Impact of Insurance on Readmission Rates, Healthcare Expenditures, and Length of Hospital Stay among Patients with Chronic Ambulatory Care Sensitive Conditions in China
Abstract
1. Introduction
2. Methods
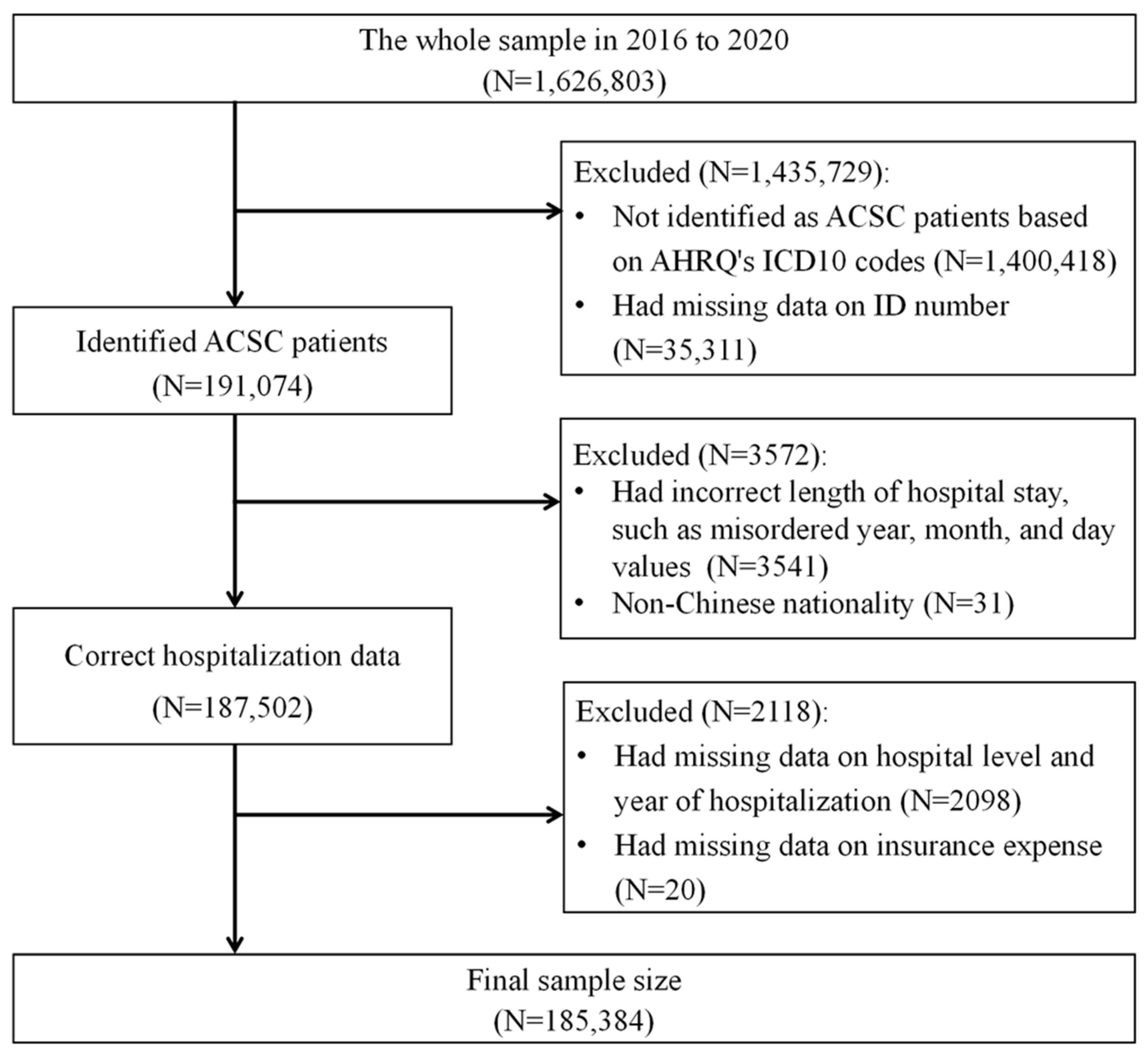
2.1. Data and Study Population
2.2. Variables of Interest
2.3. Statistical Analyses
3. Results
3.1. Sample Characteristics
3.2. Impact of Medical Insurance Type on Readmission Rates, Length of Hospital Stay, and Medical Expenses for Patients with ACSCs
3.3. Stratified Analysis of Health Insurance Type and Readmission Rates, Lengths of Hospital Stay, and Medical Expenses for Patients with Specific ACSCs
3.4. Sensitivity Analyses
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Billings, J.; Zeitel, L.; Lukomnik, J.; Carey, T.S.; Blank, A.E.; Newman, L. Impact of socioeconomic status on hospital use in New York City. Health Aff. 1993, 12, 162–173. [Google Scholar] [CrossRef] [PubMed]
- Purdy, S.; Griffin, T.; Salisbury, C.; Sharp, D. Ambulatory care sensitive conditions: Terminology and disease coding need to be more specific to aid policy makers and clinicians. Public Health 2009, 123, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Laditka, S.B.; Laditka, J.N. Utilization, costs, and access to primary care in fee-for-service and managed care plans. J. Health Soc. Policy 2001, 13, 21–39. [Google Scholar] [CrossRef] [PubMed]
- Davies, S.M.; Geppert, J.; McClellan, M.; McDonald, K.M.; Romano, P.S.; Shojania, K.G. Refinement of the HCUP Quality Indicators; AHRQ Technical Reviews: Rockville, MD, USA, 2001. [Google Scholar]
- Grosios, K.; Gahan, P.B.; Burbidge, J. Overview of healthcare in the UK. EPMA J. 2010, 1, 529–534. [Google Scholar] [CrossRef]
- Mattila, T.; Vasankari, T.; Herse, F.; Leskela, R.L.; Erhola, M.; Avellan-Hietanen, H.; Toppila-Salmi, S.; Haahtela, T. Contrasting healthcare costs of COPD and asthma in elderly. Respir. Med. 2023, 220, 107477. [Google Scholar] [CrossRef]
- Rocha, J.V.M.; Santana, R.; Tello, J.E. Hospitalization for ambulatory care sensitive conditions: What conditions make inter-country comparisons possible? Health Policy Open 2021, 2, 100030. [Google Scholar] [CrossRef]
- Chen, T.; Pan, J. The Effect of Spatial Access to Primary Care on Potentially Avoidable Hospitalizations of the Elderly: Evidence from Chishui City, China. Soc. Indic. Res. 2022, 160, 645–665. [Google Scholar] [CrossRef]
- Chen, S.; Fu, H.; Jian, W. Trends in avoidable hospitalizations in a developed City in eastern China: 2015 to 2018. BMC Health Serv. Res. 2022, 22, 856. [Google Scholar] [CrossRef]
- Lu, S.; Zhang, Y.; Zhang, L.; Klazinga, N.S.; Kringos, D.S. Characterizing Potentially Preventable Hospitalizations of High-Cost Patients in Rural China. Front. Public Health 2022, 10, 804734. [Google Scholar] [CrossRef]
- Wang, J.; Xu, D.R.; Zhang, Y.; Fu, H.; Wang, S.; Ju, K.; Chen, C.; Yang, L.; Jian, W.; Chen, L.; et al. Development of the China’s list of ambulatory care sensitive conditions (ACSCs): A study protocol. Glob. Health Res. Policy 2024, 9, 11. [Google Scholar] [CrossRef]
- Shen, M.; He, W.; Li, L. Incentives to use primary care and their impact on healthcare utilization: Evidence using a public health insurance dataset in China. Soc. Sci. Med. 2020, 255, 112981. [Google Scholar] [CrossRef] [PubMed]
