Race, Ethnicity, and Geography as Determinants of Excessive Weight and Low Physical Activity in Pediatric Population: Protocol for Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Objectives
- Model the age-related dynamics of BMI in the pediatric population of different races/ethnicities and geographies.
- Study race/ethnicity and geographic location as determinants of weight and PA in children and adolescents.
- Look for associations between weight and PA in different races/ethnicities and geographies.
3. Methods and Analysis
3.1. Study Design and Data Source
3.2. Eligibility Criteria
3.3. Study Records
3.4. Data Analysis and Synthesis
3.5. Methodology of Pilot Review
4. Results of Pilot Review
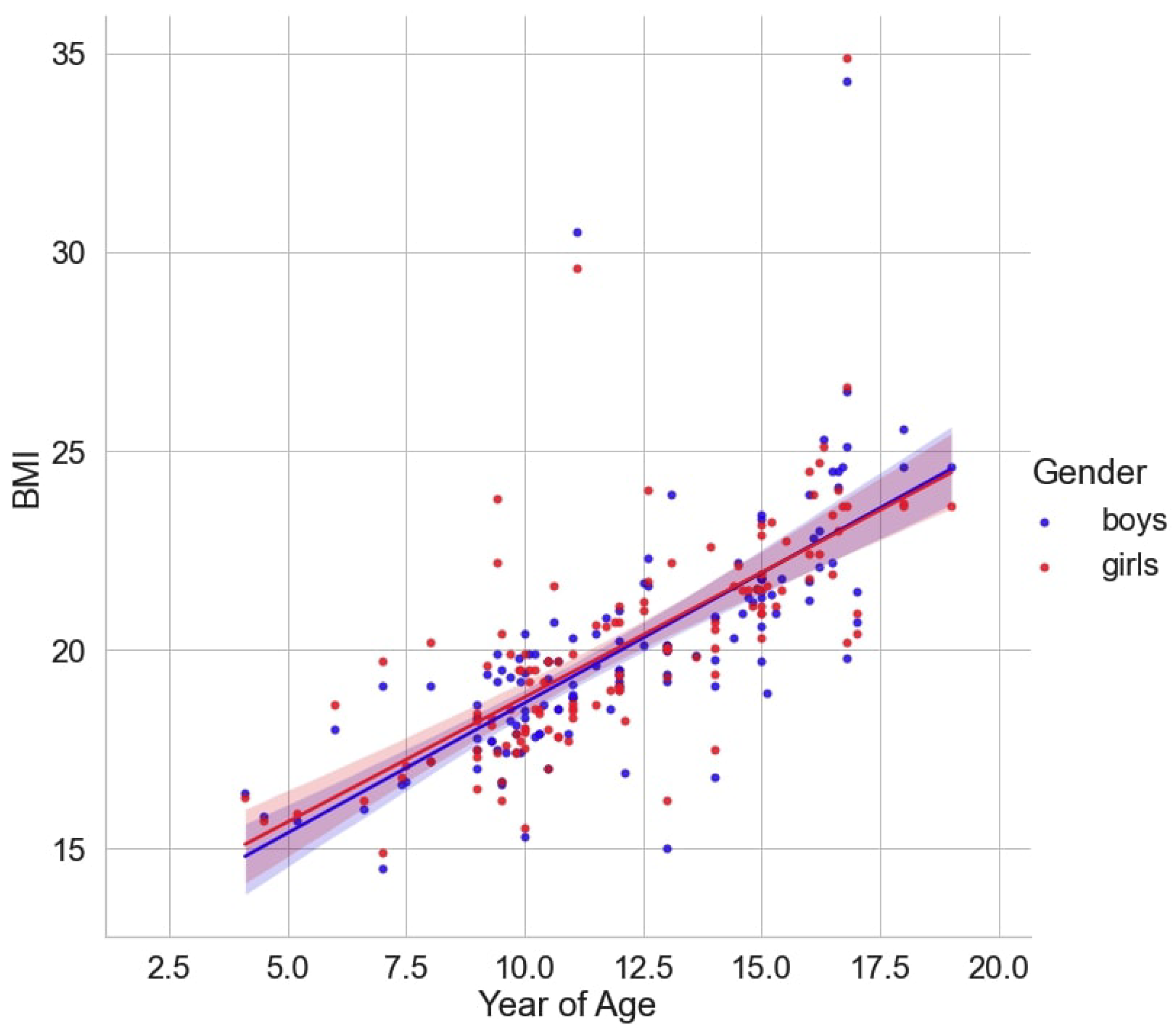
4.1. Age- and Sex-Related Differences in Growth Trajectories of BMI
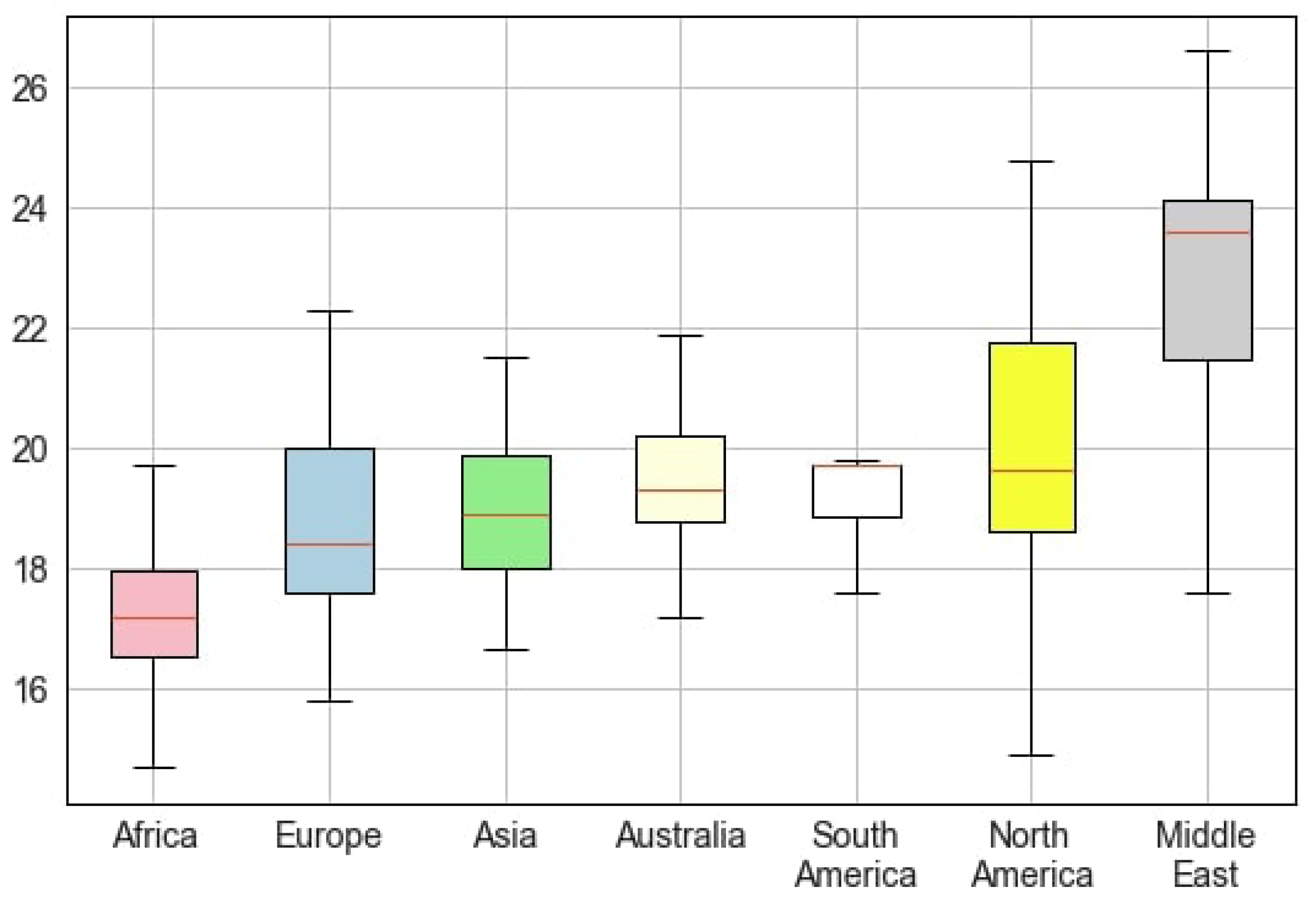
4.2. Regional and Ethnic Disparities in BMI
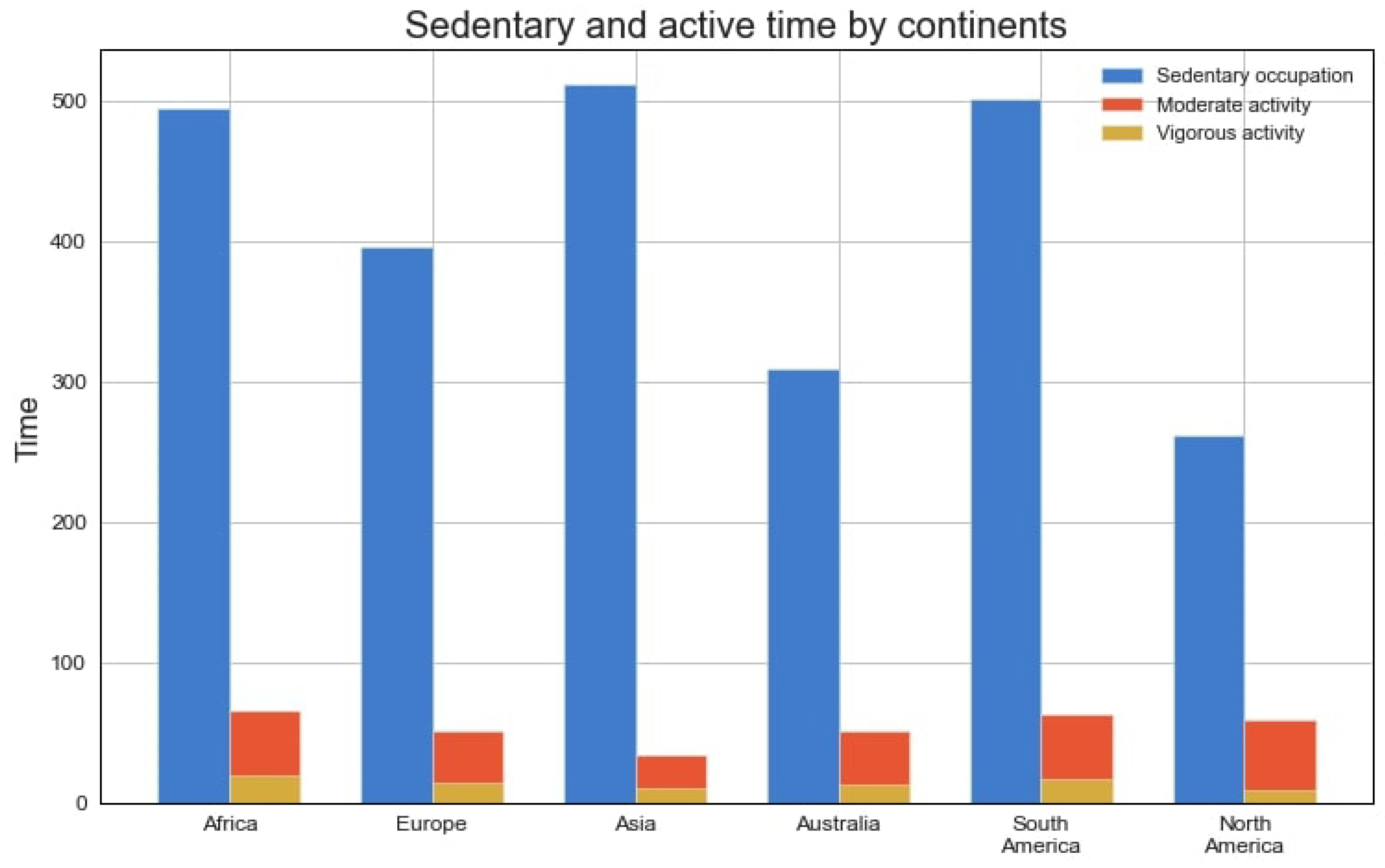
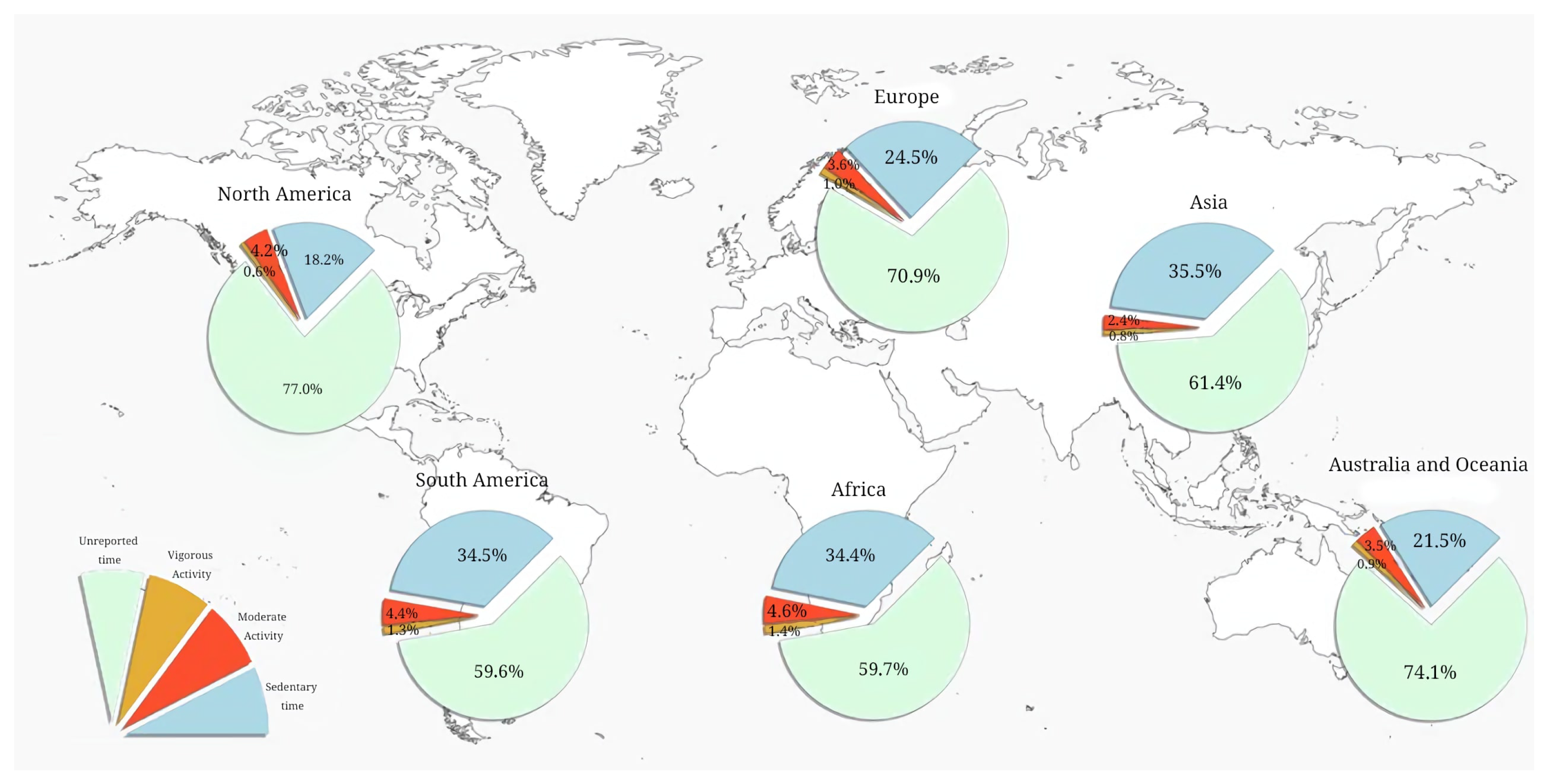
4.3. Physical Activity of Children in Different Regions
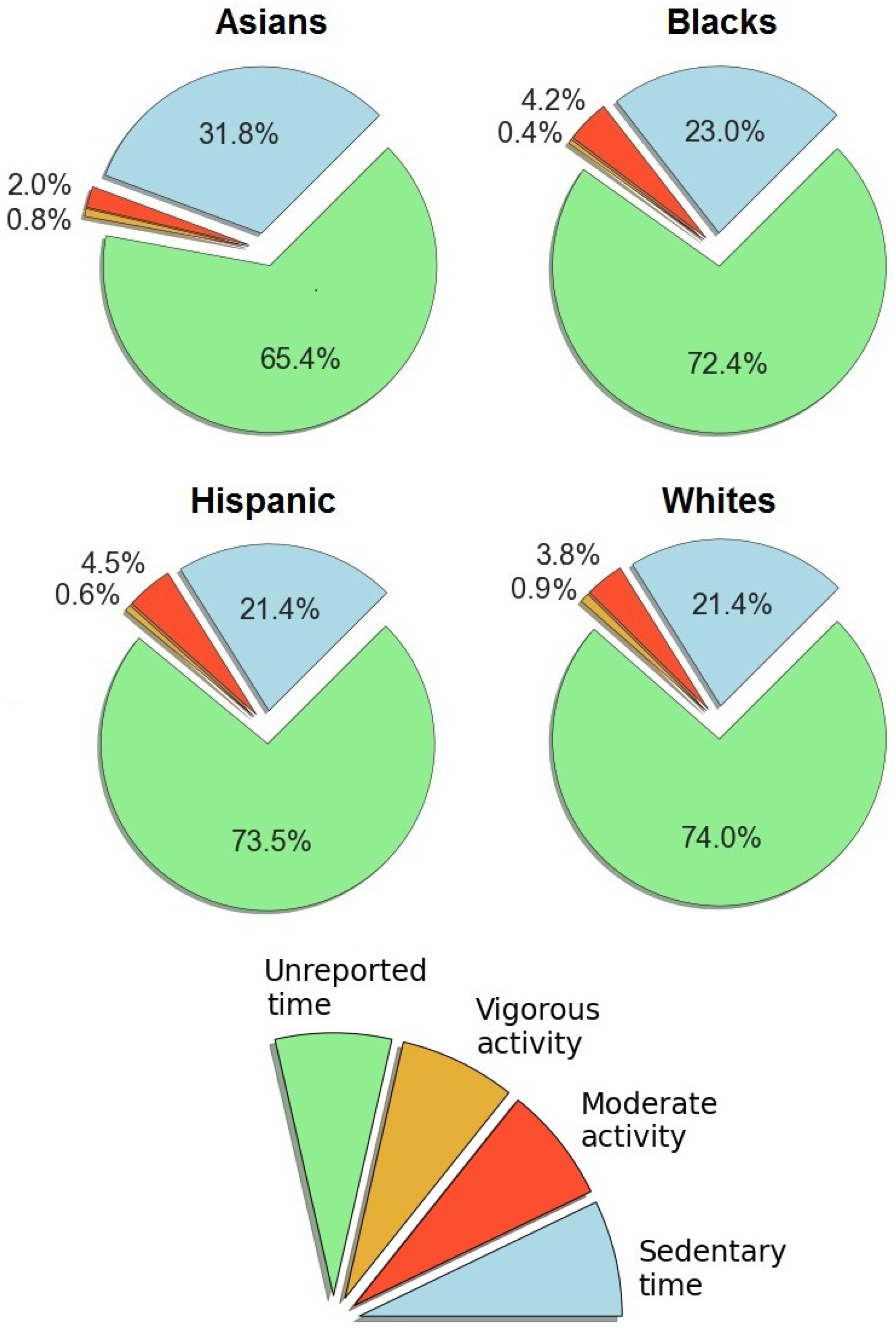
4.4. Racial/Ethnic Differences in Physical Activity
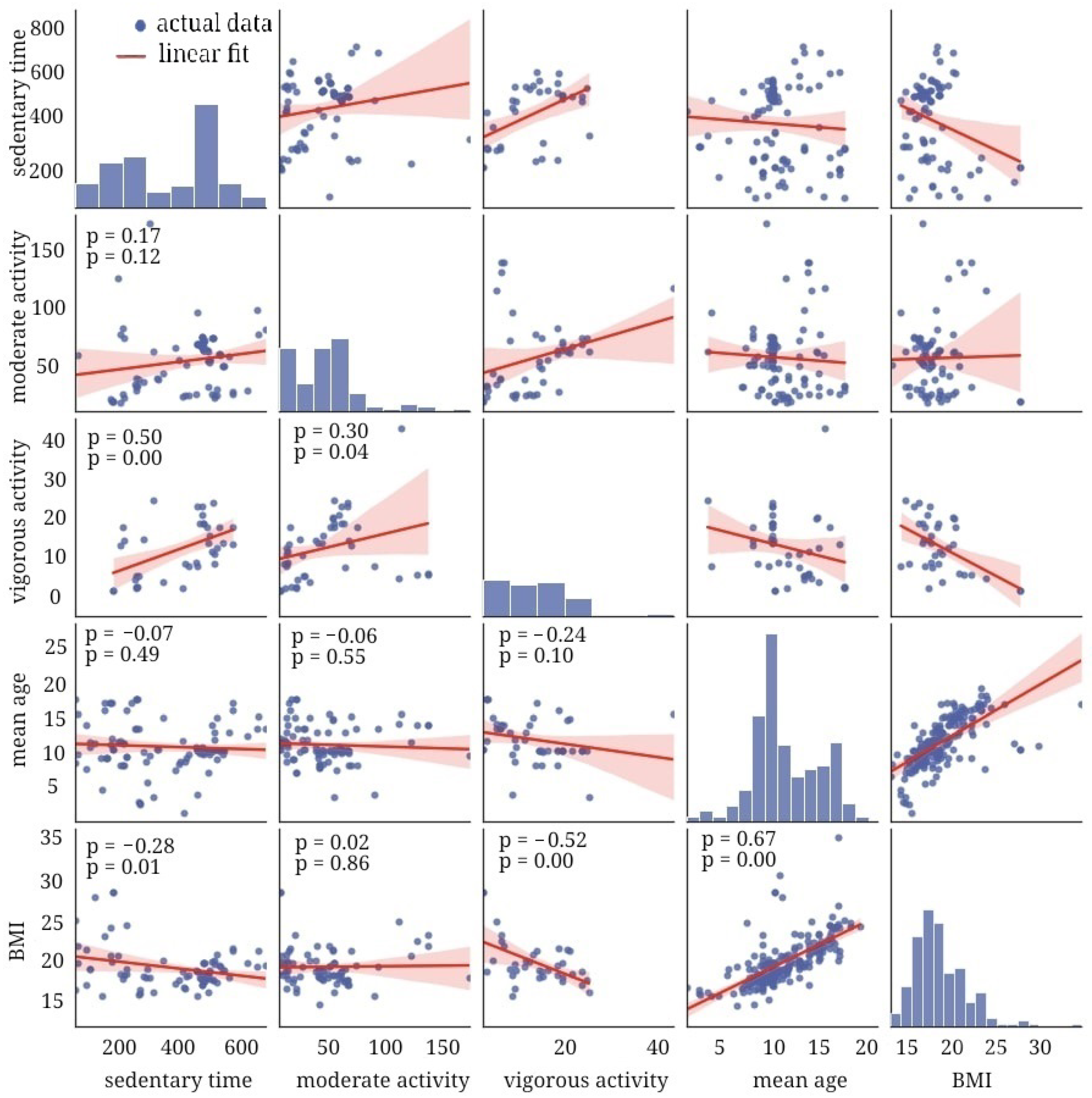
4.5. Association of Sedentary Time and Physical Activity with BMI
5. Discussion
5.1. Age-Related Dynamics of BMI
5.2. Approaches to Study Geographic and Ethnic Disparities in BMI and Physical Activity
5.3. Methods to Examine Level of Physical Activity
5.4. Role of PA in Tackling Obesity
6. Conclusions
- The prevalence of obesity is uneven across geographic regions. The epidemic has reached a plateau in Western countries and shifted to Asia and sub-Saharan Africa. Lifestyle modifications in certain regions may account for the shift in the epidemic landscape. Over 80% of children display sedentary behavior because they treat an active lifestyle as an option rather than a necessity.
