13.28) |
| Insomnia, agitation or anxiety | ||
| All | 1 | 0.11 (0.00, 0.61) |
| Ravenna | 0 | 0.00 (0.00, 1.15) |
| Forlì | 1 | 0.30 (0.01, 1.66) |
| Rimini | 0 | 0.00 (0.00, 1.42) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Montalti, M.; Fabbri, M.; Angelini, R.; Bakken, E.; Morri, M.; Tamarri, F.; Reali, C.; Soldà, G.; Silvestrini, G.; Lenzi, J. Syndromic Surveillance in Public Health Emergencies: A Systematic Analysis of Cases Related to Exposure to 2023 Floodwaters in Romagna, Italy. Healthcare 2024, 12, 1760. https://doi.org/10.3390/healthcare12171760
Montalti M, Fabbri M, Angelini R, Bakken E, Morri M, Tamarri F, Reali C, Soldà G, Silvestrini G, Lenzi J. Syndromic Surveillance in Public Health Emergencies: A Systematic Analysis of Cases Related to Exposure to 2023 Floodwaters in Romagna, Italy. Healthcare. 2024; 12(17):1760. https://doi.org/10.3390/healthcare12171760
Chicago/Turabian StyleMontalti, Marco, Marco Fabbri, Raffaella Angelini, Elizabeth Bakken, Michela Morri, Federica Tamarri, Chiara Reali, Giorgia Soldà, Giulia Silvestrini, and Jacopo Lenzi. 2024. "Syndromic Surveillance in Public Health Emergencies: A Systematic Analysis of Cases Related to Exposure to 2023 Floodwaters in Romagna, Italy" Healthcare 12, no. 17: 1760. https://doi.org/10.3390/healthcare12171760
APA StyleMontalti, M., Fabbri, M., Angelini, R., Bakken, E., Morri, M., Tamarri, F., Reali, C., Soldà, G., Silvestrini, G., & Lenzi, J. (2024). Syndromic Surveillance in Public Health Emergencies: A Systematic Analysis of Cases Related to Exposure to 2023 Floodwaters in Romagna, Italy. Healthcare, 12(17), 1760. https://doi.org/10.3390/healthcare12171760