- He, W. Effects of establishing a financing scheme for outpatient care on inpatient services: Empirical evidence from a quasi-experiment in China. Eur. J. Health Econ. 2022, 23, 7–22. [Google Scholar] [CrossRef]
- Liu, G.; Yi, J.; Yuan, Y.; Zhao, S. The short- and long-run effects of medical malpractice lawsuits on medical spending and hospital operations in China. J. Comp. Econ. 2023, 51, 1142–1161. [Google Scholar] [CrossRef]
- Tao, W.; Zeng, Z.; Dang, H.; Lu, B.; Chuong, L.; Yue, D.; Wen, J.; Zhao, R.; Li, W.; Kominski, G.F. Towards universal health coverage: Lessons from 10 years of healthcare reform in China. BMJ Glob. Health 2020, 5, e002086. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Lu, J.; Hu, S.; Cheng, K.K.; De Maeseneer, J.; Meng, Q.; Mossialos, E.; Xu, D.R.; Yip, W.; Zhang, H.; et al. The primary health-care system in China. Lancet 2017, 390, 2584–2594. [Google Scholar] [CrossRef] [PubMed]
- Yip, W.; Fu, H.; Chen, A.T.; Zhai, T.; Jian, W.; Xu, R.; Pan, J.; Hu, M.; Zhou, Z.; Chen, Q.; et al. 10 years of health-care reform in China: Progress and gaps in Universal Health Coverage. Lancet 2019, 394, 1192–1204. [Google Scholar] [CrossRef]
- Fu, W.; Zhao, S.; Zhang, Y.; Chai, P.; Goss, J. Research in health policy making in China: Out-of-pocket payments in Healthy China 2030. BMJ 2018, 360, k234. [Google Scholar] [CrossRef]
- Ricketts, T.C.; Randolph, R.; Howard, H.A.; Pathman, D.; Carey, T. Hospitalization rates as indicators of access to primary care. Health Place 2001, 7, 27–38. [Google Scholar] [CrossRef]
- Hu, T.; Mortensen, K. Mandatory Statewide Medicaid Managed Care in Florida and Hospitalizations for Ambulatory Care Sensitive Conditions. Health Serv. Res. 2018, 53, 293–311. [Google Scholar] [CrossRef]
- Sepehri, A.; Simpson, W.; Sarma, S. The influence of health insurance on hospital admission and length of stay—The case of Vietnam. Soc. Sci. Med. 2006, 63, 1757–1770. [Google Scholar] [CrossRef] [PubMed]
- Fang, H.; Eggleston, K.; Hanson, K.; Wu, M. Enhancing financial protection under China’s social health insurance to achieve universal health coverage. BMJ 2019, 365, l2378. [Google Scholar] [CrossRef] [PubMed]
- Rumalla, K.; Srinivasan, V.M.; Gaddis, M.; Kan, P.; Lawton, M.T.; Burkhardt, J.K. Readmission following extracranial-intracranial bypass surgery in the United States: Nationwide rates, causes, risk factors, and volume-driven outcomes. J. Neurosurg. 2021, 135, 431–439. [Google Scholar] [CrossRef] [PubMed]
- Ramamoorthy, V.; Rubens, M.; Saxena, A.; Bhatt, C.; Das, S.; Appunni, S.; Veledar, E.; McGranaghan, P.; Shehadeh, N.; Viamonte-Ros, A.; et al. Prevalence and Inpatient Hospital Outcomes of Malignancy-Related Ascites in the United States. Am. J. Hosp. Palliat. Care 2021, 38, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Weaver, M.R.; Nandakumar, V.; Joffe, J.; Barber, R.M.; Fullman, N.; Singh, A.; Sparks, G.W.; Yearwood, J.; Lozano, R.; Murray, C.J.L.; et al. Variation in Health Care Access and Quality Among US States and High-Income Countries with Universal Health Insurance Coverage. JAMA Netw. Open 2021, 4, e2114730. [Google Scholar] [CrossRef]