- Apart from environmental factors, individual constructs may also influence the impact of PA on weight gain. A personalized approach to disease management necessitates the analysis of endogenous and exogenous risks in combination.
- Recent systematic reviews and meta-analyses have limited generalizability, since they mostly covered a single racial/ethnic group or region/country. Another common limitation is that the studies did not consider race/ethnicity and geography as possible confounders. The proposed meta-analysis will outline trends in PA and BMI of children of different races/ethnicities and geographic regions.
7. Strengths and Limitations
- The PRISMA-P checklist was used to prepare the protocol, and the study methodology was registered with the PROSPERO international database for systematic reviews.
- The research will synthesize data on PA and BMI in the pediatric population in six geographic regions and for four ethnic/racial groups.
- Subgroup analysis will be performed to eliminate the effect of study settings on the pooled analysis.
- The review has been piloted, the results of which indicated evident disparities in PA and BMI across regions and ethnic groups.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BMI | Body mass index |
| MET | Metabolic equivalent of task |
| MPA | Moderate physical activity |
| PA | Physical activity |
| SB | Sedentary behavior |
| VPA | Vigorous physical activity |
| WHO | World Health Organization |
References
- Obesity and Overweight: Key Facts. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 7 March 2024).
- Gao, L.; Peng, W.; Xue, H.; Wu, Y.; Zhou, H.; Jia, P.; Wang, Y. Spatial–temporal trends in global childhood overweight and obesity from 1975 to 2030: A weight mean center and projection analysis of 191 countries. Glob. Health 2023, 19, 53. [Google Scholar] [CrossRef] [PubMed]