- Johar, M.; Soewondo, P.; Pujisubekti, R.; Satrio, H.K.; Adji, A. Inequality in access to health care, health insurance and the role of supply factors. Soc. Sci. Med. 2018, 213, 134–145. [Google Scholar] [CrossRef]
- Sommers, B.D.; Gawande, A.A.; Baicker, K. Health Insurance Coverage and Health—What the Recent Evidence Tells Us. N. Engl. J. Med. 2017, 377, 586–593. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.C.; Wang, J.; Shi, L.; Wu, C.; Sun, G. Health insurance coverage and access to care in China. BMC Health Serv. Res. 2022, 22, 140. [Google Scholar] [CrossRef]
- World Health Organization: Health Insurance Systems in China: A Briefing Note. 2021. Available online: https://www.who.int/publications/m/item/health-insurance-systems-in-china-a-brie-fing-note (accessed on 12 June 2024).
- Healthcare Security Administration of Foshan City. 2023. Available online: https://m12333.cn/policy/mzafc.html (accessed on 15 August 2024).
- Agency for Healthcare Research and Quality AHRQ. 2019. Available online: www.qualityindicators.ahrq.gov (accessed on 7 April 2024).
- Card, D.; Dobkin, C.; Maestas, N. The Impact of Nearly Universal Insurance Coverage on Health Care Utilization: Evidence from Medicare. Am. Econ. Rev. 2008, 98, 2242–2258. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, C.; Paradise, J. Health insurance and access to health care in the United States. Ann. N. Y. Acad. Sci. 2008, 1136, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Armour, B.S.; Pitts, M.M. Physician Financial Incentives in Managed Care. Dis. Manag. Health Outcomes 2003, 11, 139–147. [Google Scholar] [CrossRef]
- Vogeli, C.; Shields, A.E.; Lee, T.A.; Gibson, T.B.; Marder, W.D.; Weiss, K.B.; Blumenthal, D. Multiple Chronic Conditions: Prevalence, Health Consequences, and Implications for Quality, Care Management, and Costs. J. Gen. Intern. Med. 2007, 22, 391–395. [Google Scholar] [CrossRef]
- Ferro, E.G.; Secemsky, E.A.; Wadhera, R.K.; Choi, E.; Strom, J.B.; Wasfy, J.H.; Wang, Y.; Shen, C.; Yeh, R.W. Patient Readmission Rates For All Insurance Types After Implementation of the Hospital Readmissions Reduction Program. Health Aff. 2019, 38, 585–593. [Google Scholar] [CrossRef]
- Erlangga, D.; Suhrcke, M.; Ali, S.; Bloor, K. The impact of public health insurance on health care utilisation, financial protection and health status in low- and middle-income countries: A systematic review. PLoS ONE 2019, 14, e0219731. [Google Scholar] [CrossRef]
- Johnston, K.J.; Wen, H.; Joynt Maddox, K.E. Lack of Access to Specialists Associated with Mortality and Preventable Hospitalizations of Rural Medicare Beneficiaries. Health Aff. 2019, 38, 1993–2002. [Google Scholar] [CrossRef] [PubMed]
- Doshi, R.P.; Aseltine, R.H.; Sabina, A.B.; Graham, G.N. Racial and Ethnic Disparities in Preventable Hospitalizations for Chronic Disease: Prevalence and Risk Factors. J. Racial Ethn. Health Disparities 2017, 4, 1100–1106. [Google Scholar] [CrossRef] [PubMed]
- Meng, Q.; Fang, H.; Liu, X.; Yuan, B.; Xu, J. Consolidating the social health insurance schemes in China: Towards an equitable and efficient health system. Lancet 2015, 386, 1484–1492. [Google Scholar] [CrossRef]
- Liu, G.G.; Vortherms, S.A.; Hong, X. China’s Health Reform Update. Annu. Rev. Public Health 2017, 38, 431–448. [Google Scholar] [CrossRef] [PubMed]
- Qin, X.; Pan, J.; Liu, G.G. Does participating in health insurance benefit the migrant workers in China? An empirical investigation. China Econ. Rev. 2014, 30, 263–278. [Google Scholar] [CrossRef]
- Li, X.; Tian, L. The effect of non-employment-based health insurance program on firm’s offering of health insurance: Evidence from the social health insurance system in China. J. Comp. Econ. 2020, 48, 997–1010. [Google Scholar] [CrossRef]
- Kotowitz, Y. Moral Hazard. In Allocation, Information and Markets; Eatwell, J., Milgate, M., Newman, P., Eds.; Palgrave Macmillan UK: London, UK, 1989; pp. 207–213. [Google Scholar]
- Li, C.; Tang, C.; Wang, H. Effects of health insurance integration on health care utilization and its equity among the mid-aged and elderly: Evidence from China. Int. J. Equity Health 2019, 18, 166. [Google Scholar] [CrossRef]
- Cunningham, P.J. Why Even Healthy Low to Income People Have Greater Health Risks than Higher to Income People. To the Point (Blog), Commonwealth Fund. 27 September 2018. Available online: https://www.commonwealthfund.org/blog/2018/healthy-low-income-people-greater-health-risks (accessed on 12 June 2024).
- Ali, M.; Folz, R.; Miller, K.; Johnson, B.R., Jr.; Kiarie, J. A study protocol for facility assessment and follow-up evaluations of the barriers to access, availability, utilization and readiness of contraception, abortion and postabortion services in Zika affected areas. Reprod. Health 2017, 14, 18. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Khorasani, E.; Keyvanara, M.; Karimi, S.; Jazi, M.J. Views of health system experts on macro factors of induced demand. Int. J. Prev. Med. 2014, 5, 1286–1298. [Google Scholar] [PubMed]
- Chen, M.; Grabowski, D.C. Hospital Readmissions Reduction Program: Intended and Unintended Effects. Med. Care Res. Rev. 2019, 76, 643–660. [Google Scholar] [CrossRef] [PubMed]
- Nurmagambetov, T.; Kuwahara, R.; Garbe, P. The Economic Burden of Asthma in the United States, 2008–2013. Ann. Am. Thorac. Soc. 2018, 15, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Sinaiko, A.D.; Gaye, M.; Wu, A.C.; Zhang, F.; Xu, X.; Wharam, F.; Wallace, J.; Galbraith, A.A. Variation in out-of-Pocket Spending Among Low-Income Versus High-Income Commercially Insured Patients with Asthma. Health Serv. Res. 2020, 55, 10–11. [Google Scholar] [CrossRef]
- Patel, M.R.; Caldwell, C.H.; Song, P.X.; Wheeler, J.R. Patient perceptions of asthma-related financial burden: Public vs. private health insurance in the United States. Ann. Allergy Asthma Immunol. 2014, 113, 398–403. [Google Scholar] [CrossRef]
- Zeiger, R.S.; Hay, J.W.; Contreras, R.; Chen, W.; Quinn, V.P.; Seal, B.; Schatz, M. Asthma costs and utilization in a managed care organization. J. Allergy Clin. Immunol. 2008, 121, 885–892.e5. [Google Scholar] [CrossRef]
- Divino, V.; Schranz, J.; Early, M.; Shah, H.; Jiang, M.; DeKoven, M. The annual economic burden among patients hospitalized for community-acquired pneumonia (CAP): A retrospective US cohort study. Curr. Med. Res. Opin. 2020, 36, 151–160. [Google Scholar] [CrossRef]