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A.; et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128· 9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Martinez, A.; Zhou, B.; Sophiea, M.K.; Bentham, J.; Paciorek, C.J.; Iurilli, M.L.; Carrillo-Larco, R.M.; Bennett, J.E.; Di Cesare, M.; Taddei, C.; et al. Height and body-mass index trajectories of school-aged children and adolescents from 1985 to 2019 in 200 countries and territories: A pooled analysis of 2181 population-based studies with 65 million participants. Lancet 2020, 396, 1511–1524. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Chaput, J.P.; Fogelholm, M.; Hu, G.; Maher, C.; Maia, J.; Olds, T.; Sarmiento, O.L.; Standage, M.; Tremblay, M.S.; et al. International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE): Contributions to understanding the global obesity epidemic. Nutrients 2019, 11, 848. [Google Scholar] [CrossRef]
- Wang, C.; Chen, P.; Zhuang, J. A national survey of physical activity and sedentary behavior of Chinese city children and youth using accelerometers. Res. Q. Exerc. Sport 2013, 84, S12–S28. [Google Scholar] [CrossRef]
- Botey, A.P.; Bayrampour, H.; Carson, V.; Vinturache, A.; Tough, S. Adherence to Canadian physical activity and sedentary behaviour guidelines among children 2 to 13 years of age. Prev. Med. Rep. 2016, 3, 14–20. [Google Scholar] [CrossRef][Green Version]
- Gomes, T.N.; Katzmarzyk, P.T.; Hedeker, D.; Fogelholm, M.; Standage, M.; Onywera, V.; Lambert, E.V.; Tremblay, M.S.; Chaput, J.P.; Tudor-Locke, C.; et al. Correlates of compliance with recommended levels of physical activity in children. Sci. Rep. 2017, 7, 16507. [Google Scholar] [CrossRef]
- A Healthy Lifestyle—WHO Recommendations. Available online: https://www.who.int/europe/news-room/fact-sheets/item/a-healthy-lifestyle—who-recommendations (accessed on 20 March 2024).