- Rozenbaum, M.H.; Mangen, M.J.; Huijts, S.M.; van der Werf, T.S.; Postma, M.J. Incidence, direct costs and duration of hospitalization of patients hospitalized with community acquired pneumonia: A nationwide retrospective claims database analysis. Vaccine 2015, 33, 3193–3199. [Google Scholar] [CrossRef]
- Heitjan, D.F.; Wang, Y.; Yun, J. Predicting Hospital Readmission in Medicaid Patients with COPD Using Administrative and Claims Data. Respir. Care 2024, 69, 541–548. [Google Scholar] [CrossRef]
- Tao, S.; Li, H.; Xie, Y.; Chen, J.; Feng, Z. Is There a Non-Essential Hospitalization Day in Inpatients with Diabetes under Medical Insurance? Evidence from an Observational Study in China. Diabetes Metab. Syndr. Obes. 2019, 12, 2309–2316. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.; Li, Y.; Yao, Y.; Xiong, Y.; Xiang, L. The impact of an innovative payment method on medical expenditure, efficiency, and quality for inpatients with different types of medical insurance: Evidence from a pilot city, China. Int. J. Equity Health 2024, 23, 115. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Simek, S.; Garg, N.; Vaduganathan, M.; Kaiksow, F.; Stein, J.H.; Fonarow, G.C.; Pandey, A.; Bhatt, D.L. Thirty-Day Readmissions After Hospitalization for Hypertensive Emergency. Hypertension 2019, 73, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Kirkland, E.B.; Heincelman, M.; Bishu, K.G.; Schumann, S.O.; Schreiner, A.; Axon, R.N.; Mauldin, P.D.; Moran, W.P. Trends in Healthcare Expenditures Among US Adults with Hypertension: National Estimates, 2003–2014. J. Am. Heart Assoc. 2018, 7, e008731. [Google Scholar] [CrossRef]
- Zhang, H.; Ning, K.; Wang, J.; Fang, H. Research on the influence of patient cost-sharing on medical expenses and health outcomes: Taking patients with heart failure as an example. Front. Public Health 2023, 11, 1121772. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Chai, K.; Du, M.; Wang, S.; Cai, J.P.; Li, Y.; Zeng, P.; Zhu, W.; Zhan, S.; Yang, J. Prevalence and Incidence of Heart Failure Among Urban Patients in China: A National Population-Based Analysis. Circ. Heart Fail. 2021, 14, e008406. [Google Scholar] [CrossRef] [PubMed]
- Moller, J.K.; Sorensen, M.; Hardahl, C. Prediction of risk of acquiring urinary tract infection during hospital stay based on machine-learning: A retrospective cohort study. PLoS ONE 2021, 16, e0248636. [Google Scholar] [CrossRef]
- Vallejo-Torres, L.; Pujol, M.; Shaw, E.; Wiegand, I.; Vigo, J.M.; Stoddart, M.; Grier, S.; Gibbs, J.; Vank, C.; Cuperus, N.; et al. Cost of hospitalised patients due to complicated urinary tract infections: A retrospective observational study in countries with high prevalence of multidrug-resistant Gram-negative bacteria: The COMBACTE-MAGNET, RESCUING study. BMJ Open 2018, 8, e020251. [Google Scholar] [CrossRef]

| Characteristic | UEBMI (n = 44,415) | URRBMI (n = 80,752) | FMS (n = 111) | Other (n = 31,229) | Self-Pay (n = 28,877) | Total (n = 185,384) | p Value |
|---|---|---|---|---|---|---|---|
| Age; mean (SD) | 62.7 (21.3) | 53.9 (31.5) | 34.4 (33.1) | 51.7 (28.6) | 43.4 (28.6) | 54.0 (29.0) | 0.001 a |
| Age group in years | <0.001 b | ||||||
| ≤14 | 2548 (5.7%) | 19,342 (24.0%) | 52 (46.85%) | 6073 (19.5%) | 7499 (26%) | 35,514 (19.2%) | |
| 15 to 24 | 386 (0.9%) | 591 (0.7%) | 2 (1.8%) | 467 (1.5%) | 761 (2.6%) | 2207 (1.2%) | |
| 25 to 44 | 3976 (9.0%) | 2946 (3.7%) | 12 (10.8%) | 3240 (10.4%) | 3984 (13.8%) | 14,158 (7.6%) | |
| 45 to 64 | 12,055 (27.1%) | 14,267 (17.7%) | 17 (15.3%) | 8112 (26.0%) | 8609 (29.8%) | 43,060 (23.2%) | |
| 65 to 74 | 11,046 (24.9%) | 17,484 (21.7%) | 9 (8.1%) | 5900 (18.9%) | 3838 (13.3%) | 38,277 (20.7%) | |
| ≥75 | 14,404 (32.4%) | 26,122 (32.4%) | 19 (17.1%) | 7437 (23.8%) | 4186 (14.5%) | 52,168 (28.1%) | |
| Year of hospitalization | <0.001 b | ||||||
| 2016 | 8643 (19.5%) | 11,472 (14.2%) | 32 (28.8%) | 8252 (26.4%) | 2778 (9.6%) | 31,177 (16.8%) | |
| 2017 | 9256 (20.8%) | 11,775 (14.6%) | 6 (5.4%) | 7645 (24.5%) | 3482 (12.1%) | 32,164 (17.4%) | |
| 2018 | 10,488 (23.6%) | 17,398 (21.5%) | 10 (9.0%) | 5790 (18.5%) | 7100 (24.6%) | 40,786 (22.0%) | |
| 2019 | 9941 (22.4%) | 22,754 (28.2%) | 40 (36.0%) | 6434 (20.6%) | 11,432 (39.6%) | 50,601 (27.3%) | |
| 2020 | 6087 (13.7%) | 17,353 (21.5%) | 23 (20.7%) | 3108 (10.0%) | 4085 (14.2%) | 30,656 (16.5%) | |
| Sex | <0.001 b | ||||||
| Male | 24,609 (55.4%) | 41,094 (50.9%) | 71 (64.0%) | 16,700 (53.5%) | 15,965 (55.3%) | 98,439 (53.1%) | |
| Female | 19,806 (44.6%) | 39,658 (49.1%) | 40 (36.0%) | 14,529 (46.5%) | 12,912 (44.7%) | 86,945 (46.9%) | |
| Marital status | <0.001 b | ||||||
| Unmarried | 3431 (7.7%) | 21,004 (26.0%) | 55 (49.6%) | 6677 (21.4%) | 8592 (29.8%) | 39,759 (21.5%) | |
| Married | 38,043 (85.7%) | 55,507 (68.7%) | 50 (45.1%) | 22,259 (71.3%) | 18,767 (65%) | 134,626 (72.6%) | |
| Unspecified | 1976 (4.5%) | 1149 (1.4%) | 5 (4.5%) | 1926 (6.2%) | 1016 (3.5%) | 6072 (3.3%) | |
| Widowed/divorced | 965 (2.2%) | 3092 (3.8%) | 1 (0.9%) | 367 (1.2%) | 502 (1.7%) | 4927 (2.7%) | |
| Occupation | <0.001 b | ||||||
| Unemployed | 3181 (7.2%) | 20,948 (25.9%) | 61 (55.0%) | 4240 (13.6%) | 6287 (21.8%) | 34,717 (18.7%) | |
| Employed | 10,830 (24.4%) | 22,845 (28.3%) | 17 (15.3%) | 11,114 (35.6%) | 6641 (23.0%) | 51,447 (27.8%) | |
| Retired | 8878 (20.0%) | 7044 (8.7%) | 6 (5.4%) | 3283 (10.5%) | 883 (3.1%) | 20,094 (10.8%) | |
| Other | 21,526 (48.5%) | 29,915 (37.1%) | 27 (24.3%) | 12,592 (40.3%) | 15,066 (52.2%) | 79,126 (42.7%) | |
| Admission route | <0.001 b | ||||||
| Emergency | 10,161 (22.9%) | 19,220 (23.8%) | 24 (21.6%) | 4294 (13.8%) | 6518 (22.6%) | 40,217 (21.7%) | |
| Outpatient admission | 32,422 (73.0%) | 58,502 (72.5%) | 51 (46.0%) | 20,293 (65%) | 21,459 (74.3%) | 132,727 (71.6%) | |
| Other | 1832 (4.1%) | 3030 (3.8%) | 36 (32.4%) | 6642 (21.3%) | 900 (3.1%) | 12,440 (6.7%) | |
| Hospitalization frequency | <0.001 b | ||||||
| 1 time | 20,450 (46.0%) | 37,728 (46.7%) | 72 (64.9%) | 17,117 (54.8%) | 20,279 (70.2%) | 95,646 (51.6%) | |
| 2–3 times | 12,510 (28.2%) | 23,227 (28.8%) | 19 (17.1%) | 7816 (25.0%) | 5727 (19.8%) | 49,299 (26.6%) | |
| >3 times | 11,455 (25.8%) | 19,797 (24.5%) | 20 (18.0%) | 6296 (20.2%) | 2871 (9.9%) | 40,439 (21.8%) | |
| Hospital level | <0.001 b | ||||||
| Primary | 1665 (3.8%) | 3941 (4.9%) | 2 (1.8%) | 2794 (9.0%) | 1461 (5.1%) | 9863 (5.3%) | |
| Secondary | 25,709 (57.9%) | 56,643 (70.1%) | 64 (57.7%) | 20,742 (66.4%) | 16,879 (58.5%) | 120,037 (64.8%) | |