- Wong, S.H.S.; Huang, W.Y.; He, G. Longitudinal changes in objectively measured physical activity differ for weekdays and weekends among Chinese children in Hong Kong. BMC Public Health 2015, 15, 1–8. [Google Scholar] [CrossRef]
- Werneck, A.O.; Silva, D.R.; Oyeyemi, A.L.; Fernandes, R.A.; Steene-Johannesen, J.; Andersen, L.B.; Northstone, K.; Sardinha, L.B. Physical activity attenuates metabolic risk of adolescents with overweight or obesity: The ICAD multi-country study. Int. J. Obes. 2020, 44, 823–829. [Google Scholar] [CrossRef]
- Chaput, J.P.; Willumsen, J.; Bull, F.; Chou, R.; Ekelund, U.; Firth, J.; Jago, R.; Ortega, F.B.; Katzmarzyk, P.T. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5–17 years: Summary of the evidence. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 1–9. [Google Scholar] [CrossRef]
- Silva, D.A.S.; Chaput, J.P.; Katzmarzyk, P.T.; Fogelholm, M.; Hu, G.; Maher, C.; Olds, T.; Onywera, V.; Sarmiento, O.L.; Standage, M.; et al. Physical education classes, physical activity, and sedentary behavior in children. Med. Sci. Sport. Exerc. 2018, 50, 995–1004. [Google Scholar] [CrossRef] [PubMed]
- Aubert, S.; Barnes, J.D.; Abdeta, C.; Abi Nader, P.; Adeniyi, A.F.; Aguilar-Farias, N.; Tenesaca, D.S.A.; Bhawra, J.; Brazo-Sayavera, J.; Cardon, G.; et al. Global matrix 3.0 physical activity report card grades for children and youth: Results and analysis from 49 countries. J. Phys. Act. Health 2018, 15, S251–S273. [Google Scholar] [CrossRef] [PubMed]
- Vilar-Compte, M.; Bustamante, A.V.; López-Olmedo, N.; Gaitán-Rossi, P.; Torres, J.; Peterson, K.E.; Teruel, G.; Pérez-Escamilla, R. Migration as a determinant of childhood obesity in the United States and Latin America. Obes. Rev. 2021, 22, e13240. [Google Scholar] [CrossRef] [PubMed]
- Collings, P.J.; Brage, S.; Bingham, D.D.; Costa, S.; West, J.; McEachan, R.R.; Wright, J.; Barber, S.E. Physical activity, sedentary time, and fatness in a biethnic sample of young children. Med. Sci. Sport. Exerc. 2017, 49, 930. [Google Scholar] [CrossRef]
- Gordon-Larsen, P.; McMurray, R.G.; Popkin, B.M. Adolescent physical activity and inactivity vary by ethnicity: The National Longitudinal Study of Adolescent Health. J. Pediatr. 1999, 135, 301–306. [Google Scholar] [CrossRef]
- Belcher, B.R.; Berrigan, D.; Dodd, K.W.; Emken, B.A.; Chou, C.P.; Spuijt-Metz, D. Physical activity in US youth: Impact of race/ethnicity, age, gender, & weight status. Med. Sci. Sport. Exerc. 2010, 42, 2211. [Google Scholar]
- Brown, T.; Smith, S.; Bhopal, R.; Kasim, A.; Summerbell, C. Diet and physical activity interventions to prevent or treat obesity in South Asian children and adults: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2015, 12, 566–594. [Google Scholar] [CrossRef]
- El-Sayed, A.; Scarborough, P.; Galea, S. Ethnic inequalities in obesity among children and adults in the UK: A systematic review of the literature. Obes. Rev. 2011, 12, e516–e534. [Google Scholar] [CrossRef]
- Peirson, L.; Fitzpatrick-Lewis, D.; Morrison, K.; Ciliska, D.; Kenny, M.; Ali, M.U.; Raina, P. Prevention of overweight and obesity in children and youth: A systematic review and meta-analysis. Can. Med Assoc. Open Access J. 2015, 3, E23–E33. [Google Scholar] [CrossRef]
- Kelley, G.A.; Kelley, K.S.; Pate, R.R. Exercise and BMI in overweight and obese children and adolescents: A systematic review and trial sequential meta-analysis. BioMed Res. Int. 2015, 2015. [Google Scholar] [CrossRef]
- Pereira, M.M.C.e.; Padez, C.M.P.; Nogueira, H.G.d.S.M. Describing studies on childhood obesity determinants by Socio-Ecological Model level: A scoping review to identify gaps and provide guidance for future research. Int. J. Obes. 2019, 43, 1883–1890. [Google Scholar] [CrossRef] [PubMed]
- Albuquerque, D.; Nóbrega, C.; Manco, L.; Padez, C. The contribution of genetics and environment to obesity. Br. Med Bull. 2017, 123, 159–173. [Google Scholar] [CrossRef] [PubMed]
- Xia, Q.; Grant, S.F. The genetics of human obesity. Ann. N. Y. Acad. Sci. 2013, 1281, 178–190. [Google Scholar] [CrossRef] [PubMed]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef]
- Finkelstein, E.A.; Ruhm, C.J.; Kosa, K.M. Economic causes and consequences of obesity. Annu. Rev. Public Health 2005, 26, 239–257. [Google Scholar] [CrossRef]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240. [Google Scholar] [CrossRef]
- Harris, K.C.; Kuramoto, L.K.; Schulzer, M.; Retallack, J.E. Effect of school-based physical activity interventions on body mass index in children: A meta-analysis. Cmaj 2009, 180, 719–726. [Google Scholar] [CrossRef]
- Saffer, H.; Dave, D.; Grossman, M.; Ann Leung, L. Racial, ethnic, and gender differences in physical activity. J. Hum. Cap. 2013, 7, 378–410. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Begg, C.B.; Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef]
- Shi, L.; Lin, L. The trim-and-fill method for publication bias: Practical guidelines and recommendations based on a large database of meta-analyses. Medicine 2019, 98, e15987. [Google Scholar] [CrossRef] [PubMed]
- Definition of Regions. Available online: https://population.un.org/wpp/DefinitionOfRegions/#:~:text=Geographic%20regions%3A%20countries%20and%20areas,%3B%20Northern%20America%2C%20and%20Oceania (accessed on 19 March 2024).
- Lewis, C.; Cohen, P.R.; Bahl, D.; Levine, E.M.; Khaliq, W. Race and ethnic categories: A brief review of global terms and nomenclature. Cureus 2023, 15. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Dorugade, A.V. New ridge parameters for ridge regression. J. Assoc. Arab Univ. Basic Appl. Sci. 2014, 15, 94–99. [Google Scholar] [CrossRef]
- Rosenblad, A. Introduction to Meta-Analysis by Michael Borenstein, Larry V. Hedges, Julian PT Higgins, Hannah R. Rothstein. Int. Stat. Rev. 2009, 77, 478–479. [Google Scholar] [CrossRef]
- Long, L. Routine piloting in systematic reviews—a modified approach? Syst. Rev. 2014, 3, 1–5. [Google Scholar] [CrossRef]
- Bernhardsen, G.P.; Stensrud, T.; Nystad, W.; Dalene, K.E.; Kolle, E.; Ekelund, U. Early life risk factors for childhood obesity—Does physical activity modify the associations? The MoBa cohort study. Scand. J. Med. Sci. Sport. 2019, 29, 1636–1646. [Google Scholar] [CrossRef]
- de Moraes Ferrari, G.L.; Oliveira, L.C.; Araujo, T.L.; Matsudo, V.; Barreira, T.V.; Tudor-Locke, C.; Katzmarzyk, P. Moderate-to-vigorous physical activity and sedentary behavior: Independent associations with body composition variables in Brazilian children. Pediatr. Exerc. Sci. 2015, 27, 380–389. [Google Scholar] [CrossRef]
- Gába, A.; Mitáš, J.; Jakubec, L. Associations between accelerometer-measured physical activity and body fatness in school-aged children. Environ. Health Prev. Med. 2017, 22, 1–8. [Google Scholar] [CrossRef]
- Tuan, N.T.; Wang, Y. Adiposity assessments: Agreement between dual-energy X-ray absorptiometry and anthropometric measures in US children. Obesity 2014, 22, 1495–1504. [Google Scholar] [CrossRef]
- Diouf, A.; Thiam, M.; Idohou-Dossou, N.; Diongue, O.; Mégné, N.; Diallo, K.; Sembène, P.M.; Wade, S. Physical activity level and sedentary behaviors among public school children in dakar (senegal) measured by paq-c and accelerometer: Preliminary results. Int. J. Environ. Res. Public Health 2016, 13, 998. [Google Scholar] [CrossRef] [PubMed]