| Tertiary | 17,041 (38.4%) | 20,168 (25%) | 45 (40.5%) | 7693 (24.6%) | 10,537 (36.5%) | 55,484 (29.9%) | |
| Bed capacity; median (IQR) | 600 (508) | 550 (145) | 500 (125) | 608 (138) | 600 (828) | 586 (117) | 0.001 a |
| CCI; mean (SD) | 4 (2.8) | 3.4 (2.9) | 1.9 (2.9) | 2.8 (2.5) | 2.2 (2.6) | 3.3 (2.8) | 0.001 a |
| Surgical procedure | <0.001 b | ||||||
| None | 34,815 (78.4%) | 63,205 (78.3%) | 74 (66.7%) | 27,679 (88.6%) | 23,697 (82.1%) | 149,470 (80.6%) | |
| Yes | 9600 (21.6%) | 17,547 (21.7%) | 37 (33.3%) | 3550 (11.4%) | 5180 (17.9%) | 35,914 (19.4%) | |
| Readmission rates | <0.001 b | ||||||
| None | 41,128 (92.6%) | 74,360 (92.1%) | 105 (94.6%) | 29,137 (93.3%) | 27,236 (94.3%) | 171,966 (92.8%) | |
| Yes | 3287 (7.4%) | 6392 (7.9%) | 6 (5.4%) | 2092 (6.7%) | 1641 (5.7%) | 13,418 (7.2%) | |
| Length of hospital stay; mean (SD) | 8.32 (6.23) | 8.07 (5.87) | 7.47 (4.38) | 7.81 (5.56) | 6.62 (5.25) | 7.86 (5.8) | 0.001 a |
| Total medical expenses; median (IQR) | 6427.4 (4282.7) | 5357.9 (3990.5) | 4982.9 (3239.8) | 5590.3 (4251.7) | 3614.2 (3689.9) | 5438.1 (4270.2) | 0.001 a |
| Out-of-pocket expenses; median (IQR) | 2364.5 (2446.5) | 2444.6 (3257.6) | 0 (0) | 3296.8 (3089.0) | 3614.2 (3689.9) | 2770.9 (3241.7) | 0.001 a |
| Insurance-covered expenses; median (IQR) | 4710.2 (3497.0) | 3565.4 (3245.9) | 4982.9 (3239.8) | 4075.2 (3207.3) | 0 (0) | 4039.0 (3435.1) | 0.001 a |
| Disease | Medical Insurance | Readmission Rates OR (95% CI) | Length of Hospital Stay IRR (95% CI) | β (95% CI) | ||
|---|---|---|---|---|---|---|
| Total Medical Expenses | Out-of-Pocket Expenses | Insurance-Covered Expenses | ||||
| Asthma (n = 2669) | Self-pay | Ref | Ref | Ref | Ref | NA |
| UEBMI | 0.36 (0.14, 0.95) | 1.01 (0.84, 1.22) * | 0.31 (0.16, 0.45) | −0.42 (−0.78, −0.06) | 0.09 (−0.08, 0.25) * | |
| URRBMI | 0.78 (0.31, 1.97) * | 1.07 (0.81, 1.42) * | 0.27 (0.07, 0.47) | −0.33 (−0.71, 0.04) * | Ref | |
| FMS | / | / | / | NA | / | |
| Other | 1.31 (0.65, 2.63) * | 1.24 (0.96, 1.60) * | 0.40 (0.19, 0.62) | −0.05 (−0.33, 0.23) * | 0.05 (−0.22, 0.32) * | |
| CAP (n = 68,815) | Self-pay | Ref | Ref | Ref | Ref | NA |
| UEBMI | 0.65 (0.50, 0.85) | 1.03 (0.97, 1.08) * | 0.13 (−0.04, 0.30) * | −0.60 (−0.99, −0.21) | 0.01 (−0.10, 0.12) * | |
| URRBMI | 0.63 (0.47, 0.85) | 1.07 (1.02, 1.12) | 0.18 (0.08, 0.29) | −0.44 (−0.76, −0.12) | Ref | |
| FMS | 0.62 (0.10, 3.70) * | 0.96 (0.86, 1.08) * | −0.02 (−0.22, 0.19) * | NA | 0.46 (0.21, 0.72) | |
| Other | 0.63 (0.46, 0.86) | 1.09 (1.02, 1.17) | 0.25 (0.15, 0.35) | −0.19 (−0.44, 0.07) * | −0.04 (−0.15, 0.08) * | |
| COPD (n = 34,579) | Self-pay | Ref | Ref | Ref | Ref | NA |
| UEBMI | 0.47 (0.25, 0.88) | 1.15 (1.03, 1.29) | 0.35 (0.12, 0.59) | −0.54 (−1.06, −0.01) | 0.13 (−0.04, 0.29) * | |
| URRBMI | 0.52 (0.31, 0.87) | 1.20 (1.03, 1.40) | 0.31 (0.05, 0.58) | −0.44 (−0.96, 0.08) * | Ref | |
| FMS | 0.37 (0.11, 1.27) * | 0.91 (0.73, 1.14) * | 0.09 (−0.23, 0.41) * | NA | −0.18 (−0.09, 0.46) * | |
| Other | 0.68 (0.35, 1.32) * | 1.14 (0.99, 1.32) * | 0.38 (0.13, 0.62) | −0.41 (−0.87, 0.05) * | 0.10 (−0.11, 0.31) * | |
| Diabetes (n = 29,961) | Self-pay | Ref | Ref | Ref | Ref | NA |
| UEBMI | 0.93 (0.61, 1.41) * | 1.07 (1.02, 1.11) | 0.32 (0.18, 0.46) | −0.55 (−0.85, −0.25) | 0.15 (0.02, 0.27) | |
| URRBMI | 0.83 (0.59, 1.17) * | 1.03 (0.96, 1.10) * | 0.22 (0.09, 0.35) | −0.52 (−0.8, −0.24) | Ref | |
| FMS | / | 1.03 (0.75, 1.43) * | 0.03 (−0.19, 0.24) * | NA | 0.14 (−0.15, 0.42) * | |
| Other | 0.85 (0.51, 1.40) * | 1.11 (1.01, 1.23) | 0.31 (0.13, 0.50) | −0.29 (−0.55, −0.03) | 0.04 (−0.11, 0.19) * | |
| Hypertension (n = 29,746) | Self-pay | Ref | Ref | Ref | Ref | NA |
| UEBMI | 0.39 (0.19, 0.82) | 1.25 (1.17, 1.33) | 0.54 (0.35, 0.72) | −0.25 (−0.65, 0.15) * | 0.23 (0.03, 0.43) * | |
| URRBMI | 0.40 (0.23, 0.69) | 1.24 (1.13, 1.36) | 0.42 (0.22, 0.62) | −0.23 (−0.65, 0.19) * | Ref | |
| FMS | / | 1.46 (0.86, 2.46) * | 0.30 (0.00, 0.61) | NA | 0.26 (−0.12, 0.64) * | |
| Other | 0.67 (0.34, 1.32) * | 1.29 (1.18, 1.42) | 0.53 (0.28, 0.78) | −0.06 (−0.36, 0.25) * | 0.17 (−0.09, 0.43) * | |
| Heart failure (n = 10,982) | Self-pay | Ref | Ref | Ref | Ref | NA |
| UEBMI | 0.70 (0.51, 0.96) | 1.15 (1.00, 1.32) * | 0.36 (0.05, 0.67) | −0.64 (−1.13, −0.15) | 0.03 (−0.09, 0.15) * | |
| URRBMI | 0.70 (0.53, 0.91) | 1.12 (0.97, 1.30) * | 0.38 (0.06, 0.69) | −0.4 (−0.92, 0.12) * | Ref | |
| FMS | / | 1.05 (0.76, 1.45) * | −0.09 (−0.45, 0.27) * | NA | −0.22 (−0.47, 0.02) * | |
| Other | 0.69 (0.53, 0.89) | 1.16 (1.03, 1.30) | 0.62 (0.28, 0.95) | 0.01 (−0.38, 0.40) * | 0.12 (−0.06, 0.30) * | |
| UTIs (n = 8632) | Self-pay | Ref | Ref | Ref | Ref | NA |
| UEBMI | 0.60 (0.38, 0.96) | 1.04 (1.00, 1.09) * | 0.27 (0.15, 0.39) | −0.44 (−0.76, −0.11) | 0.05 (−0.04, 0.15) * | |
| URRBMI | 0.58 (0.31, 1.10) * | 1.10 (1.05, 1.16) | 0.25 (0.13, 0.36) | −0.34 (−0.64, −0.03) | Ref | |
| FMS | / | 1.38 (1.01, 1.90) | 0.43 (0.16, 0.70) | NA | 0.72 (0.40, 1.05) | |
| Other | 0.56 (0.26, 1.21) * | 1.03 (0.85, 1.25) * | 0.21 (−0.02, 0.44) * | −0.19 (−0.41, 0.03) * | 0.03 (−0.15, 0.22) * | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu Zheng, E.; Zhu, X.; Zhu, Y.; Qin, Z.; Zhang, J.; Huang, Y. Impact of Insurance on Readmission Rates, Healthcare Expenditures, and Length of Hospital Stay among Patients with Chronic Ambulatory Care Sensitive Conditions in China. Healthcare 2024, 12, 1798. https://doi.org/10.3390/healthcare12171798
Xu Zheng E, Zhu X, Zhu Y, Qin Z, Zhang J, Huang Y. Impact of Insurance on Readmission Rates, Healthcare Expenditures, and Length of Hospital Stay among Patients with Chronic Ambulatory Care Sensitive Conditions in China. Healthcare. 2024; 12(17):1798. https://doi.org/10.3390/healthcare12171798
Chicago/Turabian StyleXu Zheng, Esthefany, Xiaodi Zhu, Yi Zhu, Zhenhua Qin, Jiachi Zhang, and Yixiang Huang. 2024. "Impact of Insurance on Readmission Rates, Healthcare Expenditures, and Length of Hospital Stay among Patients with Chronic Ambulatory Care Sensitive Conditions in China" Healthcare 12, no. 17: 1798. https://doi.org/10.3390/healthcare12171798
APA StyleXu Zheng, E., Zhu, X., Zhu, Y., Qin, Z., Zhang, J., & Huang, Y. (2024). Impact of Insurance on Readmission Rates, Healthcare Expenditures, and Length of Hospital Stay among Patients with Chronic Ambulatory Care Sensitive Conditions in China. Healthcare, 12(17), 1798. https://doi.org/10.3390/healthcare12171798