- Anderson, Y.C.; Wynter, L.E.; Grant, C.C.; Stewart, J.M.; Cave, T.L.; Wild, C.E.; Derraik, J.G.; Cutfield, W.S.; Hofman, P.L. Physical activity is low in obese New Zealand children and adolescents. Sci. Rep. 2017, 7, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Dalene, K.E.; Anderssen, S.A.; Andersen, L.B.; Steene-Johannessen, J.; Ekelund, U.; Hansen, B.H.; Kolle, E. Cross-sectional and prospective associations between physical activity, body mass index and waist circumference in children and adolescents. Obes. Sci. Pract. 2017, 3, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Byrd-Williams, C.; Kelly, L.A.; Davis, J.N.; Spruijt-Metz, D.; Goran, M.I. Influence of gender, BMI and Hispanic ethnicity on physical activity in children. Int. J. Pediatr. Obes. 2007, 2, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Steele, R.M.; Van Sluijs, E.M.; Cassidy, A.; Griffin, S.J.; Ekelund, U. Targeting sedentary time or moderate-and vigorous-intensity activity: Independent relations with adiposity in a population-based sample of 10-y-old British children. Am. J. Clin. Nutr. 2009, 90, 1185–1192. [Google Scholar] [CrossRef]
- Drenowatz, C.; Eisenmann, J.C.; Pfeiffer, K.A.; Welk, G.; Heelan, K.; Gentile, D.; Walsh, D. Influence of socio-economic status on habitual physical activity and sedentary behavior in 8-to 11-year old children. BMC Public Health 2010, 10, 1–11. [Google Scholar] [CrossRef]
- Katzmarzyk, P.T.; Barreira, T.V.; Broyles, S.T.; Champagne, C.M.; Chaput, J.P.; Fogelholm, M.; Hu, G.; Johnson, W.D.; Kuriyan, R.; Kurpad, A.; et al. Physical activity, sedentary time, and obesity in an international sample of children. Med. Sci. Sport. Exerc. 2015, 47, 2062–2069. [Google Scholar] [CrossRef]
- Hodgkin, E.; Hamlin, M.J.; Ross, J.; Peters, F. Obesity, energy intake and physical activity in rural and urban New Zealand children. Rural. Remote. Health 2010, 10, 129–137. [Google Scholar] [CrossRef]
- Gordon-Larsen, P.; Adair, L.S.; Popkin, B.M. Ethnic differences in physical activity and inactivity patterns and overweight status. Obes. Res. 2002, 10, 141–149. [Google Scholar] [CrossRef]
- Mitchell, J.; Pate, R.; España-Romero, V.; O’Neill, J.; Dowda, M.; Nader, P. Moderate-To-vigorous physical activity is associated with decreases in body mass index from ages 9 to 15 years. Obesity 2013, 21, E280–E286. [Google Scholar] [CrossRef]
- Labree, W.; Van de Mheen, D.; Rutten, F.; Rodenburg, G.; Koopmans, G.; Foets, M. Differences in overweight and obesity among children from migrant and native origin: The role of physical activity, dietary intake, and sleep duration. PLoS ONE 2015, 10, e0123672. [Google Scholar] [CrossRef] [PubMed]
- McMurray, R.G.; Harrell, J.S.; Deng, S.; Bradley, C.B.; Cox, L.M.; Bangdiwala, S.I. The influence of physical activity, socioeconomic status, and ethnicity on the weight status of adolescents. Obes. Res. 2000, 8, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Laguna, M.; Ruiz, J.R.; Gallardo, C.; García-Pastor, T.; Lara, M.T.; Aznar, S. Obesity and physical activity patterns in children and adolescents. J. Paediatr. Child Health 2013, 49, 942–949. [Google Scholar] [CrossRef]
- Gutin, B.; Yin, Z.; Humphries, M.C.; Barbeau, P. Relations of moderate and vigorous physical activity to fitness and fatness in adolescents. Am. J. Clin. Nutr. 2005, 81, 746–750. [Google Scholar] [CrossRef] [PubMed]
- Moliner-Urdiales, D.; Ruiz, J.; Ortega, F.; Rey-Lopez, J.; Vicente-Rodriguez, G.; Espana-Romero, V.; Munguía-Izquierdo, D.; Castillo, M.; Sjöström, M.; Moreno, L. Association of objectively assessed physical activity with total and central body fat in Spanish adolescents; the HELENA Study. Int. J. Obes. 2009, 33, 1126–1135. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Gomez, D.; Ruiz, J.R.; Ortega, F.B.; Veiga, O.L.; Moliner-Urdiales, D.; Mauro, B.; Galfo, M.; Manios, Y.; Widhalm, K.; Béghin, L.; et al. Recommended levels of physical activity to avoid an excess of body fat in European adolescents: The HELENA Study. Am. J. Prev. Med. 2010, 39, 203–211. [Google Scholar] [CrossRef]
- Silva, P.; Aznar, S.; Aires, L.; Generelo, E.; Zaragoza, J.; Mota, J. Differences in the physical activity pattern between Portuguese and Spanish adolescents. Arch. Exerc. Health Dis. 2010, 1, 26–31. [Google Scholar] [CrossRef]
- Lohman, T.G.; Ring, K.; Pfeiffer, K.; Camhi, S.; Arredondo, E.; Pratt, C.; Pate, R.; Webber, L.S. Relationships among fitness, body composition, and physical activity. Med. Sci. Sport. Exerc. 2008, 40, 1163. [Google Scholar] [CrossRef]
- Van Stralen, M.M.; Yıldırım, M.; Wulp, A.; Te Velde, S.J.; Verloigne, M.; Doessegger, A.; Androutsos, O.; Kovács, É.; Brug, J.; Chinapaw, M.J. Measured sedentary time and physical activity during the school day of European 10-to 12-year-old children: The ENERGY project. J. Sci. Med. Sport 2014, 17, 201–206. [Google Scholar] [CrossRef]
- Dencker, M.; Thorsson, O.; Karlsson, M.K.; Lindén, C.; Svensson, J.; Wollmer, P.; Andersen, L.B. Daily physical activity and its relation to aerobic fitness in children aged 8–11 years. Eur. J. Appl. Physiol. 2006, 96, 587–592. [Google Scholar] [CrossRef]
- Rush, E.C.; Puniani, K.; Valencia, M.; Davies, P.; Plank, L. Estimation of body fatness from body mass index and bioelectrical impedance: Comparison of New Zealand European, Maori and Pacific Island children. Eur. J. Clin. Nutr. 2003, 57, 1394–1401. [Google Scholar] [CrossRef] [PubMed]
- Richardson, A.; North, K.; Graff, M.; Young, K.; Mohlke, K.; Lange, L.; Lange, E.; Harris, K.; Gordon-Larsen, P. Moderate to vigorous physical activity interactions with genetic variants and body mass index in a large US ethnically diverse cohort. Pediatr. Obes. 2014, 9, e35–e46. [Google Scholar] [CrossRef] [PubMed]
- Al-Hazzaa, H.M.; Abahussain, N.A.; Al-Sobayel, H.I.; Qahwaji, D.M.; Musaiger, A.O. Lifestyle factors associated with overweight and obesity among Saudi adolescents. BMC Public Health 2012, 12, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Collison, K.S.; Zaidi, M.Z.; Subhani, S.N.; Al-Rubeaan, K.; Shoukri, M.; Al-Mohanna, F.A. Sugar-sweetened carbonated beverage consumption correlates with BMI, waist circumference, and poor dietary choices in school children. BMC Public Health 2010, 10, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Schneider, M.; Dunton, G.F.; Cooper, D.M. Media use and obesity in adolescent females. Obesity 2007, 15, 2328–2335. [Google Scholar] [CrossRef]
- Hanson, M.D.; Chen, E. Socioeconomic status, race, and body mass index: The mediating role of physical activity and sedentary behaviors during adolescence. J. Pediatr. Psychol. 2007, 32, 250–259. [Google Scholar] [CrossRef]
- Merrigan, J.J.; Volgenau, K.M.; McKay, A.; Mehlenbeck, R.; Jones, M.T.; Gallo, S. Bidirectional Associations between Physical Activity and Sleep in Early-Elementary-Age Latino Children with Obesity. Sports 2021, 9, 26. [Google Scholar] [CrossRef]
- Klein-Platat, C.; Oujaa, M.; Wagner, A.; Haan, M.; Arveiler, D.; Schlienger, J.; Simon, C. Physical activity is inversely related to waist circumference in 12-y-old French adolescents. Int. J. Obes. 2005, 29, 9–14. [Google Scholar] [CrossRef]
- Micklesfield, L.K.; Pedro, T.M.; Kahn, K.; Kinsman, J.; Pettifor, J.M.; Tollman, S.; Norris, S.A. Physical activity and sedentary behavior among adolescents in rural South Africa: Levels, patterns and correlates. BMC Public Health 2014, 14, 1–10. [Google Scholar] [CrossRef]
- Al-Hazzaa, H.M.; Al-Sobayel, H.I.; Musaiger, A.O. Convergent validity of the Arab Teens Lifestyle Study (ATLS) physical activity questionnaire. Int. J. Environ. Res. Public Health 2011, 8, 3810–3820. [Google Scholar] [CrossRef]
- Tayyem, R.; Al Hazzaa, H.; Abu Mweis, S.; Bawadi, H.; Hammad, S.; Musaiger, A. Dietary Habits and Physical Activity Levels in Jordanian Adolescents Attending Private versus Public Schools. 2014. Available online: http://applications.emro.who.int/emhj/v20/07/EMHJ_2014_20_7_416_423.pdf (accessed on 19 March 2024).
- Wang, J.J.; Baranowski, T.; Lau, W.P.; Chen, T.A.; Pitkethly, A.J. Validation of the physical activity questionnaire for older children (PAQ-C) among Chinese children. Biomed. Environ. Sci. 2016, 29, 177–186. [Google Scholar] [PubMed]
- Duncan, M.J.; Al-hazzaa, H.M.; Al-Nakeeb, Y.; Al-Sobayel, H.I.; Abahussain, N.A.; Musaiger, A.O.; Lyons, M.; Collins, P.; Nevill, A. Anthropometric and lifestyle characteristics of active and inactive Saudi and British adolescents. Am. J. Hum. Biol. 2014, 26, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Al-Hazzaa, H.M.; Abahussain, N.A.; Al-Sobayel, H.I.; Qahwaji, D.M.; Musaiger, A.O. Physical activity, sedentary behaviors and dietary habits among Saudi adolescents relative to age, gender and region. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Allafi, A.; Al-Haifi, A.R.; Al-Fayez, M.A.; Al-Athari, B.I.; Al-Ajmi, F.A.; Al-Hazzaa, H.M.; Musaiger, A.O.; Ahmed, F. Physical activity, sedentary behaviours and dietary habits among Kuwaiti adolescents: Gender differences. Public Health Nutr. 2014, 17, 2045–2052. [Google Scholar] [CrossRef]
- Lee, J.E.; Stodden, D.F.; Gao, Z. Young children’s energy expenditure and moderate-to-vigorous physical activity on weekdays and weekends. J. Phys. Act. Health 2016, 13, 1013–1016. [Google Scholar] [CrossRef]
- Larouche, R.; Mire, E.F.; Belanger, K.; Barreira, T.V.; Chaput, J.P.; Fogelholm, M.; Hu, G.; Lambert, E.V.; Maher, C.; Maia, J.; et al. Relationships between outdoor time, physical activity, sedentary time, and body mass index in children: A 12-country study. Pediatr. Exerc. Sci. 2019, 31, 118–129. [Google Scholar] [CrossRef]
- Naseri, P.; Amiri, P.; Momenyan, S.; Zayeri, F.; Karimi, M.; Azizi, F. Longitudinal association between body mass index and physical activity among adolescents with different parental risk: A parallel latent growth curve modeling approach. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 1–13. [Google Scholar] [CrossRef]
- Farooq, A.; Basterfield, L.; Adamson, A.J.; Pearce, M.S.; Hughes, A.R.; Janssen, X.; Wilson, M.G.; Reilly, J.J. Moderate-to-vigorous intensity physical activity and sedentary behaviour across childhood and adolescence, and their combined relationship with obesity risk: A multi-trajectory analysis. Int. J. Environ. Res. Public Health 2021, 18, 7421. [Google Scholar] [CrossRef]
- Pate, R.R.; Schenkelberg, M.A.; Dowda, M.; McIver, K.L. Group-based physical activity trajectories in children transitioning from elementary to high school. BMC Public Health 2019, 19, 1–7. [Google Scholar] [CrossRef]
- Farooq, M.A.; Parkinson, K.N.; Adamson, A.J.; Pearce, M.S.; Reilly, J.K.; Hughes, A.R.; Janssen, X.; Basterfield, L.; Reilly, J.J. Timing of the decline in physical activity in childhood and adolescence: Gateshead Millennium Cohort Study. Br. J. Sport. Med. 2018, 52, 1002–1006. [Google Scholar] [CrossRef]
- Aparicio-Ugarriza, R.; Mielgo-Ayuso, J.; Ruiz, E.; Ávila, J.M.; Aranceta-Bartrina, J.; Gil, Á.; Ortega, R.M.; Serra-Majem, L.; Varela-Moreiras, G.; González-Gross, M. Active commuting, physical activity, and sedentary behaviors in children and adolescents from Spain: Findings from the ANIBES Study. Int. J. Environ. Res. Public Health 2020, 17, 668. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Zhao, P.; Diao, C.; Qiao, Y.; Katzmarzyk, P.T.; Chaput, J.P.; Fogelholm, M.; Kuriyan, R.; Kurpad, A.; Lambert, E.V.; et al. Joint associations between weekday and weekend physical activity or sedentary time and childhood obesity. Int. J. Obes. 2019, 43, 691–700. [Google Scholar] [CrossRef] [PubMed]
- Fairclough, S.J.; Ridgers, N.D.; Welk, G. Correlates of children’s moderate and vigorous physical activity during weekdays and weekends. J. Phys. Act. Health 2012, 9, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Machado-Rodrigues, A.M.; e Silva, M.J.C.; Mota, J.; Santos, R.M.; Cumming, S.P.; Malina, R.M. Physical activity and energy expenditure in adolescent male sport participants and nonparticipants aged 13 to 16 years. J. Phys. Act. Health 2012, 9, 626–633. [Google Scholar] [CrossRef] [PubMed]
- Basterfield, L.; Reilly, J.K.; Pearce, M.S.; Parkinson, K.N.; Adamson, A.J.; Reilly, J.J.; Vella, S.A. Longitudinal associations between sports participation, body composition and physical activity from childhood to adolescence. J. Sci. Med. Sport 2015, 18, 178–182. [Google Scholar] [CrossRef]
- Ferrari, G.L.d.M.; Araújo, T.L.; Oliveira, L.C.; Matsudo, V.; Fisberg, M. Association between electronic equipment in the bedroom and sedentary lifestyle, physical activity, and body mass index of children. J. De Pediatr. 2015, 91, 574–582. [Google Scholar] [CrossRef]
- Steele, R.M.; van Sluijs, E.M.; Sharp, S.J.; Landsbaugh, J.R.; Ekelund, U.; Griffin, S.J. An investigation of patterns of children’s sedentary and vigorous physical activity throughout the week. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 1–8. [Google Scholar] [CrossRef]
- Mitchell, J.; Pate, R.; Beets, M.; Nader, P. Time spent in sedentary behavior and changes in childhood BMI: A longitudinal study from ages 9 to 15 years. Int. J. Obes. 2013, 37, 54–60. [Google Scholar] [CrossRef]
- Goldfield, G.S.; Mallory, R.; Parker, T.; Cunningham, T.; Legg, C.; Lumb, A.; Parker, K.; Prud’homme, D.; Adamo, K.B. Effects of modifying physical activity and sedentary behavior on psychosocial adjustment in overweight/obese children. J. Pediatr. Psychol. 2007, 32, 783–793. [Google Scholar] [CrossRef]
- Saunders, T.J.; Tremblay, M.S.; Mathieu, M.È.; Henderson, M.; O’Loughlin, J.; Tremblay, A.; Chaput, J.P.; Group, Q.C.R. Associations of sedentary behavior, sedentary bouts and breaks in sedentary time with cardiometabolic risk in children with a family history of obesity. PLoS ONE 2013, 8, e79143. [Google Scholar] [CrossRef]
- Gaya, A.R.; Alves, A.; Aires, L.; Martins, C.L.; Ribeiro, J.C.; Mota, J. Association between time spent in sedentary, moderate to vigorous physical activity, body mass index, cardiorespiratory fitness and blood pressure. Ann. Hum. Biol. 2009, 36, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Ochoa, M.C.; Moreno-Aliaga, M.J.; Martínez-González, M.A.; Martínez, J.A.; Marti, A.; Members, G. Predictor factors for childhood obesity in a Spanish case-control study. Nutrition 2007, 23, 379–384. [Google Scholar] [CrossRef] [PubMed]
- Treuth, M.S.; Baggett, C.D.; Pratt, C.A.; Going, S.B.; Elder, J.P.; Charneco, E.Y.; Webber, L.S. A longitudinal study of sedentary behavior and overweight in adolescent girls. Obesity 2009, 17, 1003–1008. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, J.A.D.; da Costa, T.H.M. Gender differences in physical activity, sedentary behavior, and their relation to body composition in active Brazilian adolescents. J. Phys. Act. Health 2009, 6, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Sardinha, L.B.; Andersen, L.B.; Anderssen, S.A.; QUITerio, A.L.; Ornelas, R.; Froberg, K.; Riddoch, C.J.; Ekelund, U. Objectively measured time spent sedentary is associated with insulin resistance independent of overall and central body fat in 9-to 10-year-old Portuguese children. Diabetes Care 2008, 31, 569–575. [Google Scholar] [CrossRef]
- Epstein, L.H.; Roemmich, J.N.; Robinson, J.L.; Paluch, R.A.; Winiewicz, D.D.; Fuerch, J.H.; Robinson, T.N. A randomized trial of the effects of reducing television viewing and computer use on body mass index in young children. Arch. Pediatr. Adolesc. Med. 2008, 162, 239–245. [Google Scholar] [CrossRef]
- Gortmaker, S.L.; Peterson, K.; Wiecha, J.; Sobol, A.M.; Dixit, S.; Fox, M.K.; Laird, N. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch. Pediatr. Adolesc. Med. 1999, 153, 409–418. [Google Scholar] [CrossRef]
- Burke, V.; Beilin, L.J.; Durkin, K.; Stritzke, W.G.; Houghton, S.; Cameron, C.A. Television, computer use, physical activity, diet and fatness in Australian adolescents. Int. J. Pediatr. Obes. 2006, 1, 248–255. [Google Scholar] [CrossRef]
- Berkey, C.S.; Rockett, H.R.; Gillman, M.W.; Colditz, G.A. One-year changes in activity and in inactivity among 10-to 15-year-old boys and girls: Relationship to change in body mass index. Pediatrics 2003, 111, 836–843. [Google Scholar] [CrossRef]
- Fulton, J.E.; Dai, S.; Steffen, L.M.; Grunbaum, J.A.; Shah, S.M.; Labarthe, D.R. Physical activity, energy intake, sedentary behavior, and adiposity in youth. Am. J. Prev. Med. 2009, 37, S40–S49. [Google Scholar] [CrossRef]
- Berkey, C.S.; Rockett, H.R.; Field, A.E.; Gillman, M.W.; Frazier, A.L.; Camargo, C.A.; Md, J.R.; Colditz, G.A. Activity, dietary intake, and weight changes in a longitudinal study of preadolescent and adolescent boys and girls. Pediatrics 2000, 105, e56. [Google Scholar] [CrossRef] [PubMed]
- Steffen, L.M.; Dai, S.; Fulton, J.E.; Labarthe, D.R. Overweight in children and adolescents associated with TV viewing and parental weight: Project HeartBeat! Am. J. Prev. Med. 2009, 37, S50–S55. [Google Scholar] [CrossRef] [PubMed]
- Pratt, C.; Webber, L.S.; Baggett, C.D.; Ward, D.; Pate, R.R.; Murray, D.; Lohman, T.; Lytle, L.; Elder, J.P. Sedentary activity and body composition of middle school girls: The trial of activity for adolescent girls. Res. Q. Exerc. Sport 2008, 79, 458–467. [Google Scholar] [CrossRef] [PubMed]
- Laurson, K.R.; Eisenmann, J.C.; Welk, G.J.; Wickel, E.E.; Gentile, D.A.; Walsh, D.A. Combined influence of physical activity and screen time recommendations on childhood overweight. J. Pediatr. 2008, 153, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Butte, N.F.; Puyau, M.R.; Adolph, A.L.; Vohra, F.A.; Zakeri, I. Physical activity in nonoverweight and overweight Hispanic children and adolescents. Med. Sci. Sport. Exerc. 2007, 39, 1257–1266. [Google Scholar] [CrossRef]
- Ortega, F.B.; Tresaco, B.; Ruiz, J.R.; Moreno, L.A.; Martin-Matillas, M.; Mesa, J.L.; Warnberg, J.; Bueno, M.; Tercedor, P.; Gutiérrez, A.; et al. Cardiorespiratory fitness and sedentary activities are associated with adiposity in adolescents. Obesity 2007, 15, 1589–1599. [Google Scholar] [CrossRef]
- Obarzanek, E.; Schreiber, G.B.; Crawford, P.B.; Goldman, S.R.; Barrier, P.M.; Frederick, M.M.; Lakatos, E. Energy intake and physical activity in relation to indexes of body fat: The National Heart, Lung, and Blood Institute Growth and Health Study. Am. J. Clin. Nutr. 1994, 60, 15–22. [Google Scholar] [CrossRef]
- Katzmarzyk, P.T.; Malina, R.M.; Song, T.M.; Bouchard, C. Television viewing, physical activity, and health-related fitness of youth in the Quebec Family Study. J. Adolesc. Health 1998, 23, 318–325. [Google Scholar] [CrossRef]
- Goldfield, G.S.; Mallory, R.; Parker, T.; Cunningham, T.; Legg, C.; Lumb, A.; Parker, K.; Prud’homme, D.; Gaboury, I.; Adamo, K.B. Effects of open-loop feedback on physical activity and television viewing in overweight and obese children: A randomized, controlled trial. Pediatrics 2006, 118, e157–e166. [Google Scholar] [CrossRef]
- Oliveira, L.C.; Ferrari, G.L.d.M.; Araújo, T.L.; Matsudo, V. Overweight, obesity, steps, and moderate to vigorous physical activity in children. Rev. De Saude Publica 2017, 51. [Google Scholar] [CrossRef]
- Johansson, E.; Hagströmer, M.; Svensson, V.; Ek, A.; Forssén, M.; Nero, H.; Marcus, C. Objectively measured physical activity in two-year-old children–levels, patterns and correlates. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Riddoch, C.J.; Mattocks, C.; Deere, K.; Saunders, J.; Kirkby, J.; Tilling, K.; Leary, S.D.; Blair, S.N.; Ness, A.R. Objective measurement of levels and patterns of physical activity. Arch. Dis. Child. 2007, 92, 963–969. [Google Scholar] [CrossRef] [PubMed]
- Tambalis, K.D.; Panagiotakos, D.B.; Psarra, G.; Sidossis, L.S. Concomitant associations between lifestyle characteristics and physical activity status in children and adolescents. J. Res. Health Sci. 2019, 19, e00439. [Google Scholar] [PubMed]
- van Sluijs, s.M.; Jones, N.R.; Jones, A.P.; Sharp, S.J.; Harrison, F.; Griffin, S.J. School-level correlates of physical activity intensity in 10-year-old children. Int. J. Pediatr. Obes. 2011, 6, e574–e581. [Google Scholar] [CrossRef] [PubMed]
- Henderson, M.; Gray-Donald, K.; Mathieu, M.E.; Barnett, T.A.; Hanley, J.A.; O’Loughlin, J.; Tremblay, A.; Lambert, M. How are physical activity, fitness, and sedentary behavior associated with insulin sensitivity in children? Diabetes Care 2012, 35, 1272–1278. [Google Scholar] [CrossRef]
- Al-Hazzaa, H.M.; Al-Rasheedi, A.A. Adiposity and physical activity levels among preschool children in Jeddah, Saudi Arabia. Saudi Med J. 2007, 28, 766. [Google Scholar]
- Leppänen, M.; Nyström, C.D.; Henriksson, P.; Pomeroy, J.; Ruiz, J.; Ortega, F.; Cadenas-Sánchez, C.; Löf, M. Physical activity intensity, sedentary behavior, body composition and physical fitness in 4-year-old children: Results from the ministop trial. Int. J. Obes. 2016, 40, 1126–1133. [Google Scholar] [CrossRef]
- Collings, P.J.; Wijndaele, K.; Corder, K.; Westgate, K.; Ridgway, C.L.; Dunn, V.; Goodyer, I.; Ekelund, U.; Brage, S. Levels and patterns of objectively-measured physical activity volume and intensity distribution in UK adolescents: The ROOTS study. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 1–12. [Google Scholar] [CrossRef]
- Ojiambo, R.M.; Easton, C.; Casajús, J.A.; Konstabel, K.; Reilly, J.J.; Pitsiladis, Y. Effect of urbanization on objectively measured physical activity levels, sedentary time, and indices of adiposity in Kenyan adolescents. J. Phys. Act. Health 2012, 9, 115–123. [Google Scholar] [CrossRef]
- Prista, A.; Nhantumbo, L.; Saranga, S.; Lopes, V.; Maia, J.; e Seabra, A.; Vinagre, J.; Conn, C.A.; Beunen, G. Physical activity assessed by accelerometry in rural African school-age children and adolescents. Pediatr. Exerc. Sci. 2009, 21, 384–399. [Google Scholar] [CrossRef]
- Ni Mhurchu, C.; Maddison, R.; Jiang, Y.; Jull, A.; Prapavessis, H.; Rodgers, A. Couch potatoes to jumping beans: A pilot study of the effect of active video games on physical activity in children. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.W.; Farmer, V.L.; Cameron, S.L.; Meredith-Jones, K.; Williams, S.M.; Mann, J.I. School playgrounds and physical activity policies as predictors of school and home time activity. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Hume, C.; Okely, A.; Bagley, S.; Telford, A.; Booth, M.; Crawford, D.; Salmon, J. Does weight status influence associations between children’s fundamental movement skills and physical activity? Res. Q. Exerc. Sport 2008, 79, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Maddison, R.; Foley, L.S.; Olds, T.S.; Ridley, K.; Jiang, Y. Validating the multimedia activity recall for children and adolescents in a large New Zealand sample. J. Sport. Sci. 2014, 32, 470–478. [Google Scholar] [CrossRef] [PubMed]
- Fraysse, F.; Grobler, A.C.; Muller, J.; Wake, M.; Olds, T. Physical activity and sedentary activity: Population epidemiology and concordance in Australian children aged 11–12 years and their parents. BMJ Open 2019, 9, 136–146. [Google Scholar] [CrossRef]
- Janz, K.F.; Boros, P.; Letuchy, E.M.; Kwon, S.; Burns, T.L.; Levy, S.M. Physical activity, not sedentary time, predicts DXA-measured adiposity age 5–19 years. Med. Sci. Sport. Exerc. 2017, 49, 2071. [Google Scholar] [CrossRef]
- Basterfield, L.; Adamson, A.J.; Frary, J.K.; Parkinson, K.N.; Pearce, M.S.; Reilly, J.J.; Team, G.M.S.C. Longitudinal study of physical activity and sedentary behavior in children. Pediatrics 2011, 127, e24–e30. [Google Scholar] [CrossRef]
- Haslwanter, T. An introduction to statistics with python. In With Applications in the Life Sciences; Springer International Publishing: Cham, Switzerland, 2016. [Google Scholar]
- Bac, A.; Woźniacka, R.; Matusik, S.; Golec, J.; Golec, E. Prevalence of overweight and obesity in children aged 6–13 years—alarming increase in obesity in Cracow, Poland. Eur. J. Pediatr. 2012, 171, 245–251. [Google Scholar] [CrossRef]
- Vishnu, A.; Belbin, G.M.; Wojcik, G.L.; Bottinger, E.P.; Gignoux, C.R.; Kenny, E.E.; Loos, R.J. The role of country of birth, and genetic and self-identified ancestry, in obesity susceptibility among African and Hispanic Americans. Am. J. Clin. Nutr. 2019, 110, 16–23. [Google Scholar] [CrossRef]
- Young, K.L.; Graff, M.; Fernandez-Rhodes, L.; North, K.E. Genetics of obesity in diverse populations. Curr. Diabetes Rep. 2018, 18, 1–10. [Google Scholar] [CrossRef]
- Lebel, A.; Kestens, Y.; Clary, C.; Bisset, S.; Subramanian, S. Geographic variability in the association between socioeconomic status and BMI in the USA and Canada. PLoS ONE 2014, 9, e99158. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Physical Status: The Use of and Interpretation of Anthropometry, Report of a WHO Expert Committee; World Health Organization: Geneva, Switzerland, 1995. [Google Scholar]
- Reilly, J.J. Assessment of childhood obesity: National reference data or international approach? Obes. Res. 2002, 10, 838–840. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, J. A comparison of international references for the assessment of child and adolescent overweight and obesity in different populations. Eur. J. Clin. Nutr. 2002, 56, 973–982. [Google Scholar] [CrossRef] [PubMed]
- Ness-Abramof, R.; Apovian, C.M. Waist circumference measurement in clinical practice. Nutr. Clin. Pract. 2008, 23, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Fosbøl, M.; Zerahn, B. Contemporary methods of body composition measurement. Clin. Physiol. Funct. Imaging 2015, 35, 81–97. [Google Scholar] [CrossRef]
- Cole, T.J.; Faith, M.S.; Pietrobelli, A.; Heo, M. What is the best measure of adiposity change in growing children: BMI, BMI%, BMI z-score or BMI centile? Eur. J. Clin. Nutr. 2005, 59, 419–425. [Google Scholar] [CrossRef]
- De Onis, M.; Lobstein, T. Defining obesity risk status in the general childhood population: Which cut-offs should we use? Int. J. Pediatr. Obes. 2010, 5, 458–460. [Google Scholar] [CrossRef]
- Must, A.; Anderson, S. Body mass index in children and adolescents: Considerations for population-based applications. Int. J. Obes. 2006, 30, 590–594. [Google Scholar] [CrossRef]
- Freedman, D.; Kettel Khan, L.; Serdula, M.; Srinivasan, S.; Berenson, G. BMI rebound, childhood height and obesity among adults: The Bogalusa Heart Study. Int. J. Obes. 2001, 25, 543–549. [Google Scholar] [CrossRef]
- Gearhardt, A.N.; Waller, R.; Jester, J.M.; Hyde, L.W.; Zucker, R.A. Body mass index across adolescence and substance use problems in early adulthood. Psychol. Addict. Behav. 2018, 32, 309. [Google Scholar] [CrossRef]
- Jung, T.; Wickrama, K.A. An introduction to latent class growth analysis and growth mixture modeling. Soc. Personal. Psychol. Compass 2008, 2, 302–317. [Google Scholar] [CrossRef]
- McNeish, D.; Harring, J.R. Correcting model fit criteria for small sample latent growth models with incomplete data. Educ. Psychol. Meas. 2017, 77, 990–1018. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.K.; DiBari, J.N. Marked disparities in pre-pregnancy obesity and overweight prevalence among US women by race/ethnicity, nativity/immigrant status, and sociodemographic characteristics, 2012–2014. J. Obes. 2019, 2019, 2419263. [Google Scholar] [CrossRef]
- Hartono, S.; Cochrane, T.; Niyonsenga, T.; Kinfu, Y. A longitudinal analysis of the effect of maternal region-of-birth on transitions in children’s bodyweight status from early childhood to late adolescence in Australia: A population-based cohort study. Prev. Med. 2021, 153, 106832. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Herrmann, S.D.; Barreira, T.V.; Kang, M.; Ainsworth, B.E. How many hours are enough? Accelerometer wear time may provide bias in daily activity estimates. J. Phys. Act. Health 2013, 10, 742–749. [Google Scholar] [CrossRef] [PubMed]
- Sember, V.; Meh, K.; Sorić, M.; Starc, G.; Rocha, P.; Jurak, G. Validity and reliability of international physical activity questionnaires for adults across EU countries: Systematic review and meta analysis. Int. J. Environ. Res. Public Health 2020, 17, 7161. [Google Scholar] [CrossRef]
- Colley, R.C.; Butler, G.; Garriguet, D.; Prince, S.A.; Roberts, K.C. Comparison of self-reported and accelerometer-measured physical activity among Canadian youth. Health Rep 2019, 30, 3–12. [Google Scholar]
- Fanelli, E.; Abate Daga, F.; Pappaccogli, M.; Eula, E.; Astarita, A.; Mingrone, G.; Fasano, C.; Magnino, C.; Schiavone, D.; Rabbone, I.; et al. A structured physical activity program in an adolescent population with overweight or obesity: A prospective interventional study. Appl. Physiol. Nutr. Metab. 2022, 47, 253–260. [Google Scholar] [CrossRef]
- Schranz, N.; Tomkinson, G.; Parletta, N.; Petkov, J.; Olds, T. Can resistance training change the strength, body composition and self-concept of overweight and obese adolescent males? A randomised controlled trial. Br. J. Sport. Med. 2014, 48, 1482–1488. [Google Scholar] [CrossRef]
- Swift, D.L.; McGee, J.E.; Earnest, C.P.; Carlisle, E.; Nygard, M.; Johannsen, N.M. The effects of exercise and physical activity on weight loss and maintenance. Prog. Cardiovasc. Dis. 2018, 61, 206–213. [Google Scholar] [CrossRef]
- Church, T.S.; Earnest, C.P.; Skinner, J.S.; Blair, S.N. Effects of different doses of physical activity on cardiorespiratory fitness among sedentary, overweight or obese postmenopausal women with elevated blood pressure: A randomized controlled trial. JAMA 2007, 297, 2081–2091. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, J.E.; Blair, S.N.; Jakicic, J.M.; Manore, M.M.; Rankin, J.W.; Smith, B.K. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med. Sci. Sport. Exerc. 2009, 41, 459–471. [Google Scholar] [CrossRef] [PubMed]
- Bray, M.S.; Loos, R.J.; McCaffery, J.M.; Ling, C.; Franks, P.W.; Weinstock, G.M.; Snyder, M.P.; Vassy, J.L.; Agurs-Collins, T.; Group, C.W. NIH working group report—using genomic information to guide weight management: From universal to precision treatment. Obesity 2016, 24, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Leibel, R.L.; Seeley, R.J.; Darsow, T.; Berg, E.G.; Smith, S.R.; Ratner, R. Biologic responses to weight loss and weight regain: Report from an American Diabetes Association research symposium. Diabetes 2015, 64, 2299–2309. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Xia, Y.; Sun, Y.; Guo, Y.; Shi, Z.; do Vale Moreira, N.C.; Zuo, H.; Hussain, A. Effect of lifestyle intervention on HbA1c levels in overweight and obese adults with type 2 diabetes across ethnicities: A systematic review and meta-analysis of randomized controlled trials. Diabetes Res. Clin. Pract. 2023, 199, 110662. [Google Scholar] [CrossRef]
- Peña, M.M.; Dixon, B.; Taveras, E.M. Are you talking to ME? The importance of ethnicity and culture in childhood obesity prevention and management. Child. Obes. 2012, 8, 23–27. [Google Scholar] [CrossRef]
- DeBoer, M.D. Ethnicity, obesity and the metabolic syndrome: Implications on assessing risk and targeting intervention. Expert Rev. Endocrinol. Metab. 2011, 6, 279–289. [Google Scholar] [CrossRef]


| Asians | Blacks | Hispanics | Whites | p-Value | ||
|---|---|---|---|---|---|---|
| Sedentary time | Total | 458.35 ± 116.67 | 331.52 ± 160.13 | 308.03 ± 137.57 | 307.72 ± 170.83 | <0.05 |
| Girls | 464.52 ± 160.74 | 364.27 ± 194.64 | 204.48 ± 100.34 | 339.26 ± 138.85 | <0.05 | |
| Boys | 452.31 ± 140.52 | 396.36 ± 211.07 | 219.21 ± 99.68 | 360.42 ± 121.50 | <0.05 | |
| Moderate activity | Total | 29.42 ± 15.89 | 60.64 ± 27.92 | 65.10 ± 37.48 | 54.12 ± 35.61 | <0.05 |
| Girls | 20.43 ± 10.05 | 80.05 ± 73.36 | 61.01 ± 12.56 | 44.07 ± 19.86 | <0.05 | |
| Boys | 26.14 ± 11.36 | 92.42 ± 59.79 | 97.30 ± 45.68 | 57.63 ± 27.58 | <0.05 | |
| Vigorous activity | Total | 10.80 ± 3.11 | 5.93 ± 4.49 | 9.04 ± 7.22 | 13.06 ± 13.47 | <0.05 |
| Girls | 8.22 ± 2.83 | 11.79 ± 7.60 | 11.57 ± 9.15 | 13.24 ± 10.58 | <0.05 | |
| Boys | 12.00 ± 3.42 | 15.69 ± 7.31 | 16.54 ± 12.37 | 18.13 ± 13.34 | <0.05 | |
| Significant differences between cohorts are marked in bold. | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Statsenko, Y.; Smetanina, D.; Simiyu, G.L.; Belghali, M.; Ghenimi, N.; Mannaerts, G.H.H.; Almaramah, L.; Alhashmi, M.; Chun Mohammad, N.; Al Hamed, R.; et al. Race, Ethnicity, and Geography as Determinants of Excessive Weight and Low Physical Activity in Pediatric Population: Protocol for Systematic Review and Meta-Analysis. Healthcare 2024, 12, 1830. https://doi.org/10.3390/healthcare12181830
Statsenko Y, Smetanina D, Simiyu GL, Belghali M, Ghenimi N, Mannaerts GHH, Almaramah L, Alhashmi M, Chun Mohammad N, Al Hamed R, et al. Race, Ethnicity, and Geography as Determinants of Excessive Weight and Low Physical Activity in Pediatric Population: Protocol for Systematic Review and Meta-Analysis. Healthcare. 2024; 12(18):1830. https://doi.org/10.3390/healthcare12181830
Chicago/Turabian StyleStatsenko, Yauhen, Darya Smetanina, Gillian Lylian Simiyu, Maroua Belghali, Nadirah Ghenimi, Guido Hein Huib Mannaerts, Leena Almaramah, Maryam Alhashmi, Nazia Chun Mohammad, Rahaf Al Hamed, and et al. 2024. "Race, Ethnicity, and Geography as Determinants of Excessive Weight and Low Physical Activity in Pediatric Population: Protocol for Systematic Review and Meta-Analysis" Healthcare 12, no. 18: 1830. https://doi.org/10.3390/healthcare12181830
APA StyleStatsenko, Y., Smetanina, D., Simiyu, G. L., Belghali, M., Ghenimi, N., Mannaerts, G. H. H., Almaramah, L., Alhashmi, M., Chun Mohammad, N., Al Hamed, R., Alblooshi, S. F., Talbi, K., Albreiki, M., Alkaabi, F., Ponomareva, A., & Ljubisavljevic, M. (2024). Race, Ethnicity, and Geography as Determinants of Excessive Weight and Low Physical Activity in Pediatric Population: Protocol for Systematic Review and Meta-Analysis. Healthcare, 12(18), 1830. https://doi.org/10.3390/healthcare12181830







